Physical Activity Participation of Black and White Women during the First Year Postpartum: Results and Study Recruitment Strategies
Abstract
:1. Introduction
2. Methods
2.1. Recruitment Process
2.2. Physical Activity Measurement
2.3. Statistical Analysis
3. Results
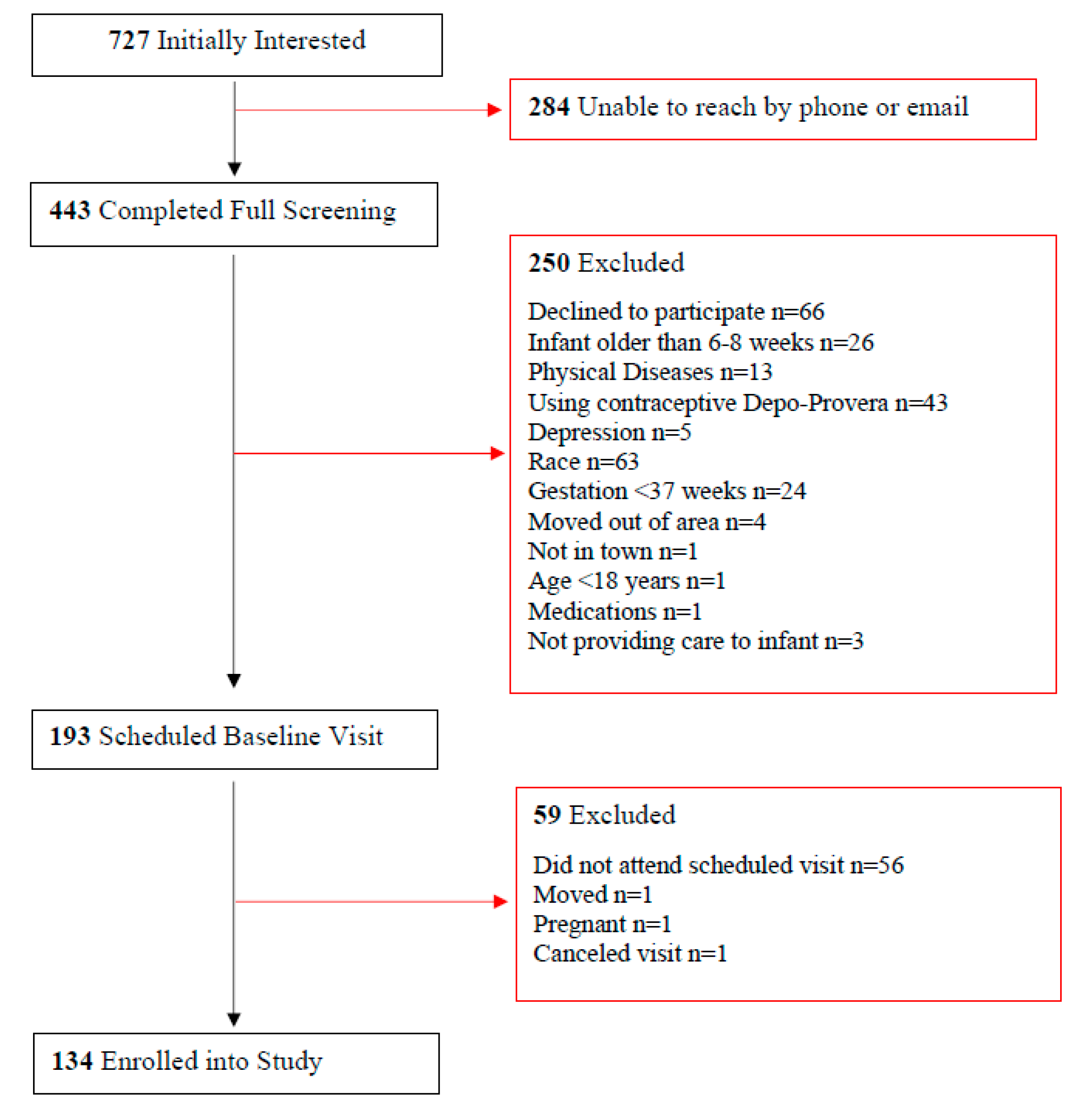
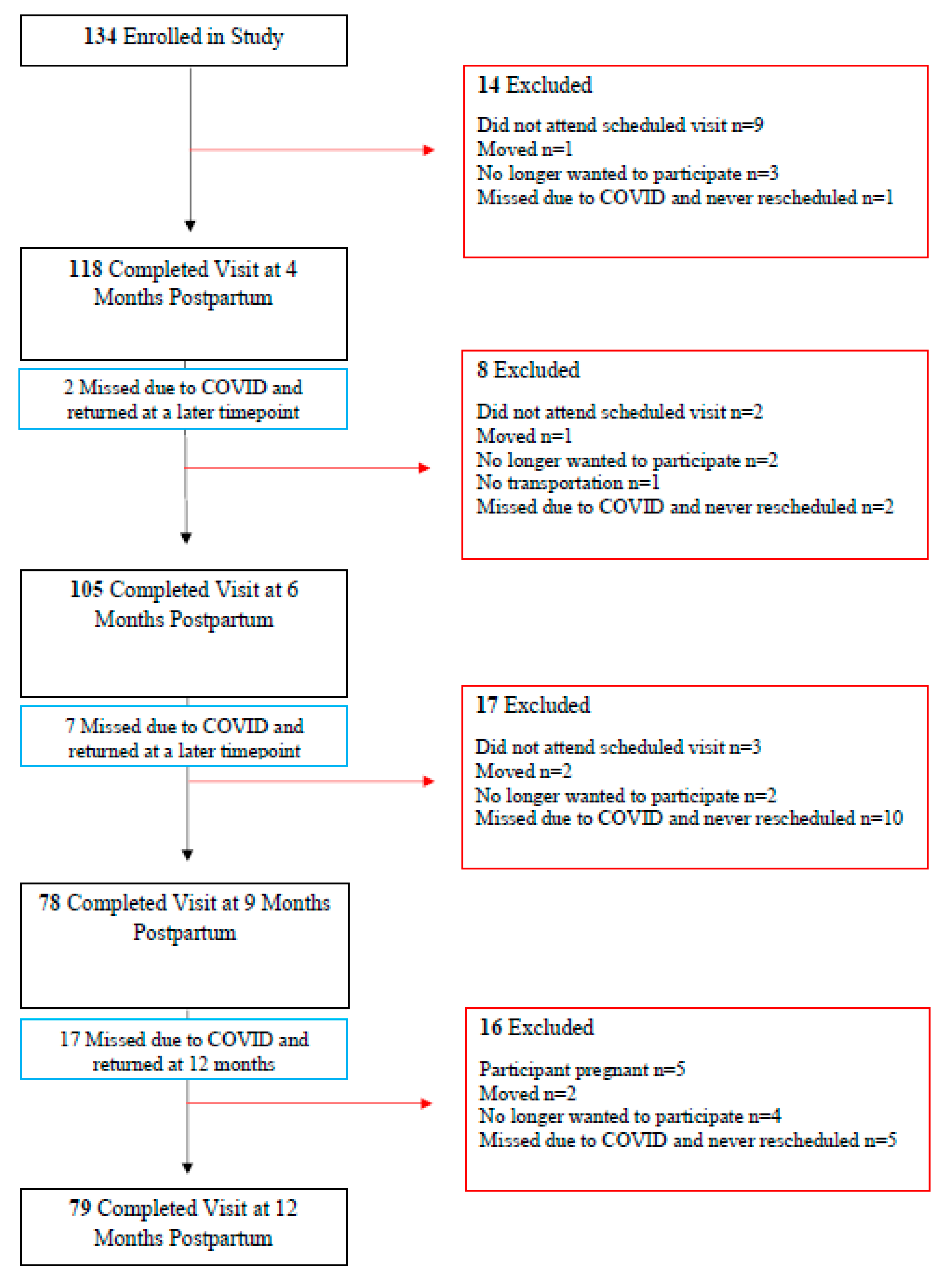
3.1. Recruitment Yield and Recruitment Strategy
3.2. Characteristics of Enrolled Participants
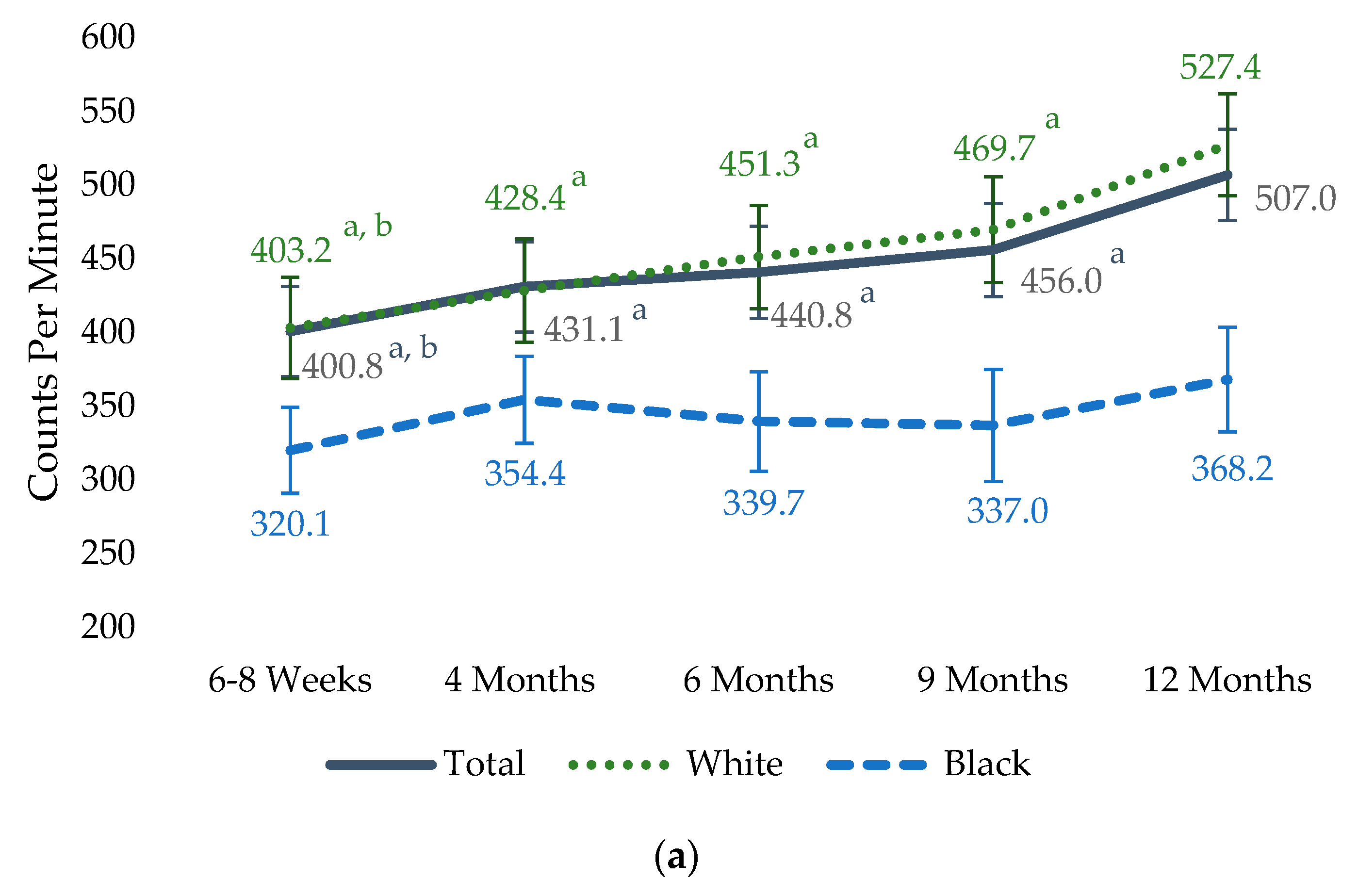
3.3. Physical Activity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Strasser, B. Physical activity in obesity and metabolic syndrome. Ann. N. Y. Acad. Sci. 2013, 1281, 141–159. [Google Scholar] [CrossRef] [PubMed]
- Kraus, W.E.; Powell, K.E.; Haskell, W.L.; Janz, K.F.; Campbell, W.W.; Jakicic, J.M.; Troiano, R.P.; Sprow, K.; Torres, A.; Piercy, K.L. Physical activity, all-cause and cardiovascular mortality, and cardiovascular disease. Med. Sci. Sports Exerc. 2019, 51, 1270. [Google Scholar] [CrossRef] [PubMed]
- He, D.; Xi, B.; Xue, J.; Huai, P.; Zhang, M.; Li, J. Association between leisure time physical activity and metabolic syndrome: A meta-analysis of prospective cohort studies. Endocrine 2014, 46, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Mammen, G.; Faulkner, G. Physical activity and the prevention of depression: A systematic review of prospective studies. Am. J. Prev. Med. 2013, 45, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Stensel, D.J.; Hardman, A.E.; Gill, J.M. Physical Activity and Health: The Evidence Explained, 3rd ed.; Routledge: London, UK, 2021. [Google Scholar]
- Ha, A.V.V.; Zhao, Y.; Binns, C.W.; Pham, N.M.; Nguyen, P.T.H.; Nguyen, C.L.; Chu, T.K.; Lee, A.H. Postpartum physical activity and weight retention within one year: A prospective cohort study in Vietnam. Int. J. Environ. Res. Public Health 2020, 17, 1105. [Google Scholar] [CrossRef]
- The American College of Obstetricians and Gynecologists. Physical activity and exercise during pregnancy and the postpartum period: ACOG Committee Opinion Summary, Number 804. Obstet. Gynecol 2020, 135, 991–993. [Google Scholar] [CrossRef]
- DiPietro, L.; Evenson, K.R.; Bloodgood, B.; Sprow, K.; Troiano, R.P.; Piercy, K.L.; Vaux-Bjerke, A.; Powell, K.E. Benefits of physical activity during pregnancy and postpartum: An umbrella review. Med. Sci. Sports Exerc. 2019, 51, 1292. [Google Scholar] [CrossRef]
- Blum, J.W.; Beaudoin, C.M.; Caton-Lemos, L. Physical activity patterns and maternal well-being in postpartum women. Matern. Child Health J. 2004, 8, 163–169. [Google Scholar] [CrossRef]
- Office of Disease Prevention and Health Promotion. 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report; Office of Disease Prevention and Health Promotion: Washington, DC, USA, 2018.
- Saligheh, M.; McNamara, B.; Rooney, R. Perceived barriers and enablers of physical activity in postpartum women: A qualitative approach. BMC Pregnancy Childbirth 2016, 16, 131. [Google Scholar] [CrossRef]
- Evenson, K.R.; Herring, A.H.; Wen, F. Self-reported and objectively measured physical activity among a cohort of postpartum women: The PIN postpartum study. J. Phys. Act. Health 2012, 9, 5–20. [Google Scholar] [CrossRef]
- Hesketh, K.R.; Evenson, K.R.; Stroo, M.; Clancy, S.M.; Østbye, T.; Benjamin-Neelon, S.E. Physical activity and sedentary behavior during pregnancy and postpartum, measured using hip and wrist-worn accelerometers. Prev. Med. Rep. 2018, 10, 337–345. [Google Scholar] [CrossRef]
- Evenson, K.R.; Brouwer, R.J.; Østbye, T. Changes in physical activity among postpartum overweight and obese women: Results from the KAN-DO study. Women Health 2013, 53, 317–334. [Google Scholar] [CrossRef] [PubMed]
- Wolpern, A.E.; Bardsley, T.R.; Brusseau, T.A.; Byun, W.; Egger, M.J.; Nygaard, I.E.; Wu, J.; Shaw, J.M. Physical activity in the early postpartum period in primiparous women. J. Sci. Med. Sport. 2021, 24, 1149–1154. [Google Scholar] [CrossRef] [PubMed]
- Fuezeki, E.; Engeroff, T.; Banzer, W. Health benefits of light-intensity physical activity: A systematic review of accelerometer data of the National Health and Nutrition Examination Survey (NHANES). Sports Med. 2017, 47, 1769–1793. [Google Scholar] [CrossRef] [PubMed]
- Rezende, L.F.M.D.; Rodrigues Lopes, M.; Rey-López, J.P.; Matsudo, V.K.R.; Luiz, O.D.C. Sedentary Behavior and Health Outcomes: An Overview of Systematic Reviews. PLoS ONE 2014, 9, e105620. [Google Scholar] [CrossRef] [PubMed]
- Hawes, A.M.; Smith, G.S.; McGinty, E.; Bell, C.; Bower, K.; LaVeist, T.A.; Gaskin, D.J.; Thorpe, R.J., Jr. Disentangling race, poverty, and place in disparities in physical activity. Int. J. Environ. Res. Public. Health 2019, 16, 1193. [Google Scholar] [CrossRef]
- Flanagin, A.; Frey, T.; Christiansen, S.L.; AMA Manual of Style Committee. Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA 2021, 326, 621–627. [Google Scholar] [CrossRef]
- Daniels, L.A.; Wilson, J.L.; Mallan, K.M.; Mihrshahi, S.; Perry, R.; Nicholson, J.M.; Magarey, A. Recruiting and engaging new mothers in nutrition research studies: Lessons from the Australian NOURISH randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 129. [Google Scholar] [CrossRef]
- Infanti, J.J.; O’Dea, A.; Gibson, I.; McGuire, B.E.; Newell, J.; Glynn, L.G.; O’Neill, C.; Connolly, S.B.; Dunne, F.P. Reasons for participation and non-participation in a diabetes prevention trial among women with prior gestational diabetes mellitus (GDM). BMC Med. Res. Methodol. 2014, 14, 13. [Google Scholar] [CrossRef]
- Martin, A.; Negron, R.; Balbierz, A.; Bickell, N.; Howell, E.A. Recruitment of black and Latina women to a randomized controlled trial. J. Health Care Poor Underserved 2013, 24, 1102–1114. [Google Scholar] [CrossRef]
- Sweet, S.; Legro, R.S.; Coney, P. A comparison of methods and results in recruiting white and black women into reproductive studies: The MMC–PSU cooperative center on reproduction experience. Contemp. Clin. Trials 2008, 29, 478–481. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Kishman, E.E.; Liu, J.; Castleberry, L.A.; McLain, A.; Sparks, J.R.; Cook, J.W. Body weight and fat trajectories of Black and White women in the first postpartum year. Obesity 2023, 31, 1655–1665. [Google Scholar] [CrossRef]
- United States Census Bureau. Population Estimates, July 1 2021 (V2021)—Columbia, South Carolina. Available online: https://www.census.gov/quickfacts/columbiacitysouthcarolina (accessed on 20 November 2022).
- Choi, L.; Liu, Z.; Matthews, C.E.; Buchowski, M.S. Validation of accelerometer wear and nonwear time classification algorithm. Med. Sci. Sports Exerc. 2011, 43, 357. [Google Scholar] [CrossRef] [PubMed]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Masse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181. [Google Scholar] [CrossRef]
- Trost, S.G.; Mciver, K.L.; Pate, R.R. Conducting accelerometer-based activity assessments in field-based research. Med. Sci. Sports Exerc. 2005, 37, S531–S543. [Google Scholar] [CrossRef]
- Swartz, A.M.; Strath, S.J.; Bassett, D.R.; O’Brien, W.L.; King, G.A.; Ainsworth, B.E. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Med. Sci. Sports Exerc. 2000, 32, S450–S456. [Google Scholar] [CrossRef]
- Nicklas, J.M.; Skurnik, G.; Zera, C.A.; Reforma, L.G.; Levkoff, S.E.; Seely, E.W. Employing a multi-level approach to recruit a representative sample of women with recent gestational diabetes mellitus into a randomized lifestyle intervention trial. Matern. Child Health J. 2016, 20, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Wilcox, S.; Wingard, E.; Burgis, J.; Schneider, L.; Dahl, A. Strategies and Challenges in Recruiting Pregnant Women with Elevated Body Mass Index for a Behavioral Lifestyle Intervention. Women Health Rep. 2020, 1, 556–565. [Google Scholar] [CrossRef] [PubMed]
- Sutton, E.F.; Cain, L.E.; Vallo, P.M.; Redman, L.M. Strategies for successful recruitment of pregnant patients into clinical trials. Obstet. Gynecol 2017, 129, 554. [Google Scholar] [CrossRef]

| Recruitment Strategy | Initially Interested n (% of Total Interested) | Enrolled in Study n (% of Enrolled, % of Initially Interested in the Specific Strategy) | Completed Study n (% of Completed, % of Enrolled for the Specific Strategy) | ||||
|---|---|---|---|---|---|---|---|
| Total n = 727 | Total n = 134 | White n = 85 | Black n = 49 | Total n = 79 | White n = 58 | Black n = 21 | |
| Lactation and Newborn Clinic | 337 (46) | 47 (35, 14) | 25 (29, 7) | 22 (45, 6) | 30 (38, 64) | 18 (31, 72) | 12 (57, 55) |
| Labor and Delivery Units | 183 (25) | 30 (22, 16) | 11 (13, 6) | 19 (39, 10) | 11 (14, 37) | 5 (9, 45) | 6 (28, 32) |
| Physician Recruitment at Obstetric Clinics | 76 (10) | 21 (16, 28) | 15 (18, 20) | 6 (12, 9) | 10 (13, 48) | 9 (15, 60) | 1 (5, 17) |
| Blogs | 36 (5) | 20 (15, 56) | 19 (22, 53) | 1 (2, 3) | 16 (20, 80) | 15 (25, 79) | 1 (5, 100) |
| Self-Referred | 34 (7) | 10 (7, 29) | 9 (11, 26) | 1 (2, 3) | 8 (10, 80) | 7 (12, 78) | 1 (5, 100) |
| Research Staff at Obstetric Clinics | 23 (3) | 1 (1, 4) | 1 (1, 4) | 0 (0, 0) | 1 (1, 100) | 1 (2, 100) | 0 (0, 0) |
| Community Events | 21 (3) | 1 (1, 5) | 1 (1, 5) | 0 (0, 0) | 1 (1, 100) | 1 (2, 100) | 0 (0, 0) |
| Interest Forms at Obstetric Clinics | 10 (1) | 1 (1, 10) | 1 (1, 10) | 0 (0, 0) | 1 (1, 100) | 1 (2, 100) | 0 (0, 0) |
| Flyers Placed at Various Locations | 5 (<1) | 2 (1, 40) | 2 (2, 40) | 0 (0, 0) | 1 (1, 50) | 1 (2, 50) | 0 (0, 0) |
| Advertisements on Radio | 2 (<1) | 1 (1, 50) | 1 (1, 50) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) |
| Total (n = 134) | White (n = 85) | Black (n = 49) | p-Value | |
|---|---|---|---|---|
| Age (years) | 30.4 ± 4.8 | 31.7 ± 4.1 | 28.0 ± 5.1 | <0.0001 |
| Weight (kg) | 79.7 ± 18.5 | 76.9 ± 15.1 | 84.6 ± 22.6 | 0.002 |
| BMI Status | 0.036 | |||
| Normal | 31 (23) | 22 (26) | 9 (18) | |
| Overweight | 51 (38) | 37 (44) | 14 (29) | |
| Obese | 52 (39) | 26 (30) | 26 (53) | |
| Parity | 0.715 | |||
| Primiparous | 50 (39) | 33 (40) | 17 (37) | |
| Multiparous | 78 (61) | 49 (60) | 29 (63) | |
| Breastfeeding Status | 0.002 | |||
| Exclusively | 93 (69) | 68 (80) | 25 (51) | |
| Some | 15 (12) | 8 (9) | 7 (15) | |
| None | 26 (19) | 9 (11) | 17 (34) | |
| Type of Delivery | 0.461 | |||
| Vaginal | 95 (73) | 61 (75) | 34 (69) | |
| Cesarean section | 35 (27) | 20 (25) | 15 (31) | |
| Relationship Status | 0.001 | |||
| Married or stable relationship | 118 (88) | 82 (97) | 36 (74) | |
| Married or stable relationship but not living with partner | 7 (5) | 1 (1) | 6 (12) | |
| Divorced or widowed | 3 (2) | 2 (2) | 1 (2) | |
| Not in a relationship | 6 (5) | 0 (0) | 6 (12) | |
| Education | 0.002 | |||
| Some high school | 1 (1) | 1 (1) | 0 (0) | |
| High school graduate | 12 (9) | 5 (6) | 7 (14) | |
| College 1–3 years | 42 (31) | 18 (21) | 24 (50) | |
| College graduate | 40 (30) | 31 (37) | 9 (18) | |
| Graduate school | 39 (29) | 30 (35) | 9 (18) | |
| Income (USD) | 0.001 | |||
| 0 to 19,999 | 10 (8) | 2 (2) | 8 (16) | |
| 20,000 to 39,999 | 30 (22) | 17 (20) | 13 (27) | |
| 40,000 to 59,999 | 26 (19) | 14 (17) | 12 (25) | |
| 60,000 to 79,999 | 20 (15) | 11 (13) | 9 (18) | |
| 80,000 to 99,999 | 12 (9) | 8 (9) | 4 (8) | |
| 100,000 to 120,000 | 16 (12) | 15 (18) | 1 (2) | |
| 120,000+ | 20 (15) | 18 (21) | 2 (4) | |
| Employment | 0.283 | |||
| On maternity leave | 57 (44) | 40 (49) | 17 (36) | |
| Employed | 37 (29) | 20 (24) | 17 (36) | |
| Unemployed | 35 (27) | 22 (27) | 13 (28) |
| Completed Study (n = 79) | Dropped (n = 55) | p-Value | |
|---|---|---|---|
| Age (years) | 31.3 ± 4.2 | 29.0 ± 5.4 | 0.009 |
| Weight (kg) | 80.4 ± 18.8 | 78.7 ± 18.2 | 0.612 |
| Percent Meeting Physical Activity Guidelines a | 46 (58) | 21 (38) | 0.015 |
| Race | 0.004 | ||
| White | 58 (73) | 27 (49) | |
| Black | 21 (27) | 28 (51) | |
| Breastfeeding | 0.015 | ||
| Exclusively | 59 (75) | 34 (62) | |
| Some | 11 (14) | 4 (7) | |
| None | 9 (11) | 17 (31) | |
| Relationship Status | |||
| Married or stable relationship | 71 (89) | 47 (85) | 0.397 |
| Married or stable relationship but not living with partner | 2 (3) | 5 (9) | |
| Divorced or widowed | 2 (3) | 1 (2) | |
| Not in a relationship | 4 (5) | 2 (4) | |
| Education | 0.001 | ||
| Some high school | 1 (1) | 0 (0) | |
| High school graduate | 2 (3) | 10 (18) | |
| College 1–3 years | 19 (24) | 23 (42) | |
| College graduate | 31 (39) | 9 (16) | |
| Graduate school | 26 (33) | 13 (24) | |
| Income (USD) | 0.217 | ||
| 0 to 19,999 | 3 (4) | 7 (13) | |
| 20,000 to 39,999 | 16 (20) | 14 (25) | |
| 40,000 to 59,999 | 17 (22) | 9 (16) | |
| 60,000 to 79,999 | 13 (16) | 7 (13) | |
| 80,000 to 99,999 | 5 (6) | 7 (13) | |
| 100,000 to 120,000 | 10 (13) | 6 (11) | |
| 120,000+ | 15 (19) | 5 (9) | |
| Employment | 0.063 | ||
| On maternity leave | 41 (52) | 18 (33) | |
| Employed | 18 (23) | 21 (38) | |
| Unemployed | 20 (25) | 16 (29) |
| Troiano | Swartz | |||||
|---|---|---|---|---|---|---|
| Total | White | Black | Total | White | Black | |
| LPA | ||||||
| 6–8 Weeks | 165.2 (9.8) a | 163.5 (9.9) a | 150.0 (10.9) | 95.3 (4.9) a | 96.4 (5.1) a | 85.0 (5.4) |
| 4 Months | 174.4 (9.8) | 171.0 (10.1) a | 160.6 (11.0) | 99.5 (4.9) | 99.9 (5.2) b | 90.4 (5.5) |
| 6 Months | 174.4 (9.9) | 173.1 (10.1) b | 156.8 (12.5) | 100.4 (5.0) | 101.1 (5.2) | 91.2 (6.3) |
| 9 Months | 175.9 (10.0) | 173.5 (10.3) | 159.3 (13.9) | 100.8 (5.0) | 100.6 (5.3) | 94.4 (7.0) |
| 12 Months | 185.0 (9.8) | 185.3 (10.0) | 160.0 (13.0) | 104.6 (4.9) | 106.5 (5.1) | 89.9 (6.5) |
| MVPA | ||||||
| 6–8 Weeks | 21.5 (3.1) a | 21.9 (3.9) | 18.2 (3.1) | 91.2 (7.9) a | 88.7 (8.5) a | 83.4 (8.6) |
| 4 Months | 22.1 (3.1) a | 21.5 (4.0) b | 19.6 (3.1) | 97.1 (7.9) b | 93.0 (8.6) a | 89.6 (8.7) |
| 6 Months | 22.2 (3.2) a | 22.4 (4.0) b | 18.4 (3.6) | 96.1 (8.0) a | 94.7 (8.6) b | 83.5 (9.9) |
| 9 Months | 24.1 (3.3) | 24.7 (4.1) | 18.0 (4.0) | 99.2 (8.1) | 97.9 (8.8) | 82.2 (10.9) |
| 12 Months | 27.6 (3.2) | 27.7 (3.9) | 24.3 (3.7) | 108.1 (7.9) | 106.8 (8.5) | 93.7 (10.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kishman, E.E.; Castleberry, L.A.; Wang, X. Physical Activity Participation of Black and White Women during the First Year Postpartum: Results and Study Recruitment Strategies. Healthcare 2023, 11, 2625. https://doi.org/10.3390/healthcare11192625
Kishman EE, Castleberry LA, Wang X. Physical Activity Participation of Black and White Women during the First Year Postpartum: Results and Study Recruitment Strategies. Healthcare. 2023; 11(19):2625. https://doi.org/10.3390/healthcare11192625
Chicago/Turabian StyleKishman, Erin E., Lauren A. Castleberry, and Xuewen Wang. 2023. "Physical Activity Participation of Black and White Women during the First Year Postpartum: Results and Study Recruitment Strategies" Healthcare 11, no. 19: 2625. https://doi.org/10.3390/healthcare11192625
APA StyleKishman, E. E., Castleberry, L. A., & Wang, X. (2023). Physical Activity Participation of Black and White Women during the First Year Postpartum: Results and Study Recruitment Strategies. Healthcare, 11(19), 2625. https://doi.org/10.3390/healthcare11192625







