Using Lean Six Sigma in a Private Hospital Setting to Reduce Trauma Orthopedic Patient Waiting Times and Associated Administrative and Consultant Caseload
Abstract
1. Introduction
2. Methods
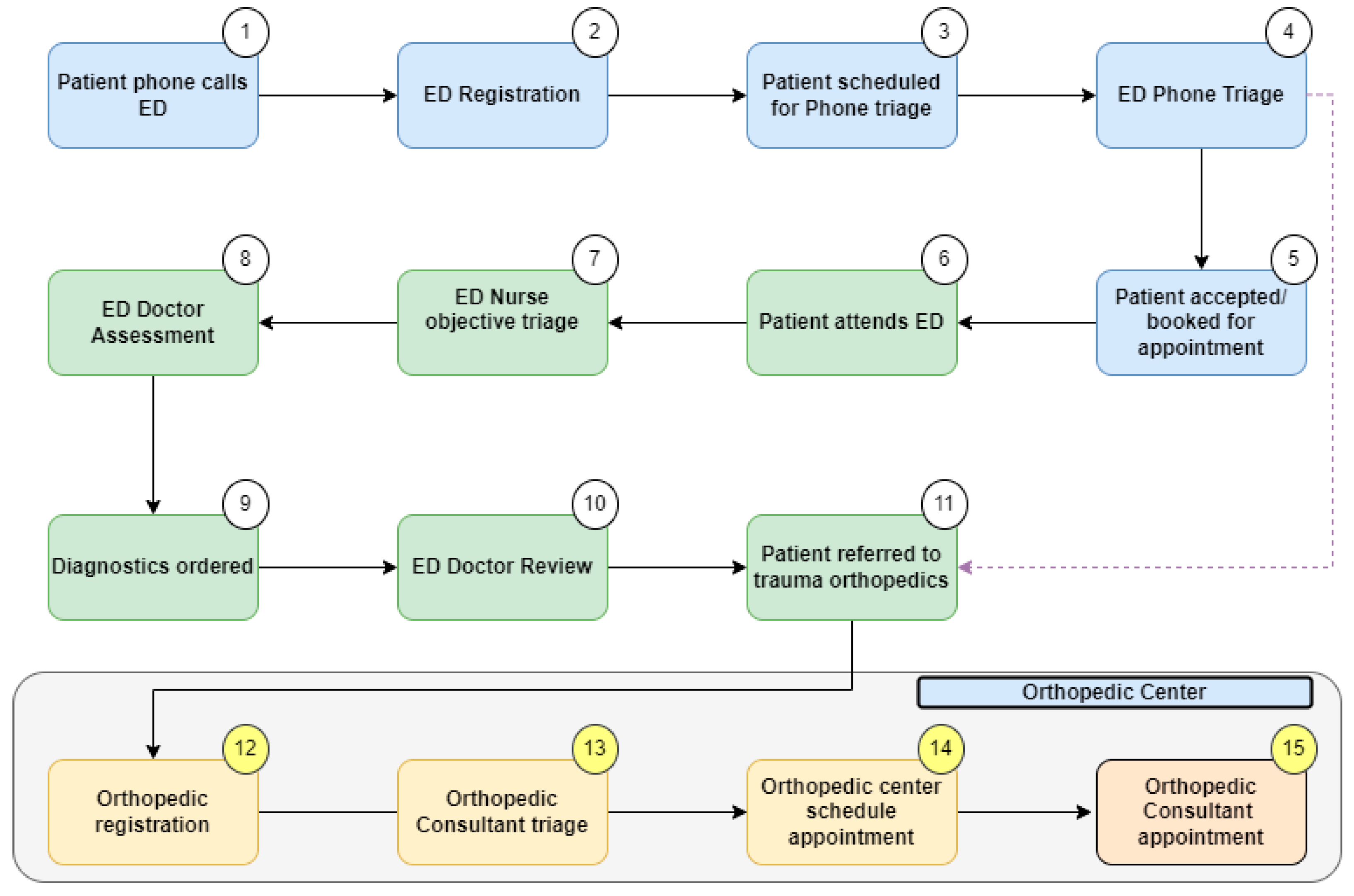
2.1. Define Phase
- Waiting times:
- for a patient to be registered in the orthopedic service as a trauma orthopedic referral from the ED and informed of the receipt of their referral via text message;
- for the consultant to triage the referral;
- for the patient to attend their orthopedic trauma appointment following the ED referral.
- Time taken and number of steps or touch points (points at which staff come into contact with the patient or action the referral) to:
- register a referral;
- triage a referral;
- book the patient’s appointment.
- The efficiency of the trauma consultant’s (total n = 6) caseload is represented by the following:
- opportunity to review the elective caseload;
- conversion rate from appointment to surgery.
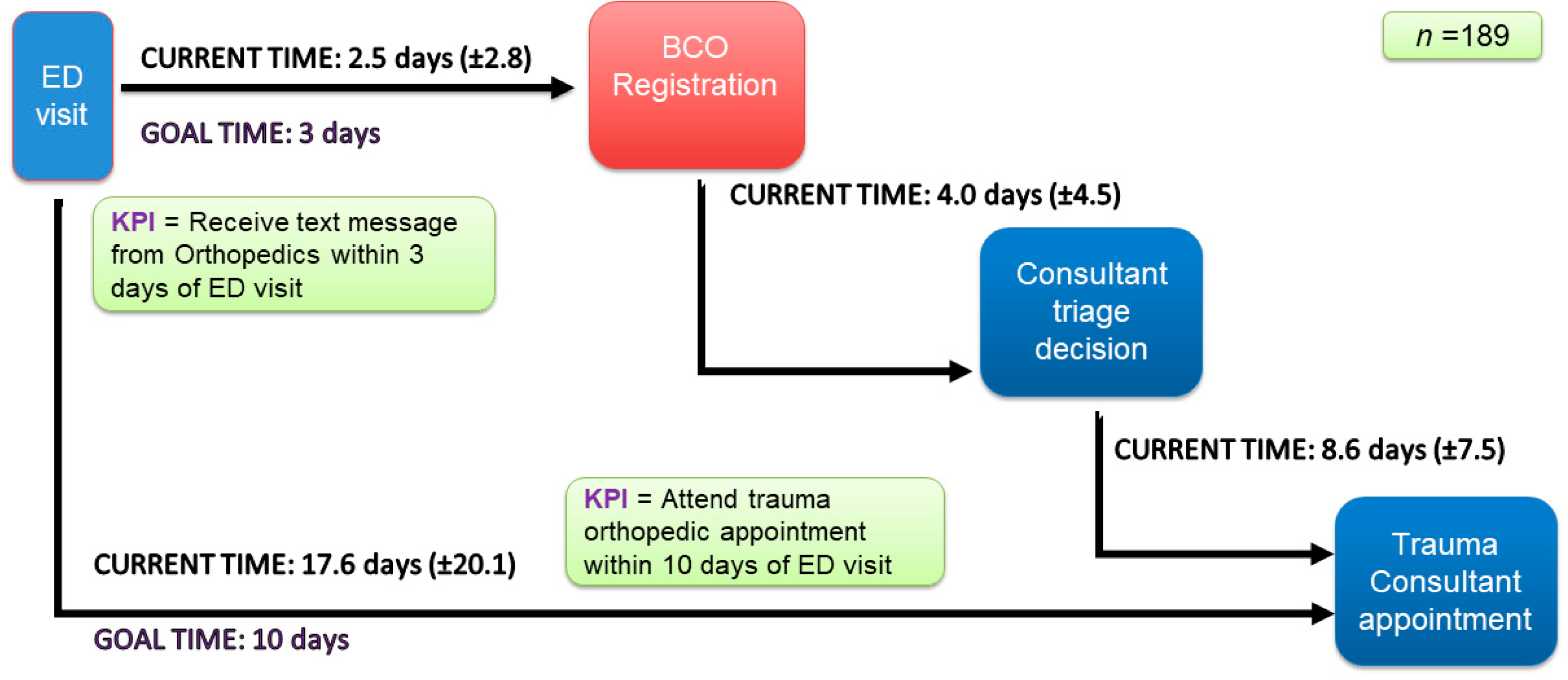
2.2. Measure Phase
2.3. Analyze Phase
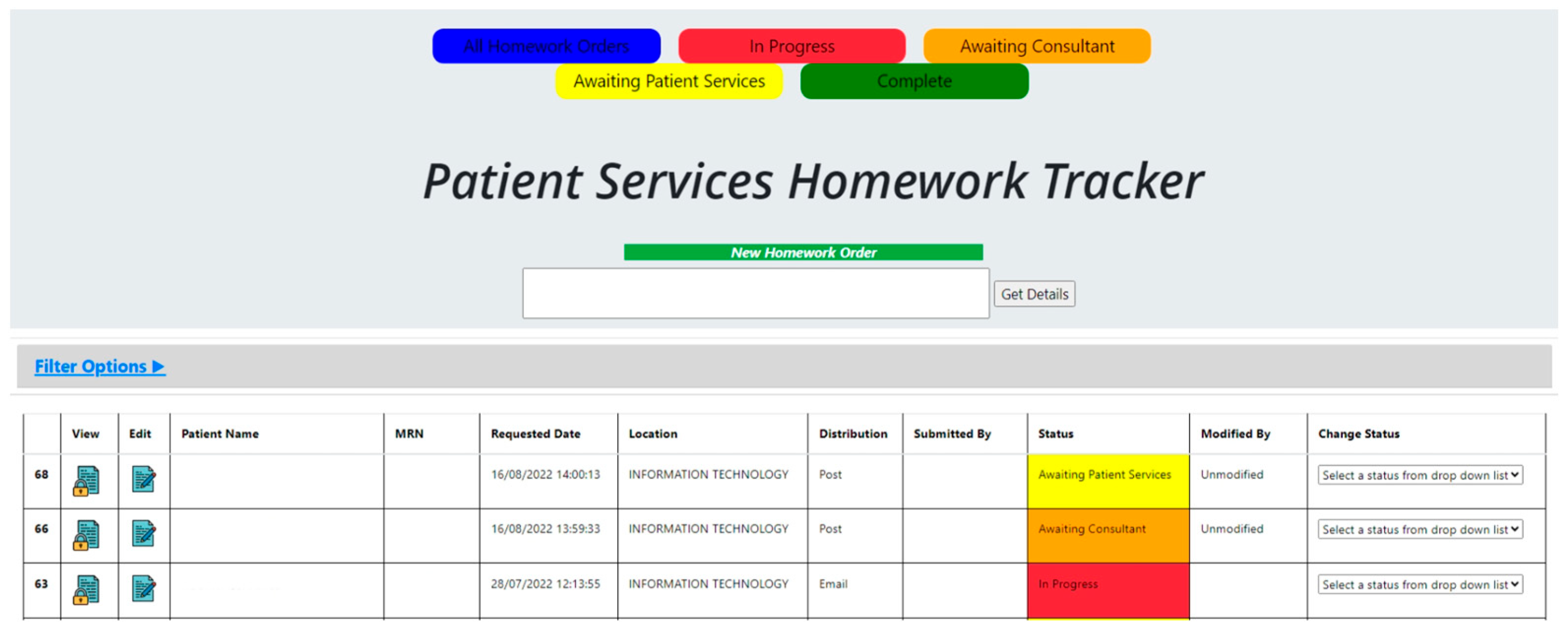
2.4. Improve Phase
- (1)
- Designing an IT system to track and triage patients (the “Patient Services Homework Tracker”).
- (2)
- Ring-fencing trauma orthopedic slots.
- (3)
- Developing an information leaflet about the pathway for staff and patients.
- (4)
- Offering physiotherapy as opposed to consultant review (where clinically indicated) as an option for patients.
- (5)
- Creating a consultant triage roster to enable optimal communication between the team with improved visibility of staffing.
- The urgency of the appointment is classified by the surgeons at the study site as operative routine, non-operative routine, and non-operative urgent.
- Which trauma consultant was the patient referred to by the triaging consultant.
- Whether or not a physiotherapy referral was advised.
3. Results
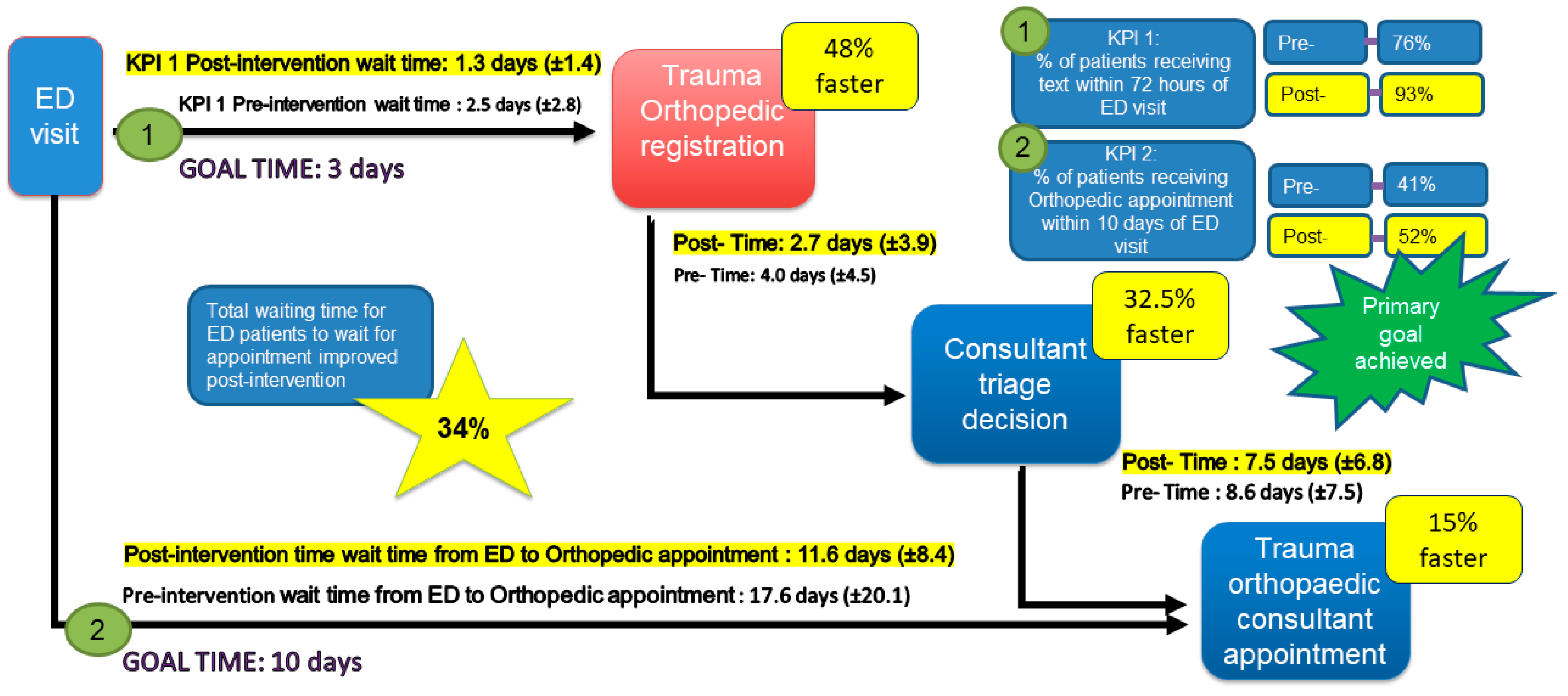
3.1. Reduction in Patient Wait Times
3.2. Reduction in Registering and Triage time, Touch Points, and IT System
3.3. Increased Trauma Consultant Clinic Capacity and Surgical Cases
3.4. Patient and Staff Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cummins, N.M.; Barry, L.A.; Caravan, C.; Devlin, C.; Corey, G.; Cummins, F.; Ryan, D.; Cronin, S.; Wallace, E.; McCarthy, G.; et al. The “better data, better planning” census: A cross-sectional, multi-centre study investigating the factors influencing patient attendance at the emergency department in Ireland. BMC Health Serv. Res. 2022, 22, 471. [Google Scholar] [CrossRef] [PubMed]
- O’Reilly, M.F.; Mohamed, K.M.; Sheehan, E.C. General practitioner attitudes and experiences of orthopedic services in the Irish midlands. Ir. J. Med. Sci. 2019, 188, 735–741. [Google Scholar] [CrossRef] [PubMed]
- RCSI University of Medicine and Health Sciences. Increase in Waiting Lists for Elective Orthopedic Appointments during Pandemic. Royal College of Surgeons in Ireland. Available online: https://www.rcsi.com/dublin/news-and-events/news/news-article/2021/11/increase-in-waiting-lists-for-elective-orthopaedic-appointments-during-pandemic (accessed on 18 August 2022).
- RCSI University of Medicine and Health Sciences. Impact of COVID-19 on Surgical Services Detailed in New NCPS Report. Royal College of Surgeons in Ireland. Available online: https://www.rcsi.com/dublin/news-and-events/news/news-article/2021/10/impact-of-covid-19-on-surgical-services-detailed-in-new-ncps-report (accessed on 18 August 2022).
- Australian Institute of Health and Welfare; Australian Government. Elective Surgery Waiting Times 2021–2022. Elective Surgery Access. Hospitals—Australian Institute of Health and Welfare. Available online: https://www.aihw.gov.au/reports-data/myhospitals/intersection/access/eswt#:~:text=National%20data%20is%20available.,than%20365%20days%20for%20surgery.&text=This%20table%20shows%20waiting%20times,%E2%80%9313%20and%202021%E2%80%9322 (accessed on 7 December 2022).
- NHS England. Statistical Press Notice, NHS Referral to Treatment (RTT) Waiting Times Data September 2022. Available online: https://www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2022/11/Sep22-RTT-SPN-pre-release-version-34691.pdf (accessed on 7 December 2022).
- Glogovac, G.; Kennedy, M.E.; Wesigerber, M.R.; Kakazu, R.; Grawe, B.M. Wait times in musculoskeletal patients: What contributes to patient satisfaction. J. Patient Exp. 2020, 7, 549–553. [Google Scholar] [CrossRef]
- Strategy for the Design of Integrated Outpatient Services 2016–2020, Outpatient Services Improvement Program. Outpatient Services Performance Improvement Programme. Available online: https://www.hse.ie/eng/about/who/acute-hospitals-division/outpatient-services-performance-improvement-programme/ (accessed on 18 August 2022).
- Daly, A.; Teeling, S.P.; Ward, M.; McNamara, M.; Robinson, C. The use of Lean Six Sigma for improving availability of and access to Emergency Department data to facilitate patient flow. Int. J. Environ. Res. Public Health 2021, 18, 11030. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, N.; Teeling, S.P.; Ward, M.; McNamara, M.; Koshy, L. Operation Note Transformation: The application of Lean Six Sigma to improve the process of documenting the operation note in a private hospital setting. Int. J. Environ. Res. Public Health 2021, 18, 12217. [Google Scholar] [CrossRef] [PubMed]
- Fennelly, O.; Blake, C.; Fitzgerald, O.; Breen, R.; Ashton, J.; Brennan, A.; Caffrey, A.; Desmeules, F.; Cunningham, C. Advanced practice physiotherapy-led triage in Irish orthopedic and rheumatology services: National data audit. BMC Musculoskelet. Disord. 2018, 19, 181. [Google Scholar] [CrossRef] [PubMed]
- Teeling, S.P.; Dewing, J.; Baldie, D. A realist inquiry to identify the contribution of Lean Six Sigma to Person-Centered Care and Cultures. Int. J. Environ. Res. Public Health 2021, 18, 10427. [Google Scholar] [CrossRef]
- Antony, J.; Snee, R.; Hoerl, R. Lean Six Sigma: Yesterday, today and tomorrow. Int. J. Qual. Reliab. Manag. 2017, 34, 1073–1093. [Google Scholar] [CrossRef]
- Antony, J. Six Sigma vs. Lean: Some perspectives from leading academics and practitioners. Int. J. Product. Perform. Manag. 2011, 50, 185–190. [Google Scholar] [CrossRef]
- Rosa, A.; Marolla, G.; Lega, F. Lean adoption in hospitals: The role of contextual factors and introduction strategy. BMC Health Serv. Res. 2021, 21, 889. [Google Scholar] [CrossRef]
- Al-Zuheri, A.; Vlachos, I.; Amer, Y. Application of Lean Six Sigma to reduce patient waiting time: Literature Review. Int. J. Qual. Res. 2021, 15, 241–258. [Google Scholar] [CrossRef]
- Kam, A.W.; Collins, S.; Park, T.; Mihail, M.; Stanway, F.F.; Lewis, N.L.; Polya, D.; Fraser-Bell, S.; Roberts, T.V.; Smith, J.E.H. Using Lean Six Sigma techniques to improve efficiency in outpatient ophthalmology clinics. BMC Health Serv. Res. 2021, 21, 38. [Google Scholar] [CrossRef]
- Niemeijer, G.C.; Trip, A.; Ahaus, K.T.; Does, R.J.; Wendt, K.W. Quality in trauma care: Improving the discharge procedure of patients by means of Lean Six Sigma. J. Trauma Acute Care Surg. 2010, 69, 614–618. [Google Scholar] [CrossRef]
- Müller, M.K.; Dedes, K.J.; Dindo, D.; Steiner, S.; Hahnlosser, D.; Clavien, P.A. Impact of clinical pathways in surgery. Langenbeck’s Arch. Surg. 2009, 394, 31–39. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Improta, G.; Balato, G.; Romano, M.; Ponsiglione, A.M.M.; Raiola, E.; Russo, M.A.; Cuccaro, P.; Santillo, L.C.; Cesarelli, M. Improving performances of the knee replacement surgery process by applying DMAIC principles. J. Eval. Clin. Pract. 2017, 23, 1401–1407. [Google Scholar] [CrossRef]
- These, M.S. Observational and interventional study design types: An overview. Biochem. Med. 2014, 23, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Tjahjono, B.; Ball, P.; Vitanov, V.I.; Scorzafave, C.; Nogueira, J.; Calleja, J.; Minguet, M.; Narasimha, L.; Rivas, A.; Srivastava, A.; et al. Six Sigma: Literature Review. Int. J. Lean Six Sigma 2010, 1, 216–233. [Google Scholar] [CrossRef]
- Ogbeiwi, O. General concepts of goals and goal setting in healthcare, a narrative review. J. Manag. Organ. 2021, 27, 324–371. [Google Scholar] [CrossRef]
- Galli, B. Can project management help improve Lean Six Sigma. IEEE Eng. Manag. Rev. 2018, 26, 55–64. [Google Scholar] [CrossRef]
- Riebling, N.B.; Norouzzadeh, S.; Reeder, G.; Mouradian, C.; Hillier, A.; Cowan, R.; Doerfler, M. Quantifying patient satisfaction with process metrics using a weighted bundle approach. BMJ Open Qual. 2019, 8, e000458. [Google Scholar] [CrossRef]
- Found, P.; Harrison, R. Understanding Lean Voice of Customer. Int. J. Lean Six Sigma 2012, 3, 251–257. [Google Scholar] [CrossRef]
- Dalton, J. Gemba Walks. In Great Big Agile; Apress: Berkeley, CA, USA, 2019. [Google Scholar]
- Taghizadegan, S. Mastering Lean Six Sigma: Advanced Black Belt Concepts; Momentum Press: New York, NY, USA, 2013. [Google Scholar]
- Colligan, L.; Anderson, J.E.; Potts, H.W.W.; Berman, J. Does the process map influence the outcome of quality improvement work? A comparison of sequential flow diagram and a hierarchical task analysis diagram. BMC Health Serv. Res. 2010, 10, 7. [Google Scholar] [CrossRef]
- Egan, P.; Pierce, A.; Flynn, A.; Teeling, S.P.; Ward, M.; McNamara, M. Releasing operating room nursing time to care through the reduction of surgical case preparation time: A lean six sigma pilot study. Int. J. Environ. Res. Public Health 2021, 18, 12098. [Google Scholar] [CrossRef]
- Kanamori, S.; Sow, S.; Castro, M.C.; Matsuno, R.; Tsuru, A.; Jimba, M. Implementation of 5S management method for lean healthcare at a health center in Senegal; A qualitative study of staff perception. Glob. Health Action 2015, 8, 27256. [Google Scholar] [CrossRef]
- Brown, R.; Grehan, P.; Brennan, M.; Carter, D.; Brady, A.; Moore, E.; Teeling, S.P.; Ward, M.; Eaton, D. Using Lean Six Sigma to improve rates of day of surgery admission in a national thoracic surgery department. Int. J. Qual. Health Care 2019, 31, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Sarker, A.; Mukhopadhyay, A.; Ghosh, S. An outline of the “Control Phase” for implementing Lean Six Sigma. Int. J. Lean Six Sigma 2014, 5, 230–252. [Google Scholar] [CrossRef]
- O’Reilly, M.; Breathnach, O.; Conlon, B.; Kiernan, C.; Sheehan, E. Trauma assessment clinic: Virtually a safe and smarter way of managing trauma care in Ireland. Injury 2019, 50, 898–902. [Google Scholar] [CrossRef]
- Pacheco, D.; Perher, I.; Vaccaro, G.L.R.; Jung, C.F. 18 comparative aspects between Lean and Six Sigma: Complementarity and implications. Int. J. Lean Six Sigma 2014, 6, 161–175. [Google Scholar] [CrossRef]
- Aij, K.H.; Simons, F.E.; Widdershoven, G.A.M.; Visse, M. Experiences of leaders in the implementation of Lean in a teaching hospital—Barriers and facilitators in clinical practices: A qualitative study. BMJ Open 2013, 3, e003605. [Google Scholar] [CrossRef] [PubMed]
- Daly, A.; Wolfe, N.; Teeling, S.P.; Ward, M.; McNamara, M. Redesigning the process for scheduling elective Orthopedic Surgery: A combined Lean Six Sigma and Person-Centered Approach. Int. J. Environ. Res. Public Health 2021, 18, 11946. [Google Scholar] [CrossRef] [PubMed]
- Waring, J.J.; Bishop, S. Lean healthcare: Rhetoric, ritual and resistance. Soc. Sci. Med. 2010, 71, 1332–1340. [Google Scholar] [CrossRef] [PubMed]
- Oshry, B. Context, Context, Context: How Our Blindness to Context Cripples Even the Smartest Organisations; Triarchy Press: Dorset, UK, 2018. [Google Scholar]
- Laloux, F. Reinventing Organisations: A Guide to Creating Organisations Inspired by the Next Stage of Human Conviousness, 1st ed.; Nelson Publishing: Brussels, Belgium, 2014. [Google Scholar]
- Daly, A.; Teeling, S.P.; Garvey, S.; Ward, M.; McNamara, M. Using a combined lean and person-centred approach to support the resumption of routine hospital activity following the first wave of COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 2754. [Google Scholar] [CrossRef] [PubMed]
- Teeling, S.P.; Keown, A.M.; Cunningham, U.; Keegan, D. The application of a person-centred approach to process improvement in ophthalmology services in the North East of the Republic of Ireland. Int. Pract. Dev. J. 2023, 13, 6. [Google Scholar] [CrossRef]
- Teeling, S.P.; McGuirk, M.; McNamara, M.; McGroarty, M.; Igoe, A. The Utilization of Lean Six Sigma Methodologies in Enhancing Surgical Pathways and Surgical Rehabilitation. Appl. Sci. 2023, 13, 6920. [Google Scholar] [CrossRef]
- Müller, M.; Jürgens, J.; Raedaèlli, M.; Klingberg, K.; Haultz, W.E.; Stock, S. Impact of the communication and patient hand-off tool SBAR on patient safety: A systematic review. BMJ Open 2018, 8, e022202. [Google Scholar] [CrossRef]
| Improvement Tool | Description |
|---|---|
| Project Charter [22] | A project charter defines the problem statement and establishes baseline data for the project. It is used to identify goals and the scope of the project. |
| SMART goals [23] | SMART is used to manage the project goals to determine if they are Specific, Measurable, Achievable, Relevant, and Timebound (SMART). |
| SIPOC [24] | A high-level SIPOC (Supplier, Input, Process, Output, and Customer) highlights the process steps and defines the customers and stakeholders. |
| RACI [24] | RACI (Responsible, Accountable, Consulted, Informed) identifies which stakeholders are responsible and accountable and which need to be kept informed or consulted. |
| CTQ [25] | The CTQ (Critical to Quality) is designed to capture the key measurable characteristics of a process or service whose performance standards must be met to satisfy the service user. |
| VOC [26] | The Voice of Customer (VOC) tool engages with the customer to gather their feedback about their experiences with and expectations for your products or services. |
| Gemba [27] | Observation of the actual process taking place |
| Fishbone [28] | Identifies root causes, representing the effect and the factors or causes influencing it. |
| FMEA [28] | Failure Mode and Effect Analysis is a risk analysis tool that is used to prevent an event from happening. It highlights the aspects of a process that should be targeted for improvement. |
| Process Map [29] | Process mapping supports a better understanding of complex systems and the adaptation of improvement interventions in their local context. |
| TIMWOODS [30] | A useful tool wherein each letter stands for one of eight potential wastes: Transport, Inventory, Motion, Waiting time, Overprocessing, Overproduction, Defects, and Skills (TIMWOODS) |
| 5S [31] | A system to reduce waste and optimize productivity through maintaining an orderly workplace and using visual cues. A cyclical methodology of ‘Sort, Set in Order, Shine, Standardize, and Sustain the cycle. |
| PICK Chart [32] | Possible, Implement, Challenge, Killed (PICK) chart is a visual tool to prioritize the potential improvements to give the biggest reward. |
| Practicality Tool [30] | Ranks solutions in terms of the way out there, quite impractical, might be workable, close workable, and could be implemented today. |
| Control Plan [33] | What was measured, why, who is responsible, and what actions are required. |
| Waste | Impact | Identified | |
|---|---|---|---|
| T | Transport | Moving information |
|
| I | Inventory | Information unavailable |
|
| M | Motion | Excessive movement in workspace |
|
| W | Waiting time | Waiting for information or items to arrive |
|
| O | Over- processing | Doing more work than is necessary |
|
| O | Over- production | Doing work before it is needed |
|
| D | Defects | Mistakes or errors requiring re-work |
|
| S | Skills | Not using workers for their abilities |
|
| Pre-Intervention | Post-Intervention | |
|---|---|---|
| T | Excessive time taken to process referrals Excessive change between software to process referrals | Time taken was reduced by 52% Changes between software reduced from 17 to 7 |
| I | Referral details in are different formats and are difficult to locate Various methods of referral | Referrals from ED received via tracker only |
| M | Numerous touch points to process referrals Numerous touch points to triage referral | Touch points were reduced by 51% for patient service staff Touch points were reduced by 27% for consultants to triage referrals |
| W | Staff searching for correct patient details Staff searching for referral information Staff waiting for the triage outcome Patient waiting for an appointment | Overall waiting was reduced by 34% Reduced searching for documents as all are accessible via the tracker |
| O | Logging the same information repeatedly in different software Re-checking previous patients for updates Re-work contacting other teams due to an incomplete referral | Excel will not be used; the tracker is a live document. Only completed referrals will be forwarded to Orthopedics via the tracker |
| O | Duplicate entries on Meditech and Excel and review past fields | Tracker is a live document categorizing referral progress through ‘Awaiting consultant’, ‘Awaiting patient services’, ‘Complete’, etc. |
| D | No diagnostics are available No referral available—patient calling department Patient Services team did not email the referral Patients attending trauma orthopedic consultants unnecessarily | Transparent and up-to-date viewing of referrals possible for ED and orthopedics using tacker Consultant has the option to triage to physiotherapy if appropriate |
| S | Not utilizing new patient services staff for administrative tasks Not utilizing physiotherapy for assessment or triage Not utilizing trauma orthopedic consultants for appropriate patient caseload | More efficient triage process will release time for patient services staff to complete other duties Orthopedic and physiotherapy staff are assessing appropriate patients due to the triage structure |
| Consultant Caseload (n = 6) | Pre-Intervention Number | Post-Intervention Number | % Change (+/−) |
|---|---|---|---|
| Elective new appointment | 257 | 245 | −4.6 |
| Elective review appointment | 361 | 546 | +51 |
| Trauma new appointment | 85 | 97 | +14 |
| Total appointment number | 702 | 878 | +22 |
| Surgery Post-ED Referral | Pre-Intervention % | Post-Intervention % | % Change |
| Trauma surgery | 6.3 | 12 | +5.7 |
| Non-trauma surgery | 5.2 | 7.5 | +2.3 |
| Total surgery | 14 | 22 | +8 |
| Patient Survey | Pre-Intervention | Post-Intervention |
|---|---|---|
| What would be your expectations regarding the wait time between your ED visit and the consultant appointment? | 10.77 days (range 0–28 days) | 10.3 days (range 0–28 days) |
| What is your satisfaction level based on your experience with the current process? | 6.1/10 | 6.6/10 |
| Would you avail of an Allied Therapy appointment if advised by your triaging Orthopedic consultant? | 70% see Allied Health | 80% see Allied Health |
| Orthopedic patient services survey | Pre-intervention | Post-intervention |
| What percentage of your working week is spent registering ED patients? | 30% | 30% |
| Approximately how long does it take to register a trauma referral from the ED? | 10 min | 5 min |
| How satisfied are you with the current process? | 2 (Low) | 4 (High) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pierce, A.; Teeling, S.P.; McNamara, M.; O’Daly, B.; Daly, A. Using Lean Six Sigma in a Private Hospital Setting to Reduce Trauma Orthopedic Patient Waiting Times and Associated Administrative and Consultant Caseload. Healthcare 2023, 11, 2626. https://doi.org/10.3390/healthcare11192626
Pierce A, Teeling SP, McNamara M, O’Daly B, Daly A. Using Lean Six Sigma in a Private Hospital Setting to Reduce Trauma Orthopedic Patient Waiting Times and Associated Administrative and Consultant Caseload. Healthcare. 2023; 11(19):2626. https://doi.org/10.3390/healthcare11192626
Chicago/Turabian StylePierce, Anthony, Seán Paul Teeling, Martin McNamara, Brendan O’Daly, and Ailish Daly. 2023. "Using Lean Six Sigma in a Private Hospital Setting to Reduce Trauma Orthopedic Patient Waiting Times and Associated Administrative and Consultant Caseload" Healthcare 11, no. 19: 2626. https://doi.org/10.3390/healthcare11192626
APA StylePierce, A., Teeling, S. P., McNamara, M., O’Daly, B., & Daly, A. (2023). Using Lean Six Sigma in a Private Hospital Setting to Reduce Trauma Orthopedic Patient Waiting Times and Associated Administrative and Consultant Caseload. Healthcare, 11(19), 2626. https://doi.org/10.3390/healthcare11192626








