Virtual Reality-Based Exercise Therapy for Patients with Chronic Musculoskeletal Pain: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Identification of Purpose and Research Questions
2.2. Search Strategy
2.3. Eligibility Criteria for Study Selection
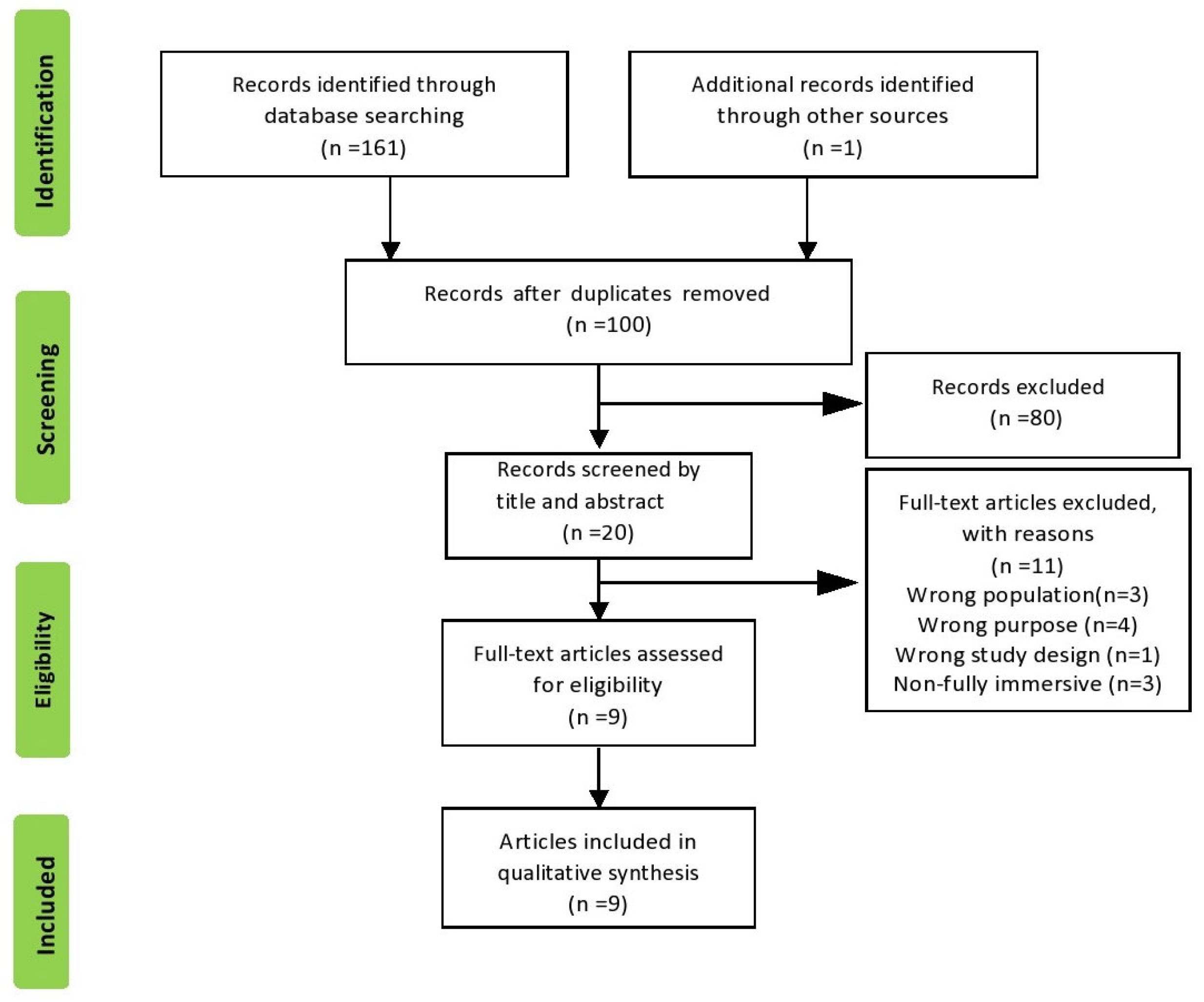
2.4. Screening
2.5. Data Extraction and Results Synthesis
2.6. Methodological Quality of RCTs
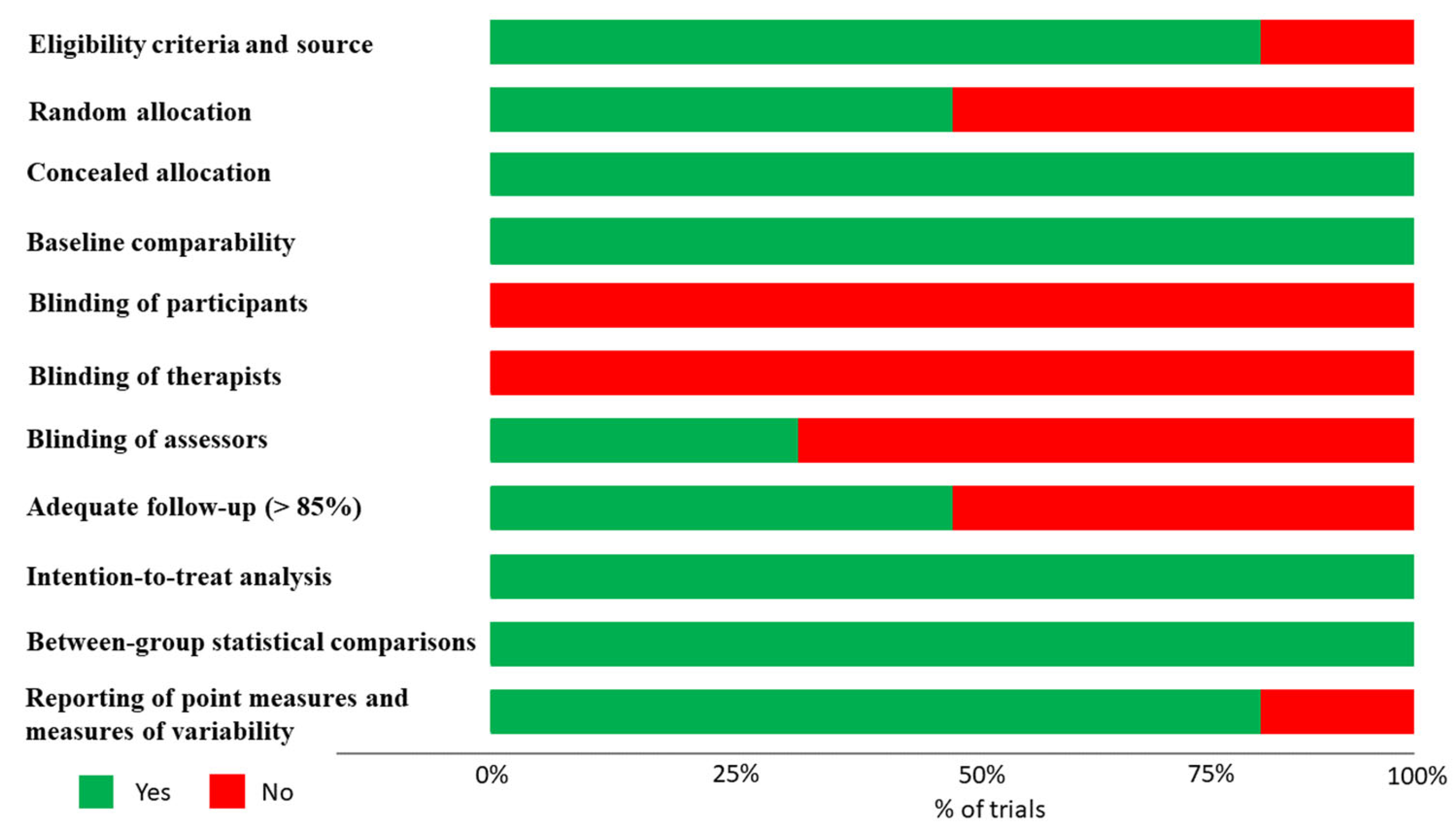
3. Results
3.1. Literature Search
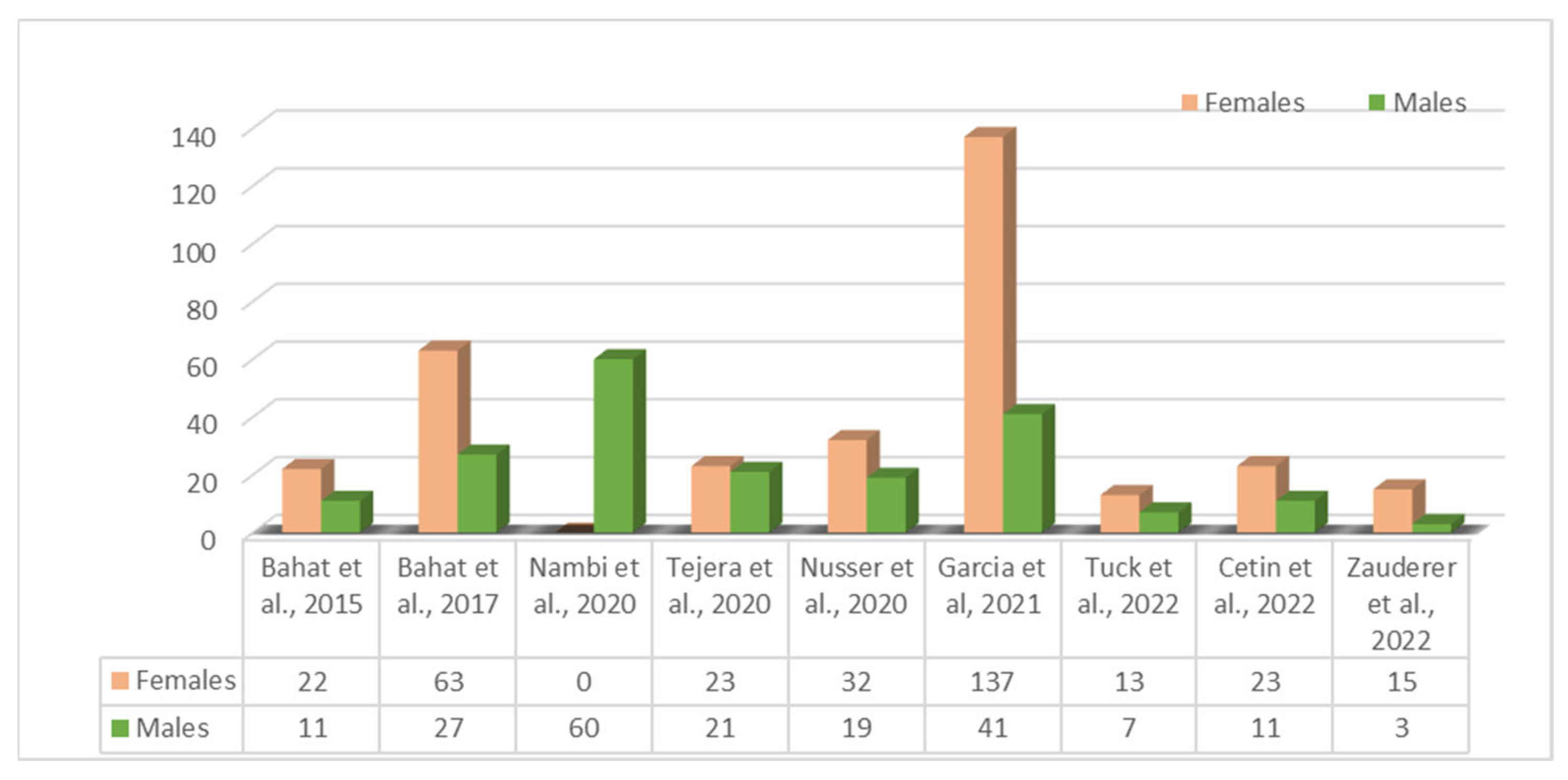
3.2. Study Characteristics
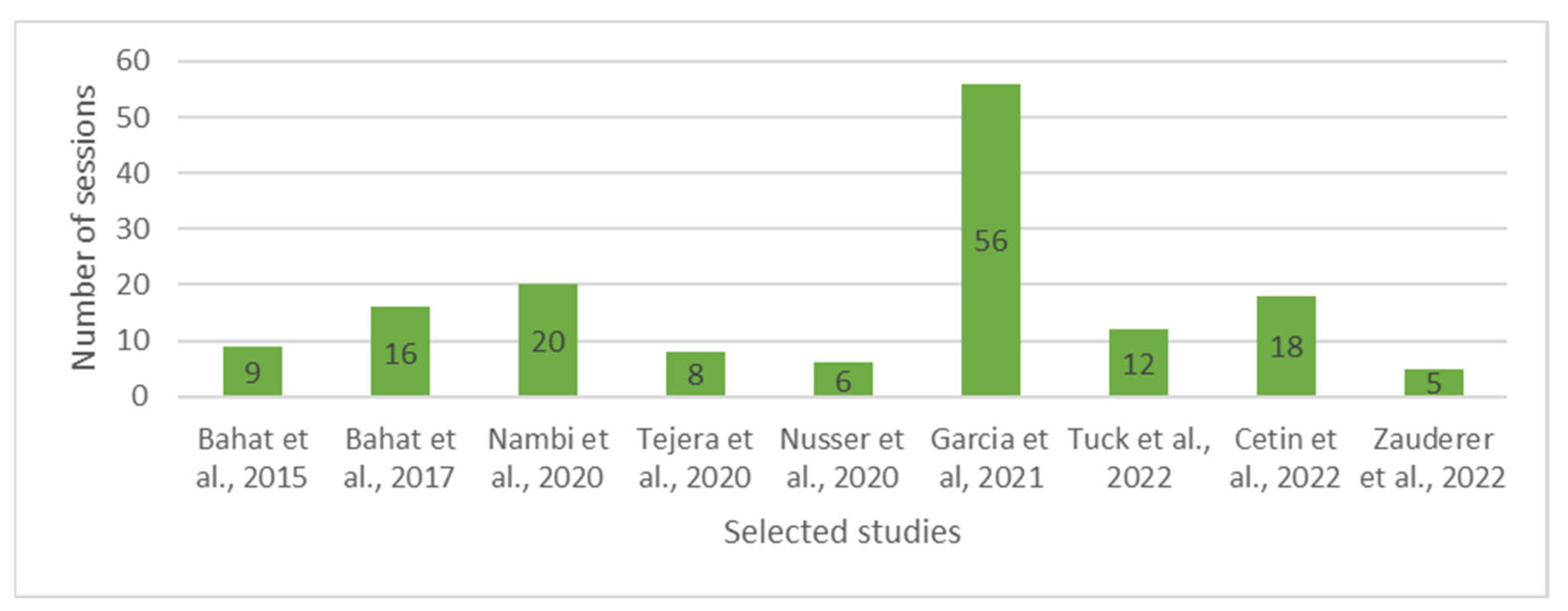
3.3. Virtual-Reality-Based Exercise Treatment
3.4. Outcomes Measures
3.5. Effectiveness of VRET
3.6. Pain Intensity
3.7. Disability
3.8. ROM
3.9. Kinesiophobia
3.10. Pain Catastrophizing
3.11. Pressure Pain Threshold
3.12. Temporal Summation and Conditioned Pain Modulation
3.13. Blood Serum Hormones
3.14. Satisfaction
3.15. Qualitative Analyses
3.16. Barriers
4. Discussion
4.1. Main Findings
4.2. Challenges in the Utilization of VRET
4.3. Future Directions
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fayaz, A.; Croft, P.; Langford, R.M.; Donaldson, L.J.; Jones, G.T. Prevalence of chronic pain in the UK: A systematic review and meta-analysis of population studies. BMJ Open 2016, 6, e010364. [Google Scholar] [CrossRef]
- Johannes, C.B.; Le, T.K.; Zhou, X.; Johnston, J.A.; Dworkin, R.H. The Prevalence of Chronic Pain in United States Adults: Results of an Internet-Based Survey. J. Pain 2010, 11, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Lentz, T.A.; Barabas, J.A.; Day, T.; Bishop, M.D.; George, S.Z. The Relationship of Pain Intensity, Physical Impairment, and Pain-Related Fear to Function in Patients With Shoulder Pathology. J. Orthop. Sports Phys. Ther. 2009, 39, 270–277. [Google Scholar] [CrossRef]
- Martinez-Calderon, J.; Flores-Cortes, M.; Clavero-Cano, S.; Morales-Asencio, J.M.; Jensen, M.P.; Rondon-Ramos, A.; Diaz-Cerrillo, J.L.; Ariza-Hurtado, G.R.; Luque-Suarez, A. The Role of Positive Psychological Factors in the Association between Pain Intensity and Pain Interference in Individuals with Chronic Musculoskeletal Pain: A Cross-Sectional Study. J. Clin. Med. 2020, 9, 3252. [Google Scholar] [CrossRef]
- Nijs, J.; D’Hondt, E.; Clarys, P.; Deliens, T.; Polli, A.; Malfliet, A.; Coppieters, I.; Willaert, W.; Tumkaya Yilmaz, S.; Elma, Ö.; et al. Lifestyle and Chronic Pain across the Lifespan: An Inconvenient Truth? PM R 2020, 12, 410–419. [Google Scholar] [CrossRef]
- Varela, A.J.; Van Asselt, K.W. The relationship between psychosocial factors and reported disability: The role of pain self-efficacy. BMC Musculoskelet. Disord. 2022, 23, 21. [Google Scholar] [CrossRef] [PubMed]
- Macías-Toronjo, I.; Rojas-Ocaña, M.J.; Sánchez-Ramos, J.L.; García-Navarro, E.B. Pain catastrophizing, kinesiophobia and fear-avoidance in non-specific work-related low-back pain as predictors of sickness absence. PLoS ONE 2020, 15, e0242994. [Google Scholar] [CrossRef]
- Smith, B.E.; Hendrick, P.; Bateman, M.; Holden, S.; Littlewood, C.; Smith, T.O.; Logan, P. Musculoskeletal pain and exercise—Challenging existing paradigms and introducing new. Br. J. Sports Med. 2019, 53, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Kosek, E.; Van Oosterwijck, J.; Meeus, M. Dysfunctional endogenous analgesia during exercise in patients with chronic pain: To exercise or not to exercise? Pain Physician 2012, 15 (Suppl. S3), ES205–ES213. [Google Scholar] [CrossRef] [PubMed]
- Lima, L.V.; Abner, T.S.S.; Sluka, K.A. Does exercise increase or decrease pain? Central mechanisms underlying these two phenomena. J. Physiol. 2017, 595, 4141–4150. [Google Scholar] [CrossRef]
- Da Silva Santos, R.; Galdino, G. Endogenous systems involved in exercise-induced analgesia. J. Physiol. Pharmacol. 2018, 69, 3–13. [Google Scholar]
- LA Wender, C. Immersive virtual reality to relieve exercise-induced pain caused by aerobic cycling. Pain Manag. 2022, 12, 665–674. [Google Scholar] [CrossRef]
- Gumaa, M.; Youssef, A.R. Is Virtual Reality Effective in Orthopedic Rehabilitation? A Systematic Review and Meta-Analysis. Phys. Ther. 2019, 99, 1304–1325. [Google Scholar] [CrossRef] [PubMed]
- Hyodo, K.; Kidokoro, T.; Yamaguchi, D.; Iida, M.; Watanabe, Y.; Ueno, A.; Noda, T.; Kawahara, K.; Nishida, S.; Kai, Y.; et al. Feasibility, Safety, Enjoyment, and System Usability of Web-Based Aerobic Dance Exercise Program in Older Adults: Single-Arm Pilot Study. JMIR Aging 2023, 6, e39898. [Google Scholar] [CrossRef]
- Kim, J.; Son, J.; Ko, N.; Yoon, B. Unsupervised Virtual Reality-Based Exercise Program Improves Hip Muscle Strength and Balance Control in Older Adults: A Pilot Study. Arch. Phys. Med. Rehabil. 2013, 94, 937–943. [Google Scholar] [CrossRef]
- Valenzuela, T.; Okubo, Y.; Woodbury, A.; Lord, S.R.; Delbaere, K. Adherence to Technology-Based Exercise Programs in Older Adults: A Systematic Review. J. Geriatr. Phys. Ther. 2018, 41, 49–61. [Google Scholar] [CrossRef]
- Trost, Z.; France, C.; Anam, M.; Shum, C. Virtual reality approaches to pain: Toward a state of the science. Pain 2021, 162, 325–331. [Google Scholar] [CrossRef]
- Wiederhold, B.K.; Gao, K.; Sulea, C.; Wiederhold, M.D. Virtual Reality as a Distraction Technique in Chronic Pain Patients. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Baker, N.A.S.; Polhemus, A.H.O.; Ospina, E.H.; Feller, H.O.; Zenni, M.M.; Deacon, M.M.; DeGrado, G.O.; Basnet, S.B.; Driscoll, M.M. The State of Science in the Use of Virtual Reality in the Treatment of Acute and Chronic Pain: A Systematic Scoping Review. Clin. J. Pain 2022, 38, 424–441. [Google Scholar] [CrossRef]
- Wong, K.P.; Tse, M.M.Y.; Qin, J. Effectiveness of Virtual Reality-Based Interventions for Managing Chronic Pain on Pain Reduction, Anxiety, Depression and Mood: A Systematic Review. Healthcare 2022, 10, 2047. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Treede, R.-D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef]
- Verhagen, A.P.; de Vet, H.C.; de Bie, R.A.; Kessels, A.G.; Boers, M.; Bouter, L.M.; Knipschild, P.G. The Delphi List: A Criteria List for Quality Assessment of Randomized Clinical Trials for Conducting Systematic Reviews Developed by Delphi Consensus. J. Clin. Epidemiol. 1998, 51, 1235–1241. [Google Scholar] [CrossRef] [PubMed]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) Scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef]
- Tuck, N.; Pollard, C.; Good, C.; Williams, C.; Lewis, G.; Hames, M.; Aamir, T.; Bean, D. Active Virtual Reality for Chronic Primary Pain: Mixed Methods Randomized Pilot Study. JMIR Form. Res. 2022, 6, e38366. [Google Scholar] [CrossRef]
- Zauderer, J.; Lefèvre-Colau, M.-M.; Davoine, É.; Hocquart, M.; Rannou, F.; Roby-Brami, A.; Nguyen, C.; Roren, A. Exercise therapy program using immersive virtual reality for people with non-specific chronic neck pain: A 3-month retrospective open pilot and feasibility study. Ann. Phys. Rehabil. Med. 2022, 65, 101527. [Google Scholar] [CrossRef]
- Garcia, L.M.; Birckhead, B.J.; Krishnamurthy, P.; Sackman, J.; Mackey, I.G.; Louis, R.G.; Salmasi, V.; Maddox, T.; Darnall, B.D. An 8-Week Self-Administered At-Home Behavioral Skills-Based Virtual Reality Program for Chronic Low Back Pain: Double-Blind, Randomized, Placebo-Controlled Trial Conducted During COVID-19. J. Med. Internet Res. 2021, 23, e26292. [Google Scholar] [CrossRef] [PubMed]
- Cetin, H.; Kose, N.; Oge, H.K. Virtual reality and motor control exercises to treat chronic neck pain: A randomized controlled trial. Musculoskelet. Sci. Pract. 2022, 62, 102636. [Google Scholar] [CrossRef]
- Bahat, H.S.; Takasaki, H.; Chen, X.; Bet-Or, Y.; Treleaven, J. Cervical kinematic training with and without interactive VR training for chronic neck pain—A randomized clinical trial. Man. Ther. 2015, 20, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Bahat, H.S.; Croft, K.; Carter, C.; Hoddinott, A.; Sprecher, E.; Treleaven, J. Remote kinematic training for patients with chronic neck pain: A randomised controlled trial. Eur. Spine J. 2018, 27, 1309–1323. [Google Scholar] [CrossRef]
- Tejera, D.M.; Beltran-Alacreu, H.; Cano-De-La-Cuerda, R.; Hernández, J.V.L.; Martín-Pintado-Zugasti, A.; Calvo-Lobo, C.; Gil-Martínez, A.; Fernández-Carnero, J. Effects of Virtual Reality versus Exercise on Pain, Functional, Somatosensory and Psychosocial Outcomes in Patients with Non-specific Chronic Neck Pain: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 5950. [Google Scholar] [CrossRef] [PubMed]
- Nambi, G.; Abdelbasset, W.K.; Alrawaili, S.M.; Alsubaie, S.F.; Abodonya, A.M.; Saleh, A.K. Virtual reality or isokinetic training; its effect on pain, kinesiophobia and serum stress hormones in chronic low back pain: A randomized controlled trial. Technol. Health Care 2021, 29, 155–166. [Google Scholar] [CrossRef]
- Nusser, M.; Knapp, S.; Kramer, M.; Krischak, G. Effects of virtual reality-based neck-specific sensorimotor training in patients with chronic neck pain: A randomized controlled pilot trial. J. Rehabil. Med. 2021, 53, jrm00151. [Google Scholar] [CrossRef]
- Birckhead, B.; Khalil, C.; Liu, X.; Conovitz, S.; Rizzo, A.; Danovitch, I.; Bullock, K.; Spiegel, B. Recommendations for Methodology of Virtual Reality Clinical Trials in Health Care by an International Working Group: Iterative Study. JMIR Ment. Health 2019, 6, e11973. [Google Scholar] [CrossRef] [PubMed]
- Grassini, S. Virtual Reality Assisted Non-Pharmacological Treatments in Chronic Pain Management: A Systematic Review and Quantitative Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4071. [Google Scholar] [CrossRef] [PubMed]
- Tao, G.; Garrett, B.; Taverner, T.; Cordingley, E.; Sun, C. Immersive virtual reality health games: A narra-tive review of game design. J. Neuroeng. Rehabil. 2021, 18, 31. [Google Scholar] [CrossRef]
- Garrett, B.; Taverner, T.; Gromala, D.; Tao, G.; Cordingley, E.; Sun, C. Virtual Reality Clinical Research: Promises and Challenges. JMIR Serious Games 2018, 6, e10839. [Google Scholar] [CrossRef]
- Thomas, J.S.; France, C.R.; Applegate, M.E.; Leitkam, S.T.; Walkowski, S. Feasibility and Safety of a Virtual Reality Dodgeball Intervention for Chronic Low Back Pain: A Randomized Clinical Trial. J. Pain 2016, 17, 1302–1317. [Google Scholar] [CrossRef]
- LaViola, J.J. A discussion of cybersickness in virtual environments. ACM SIGCHI Bull. 2000, 32, 47–56. [Google Scholar] [CrossRef]
- Caserman, P.; Garcia-Agundez, A.; Zerban, A.G.; Göbel, S. Cybersickness in current-generation virtual reality head-mounted displays: Systematic review and outlook. Virtual Real. 2021, 25, 1153–1170. [Google Scholar] [CrossRef]
| Q1: | What is the current state of research on the use of VR equipment (e.g., headsets, haptic devices) combined with specific types of therapeutic exercise (e.g., aerobic, anaerobic, motor control exercises) for patients with CMP? |
| Q2: | What specific parameters of exercise (e.g., frequency, intensity, type, time) are utilized? |
| Q3: | Do the VR interventions incorporate any motivational or target-setting materials? Do they include any cognitive tasks (dual tasks, memory tasks, divided attention activities)? |
| Q4: | What are the outcomes that have been measured in studies using VRET for patients with CPM? Which pathologies were treated? |
| Q5: | What are the benefits and limitations of using VR technology combined with specific types of therapeutic exercise for patients with CMP, and are there any reported adverse effects? |
| Q6: | What gaps in the literature exist regarding the use of VR technology combined with specific types of therapeutic exercise for patients with CMP, and how could future research address these gaps? |
| Study | Reported Barriers |
|---|---|
| Bahat et al., 2015 [29] | 4/32 participants experienced motion sickness with the use of the VR device during the assessment. |
| Bahat et al., 2017 [30] | Out of 14 dropouts at post-intervention assessment, 5 were due to VR-associated sickness and headache. |
| Nusser et al., 2020 [33] | Complaints about the weight of the helmet and the treatment planning. |
| Garcia et al., 2021 [27] | 7/72 (9.7%) from the VR group reported experiencing nausea and motion sickness during the treatment phase of the study. |
| Zauderer et al., 2022 [26] | Concerns for both participants and physiotherapists were the weight of the headset, the discomfort of wearing corrective glasses inside the VR headset, and difficulty scoring the pain intensity when wearing the VR device. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bilika, P.; Karampatsou, N.; Stavrakakis, G.; Paliouras, A.; Theodorakis, Y.; Strimpakos, N.; Kapreli, E. Virtual Reality-Based Exercise Therapy for Patients with Chronic Musculoskeletal Pain: A Scoping Review. Healthcare 2023, 11, 2412. https://doi.org/10.3390/healthcare11172412
Bilika P, Karampatsou N, Stavrakakis G, Paliouras A, Theodorakis Y, Strimpakos N, Kapreli E. Virtual Reality-Based Exercise Therapy for Patients with Chronic Musculoskeletal Pain: A Scoping Review. Healthcare. 2023; 11(17):2412. https://doi.org/10.3390/healthcare11172412
Chicago/Turabian StyleBilika, Paraskevi, Natalia Karampatsou, Giorgos Stavrakakis, Achilleas Paliouras, Yannis Theodorakis, Nikolaos Strimpakos, and Eleni Kapreli. 2023. "Virtual Reality-Based Exercise Therapy for Patients with Chronic Musculoskeletal Pain: A Scoping Review" Healthcare 11, no. 17: 2412. https://doi.org/10.3390/healthcare11172412
APA StyleBilika, P., Karampatsou, N., Stavrakakis, G., Paliouras, A., Theodorakis, Y., Strimpakos, N., & Kapreli, E. (2023). Virtual Reality-Based Exercise Therapy for Patients with Chronic Musculoskeletal Pain: A Scoping Review. Healthcare, 11(17), 2412. https://doi.org/10.3390/healthcare11172412