The Impact of Systemic Sclerosis on Sexual Health: An Italian Survey
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Study Procedures
2.4. Statistical Analysis
3. Results
3.1. General Characteristics
3.2. Vulvovaginal Atrophy (VVA) Symptoms
3.3. Sexual Function
3.4. Relationship with the Partner
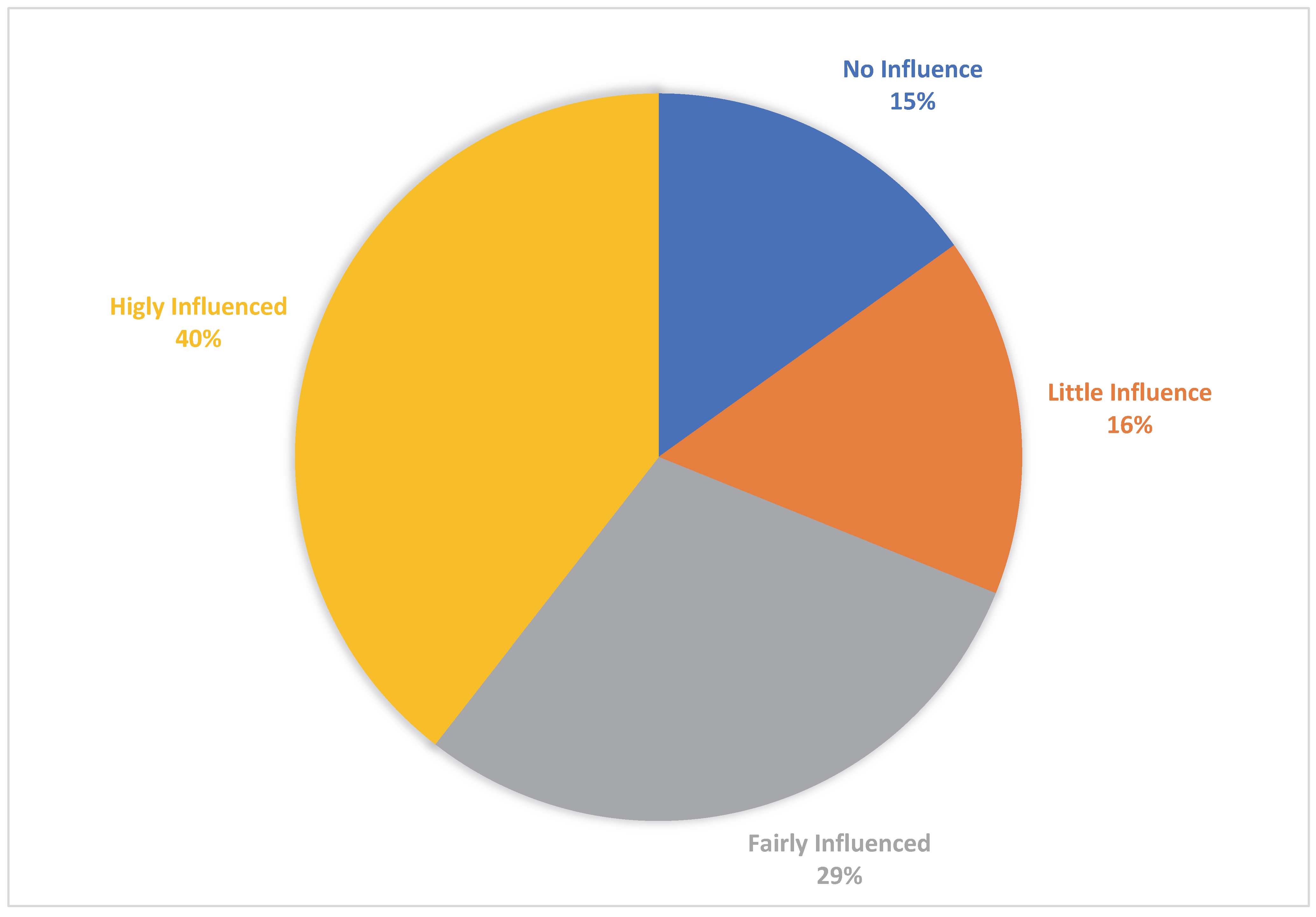
3.5. Relationship with the Physician
3.6. Women’s Considerations of Therapies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Denton, C.P.; Khanna, D. Systemic sclerosis. Lancet 2017, 390, 1685–1699. [Google Scholar] [CrossRef] [PubMed]
- Sampaio-Barros, P.D.; Samara, A.M.; Neto, J.F.M. Gynaecologic history in systemic sclerosis. Clin. Rheumatol. 2000, 19, 184–187. [Google Scholar] [CrossRef]
- Saad, S.C.; Pietrzykowski, J.E.; Lewis, S.S.; Stepien, A.M.; Latham, V.A.; Messick, S.; Ensz, S.L.; Wetherell, C.; Behrendt, A.E. Vaginal Lubrication in Women with Scleroderma and Sjogren’s Syndrome. Sex. Disabil. 1999, 17, 103–113. [Google Scholar] [CrossRef]
- Schover, L.R.; Jensen, S.R. Sexuality and Chronic Illness: A Comprehensive Approach; Guilford: New York, NY, USA, 1988. [Google Scholar]
- Trilpell, L.M.; Nietern, P.J.; Brown, A.N. (Eds.) Prevalence of female sexual dysfunction among women with systemic sclerosis. In Proceedings of the 9th International Workshop on Scleroderma Research, Boston, MA, USA, 5–9 August 2006. [Google Scholar]
- Bhadauria, S.; Moser, D.K.; Clements, P.J.; Singh, R.R.; Lachenbruch, P.A.; Pitkin, R.M.; Weiner, S.R. Genital tract abnormalities and female sexual function impairment in systemic sclerosis. Am. J. Obstet. Gynecol. 1995, 172, 580–587. [Google Scholar] [CrossRef]
- Schouffoer, A.A.; van der Marel, J.; Ter Kuile, M.M.; Weijenborg, P.T.M.; Voskuyl, A.; Vlieland, C.W.V.; van Laar, J.M.; Vlieland, T.P.M.V. Impaired sexual function in women with systemic sclerosis: A cross-sectional study. Arthritis Rheum. 2009, 61, 1601–1608. [Google Scholar] [CrossRef] [PubMed]
- Knafo, R.; Thombs, B.D.; Jewett, L.; Hudson, M.; Wigley, F.; Haythornthwaite, J.A. (Not) talking about sex: A systematic comparison of sexual impairment in women with systemic sclerosis and other chronic disease samples. Rheumatology 2009, 48, 1300–1303. [Google Scholar] [CrossRef]
- Levis, B.; Hudson, M.; Knafo, R.; Baron, M.; Nielson, W.R.; Hill, M.; Thombs, B.D.; Canadian Scleroderma Research Group (CSRG). Rates and correlates of sexual activity and impairment among women with systemic sclerosis. Arthritis Care Res. 2011, 64, 340–350. [Google Scholar] [CrossRef]
- Tristano, A.G. The impact of rheumatic diseases on sexual function. Rheumatol. Int. 2009, 29, 853–860. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Preliminary criteria for the classification of systemic sclerosis (scleroderma). Arthritis Rheum. 1980, 23, 581–590. [Google Scholar] [CrossRef]
- Meston, M.; Freihart, B.; Handy, A.; Kilimnik, C.; Rosen, R. Scoring and Interpretation of the FSFI: What can be Learned From 20 Years of use? J. Sex. Med. 2020, 17, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Filocamo, M.T.; Serati, M.; Marzi, V.L.; Costantini, E.; Milanesi, M.; Pietropaolo, A.; Polledro, P.; Gentile, B.; Maruccia, S.; Fornia, S.; et al. The Female Sexual Function Index (FSFI): Linguistic Validation of the Italian Version. J. Sex. Med. 2014, 11, 447–453. [Google Scholar] [CrossRef]
- Prady, J.; Vale, A.; Hill, J. Body image and sexuality. In Rheumatology Nursing: A Creative Approach; Hill, J., Ed.; Churchill Livingstone: Edinburgh, Scotland, 1998; pp. 109–124. [Google Scholar]
- Wells, D. Caring for Sexuality in Health and Illness; Churchill Livingstone: Edinburgh, Scotland, 2000. [Google Scholar]
- Impens, A.J.; Seibold, J.R. Vascular Alterations and Sexual Function in Systemic Sclerosis. Int. J. Rheumatol. 2010, 2010, 139020. [Google Scholar] [CrossRef]
- Knafo, R.; Haythornthwaite, J.A.; Heinberg, L.; Wigley, F.M.; Thombs, B.D. The association of body image dissatisfaction and pain with reduced sexual function in women with systemic sclerosis. Rheumatology 2011, 50, 1125–1130. [Google Scholar] [CrossRef] [PubMed]
- Impens, A.J.; Rothman, J.; Schiopu, E.; Cole, J.C.; Dang, J.; Gendrano, N.; Rosen, R.C.; Seibold, J.R. Sexual activity and functioning in female scleroderma patients. Clin. Exp. Rheumatol. 2009, 27, 38–43. [Google Scholar] [PubMed]
- Jewett, L.R.; Hudson, M.; Haythornthwaite, J.A.; Heinberg, L.; Wigley, F.M.; Baron, M.; Thombs, B.D. Development and validation of the brief-satisfaction with appearance scale for systemic sclerosis. Arthritis Care Res. 2010, 62, 1779–1786. [Google Scholar] [CrossRef]
- Bongi, S.M.; Del Rosso, A.; Mikhaylova, S.; Baccini, M.; Cerinic, M.M. Sexual Function in Italian Women with Systemic Sclerosis Is Affected by Disease-related and Psychological Concerns. J. Rheumatol. 2013, 40, 1697–1705. [Google Scholar] [CrossRef]
- Frikha, F.; Masmoudi, J.; Saidi, N.; Bahloul, Z. Sexual dysfunction in married women with systemic sclerosis. Pan Afr. Med, J. 2014, 17, 82. [Google Scholar] [CrossRef]
- Parish, S.J.; Nappi, R.; Krychman, M.L.; Spadt, K.; Simon, J.; Goldstein, J.; Kingsberg, S. Impact of vulvovaginal health on postmenopausal women: A review of surveys on symptoms of vulvovaginal atrophy. Int. J. Women’s Health 2013, 5, 437–447. [Google Scholar] [CrossRef]
- Sanchez, K.; Denys, P.; Giuliano, F.; Palazzo, C.; Bérezné, A.; Abid, H.; Rannou, F.; Poiraudeau, S.; Mouthon, L. Systemic sclerosis: Sexual dysfunction and lower urinary tract symptoms in 73 patients. Presse Med. 2016, 45, e79–e89. [Google Scholar] [CrossRef]
- Knafo, R.; Jewett, L.R.; Ba, M.B.; Thombs, B.D. Sexual function in women with systemic sclerosis: Comment on the article by Schouffoer et al. Arthritis Care Res. 2010, 62, 1200–1202. [Google Scholar] [CrossRef] [PubMed]
- North American Menopause Society. Management of symptomatic vulvovaginal atrophy: 2013 position statement of the North American Menopause Society. Menopause 2013, 20, 888–902. [Google Scholar] [CrossRef] [PubMed]
- Salvatore, S.; Benini, V.; Ruffolo, A.F.; Degliuomini, R.S.; Redaelli, A.; Casiraghi, A.; Candiani, M. Current challenges in the pharmacological management of genitourinary syndrome of menopause. Expert Opin. Pharmacother. 2023, 24, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Portman, D.J.; Bachmann, G.A.; Simon, J.A. Ospemifene, a novel selective estrogen receptor modulator for treating dyspareunia associated with postmenopausal vulvar and vaginal atrophy. Menopause 2013, 20, 623–630. [Google Scholar] [CrossRef]
- Filippini, M.; Porcari, I.; Ruffolo, A.F.; Casiraghi, A.; Farinelli, M.; Uccella, S.; Franchi, M.; Candiani, M.; Salvatore, S. CO2-Laser therapy and Genitourinary Syndrome of Menopause: A Systematic Review and Meta-Analysis. J. Sex. Med. 2022, 19, 452–470. [Google Scholar] [CrossRef]
- Benini, V.; Ruffolo, A.F.; Casiraghi, A.; Degliuomini, R.S.; Frigerio, M.; Braga, A.; Serati, M.; Torella, M.; Candiani, M.; Salvatore, S. New Innovations for the Treatment of Vulvovaginal Atrophy: An Up-to-Date Review. Medicina 2022, 58, 770. [Google Scholar] [CrossRef]
- Ingegnoli, F.; Ughi, N.; Mihai, C. Update on the epidemiology, risk factors, and disease outcomes of systemic sclerosis. Best Pract Res Clin Rheumatol. 2018, 32, 223–240. [Google Scholar] [CrossRef]

| N = 107 | |
|---|---|
| Age, mean (±SD), years | 53.47 (±13.27) |
| Systemic sclerosis duration, mean (±SD), years | 12.48 (±10.28) |
| Menopausal status, n (%) | 58 (54.2) |
| Hysterectomy, n (%) | 13 (12.1) |
| Bilateral salpingo-oophorectomy, n (%) | 10 (9.3) |
| Malignant neoplasia, n (%) | 3 (2.8) |
| Sexually active women, n (%) | 97 (90.7) |
| Age of sexually active women, mean (±SD), years | 53.28 (±13.70) |
| Systemic sclerosis duration of sexually active women, mean (±SD), years | 12.76 (±10.34) |
| N = 107 | |
|---|---|
| Vaginal dryness, n (%) | 89 (83.2) |
| Vaginal dryness severity §, mean (±SD) | 7.38 (±1.82) |
| Dyspareunia, n (%) | 88 (82.2) |
| Dyspareunia severity *, mean (±SD) | 7.72 (±1.44) |
| N = 97 | |
|---|---|
| Sexual dysfunction, n (%) | 87 (89.7) |
| Desire, mean (±SD) | 2.23 (±1.00) |
| Arousal, mean (±SD) | 2.66 (±1.74) |
| Lubrification, mean (±SD) | 2.56 (±1.91) |
| Orgasm, mean (±SD) | 2.69 (±2.04) |
| Satisfaction, mean (±SD) | 2.93 (±1.84) |
| Pain, mean (±SD) | 2.57 (±2.05) |
| Total, mean (±SD) | 15.66 (±9.36) |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| HR (95%CI) | p-Value | HR (95%CI) | p-Value | |
| Vulvovaginal Atrophy Symptoms | ||||
| Age, years | 1.05 (1.01–1.13) | 0.01 | 1.04 (0.98–1.11) | 0.17 |
| Systemic sclerosis duration, years | 1.06 (0.99–1.13) | 0.09 | ||
| Menopause | 3.43 (1.11–10.58) | 0.03 | 1.44 (0.27–7.61) | 0.66 |
| Sexual Dysfunction * | ||||
| HR (95%CI) | p-Value | HR (95%CI) | p-Value | |
| Age, years | 1.08 (1.02–1.15) | 0.002 | 1.08 (1.00–1.18) | 0.04 |
| Systemic sclerosis duration, years | 1.01 (0.95–1.02) | 0.61 | ||
| Menopause | 5.16 (1.03–25.71) | 0.02 | 0.90 (0.08–9.38) | 0.93 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruffolo, A.F.; Serati, M.; Casiraghi, A.; Benini, V.; Scancarello, C.; Di Dedda, M.C.; Garbagnati, C.; Braga, A.; Candiani, M.; Salvatore, S. The Impact of Systemic Sclerosis on Sexual Health: An Italian Survey. Healthcare 2023, 11, 2346. https://doi.org/10.3390/healthcare11162346
Ruffolo AF, Serati M, Casiraghi A, Benini V, Scancarello C, Di Dedda MC, Garbagnati C, Braga A, Candiani M, Salvatore S. The Impact of Systemic Sclerosis on Sexual Health: An Italian Survey. Healthcare. 2023; 11(16):2346. https://doi.org/10.3390/healthcare11162346
Chicago/Turabian StyleRuffolo, Alessandro Ferdinando, Maurizio Serati, Arianna Casiraghi, Vittoria Benini, Chiara Scancarello, Maria Carmela Di Dedda, Carla Garbagnati, Andrea Braga, Massimo Candiani, and Stefano Salvatore. 2023. "The Impact of Systemic Sclerosis on Sexual Health: An Italian Survey" Healthcare 11, no. 16: 2346. https://doi.org/10.3390/healthcare11162346
APA StyleRuffolo, A. F., Serati, M., Casiraghi, A., Benini, V., Scancarello, C., Di Dedda, M. C., Garbagnati, C., Braga, A., Candiani, M., & Salvatore, S. (2023). The Impact of Systemic Sclerosis on Sexual Health: An Italian Survey. Healthcare, 11(16), 2346. https://doi.org/10.3390/healthcare11162346







