Drivers of Patients’ Behavioral Intention toward Public and Private Clinics’ Services
Abstract
:1. Introduction
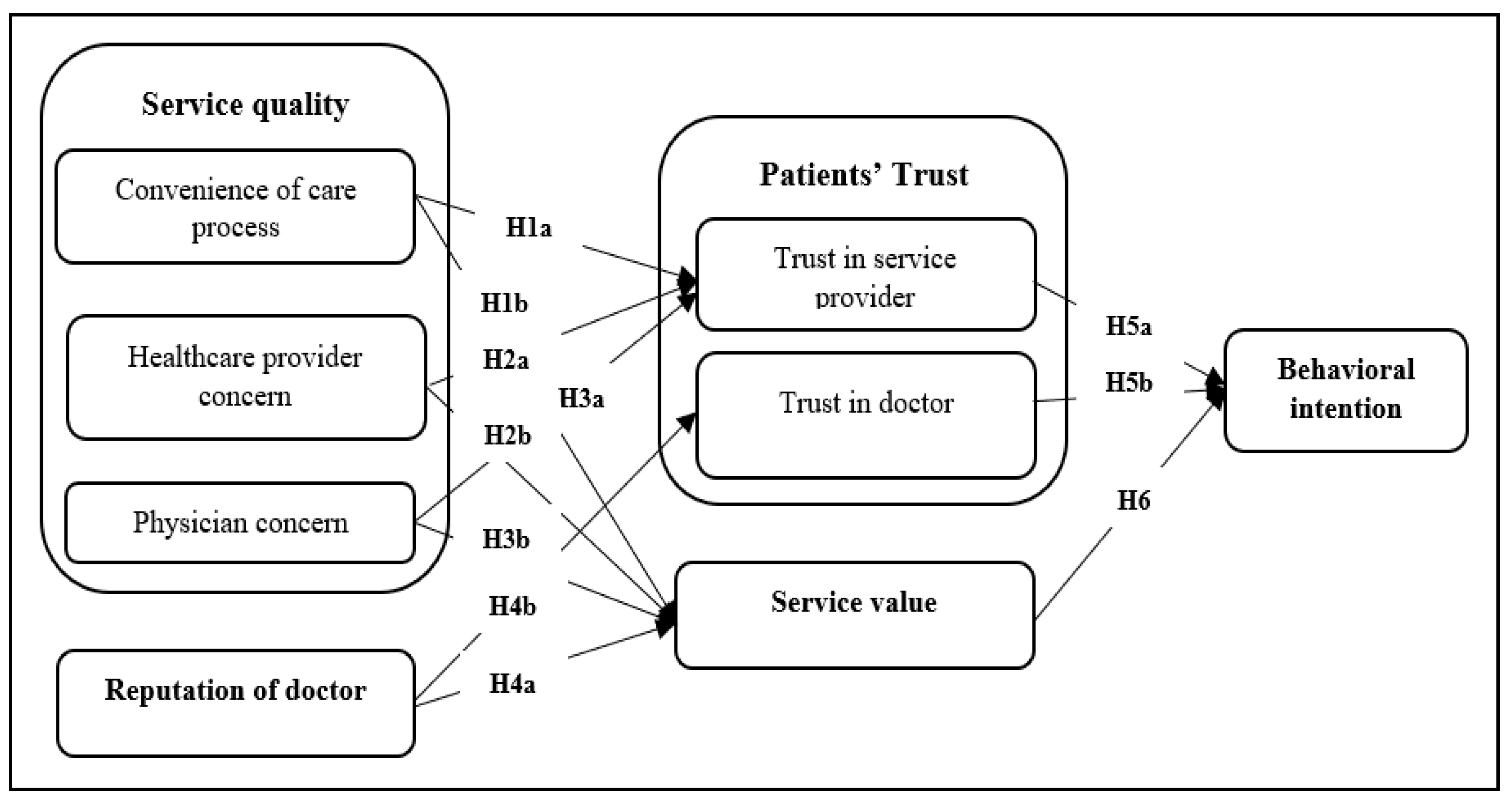
2. Conceptual Framework and Research Hypotheses
2.1. Behavioral Intention toward Healthcare Service Providers, Patients’ Trust, and Service Value
2.2. Service Quality: Drivers of Service Value and Trust
2.3. The Convenience of the Healthcare Process
2.4. Healthcare Provider Concern
2.5. Physician Concern
2.6. Reputation of Doctors
2.7. Drivers of Patients’ Behavioral Intention: Patients’ Trust and Service Value
2.7.1. Patients’ Trust
2.7.2. Service Value
3. Methods and Materials
3.1. Data Collection and Sample
3.2. Measurement Scales
4. Results
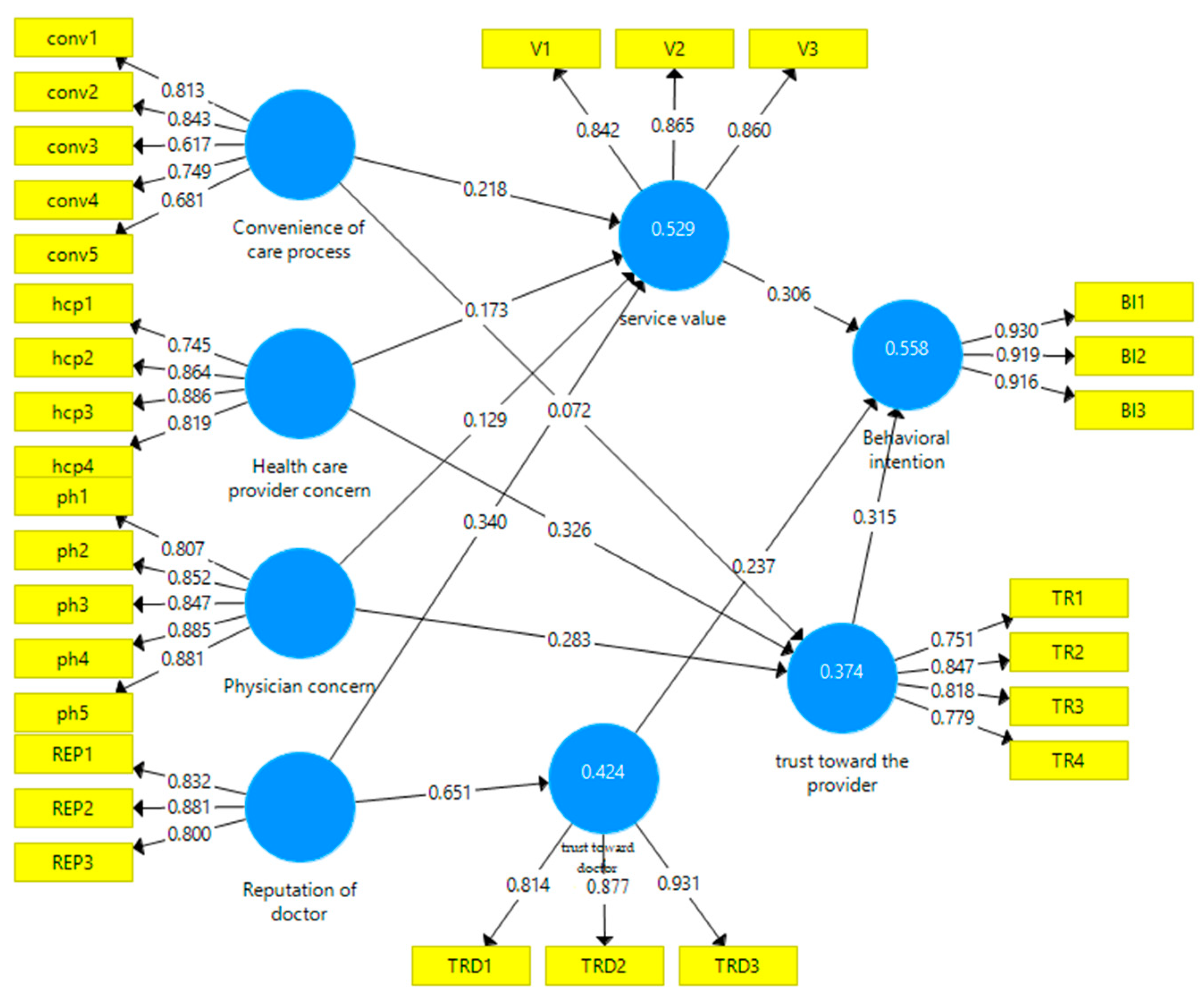
4.1. Measurement Model
4.2. Structural Model’s Predictive Relevance
4.2.1. The Productiveness of the Model
4.2.2. Hypotheses’ Verification
5. Discussion
5.1. Hypotheses Discussion
5.2. Implications, Limitations, and Future Research Pathways
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Construct | Items | Source | |
|---|---|---|---|
| The convenience of the care process | 1 | The procedure to get the lab test was convenient | Choi et al. [4] |
| 2 | The lab test was done in a prompt way. | ||
| 3 | The payment procedure was quick and simple. | ||
| 4 | The process for setting up the appointment was simple and easy. | ||
| 5 | I did not have to wait long for the medical examination from the physician. | ||
| Healthcare providers’ concern | 1 | The nurses were friendly | Choi et al. [4] |
| 2 | The care providers explained the medication process well. | ||
| 3 | Care providers truly cared for me | ||
| 4 | There was good coordination among the care providers | ||
| Physician’s concern | 1 | The physician was polite | Choi et al. [4] |
| 2 | The physician adequately explained my condition, examination results, and the treatment process | ||
| 3 | The physician allowed me to ask many questions enough to clarify everything | ||
| 4 | The physician paid enough consideration to my concerns in deciding on a medical procedure | ||
| 5 | The physician made me feel comfortable | ||
| Reputation of the doctor | 1 | My doctor always fulfills his commitments | Torres et al. [65] |
| 2 | My doctor has a good reputation | ||
| 3 | My doctor’s reputation is better than the reputation of other Doctors | ||
| Service value | 1 | Compared with the time and money that has been given the service was valuable | Zeithaml [50] |
| 2 | At a price has been paid, the service was acceptable (excellent compared to the price) | ||
| 3 | It was worth taking this healthcare service rather than others | ||
| Behavioral intention | 1 | I will recommend that other people use this hospital | Choi et al. [4] |
| 2 | If I needed medical services in the future, I would consider this hospital as my first | ||
| 3 | I will tell other people good things about this hospital | ||
| Service provider’s trust | 1 | I often hear positive news about the hospital in the media (on TV, the internet, and in magazines) | Zheng et al. [68] |
| 2 | I hear the hospital is recognized by official authority and/or the National Institutes of Health | ||
| 3 | I hear the hospital gains accreditation recognized by government official authority | ||
| 4 | I trust my doctor’s decisions about which treatments are best for me | ||
| Trust in Doctors | 1 | My doctor only thinks about what is best for me | Zheng et al. [68] |
| 2 | I have no worries about putting my life in my doctor’s hands | ||
| 3 | All in all, I have complete trust in my doctor |
| Behavioral Intention | Convenience of the Care Process | Healthcare Provider Concern | Physician Concern | Reputation of Doctor | Service Value | Trust toward Doctor | Trust toward the Provider | |
|---|---|---|---|---|---|---|---|---|
| BI1 | 0.930 | 0.539 | 0.517 | 0.587 | 0.610 | 0.612 | 0.614 | 0.602 |
| BI2 | 0.919 | 0.573 | 0.522 | 0.519 | 0.590 | 0.596 | 0.615 | 0.590 |
| BI3 | 0.916 | 0.572 | 0.538 | 0.565 | 0.550 | 0.566 | 0.608 | 0.602 |
| REP1 | 0.537 | 0.471 | 0.610 | 0.692 | 0.832 | 0.593 | 0.584 | 0.486 |
| REP2 | 0.568 | 0.435 | 0.508 | 0.608 | 0.881 | 0.509 | 0.582 | 0.525 |
| REP3 | 0.484 | 0.360 | 0.384 | 0.457 | 0.800 | 0.517 | 0.460 | 0.475 |
| TR1 | 0.539 | 0.343 | 0.365 | 0.319 | 0.404 | 0.375 | 0.476 | 0.751 |
| TR2 | 0.462 | 0.323 | 0.458 | 0.395 | 0.465 | 0.393 | 0.502 | 0.847 |
| TR3 | 0.452 | 0.292 | 0.358 | 0.372 | 0.387 | 0.402 | 0.477 | 0.818 |
| TR4 | 0.587 | 0.441 | 0.584 | 0.602 | 0.584 | 0.551 | 0.705 | 0.779 |
| TRD1 | 0.514 | 0.388 | 0.498 | 0.552 | 0.535 | 0.491 | 0.814 | 0.592 |
| TRD2 | 0.586 | 0.514 | 0.581 | 0.568 | 0.535 | 0.631 | 0.877 | 0.591 |
| TRD3 | 0.638 | 0.485 | 0.586 | 0.589 | 0.633 | 0.659 | 0.931 | 0.641 |
| V1 | 0.474 | 0.465 | 0.499 | 0.454 | 0.504 | 0.842 | 0.523 | 0.455 |
| V2 | 0.488 | 0.491 | 0.518 | 0.440 | 0.503 | 0.865 | 0.596 | 0.453 |
| V3 | 0.657 | 0.521 | 0.549 | 0.639 | 0.631 | 0.860 | 0.621 | 0.503 |
| conv1 | 0.532 | 0.813 | 0.577 | 0.500 | 0.439 | 0.506 | 0.510 | 0.447 |
| conv2 | 0.553 | 0.843 | 0.570 | 0.470 | 0.413 | 0.495 | 0.443 | 0.393 |
| conv3 | 0.330 | 0.617 | 0.343 | 0.341 | 0.337 | 0.315 | 0.256 | 0.230 |
| conv4 | 0.405 | 0.749 | 0.440 | 0.390 | 0.367 | 0.386 | 0.337 | 0.265 |
| conv5 | 0.399 | 0.681 | 0.519 | 0.354 | 0.321 | 0.410 | 0.370 | 0.281 |
| hcp1 | 0.495 | 0.571 | 0.745 | 0.601 | 0.462 | 0.510 | 0.466 | 0.447 |
| hcp2 | 0.495 | 0.498 | 0.864 | 0.598 | 0.541 | 0.494 | 0.542 | 0.484 |
| hcp3 | 0.494 | 0.566 | 0.886 | 0.617 | 0.556 | 0.536 | 0.609 | 0.540 |
| hcp4 | 0.404 | 0.593 | 0.819 | 0.455 | 0.440 | 0.492 | 0.481 | 0.409 |
| ph1 | 0.516 | 0.437 | 0.514 | 0.807 | 0.568 | 0.479 | 0.538 | 0.416 |
| ph2 | 0.556 | 0.529 | 0.671 | 0.852 | 0.638 | 0.530 | 0.625 | 0.479 |
| ph3 | 0.481 | 0.431 | 0.552 | 0.847 | 0.578 | 0.504 | 0.476 | 0.444 |
| ph4 | 0.502 | 0.488 | 0.566 | 0.885 | 0.621 | 0.531 | 0.524 | 0.506 |
| ph5 | 0.529 | 0.501 | 0.628 | 0.881 | 0.612 | 0.558 | 0.614 | 0.492 |
References
- Rivers, P.A.; Glover, S.H. Health care competition, strategic mission, and patient satisfaction: Research model and propositions. J. Health Organ. Manag. 2008, 22, 627–641. [Google Scholar] [CrossRef]
- Murhadi, W.R.; Karsana, W. Effect of service quality and patient satisfaction on behavioral intention. J. Entrep. Bus. 2021, 2, 25–36. [Google Scholar] [CrossRef]
- Rajic, T.; Rakic, A.; Milosevic, I. Modeling health care customer satisfaction: Evidence from Serbia. Serbian J. Manag. 2021, 16, 125–145. [Google Scholar] [CrossRef]
- Choi, K.S.; Cho, W.H.; Lee, S.H.; Lee, H.; Kim, C. The relationships among quality, value, satisfaction, and behavioral intention in health care provider choice: A South Korean study. J. Bus. Res. 2004, 57, 913–921. [Google Scholar] [CrossRef]
- Amarantou, V.; Chatzoudes, D.; Kechagia, V.; Chatzoglou, P.D. The impact of service quality on patient satisfaction and revisiting intentions: The case of public emergency departments. Qual. Manag. Health Care. 2019, 28, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Hu, Y.; Pfaff, H.; Wang, L.; Deng, L.; Lu, C.; Xia, S.; Cheng, S.; Zhu, X.; Wu, X. Determinants of Patients’ Intention to Use the Online Inquiry Services Provided by Internet Hospitals: Empirical Evidence from China. J. Med. Internet Res. 2020, 22, e22716. [Google Scholar] [CrossRef]
- Cherif, E.; Nora, B.; Mzough, M. Do personal health concerns and trust in healthcare providers mitigate privacy concerns? Effects on patients’ intention to share personal health data on electronic health records. Soc. Sci. Med. 2021, 283, 114146. [Google Scholar] [CrossRef]
- Park, S.; Kim, H.-K.; Choi, M.; Lee, M. Factors affecting revisit intention for medical services at dental clinics. PLoS ONE 2021, 16, e0250546. [Google Scholar] [CrossRef]
- Pratama, V.; Hartini, S. The effect of perception of health care service quality on patient satisfaction and loyalty in mother and child hospital. J. Theory Appl. Manag. 2020, 13, 234–253. [Google Scholar] [CrossRef]
- Dobbs, P.; Warriner, D. Value-based health care: The strategy that will solve the NHS. Br. J. Hosp. Med. 2018, 79, 306–307. [Google Scholar] [CrossRef]
- Canaway, R.; Bismark, M.; Dunt, D.; Kelahar, M. Medical directors’ perspectives on strengthening hospital quality and safety. J. Health Organ. Manag. 2017, 31, 696–712. [Google Scholar] [CrossRef] [PubMed]
- Han, H. The healthcare hotel: Distinctive attributes for international medical travelers. Tour. Manag. 2013, 36, 257–268. [Google Scholar] [CrossRef]
- Zainuddin, N.; Previte, J.; Russell-Bennett, R. A social marketing approach to value creation in a well-women’s health service. J. Mark. Manag. 2011, 227, 361–385. [Google Scholar] [CrossRef]
- Rocha, J.; Pinto, A.; Batista, M.; Paula, J.S.D.; Ambrosano, G. The importance of the evaluation of expectations and perceptions to improve the dental service quality. Inter. J. Health Care Qual. Assur. 2017, 30, 568–576. [Google Scholar] [CrossRef]
- Upadhyai, R.; Upadhyai, N.; Jain, A.K.; Chopra, G.; Roy, H.; Pant, V. Development and validation of a scale for measuring hospital service quality: A dyadic approach. J. Health Res. 2021, 21, 102–127. [Google Scholar] [CrossRef]
- Gutman, J. Means-End Chains as Goal Hierarchies. Psychol. Mark. 1997, 14, 545–560. [Google Scholar] [CrossRef]
- Cronin, J.J.; Brady, M.K.; Hult, G.T.M. Assessing the effects of quality, value, and customer satisfaction on consumer behavioral intentions in service environments. J. Retail. 2000, 76, 193–218. [Google Scholar] [CrossRef]
- Spence, M. Job Market Signaling. Quar. J. Econ. 1973, 87, 355–374. Available online: https://www.jstor.org/stable/1882010 (accessed on 2 August 2023). [CrossRef]
- Ai, Y.; Rahman, M.K.; Newaz, M.S.; Gazi, M.A.I.; Rahaman, M.A.; Mamun, A.A.; Chen, X. Determinants of patients’ satisfaction and trust toward healthcare service environment in general practice clinics. Front. Psychol. 2022, 13, 856750. [Google Scholar] [CrossRef]
- Tanwar, T.; Kumar, U.D.; Mustafee, N. Optimal package pricing in healthcare services. J. Oper. Res. Soc. 2020, 71, 1860–1872. [Google Scholar] [CrossRef]
- Batalden, M.; Batalden, P.; Margolis, P.; Seid, M.; Armstrong, G.; Opipari-Arrigan, L.; Hartung, H. Coproduction of healthcare service. BMJ Qual. Saf. 2016, 25, 509–517. [Google Scholar] [CrossRef]
- Hwang, J.; Joo, K.; Kim, I. Identifying Chinese tourists’ shopping values and their consequences in the context of a duty-free shop: The moderating role of country image. Sustainability 2023, 15, 5304. [Google Scholar] [CrossRef]
- Fishbein, M.; Ajzen, I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research; Addison-Wesley: Reading, MA, USA, 1975. [Google Scholar]
- Baker, D.; Crompton, J. Quality, Satisfaction, and Behavioral Intentions. Ann. Tour. Res. 2000, 27, 785–804. [Google Scholar] [CrossRef]
- Perera, S.; Dabney, B.W. Case management service quality, and patient-centered care. J. Health Organ. Manag. 2020, 34, 551–568. [Google Scholar] [CrossRef]
- Rahman, M.S.; Mannan, M.; Hossain, M.A.; Zaman, M.H. Patient’s behavioral intention: Public and private hospitals context. Mark. Intell. Plan. 2018, 36, 349–364. [Google Scholar] [CrossRef]
- Chiou, J.S.; Droge, C. Service Quality, Trust, Specific Asset Investment, and Expertise: Direct and Indirect Effects in a Satisfaction-Loyalty Framework. J. Acad. Mark. Sci. 2006, 34, 613–627. [Google Scholar] [CrossRef]
- Parasuraman, A.; Zeithaml, V.A.; Berry, L.L. SERVQUAL: A multiple-item scale for measuring consumer perceptions of service quality. J. Retail. 1985, 64, 794–839. [Google Scholar]
- Morgan, R.M.; Hunt, S.D. The commitment-trust theory of relationship marketing. J. Mark. 1994, 58, 20–38. [Google Scholar] [CrossRef]
- Mayer, R.C.; Davis, J.H.; Schoorman, F.D. An integrative model of organizational trust. Acad. Manag. Rev. 1995, 20, 709–734. [Google Scholar] [CrossRef]
- Hernandez, J.M.; Dos Santos, C.C. Development-based trust: Proposing and validating a new trust measurement model for buyer-seller relationships. BAR Braz. Adm. Rev. 2010, 7, 172–197. [Google Scholar] [CrossRef]
- Porter, M.E. What is value in health care? The New England. J. Med. 2010, 363, 2477–2481. [Google Scholar] [CrossRef]
- Erkutlu, H.; Chopra, J. Value congruence and commitment to change in healthcare organizations. J. Adv. Manag. Res. 2016, 13, 316–333. [Google Scholar] [CrossRef]
- Norman, R.; Chalkidou, K.; Culyer, A. Health Economics Approach to US Value Frameworks: Serving the Needs of Decision Making. Value Health 2018, 21, 117–118. [Google Scholar] [CrossRef] [PubMed]
- Nordgren, L. Value creation in health care services–developing service productivity Experiences from Sweden. Int. J. Public Sect. Manag. 2009, 22, 114–127. [Google Scholar] [CrossRef]
- Pekkaya, M.; Pulat İmamoğlu, Ö.; Koca, H. Evaluation of healthcare service quality via Servqual scale: An application on a hospital. Intern. J. Healthc. Manag. 2019, 12, 340–347. [Google Scholar] [CrossRef]
- Endeschaw, B. Healthcare service quality-measurement models: A review. J. Health Res. 2021, 35, 106–117. [Google Scholar] [CrossRef]
- Upadhyai, R.; Jain, A.K.; Roy, H.; Pant, V. A review of healthcare service quality dimensions and their measurement. J. Health Manag. 2019, 21, 102–127. [Google Scholar] [CrossRef]
- Tuzovic, S.; Kuppelwieser, V. Developing a framework of service convenience in health care: An exploratory study for a primary care provider. Health Mark. Q. 2016, 33, 127–148. [Google Scholar] [CrossRef]
- Maarse, H.; Jeurissen, P. Low institutional trust in health insurers in Dutch health care. Health Policy 2019, 123, 288–292. [Google Scholar] [CrossRef]
- Higgins, A.; Barnett, J.; Meads, C.; Singh, J.; Longworth, L. Does Convenience Matter in Health Care Delivery? A Systematic Review of Convenience-Based Aspects of Process Utility. Value Health 2014, 17, 877–887. [Google Scholar] [CrossRef]
- Masterson, L. Convenience Is More Important to Patients than the Quality of Care, a Survey Finds, a Report Published in Health Care Drive. 2019. Available online: https://www.healthcaredive.com/news/convenience-more-important-to-patients-than-quality-of-care-survey-finds/545365/ (accessed on 3 April 2023).
- Sulphey, M.; Jasimm, K. Ascertaining service quality and medical practitioners’ sensitivity towards surgical instruments using SERVQUAL. Bench Intern. J. 2020, 28, 370–405. [Google Scholar] [CrossRef]
- Aagja, J.P.; Mammen, T.; Saraswat, A. Validating service convenience scale and profiling customers: A study in the Indian retail context. Vikalpa J. Decis. Mak. 2011, 36, 25–49. [Google Scholar] [CrossRef]
- Lewandowski, R.; Goncharuk, A.G.; Cirella, G.T. Restoring patient trust in healthcare: Medical information impact case study in Poland. BMC Health Serv. Res. 2021, 21, 865. [Google Scholar] [CrossRef]
- Mechanic, D.; Meyer, S. Concepts of trust among patients with serious illness. Soc. Sci. Med. 2000, 51, 657–668. [Google Scholar] [CrossRef]
- Van Der Schee, E.; Groenewegen, P.P.; Friele, R.D. Public trust in health care: A performance indicator? J. Health Organ. Manag. 2006, 20, 468–476. [Google Scholar] [CrossRef] [PubMed]
- Bouhlel, O.; Garrouch, K.; Mzoughi, M.N. Assessing the Success of Mobile Banking in Saudi Arabia: Re-Specification and Validation of the DeLone and McLean Model. Int. J. E-Serv. Mob. Appl. IJESMA 2023, 15, 1–24. [Google Scholar] [CrossRef]
- Ghali, Z. Motives of customers’ e-loyalty towards e-banking services: A study in Saudi Arabia. J. Dec. Syst. 2021, 30, 1–23. [Google Scholar] [CrossRef]
- Zeithaml, V.A. Consumer perceptions of price, quality, and value: A means-end model and synthesis of evidence. J. Mark. 1988, 52, 2–22. [Google Scholar] [CrossRef]
- Morris, B.; Abram, M.A. President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. 1982. 1, 109p. Available online: https://repository.library.georgetown.edu/bitstream/handle/10822/559354/making_health_care_decisions.pdf?sequence=1&isAllowed=y (accessed on 23 May 2023).
- Williams, S.J.; Nightingale, E.O.; Filner, B. The Physician’s Role in a Changing Health Care System”, Chapter 4 of the Book Medical Education and Societal Needs: A Planning Report for the Health Professions; National Academies Press (US): Washington, DC, USA, 1983. Available online: https://www.ncbi.nlm.nih.gov/books/NBK217690/ (accessed on 3 August 2023).
- Brenan, M. Nurses Again Outpace Other Professions for Honesty, Anethics. 2018. Available online: https://news.gallup.com/poll/245597/nurses-again-outpace-professions-honesty-ethics.aspx#:%7E:text=WASHINGTON%2C%20D.C.%20%2D%2D%20More%20than,the%2017th%20consecutive%20year (accessed on 12 August 2023).
- Coman, E.; Diaconu, A.; Mesesan Schmitz, L.; Repanovici, A.; Baritz, M.; Coman, C.; Fotea, S. Patient Satisfaction with Private Recovery Services and Importance of Physician Behavior during COVID Time. Healthcare 2021, 9, 928. [Google Scholar] [CrossRef]
- He, J.; Hu, C.; Lin, C.C. Service Innovation, Inter-organizational Trust, and Performance in Hospital Platforms: Social Network and Agency Perspectives. Front. Public Health 2022, 10, 819371. [Google Scholar] [CrossRef]
- Arrow, K.J. Uncertainty and the welfare economics of medical care. Am. Econ. Rev. 1963, 53, 941–973. [Google Scholar]
- Dobrzykowski, D.D.; McFadden, K.L. Examining Governance in Hospital Operations: The Effects of Trust and Physician Employment in Achieving Efficiency and Patient Satisfaction. Dec. Sci. 2020, 51, 74–109. [Google Scholar] [CrossRef]
- Major, I. Two-Sided Information Asymmetry in the Healthcare Industry. Int. Adv. Econ. Res. 2019, 25, 177–193. [Google Scholar] [CrossRef]
- Higgins, J.A.; Schmuhl, N.B.; Woutlet, C.K.; Rice, L.W.; Rice, L.W. The importance of physician concern and expertise in increasing abortion health care access in local contexts. Am. J. Public Health 2021, 111, 33–36. [Google Scholar] [CrossRef]
- Einwiller, S. When Reputation Engenders Trust: An Empirical Investigation in Business-to-Consumer Electronic Commerce. Electron. Mark. 2003, 13, 196–209. [Google Scholar] [CrossRef]
- Kaushik, A.K.; Mohan, G.; Kumar, V. Examining the antecedents and consequences of customers’ trust toward mobile retail apps in India. J. Internet Commer. 2020, 19, 1–31. [Google Scholar] [CrossRef]
- Garrouch, K. Does the reputation of the provider matter? A model explaining the continuance intention of mobile wallet applications. J. Decim. Syst. 2021, 30, 150–171. [Google Scholar] [CrossRef]
- Milan, G.S.; Eberle, L.; Bebber, S. Perceived Value, Reputation, Trust, and Switching Costs as Determinants of Customer Retention. J. Relat. Mark. 2015, 14, 109–123. [Google Scholar] [CrossRef]
- Kadhim, K.G.; Harun, A.; Hamawandy, N.M. Factors influencing (Reputation, Perceived Value, Location, Convenience, Internal Environment, and Staff) on Customer Loyalty through Satisfaction: Perspective from Malaysia Hypermarket Industry. J. Contemp. Issues Bus. Gov. 2021, 27, 5243–5263. [Google Scholar]
- Torres, E.; Vasquez-Parraga, A.Z.; Barra, C. The path of patient loyalty and the role of doctor reputation. Health Mark. Quart. 2009, 26, 183–197. [Google Scholar] [CrossRef]
- Hall, M.A.; Camacho, F.; Dugan, E.; Balkrishnan, R. Trust in the medical profession: Conceptual and measurement issues. Health Serv. Res. 2002, 37, 1419–1439. [Google Scholar] [CrossRef]
- Rahman, M.S.; Hossain, M.A.; Zaman, M.H.; Mannan, M. E-Service Quality and Trust on Customer’s Patronage Intention: Moderation Effect of Adoption of Advanced Technologies. J. Glob. Inf. Manag. 2020, 28, 39–55. [Google Scholar] [CrossRef]
- Zheng, S.; Hui, S.F.; Yang, Z. Hospital trust or doctor trust? A fuzzy analysis of trust in the health care setting. J. Bus. Res. 2017, 78, 217–225. [Google Scholar] [CrossRef]
- Kim, J.; Nam, M.; Kim, I. The effect of trust on value on travel websites: Enhancing well-being and word-of-mouth among the elderly. J. Trav. Tour. Mark. 2019, 36, 76–89. [Google Scholar] [CrossRef]
- Ngobo, P.V. Drivers of customers’ cross-buying intentions. Eur. J. Mark. 2004, 38, 1129–1157. [Google Scholar] [CrossRef]
- Nordgren, S.; Fridlund, B. Patients’ perceptions of self-determination as expressed in the context of care. J. Adv. Nurs. 2001, 35, 117–125. [Google Scholar] [CrossRef]
- Hwang, J.; Lee, K.-W.; Kim, D.; Kim, I. Robotic Restaurant Marketing Strategies in the Era of the Fourth Industrial Revolution: Focusing on Perceived Innovativeness. Sustainability 2020, 12, 9165. [Google Scholar] [CrossRef]
- Medhekar, A.; Wong, H.Y.; Hall, J.E. Health-care providers perspective on the value in medical travel to India. Tour. Rev. 2020, 75, 717–731. [Google Scholar] [CrossRef]
- Dodds, S.; Bulmer, S.; Murphy, A. Consumer value in complementary and alternative medicine (CAM) health care services. Australas. Mark. J. 2014, 22, 218–229. [Google Scholar] [CrossRef]
- Fornell, C.; Johnson, M.; Anderson, E.; Cha, J.; Bryant, B. The American Customer Satisfaction Index: Nature, Purpose and Findings. J. Mark. 1996, 60, 7–18. [Google Scholar] [CrossRef]
- Global Media Insight. Saudi Arabia Population Statistics Article. 2022. Available online: https://www.globalmediainsight.com/blog/saudi-arabia-population-statistics/ (accessed on 17 May 2022).
- Hair, J.F., Jr.; Hult, T.G.; Ringle, C.M.; Arstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM); Sage Publications: New York, NY, USA, 2014. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Hair, J.R.; Joseph, F.; Anderson, R.E.; Tatham, R.L. Multivariate Data Analysis with Readings; Macmillan: London, UK, 1998. [Google Scholar]
- Cohen, J. Statistical Power Analysis, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Geisser, S. A predictive approach to the random effect model. Biometrika 1974, 61, 101–107. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sinkovics, R.R. The use of partial least squares path modeling in international marketing. Adv. Intern. Mark. 2009, 20, 277–319. [Google Scholar] [CrossRef]
- Chang, C.S.; Chen, S.Y.; Lan, Y.T. Service quality, trust, and patient satisfaction in interpersonal-based medical service encounters. BMC Health Serv. Res. 2013, 13, 22. [Google Scholar] [CrossRef] [PubMed]
- Alrubaiee, L.; Alkaaida, F. The Mediating Effect of Patient Satisfaction in the Patients’ Perceptions of Healthcare Quality–Patient Trust Relationship. Intern. J. Mark. Stud. 2011, 3, 103–127. [Google Scholar] [CrossRef]
- Zhou, T. Understanding users’ initial trust in mobile banking: An elaboration likelihood perspective. Comput. Hum. Behav. 2020, 28, 1518–1525. [Google Scholar] [CrossRef]
- Mzoughi, M.N.; Garrouch, K.F. Reactions to Store Environment and Interpersonal Service Quality in Supermarkets vs Hypermarkets. J. Distrib. Sci. 2022, 20, 67–76. [Google Scholar] [CrossRef]
- Zarei, E.; Daneshkohan, A.; Khabiri, R.; Arab, M. The Effect of Hospital Service Quality on Patient’s Trust. Iran. Red Crescent Med. J. 2014, 17, 1. [Google Scholar] [CrossRef]
| Variable | Classification | Number | Percentage |
|---|---|---|---|
| Gender | Male | 125 | 51.65% |
| Female | 117 | 48.34% | |
| Age range | 18–25 | 21 | 8.67% |
| 26–30 | 83 | 34.30% | |
| 31–40 | 93 | 38.42% | |
| 41–50 | 34 | 14.04% | |
| More than 50 | 11 | 4.55% | |
| Nationality | Saudi | 219 | 90.5% |
| Non-Saudi | 23 | 9.5% | |
| Public vs. private hospital | Public hospital | 92 | 38% |
| Private hospital | 150 | 62% |
| Construct | Cronbach’s Alpha | Rho_A | CR | (AVE) |
|---|---|---|---|---|
| Behavioral intention | 0.911 | 0.911 | 0.944 | 0.849 |
| Convenience of the care process | 0.799 | 0.826 | 0.861 | 0.555 |
| Healthcare provider concern | 0.848 | 0.853 | 0.898 | 0.689 |
| Physician concern | 0.908 | 0.911 | 0.931 | 0.731 |
| Reputation of doctor | 0.789 | 0.795 | 0.876 | 0.703 |
| service value | 0.819 | 0.833 | 0.891 | 0.732 |
| Trust toward doctor | 0.846 | 0.858 | 0.907 | 0.766 |
| Trust toward the provider | 0.814 | 0.823 | 0.876 | 0.639 |
| Variable | Classification | F2 | R2 | Q2 |
|---|---|---|---|---|
| Behavioral intention | Service Value | 0.111 | 0.558 | 0.442 |
| Trust in the physician | 0.049 | |||
| Trust toward the HC provider | 0.113 | |||
| Trust toward the HC provider | Convenience | 0.004 | 0.374 | 0.303 |
| HC provider concern | 0.07 | |||
| Physician concern | 0.065 | |||
| Trust in the physician | Reputation of the doctor | 0.735 | 0.424 | 0.303 |
| Service value | Convenience | 0.053 | 0.529 | 0.358 |
| HC provider concern | 0.025 | |||
| Physician concern | 0.014 | |||
| Reputation of the doctor | 0.115 |
| Original Sample (O) | Sample Mean (M) | Standard Deviation (STDEV) | t-Statistics (|O/STDEV|) | p-Values | Hypotheses | |
|---|---|---|---|---|---|---|
| Convenience of care process → Trust toward the provider | 0.072 | 0.079 | 0.072 | 1.008 | 0.314 | H1a rejected |
| Convenience of care process → Service value | 0.218 | 0.221 | 0.061 | 3.559 | 0.000 | H1b accepted |
| Healthcare provider concern → Trust toward the provider | 0.326 | 0.326 | 0.085 | 3.837 | 0.000 | H2a accepted |
| Healthcare provider concern → Service value | 0.173 | 0.171 | 0.075 | 2.314 | 0.021 | H2b accepted |
| Physician concern → Trust toward the provider | 0.283 | 0.281 | 0.084 | 3.360 | 0.001 | H3a accepted |
| Physician concern → Service value | 0.129 | 0.131 | 0.086 | 1.499 | 0.134 | H3b rejected |
| Reputation of doctor → Service value | 0.340 | 0.339 | 0.076 | 4.457 | 0.000 | H4a accepted |
| Reputation of the doctor → Trust toward the doctor | 0.651 | 0.653 | 0.040 | 16.105 | 0.000 | H4b accepted |
| Trust toward the provider → Behavioral intention | 0.315 | 0.319 | 0.063 | 4.985 | 0.000 | H5a accepted |
| Trust toward doctor → Behavioral intention | 0.237 | 0.233 | 0.086 | 2.742 | 0.006 | H5b accepted |
| Service value → Behavioral intention | 0.306 | 0.310 | 0.070 | 4.381 | 0.000 | H6 accepted |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghali, Z.; Garrouch, K.; Aljasser, A. Drivers of Patients’ Behavioral Intention toward Public and Private Clinics’ Services. Healthcare 2023, 11, 2336. https://doi.org/10.3390/healthcare11162336
Ghali Z, Garrouch K, Aljasser A. Drivers of Patients’ Behavioral Intention toward Public and Private Clinics’ Services. Healthcare. 2023; 11(16):2336. https://doi.org/10.3390/healthcare11162336
Chicago/Turabian StyleGhali, Zohra, Karim Garrouch, and Abdulrahman Aljasser. 2023. "Drivers of Patients’ Behavioral Intention toward Public and Private Clinics’ Services" Healthcare 11, no. 16: 2336. https://doi.org/10.3390/healthcare11162336
APA StyleGhali, Z., Garrouch, K., & Aljasser, A. (2023). Drivers of Patients’ Behavioral Intention toward Public and Private Clinics’ Services. Healthcare, 11(16), 2336. https://doi.org/10.3390/healthcare11162336





