Program Report: Improving Patient Experience at an Outpatient Clinic Using Continuous Improvement Tools
Abstract
1. Introduction
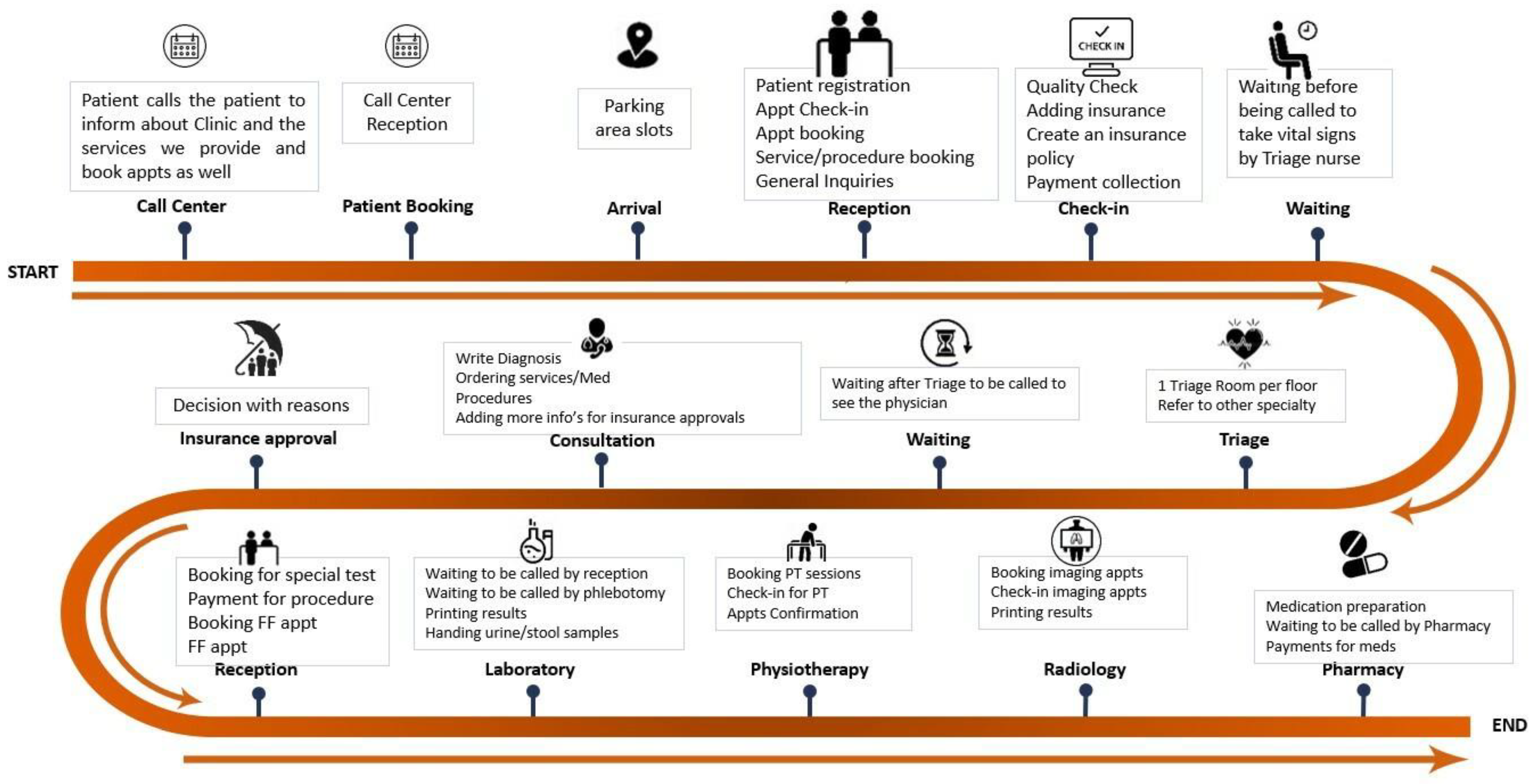
2. Methods
2.1. Data Collection
2.2. Continuous Improvement Process
3. Results
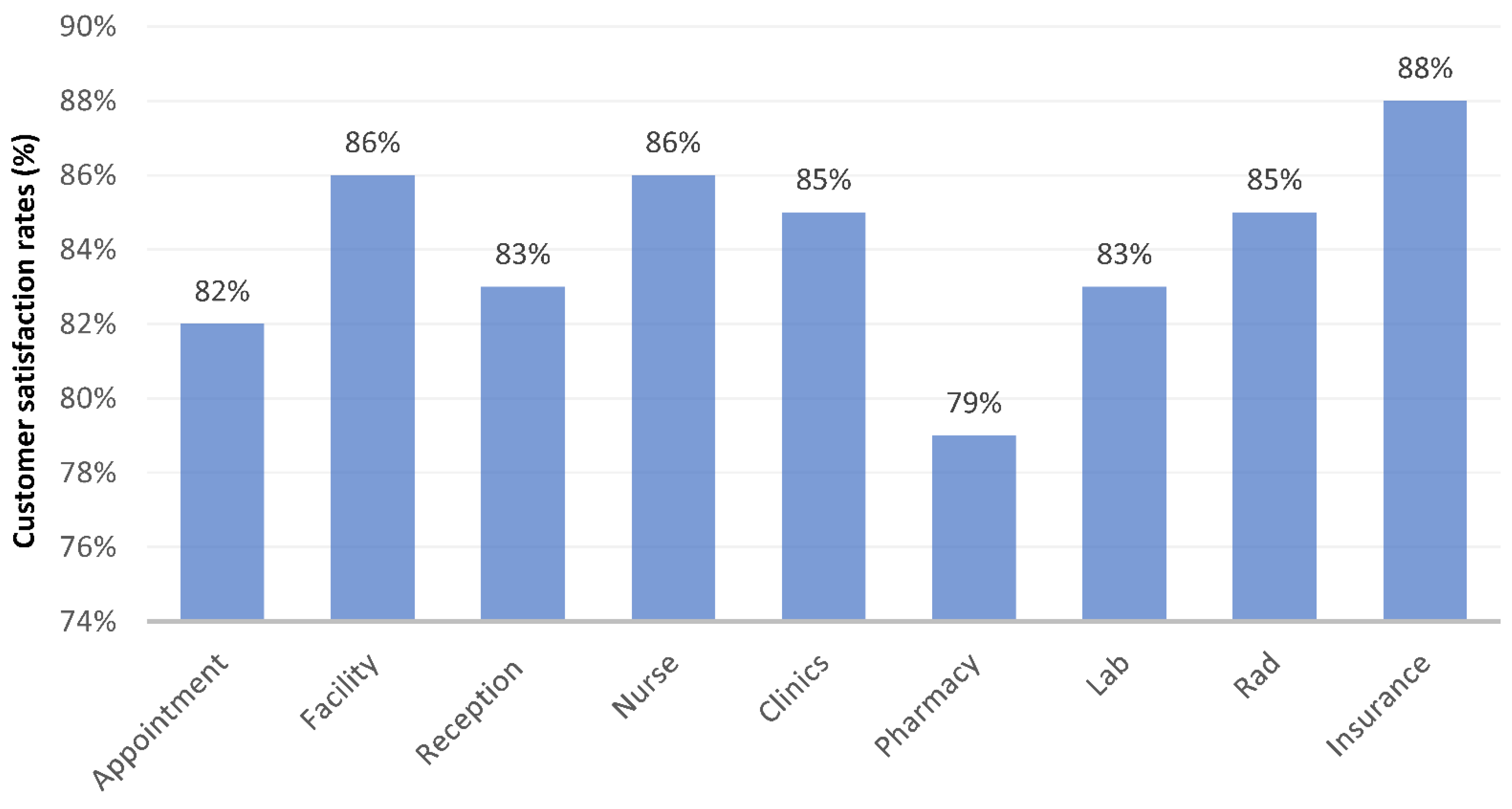
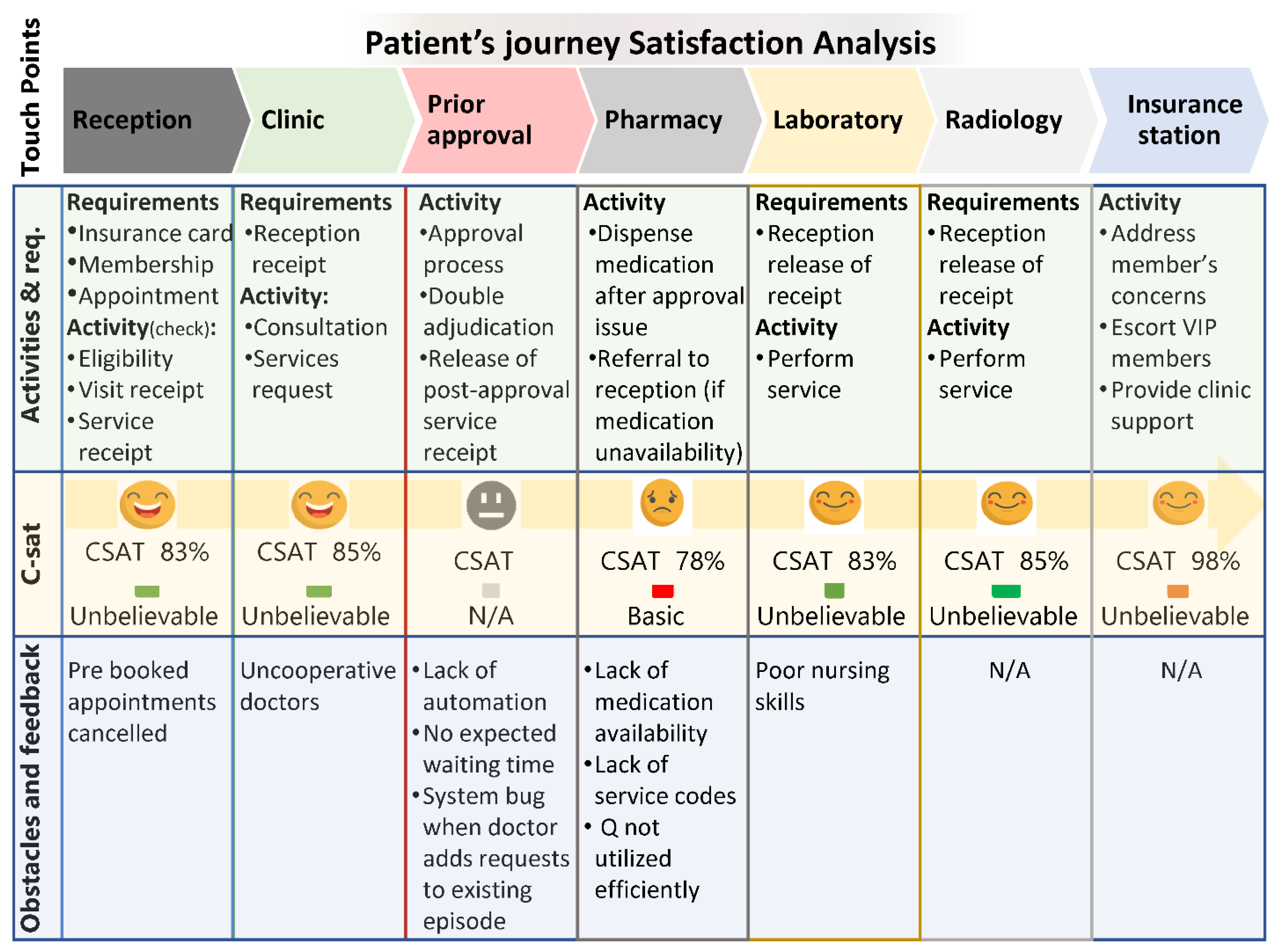
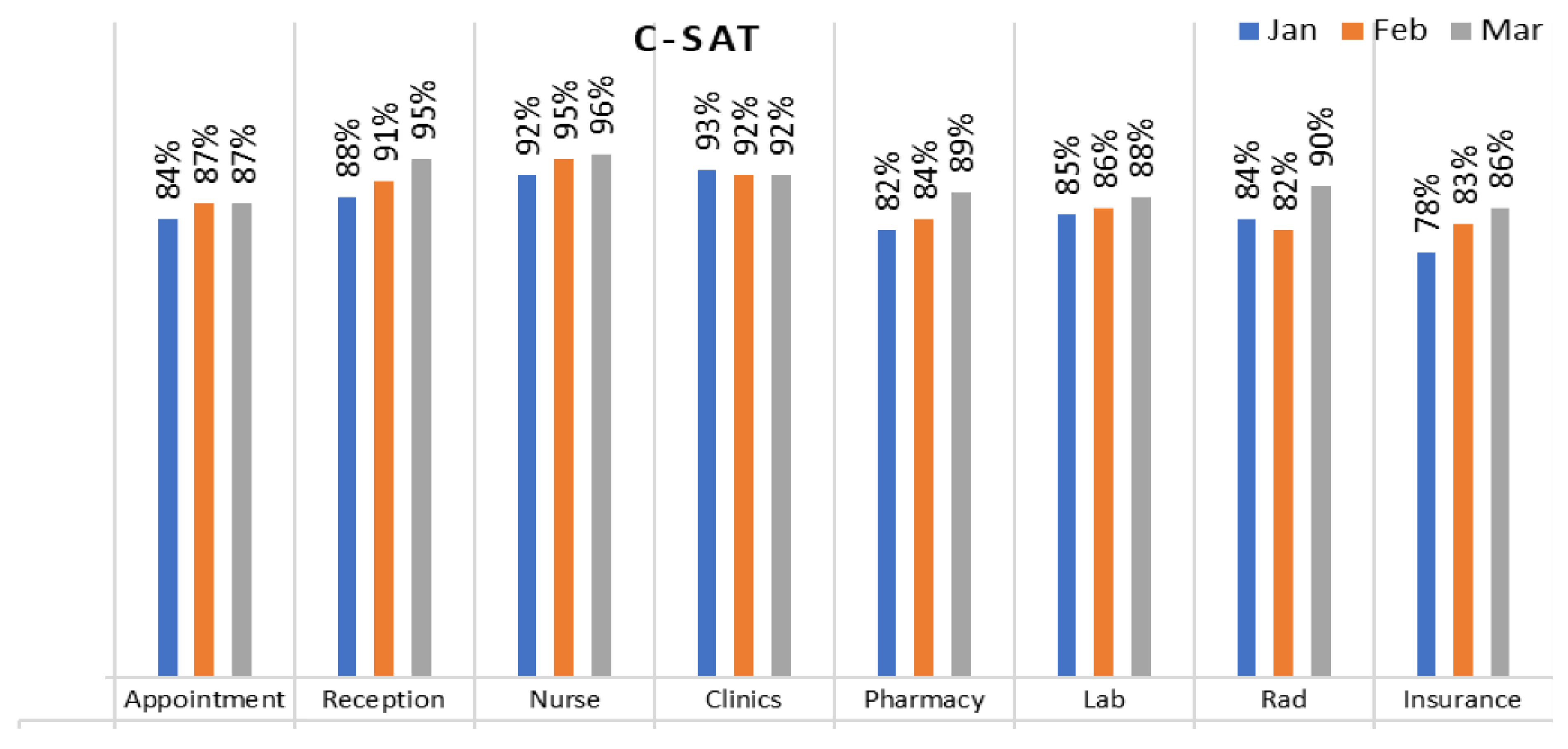
3.1. Customer Satisfaction
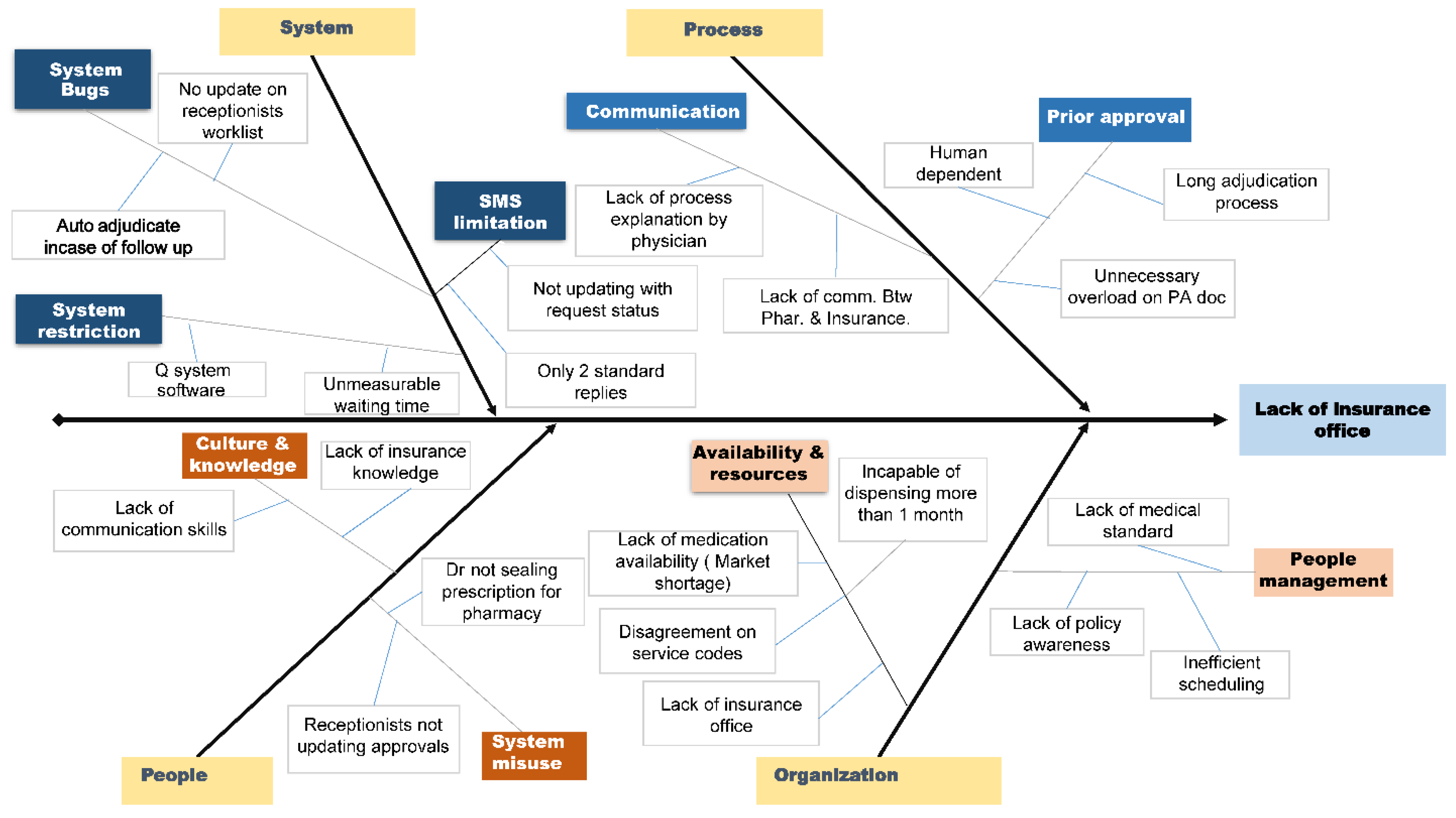
3.2. Root Causes of Patients’ Dissatisfaction
3.3. Continuous Improvement Program Application
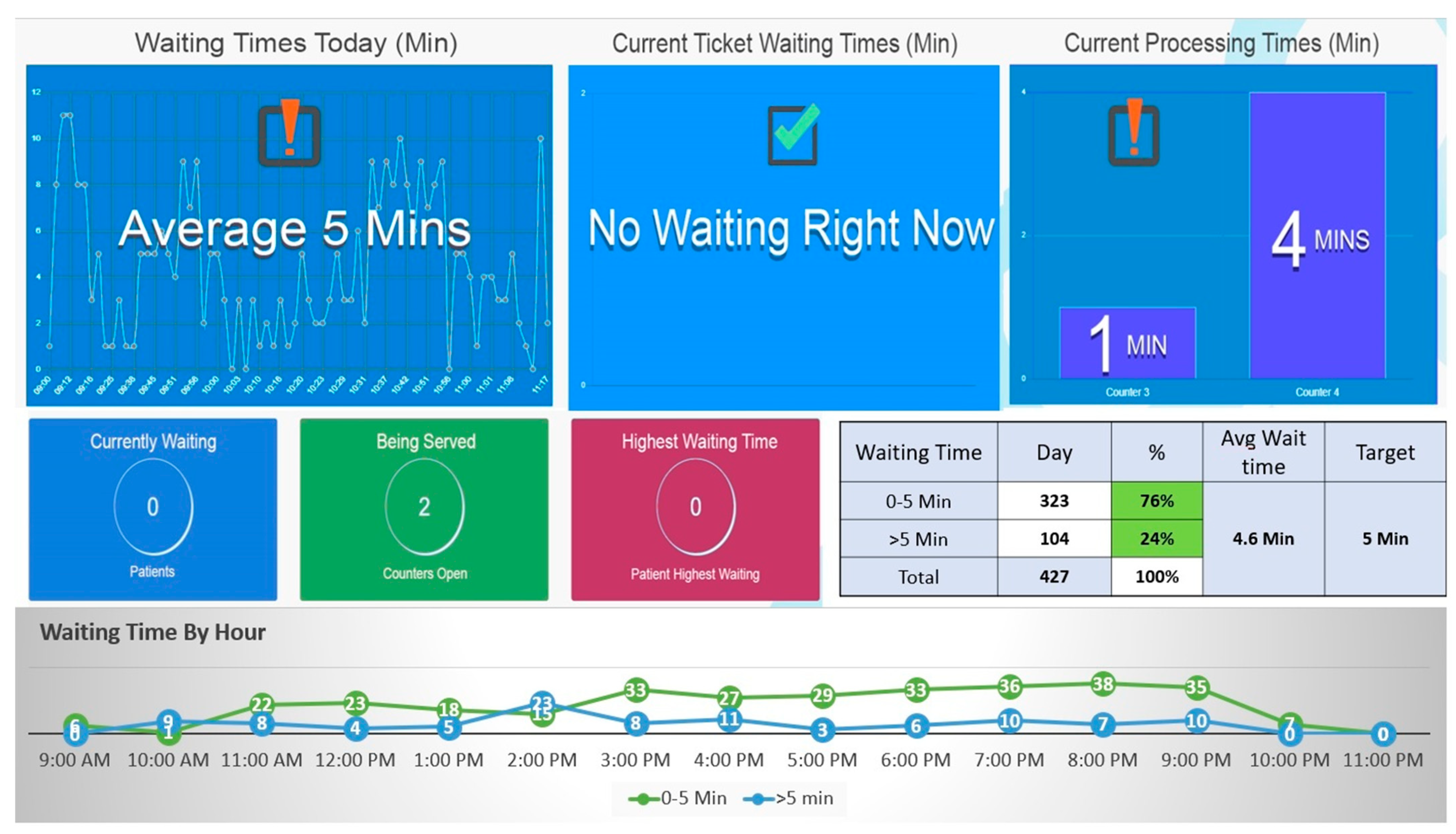
3.4. System Display and Preliminary Evaluation
4. Discussion
4.1. Progress Made
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khan, S.A.; Kaviani, M.A.; Galli, B.J.; Ishtiaq, P. Application of continuous improvement techniques to improve organization performance: A case study. Int. J. Lean Six Sigma 2019, 10, 542–565. [Google Scholar] [CrossRef]
- Doyle, C.; Lennox, L.; Bell, D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013, 3, e001570. [Google Scholar] [CrossRef] [PubMed]
- Galli, B.J.; Kaviani, M.A. The Impacts of Risk on Deploying and Sustaining Lean Six Sigma Initiatives. Int. J. Risk Conting. Manag. 2018, 7, 46–70. [Google Scholar] [CrossRef]
- Shang, G.; Pheng, S. Understanding the application of Kaizen methods in construction firms in China. J. Technol. Manag. China 2013, 8, 18–33. [Google Scholar] [CrossRef]
- McLean, R.; Antony, J. Why continuous improvement initiatives fail in manufacturing environments? A systematic review of the evidence. Int. J. Product. Perform. Manag. 2014, 63, 370–376. [Google Scholar] [CrossRef]
- Indrawati, S.; Ridwansyah, M. Manufacturing Continuous Improvement Using Lean Six Sigma: An Iron Ores Industry Case Application. Procedia Manuf. 2015, 4, 528–534. [Google Scholar] [CrossRef]
- McCalman, J.; Bailie, R.; Bainbridge, R.; McPhail-Bell, K.; Percival, N.; Askew, D.; Fagan, R.; Tsey, K. Continuous Quality Improvement and Comprehensive Primary Health Care: A Systems Framework to Improve Service Quality and Health Outcomes. Front. Public Health 2018, 6, 76. [Google Scholar] [CrossRef]
- Chudiwal, S.S.; Dehghan, M.H.G. Quality by design (QbD) approach for design and development of drug-device combination products: A case study on flunisolide nasal spray. Pharm. Dev. Technol. 2018, 23, 1077–1087. [Google Scholar] [CrossRef] [PubMed]
- Fujita, H.; Doi, K.; Chan, H.P.; Giger, M.L.; Duda, E.E. Dynamic and static phantoms for evaluation of digital subtraction angiographic systems. Radiology 1985, 155, 799–803. [Google Scholar] [CrossRef] [PubMed]
- Prakash, B. Patient satisfaction. J. Cutan. Aesthetic Surg. 2010, 3, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Berg, J.S.; Dischler, J.; Wagner, D.J.; Raia, J.J.; Palmer-Shevlin, N. Medication compliance: A healthcare problem. Ann. Pharmacother. 1993, 27, S1–S24. [Google Scholar] [PubMed]
- Trigg, L. Patients’ opinions of health care providers for supporting choice and quality improvement. J. Health Serv. Res. Policy 2011, 16, 102–107. [Google Scholar] [CrossRef] [PubMed]
| Category | Countermeasure | Task | Priority | |
|---|---|---|---|---|
| People | Optimize the utilization of human resources | Establishing a task force dedicated to providing comprehensive training on the table of benefits to all relevant staff members | M | Done |
| Implement technical skills training to ensure optimal utilization of the system, with a particular emphasis on providing doctors with access and proper training to effectively prescribe medications, thereby reducing the occurrence of technical errors and minimizing delays in the pharmacy. | H | Done | ||
| Ensure compliance with prescribing requirements to ensure the completion of prescriptions (whether manual or electronic) before reaching the pharmacy. | H | Done | ||
| Ensure effective communication between the pharmacy and the medical team to facilitate the exchange of any required information or changes at both levels. Additionally, service coordinators should provide support in cases where a response is not received | M | Done | ||
| Provide comprehensive soft skill training to the entire pharmacy team, focusing specifically on customer service excellence | H | Done | ||
| Implement a technical training program covering all retail products | H | Done | ||
| System | Eliminate system errors and enhance software utilization | Develop Queuing system software | H | Done |
| Develop full patient journey monitoring | H | Done | ||
| Revise the “MY Operation” system to eliminate incorrect auto-adjudication during follow-up episodes. | H | Done | ||
| Verify the system’s capability to support the setup of the table of benefits. | M | Done | ||
| Implement a system flag to identify uncovered medications at the point of delivery. | H | Done | ||
| Integrate the system at the pre-authorization level to reduce processing time, mitigate human errors, and optimize the staffing needs for the insurance office at My Clinic. | M | Done | ||
| Establish comprehensive SMS communication with members to provide updates on the status of their requests. | L | Done | ||
| Pharmacy/Integration of Clinical Support software: to Integrate the Lexicomp/UpToDate with pharmacy & Clinical AppLonger dispensing time to ensure Patient safety (Drug Interactions/drug dosing safety…etc.)—Impact 3 Min web browsing | H | Done | ||
| Implement automated barcode scanning to eliminate errors associated with batch barcode reading, ensuring accurate selection from a drop-down list in both the clinical application and point of sale for all items. This enhancement promotes patient safety by enabling the selection of the same dispensed batch and increases the dispensing time, resulting in a positive impact of one minute. | V.H | Done | ||
| Integrate credit/debit card readers into the point of sale (POS) system at the pharmacy to facilitate automated payments for mixed self and insurance payments. This integration will streamline the payment process, reducing the time required for transactions by two minutes. | V.H | Done | ||
| Organization | Leveling and optimizing resources | Address service code issues in the pharmacy | V.H | Done |
| Establish key performance indicators for clinical practice. | H | Done | ||
| Allocate dedicated administrative staff to handle pre-authorized transactions exclusively. | M | Done | ||
| Evaluate and revise the capacity plan for pharmacist scheduling. | M | Done | ||
| Design and share the end-to-end process for the insurance office. | V.H | Done | ||
| Process | Automat back-end insurance office | Ensure timely procurement of all unavailable medications to maintain a consistent supply. | H | done |
| Streamline inventory management practices for medications. | H | Done | ||
| Revise the pharmacy planogram to enhance the display of newly added retail stock-keeping units, thereby boosting retail sales. | H | Done |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siddiqui, M.U.H.; Khafagy, A.A.; Majeed, F. Program Report: Improving Patient Experience at an Outpatient Clinic Using Continuous Improvement Tools. Healthcare 2023, 11, 2301. https://doi.org/10.3390/healthcare11162301
Siddiqui MUH, Khafagy AA, Majeed F. Program Report: Improving Patient Experience at an Outpatient Clinic Using Continuous Improvement Tools. Healthcare. 2023; 11(16):2301. https://doi.org/10.3390/healthcare11162301
Chicago/Turabian StyleSiddiqui, Muhammad Usman Hassan, Abdullah Ahmed Khafagy, and Faisal Majeed. 2023. "Program Report: Improving Patient Experience at an Outpatient Clinic Using Continuous Improvement Tools" Healthcare 11, no. 16: 2301. https://doi.org/10.3390/healthcare11162301
APA StyleSiddiqui, M. U. H., Khafagy, A. A., & Majeed, F. (2023). Program Report: Improving Patient Experience at an Outpatient Clinic Using Continuous Improvement Tools. Healthcare, 11(16), 2301. https://doi.org/10.3390/healthcare11162301






