Socioeconomic Inequalities and Factors Associated with the Use of Modern Contraceptive Methods in Women of Childbearing Age in Ecuador, 2018
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Population and Sample
2.3. Variables
2.3.1. Dependent Variable
2.3.2. Independent Variable for the Analysis of Inequalities
2.3.3. Covariables
2.4. Statistical Analysis
2.5. Ethical Considerations
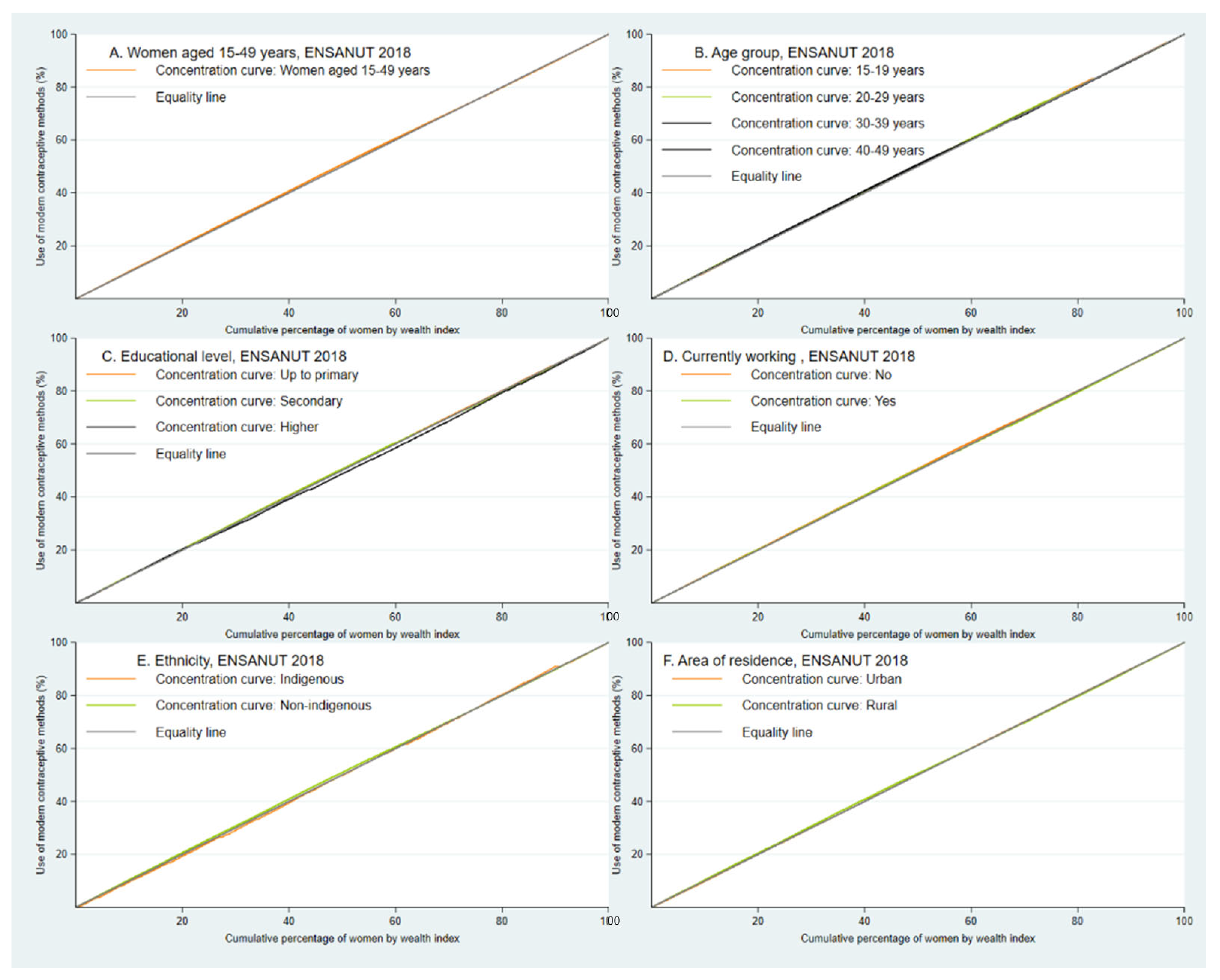
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Indicator Metadata Registry Details. Available online: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/4988 (accessed on 14 November 2022).
- Un Nuevo Estudio de la OMS Relaciona Las Altas Tasas de Embarazos no Planificados con Las Deficiencias de Los Servicios de Planificación Familiar. Available online: https://www.who.int/es/news/item/25-10-2019-high-rates-of-unintended-pregnancies-linked-to-gaps-in-family-planning-services-new-who-study (accessed on 12 October 2021).
- Organización Mundial de la Salud Contraception. 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/112319/WHO_RHR_14.07_eng.pdf?sequence=8 (accessed on 20 October 2021).
- Instituto Nacional de Estadística y Censos. Principales Resultados ENSANUT 2018. 2018. Available online: https://www.ecuadorencifras.gob.ec/documentos/web-inec/Estadisticas_Sociales/ENSANUT/ENSANUT_2018/Principales%20resultados%20ENSANUT_2018.pdf (accessed on 3 December 2022).
- Fondo de Población de las Naciones Unidas. Consecuencias Socioeconomicas del Embarazo y la Maternidad Adolescente del Perú. Available online: https://peru.unfpa.org/sites/default/files/pub-pdf/estudio_csemap_ver_digital_1.pdf (accessed on 13 October 2021).
- Sreeramareddy, C.T.; Acharya, K.; Tiwari, I. Inequalities in demand satisfied with modern methods of family planning among women aged 15–49 years: A secondary data analysis of Demographic and Health Surveys of six South Asian countries. BMJ Open 2022, 12, e049630. [Google Scholar] [CrossRef]
- de Leon, R.G.P.; Ewerling, F.; Serruya, S.J.; Silveira, M.F.; Sanhueza, A.; Moazzam, A.; Becerra-Posada, F.; Coll, C.V.N.; Hellwig, F.; Victora, C.G.; et al. Contraceptive use in Latin America and the Caribbean with a focus on long-acting reversible contraceptives: Prevalence and inequalities in 23 countries. Lancet Glob. Health 2019, 7, e227–e235. [Google Scholar] [CrossRef]
- Hlongwa, M.; Kalinda, C.; Peltzer, K.; Hlongwana, K. Factors associated with modern contraceptive use: A comparative analysis between younger and older women in Umlazi Township, KwaZulu-Natal, South Africa. Women’s Health 2021, 17, 17455065211060640. [Google Scholar]
- Tsehay, C.T. Factors associated with modern contraceptive demands satisfied among currently married/in-union women of reproductive age in Ethiopia: A multilevel analysis of the 2016 Demographic and Health Survey. BMJ Open 2022, 12, e049341. Available online: https://pubmed.ncbi.nlm.nih.gov/35110305/ (accessed on 15 November 2022).
- Akamike, I.C.; Okedo-Alex, I.N.; Eze, I.I.; Ezeanosike, O.B.; Uneke, C.J. Why does uptake of family planning services remain sub-optimal among Nigerian women? A systematic review of challenges and implications for policy. Contracept. Reprod. Med. 2020, 5, 30. [Google Scholar] [CrossRef] [PubMed]
- Blumenberg, C.; Hellwig, F.; Ewerling, F.; Barros, A.J.D. Socio-demographic and economic inequalities in modern contraception in 11 low- and middle-income countries: An analysis of the PMA2020 surveys. Reprod. Health 2020, 17, 82. [Google Scholar] [CrossRef] [PubMed]
- Rios-Quituizaca, P.; Gatica-Domínguez, G.; Nambiar, D.; Santos, J.L.F.; Barros, A.J.D. Ethnic inequalities in reproductive, maternal, newborn and child health interventions in Ecuador: A study of the 2004 and 2012 national surveys. eClinicalMedicine 2022, 45. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Estadística y Censos. Boletín Técnico ENSANUT 2018; Instituto Nacional de Estadística y Censo: Quito, Ecuador, 2019; p. 21. Available online: https://www.ecuadorencifras.gob.ec/documentos/web-inec/Estadisticas_Sociales/ENSANUT/ENSANUT_2018/Boletin%20ENSANUT%2028_12.pdf (accessed on 7 October 2022).
- Instituto Nacional de Estadística y Censos. Metodología ENSANUT-2018. 2019. Available online: https://www.ecuadorencifras.gob.ec/documentos/web-inec/Estadisticas_Sociales/ENSANUT/ENSANUT_2018/Metodologia%20ENSANUT%202018.pdf (accessed on 3 December 2021).
- INEC. Encuesta Nacional de Salud y Nutrición. Instituto Nacional de Estadística y Censos. Available online: https://www.ecuadorencifras.gob.ec/documentos/web-inec/Estadisticas_Sociales/ENSANUT/ENSANUT_2018/Formularios%20ENSANUT%202018_1.zip (accessed on 11 December 2022).
- O’Donnell, O.; van Doorslaer, E.; Wagstaff, A.; Lindelow, M. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation; World Bank: Washington, DC, USA, 2008; Available online: https://openknowledge.worldbank.org/handle/10986/6896 (accessed on 3 February 2022).
- Intriago, E.M.; Carvajal, M.S.; Valeriano, K.L. Construcción de un índice de riqueza utilizando Componentes Principales. Matemática 2020, 18, 1–13. [Google Scholar]
- O’Neill, J.; Tabish, H.; Welch, V.; Petticrew, M.; Pottie, K.; Clarke, M.; Evans, T.; Pardo, J.P.; Waters, E.; White, H.; et al. Applying an equity lens to interventions: Using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J. Clin. Epidemiol. 2014, 67, 56–64. [Google Scholar] [CrossRef]
- Cochrane Equity. PROGRESS-Plus. Available online: https://methods.cochrane.org/equity/projects/evidence-equity/progress-plus (accessed on 9 December 2022).
- Zegeye, B.; Ahinkorah, B.O.; Idriss-Wheeler, D.; Olorunsaiye, C.Z.; Adjei, N.K.; Yaya, S. Modern contraceptive utilization and its associated factors among married women in Senegal: A multilevel analysis. BMC Public Health 2021, 21, 231. [Google Scholar] [CrossRef]
- Seidu, A.A.; Agbaglo, E.; Dadzie, L.K.; Ahinkorah, B.O.; Ameyaw, E.K.; Tetteh, J.K.; Yaya, S. Modern contraceptive utilization and associated factors among married and cohabiting women in Papua New Guinea: A population-based cross-sectional study. Contracept. Reprod. Med. 2020, 5, 22. [Google Scholar]
- Manual del Encuestador ENSANUT F1.pdf. Available online: https://www.ecuadorencifras.gob.ec/documentos/web-inec/Estadisticas_Sociales/ENSANUT/ENSANUT_2018/Manuales%20ENSANUT%202018_1.zip (accessed on 14 November 2022).
- Aboluwaji, D.; Olufunke, A. Differentials in Contraceptive Use Among Selected Minority Ethnic Groups in Nigeria. Available online: https://www.frontiersin.org/articles/10.3389/fgwh.2022.878779/full (accessed on 11 December 2022).
- Melo, C.R.M.; Borges, A.L.V.; Duarte, L.S.; Nascimento, N.d.C. Uso de métodos anticonceptivos e intencionalidad de embarazo entre las mujeres usuarias del Sistema Público de Salud Brasileño. Rev. Lat. Am. Enferm. 2020, 28. [Google Scholar] [CrossRef]
- Dulanto-Ramos, Y.B.; Luna-Muñoz, C.; Roldan, L.; Dulanto-Ramos, Y.B.; Luna-Muñoz, C.; Roldan, L. Factores asociados al no uso de métodos anticonceptivos en mujeres adolescentes del Péru. Endes 2018–2020. Rev. Fac. Med. Humana 2022, 22, 345–352. [Google Scholar] [CrossRef]
- Kavanaugh, M.L.; Douglas-Hall, A.; Finn, S.M. Health insurance coverage and contraceptive use at the state level: Findings from the 2017 Behavioral Risk Factor Surveillance System. Contracept X 2019, 2, 100014. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, O.; O’Neill, S.; Van Ourti, T.; Walsh, B. Conindex: Estimation of concentration indices. Stata J. 2016, 16, 112–138. [Google Scholar] [CrossRef] [PubMed]
- Prevalence and Determinants of Contraceptive Use among Employed and Unemployed Women in Bangladesh—PMC. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5187648/ (accessed on 3 August 2023).
- Abbas, S.; Isaac, N.; Zia, M.; Zakar, R.; Fischer, F. Determinants of women’s empowerment in Pakistan: Evidence from Demographic and Health Surveys, 2012–2013 and 2017–2018. BMC Public Health 2021, 21, 1328. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Alvites, A.L.; Yrala-Castillo, G.; Al-Kassab-Córdova, A.; Munayco, C.V. Associated factors, inequalities, and spatial distribution of the use of modern contraceptive methods among women of reproductive age in Peru: A population-based cross-sectional study. BMC Public Health 2022, 22, 2267. [Google Scholar] [CrossRef]
- Reglamento Para Regular el Acceso de Metodos Anticonceptivos. Available online: https://www.controlsanitario.gob.ec/wp-content/uploads/downloads/2019/01/Acuerdo-Ministerial-2490.pdf (accessed on 7 July 2023).
- Adebowale, S.A.; Adeoye, I.A.; Palamuleni, M.E. Contraceptive use among Nigerian women with no fertility intention: Interaction amid potential causative factors. Afr. Popul. Stud. 2013, 27, 127–139. [Google Scholar] [CrossRef]
- Apanga, P.A.; Kumbeni, M.T.; Ayamga, E.A.; Ulanja, M.B.; Akparibo, R. Prevalence and Factors Associated with Modern Contraceptive Use among Women of Reproductive Age in 20 African Countries: A Large Population-Based study. BMJ Open 2020, 10, e041103. [Google Scholar] [CrossRef]
- Forty, J.; Rakgoasi, S.D.; Keetile, M. Patterns and determinants of modern contraceptive use and intention to usecontraceptives among Malawian women of reproductive ages (15–49 years). Contracept. Reprod. Med. 2021, 6, 21. [Google Scholar] [CrossRef]
- De Vargas Nunes Coll, C.; Ewerling, F.; Hellwig, F.; de Barros, A.J.D. Contraception in adolescence: The influence of parity and marital status on contraceptive use in 73 low-and middle-income countries. Reprod. Health 2019, 16, 21. [Google Scholar] [CrossRef] [PubMed]
- Salgado, J.Q.; Márquez, V.S. El tipo de unión y el aborto: Una comparación generacional para México. Estud. Demográficos Y Urbanos 2004, 19, 377–412. [Google Scholar] [CrossRef][Green Version]
- Afriyie, P.; Tarkang, E.E. Factors influencing use of modern contraception among married women in Ho West district, Ghana: Descriptive cross-sectional study. Pan Afr. Med. J. 2019, 33, 15. [Google Scholar] [CrossRef] [PubMed]
- Aspilcueta-Gho, D. Rol del Varón en la Anticoncepción, Como Usuario y Como Pareja. Rev. Peru. Med. Exp. Salud Publica 2013, 30, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Ecuador. United States Department of State. Available online: https://www.state.gov/reports/2020-report-on-international-religious-freedom/ecuador/ (accessed on 30 June 2023).
- Eduardo Durán, F.E. Factores Asociados al Uso de Métodos Anticonceptivos Modernos en Mujeres y Hombres Bolivia 2003–2008. Rev. Cienc. Tecnol. E Innov. 2020, 18, 11–42. [Google Scholar]
- Instituto Nacional de las Mujeres Breve. Análisis de la Situación de Salud Reproductiva de Mujeres de Habla Indígena y no Indígena. Available online: http://cedoc.inmujeres.gob.mx/documentos_download/101214.pdf (accessed on 16 July 2022).
- Sánchez-Retana, C.; Leiva-Granados, R. Factores Incidentes en el Uso de Métodos Anticonceptivos en la Población Adolescente y Adulta Joven en Costa Rica. Poblac. Salud En Mesoamérica. [CrossRef]
- Meléndez-Asipali, J.A.; Espinoza, R.; Rivadeneyra-Romero, R.; Vela-Ruiz, J.M.; De La Cruz-Vargas, J.A.; Meléndez-Asipali, J.A.; Espinoza, R.; Rivadeneyra-Romero, R.; Vela-Ruiz, J.M.; De La Cruz-Vargas, J.A. Factores asociados al uso de métodos anticonceptivos en mujeres en edad fértil de 15 a 49 años según encuesta demográfica en Perú. Rev. Cuerpo Méd. Hosp. Nac. Almanzor Aguinaga Asenjo 2022, 15, 180–184. [Google Scholar] [CrossRef]
- Islam, K.; Haque, R.; Hema, P.S. Regional Variations of Contraceptive Use in Bangladesh: A Disaggregate Analysis by Place of Residence. PLoS ONE 2020, 15, e0230143. [Google Scholar] [CrossRef]
- Allen-Leigh, B.; Villalobos-Hernández, A.; Hernández-Serrato, M.I. Inicio de vida sexual, uso de anticonceptivos y planificación familiar en mujeres adolescentes y adultas en México. Salud Pública México 2013, 55, 235. [Google Scholar] [CrossRef]
- Keogh, S.C.; Otupiri, E.; Castillo, P.W.; Chiu, D.W.; Polis, C.B.; Nakua, E.K.; Bell, S.O. Hormonal contraceptive use in Ghana: The role of method attributes and side effects in method choice and continuation. Contraception 2021, 104, 235–245. [Google Scholar] [CrossRef]
- Ross, J.A. Contraceptive Use, Access to Methods, and Program Efforts in Urban Areas. Front. Glob. Women’s Health 2021, 2, 636581. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística e Informática. Capítulo 4: Planificación Familiar. 2021. Available online: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1838/pdf/cap004.pdf (accessed on 16 July 2022).
- Ministerio de Salud Pública. Plan Nacional de Salud Sexual y Salud Reproductiva 2017–2021. Available online: https://ecuador.unfpa.org/sites/default/files/pub-pdf/PLAN%20NACIONAL%20DE%20SS%20Y%20SR%202017-2021.pdf (accessed on 2 July 2022).
| Characteristics | n | % * |
|---|---|---|
| Age group (years) | ||
| 15–19 | 934 | 3.9 |
| 20–29 | 6731 | 29.4 |
| 30–39 | 7261 | 40.1 |
| 40–49 | 4180 | 26.6 |
| Educational level | ||
| Up to primary | 6390 | 33.7 |
| Secondary | 8801 | 44.9 |
| Higher | 3915 | 21.4 |
| Marital status | ||
| Married | 8815 | 47.3 |
| Cohabitant | 10,291 | 52.7 |
| Currently working | ||
| No | 10,135 | 51.5 |
| Yes | 8971 | 48.5 |
| Parity | ||
| 0–1 | 4905 | 24.5 |
| 2 | 5914 | 31.3 |
| 3 or more | 8287 | 44.2 |
| Ethnicity | ||
| Indigenous | 2127 | 6.6 |
| Non-indigenous | 16,979 | 93.4 |
| Health insurance | ||
| Yes | 5442 | 31.3 |
| No | 13,664 | 68.7 |
| Wealth quintile | ||
| Very poor | 3984 | 16.2 |
| Poor | 4128 | 20.5 |
| Medium | 4102 | 21.2 |
| Rich | 3772 | 21.5 |
| Very rich | 3120 | 20.6 |
| Area of residence | ||
| Rural | 7144 | 30.1 |
| Urban | 11,962 | 69.9 |
| Region of residence | ||
| Highlands | 7216 | 43.5 |
| Coast | 7285 | 51.1 |
| Amazon | 3908 | 5.2 |
| Island | 697 | 0.2 |
| Characteristics | MCM | p Value * | |
|---|---|---|---|
| No (n = 1389) | Yes (n = 17,717) | ||
| % (95% CI) | % (95% CI) | ||
| Overall | 7.2 (6.6–7.9) | 92.8 (92.1–93.4) | |
| Age group (years) | |||
| 15–19 | 2.2 (1.3–3.8) | 4.0 (3.6–4.4) | 0.131 |
| 20–29 | 27.8 (24.2–31.6) | 29.5 (28.4–30.7) | |
| 30–39 | 40.6 (36.1–45.3) | 40.1 (38.8–41.4) | |
| 40–49 | 29.4 (25.0–34.2) | 26.4 (25.2–27.6) | |
| Educational level | |||
| Up to primary | 26.3 (22.4–30.7) | 34.3 (32.8–35.8) | <0.001 |
| Secondary | 43.3 (38.8–47.8) | 45.0 (43.5–46.5) | |
| Higher | 30.4 (26.1–35.1) | 20.7 (19.5–22.0) | |
| Marital status | |||
| Married | 55.5 (50.6–60.3) | 46.7 (45.2–48.1) | 0.001 |
| Cohabitant | 44.5 (39.7–49.4) | 53.3 (51.9–54.8) | |
| Currently working | |||
| No | 38.6 (34.2–43.2) | 52.5 (51.1–54.0) | <0.001 |
| Yes | 61.4 (56.8–65.8) | 47.5 (46.0–48.9) | |
| Parity | |||
| 0–1 | 35.9 (31.3–40.8) | 23.6 (22.6–24.7) | <0.001 |
| 2 | 34.6 (30.4–39.0) | 31.0 (29.9–32.2) | |
| 3 or more | 29.5 (25.6–33.8) | 45.3 (44.1–46.6) | |
| Ethnicity | |||
| Indigenous | 11.1 (8.2–14.8) | 6.2 (5.6–6.9) | <0.001 |
| Non-indigenous | 88.9 (85.2–91.8) | 93.8 (93.1–94.4) | |
| Health insurance | |||
| Yes | 36.1 (31.6–40.8) | 30.9 (29.5–32.4) | 0.027 |
| No | 63.9 (59.2–68.4) | 69.1 (67.6–70.5) | |
| Wealth quintile | |||
| Very poor | 12.3 (9.8–15.3) | 16.5 (15.4–17.7) | <0.001 |
| Poor | 16.2 (13.0–20.0) | 20.8 (19.7–22.0) | |
| Medium | 20.3 (17.1–23.9) | 21.3 (20.1–22.5) | |
| Rich | 32.1 (27.6–37.0) | 20.7 (19.5–21.9) | |
| Very rich | 19.1 (15.8–23.0) | 20.7 (19.2–22.3) | |
| Area of residence | |||
| Rural | 22.6 (19.6–26.0) | 30.7 (29.4–32.0) | <0.001 |
| Urban | 77.4 (74.0–80.4) | 69.3 (68.0–70.6) | |
| Region of residence | |||
| Highlands | 43 (38.2–47.8) | 43.5 (41.9–45.2) | 0.667 |
| Coast | 51.1 (46.4–55.9) | 51.1 (49.5–52.7) | |
| Amazon | 5.6 (4.7–6.6) | 5.2 (4.9–5.5) | |
| Island | 0.3 (0.3–0.4) | 0.2 (0.2–0.2) | |
| Characteristics | MCM | |||
|---|---|---|---|---|
| ECI | SE | p Value * | p Value across Categories ** | |
| Overall | −0.02393248 | 0.00707563 | 0.0007 | |
| Age groups (years) | ||||
| 15–19 | −0.01827511 | 0.02435466 | 0.453 | 0.027 |
| 20–29 | −0.02732495 | 0.01230476 | 0.027 | |
| 30–39 | −0.01934179 | 0.01065013 | 0.070 | |
| 40–49 | −0.0146222 | 0.01381501 | 0.290 | |
| Educational level | ||||
| Up to primary | −0.01697803 | 0.01093103 | 0.121 | 0.0514 |
| Secondary | −0.01367809 | 0.01017993 | 0.179 | |
| Higher | 0.05022723 | 0.01725384 | 0.004 | |
| Currently working | ||||
| No | −0.02500584 | 0.00858693 | 0.004 | 0.0769 |
| Yes | 0.00051558 | 0.0115945 | 0.965 | |
| Ethnicity | ||||
| Indigenous | 0.01719356 | 0.03613912 | 0.634 | 0.1899 |
| Non indigenous | −0.03107635 | 0.00706549 | <0.001 | |
| Area of residence | ||||
| Rural | −0.00125461 | 0.00936669 | 0.8935 | 0.258 |
| Urban | −0.01627268 | 0.00940888 | 0.084 | |
| Characteristics | Crude Model | Adjusted Model * | ||
|---|---|---|---|---|
| PR (95% CI) | p Value | aPR (95% CI) | p Value | |
| Age group (years) | ||||
| 15–19 | Reference | Reference | ||
| 20–29 | 0.97 (0.95–1.00) | 0.028 | 0.96 (0.93–0.99) | 0.003 |
| 30–39 | 0.97 (0.94–0.99) | 0.012 | 0.93 (0.89–0.96) | <0.001 |
| 40–49 | 0.96 (0.93–0.99) | 0.004 | 0.91 (0.88–0.95) | <0.001 |
| Educational level | ||||
| Up to primary | Reference | Reference | ||
| Secondary | 0.99 (0.97–1.00) | 0.053 | 1.00 (0.98–1.01) | 0.707 |
| Higher | 0.95 (0.93–0.97) | <0.001 | 0.98 (0.95–1.01) | 0.116 |
| Marital status | ||||
| Married | Reference | Reference | ||
| Cohabitant | 1.03 (1.01–1.04) | 0.001 | 1.02 (1.00–1.04) | 0.027 |
| Currently working | ||||
| No | Reference | Reference | ||
| Yes | 0.96 (0.95–0.97) | <0.001 | 0.97 (0.96–0.99) | <0.001 |
| Parity | ||||
| 0–1 | Reference | Reference | ||
| 2 | 1.03 (1.01–1.05) | 0.011 | 1.05 (1.02–1.08) | <0.001 |
| 3 or more | 1.06 (1.04–1.09) | <0.001 | 1.10 (1.07–1.13) | <0.001 |
| Ethnicity | ||||
| Indigenous | Reference | Reference | ||
| Non-indigenous | 1.06 (1.02–1.10) | 0.002 | 1.07 (1.03–1.12) | 0.001 |
| Health insurance | ||||
| Yes | Reference | Reference | ||
| No | 1.02 (1.00–1.03) | 0.036 | 1.00 (0.98–1.02) | 0.838 |
| Wealth quintile | ||||
| Very poor | Reference | Reference | ||
| Poor | 1.00 (0.98–1.02) | 0.785 | 1.01 (0.99–1.03) | 0.513 |
| Medium | 0.98 (0.97–1.00) | 0.112 | 1.01 (0.98–1.03) | 0.617 |
| Rich | 0.94 (0.92–0.97) | <0.001 | 0.97 (0.95–1.00) | 0.054 |
| Very rich | 0.99 (0.97–1.01) | 0.192 | 1.03 (1.00–1.06) | 0.036 |
| Area of residence | ||||
| Rural | Reference | Reference | ||
| Urban | 0.97 (0.96–0.99) | <0.001 | 0.98 (0.97–0.99) | 0.006 |
| Region of residence | ||||
| Highlands | Reference | Reference | ||
| Coast | 1.00 (0.98–1.01) | 0.888 | 0.98 (0.96–0.99) | 0.034 |
| Amazon | 0.99 (0.98–1.01) | 0.438 | 0.99 (0.97–1.01) | 0.207 |
| Island | 0.96 (0.94–0.99) | 0.010 | 0.98 (0.95–1.00) | 0.094 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Callata-Cardenas, S.; Peña-Cerna, F.M.d.R.; Hernández-Vásquez, A.; Azañedo, D. Socioeconomic Inequalities and Factors Associated with the Use of Modern Contraceptive Methods in Women of Childbearing Age in Ecuador, 2018. Healthcare 2023, 11, 2293. https://doi.org/10.3390/healthcare11162293
Callata-Cardenas S, Peña-Cerna FMdR, Hernández-Vásquez A, Azañedo D. Socioeconomic Inequalities and Factors Associated with the Use of Modern Contraceptive Methods in Women of Childbearing Age in Ecuador, 2018. Healthcare. 2023; 11(16):2293. https://doi.org/10.3390/healthcare11162293
Chicago/Turabian StyleCallata-Cardenas, Sandra, Fátima Milagros del Rosario Peña-Cerna, Akram Hernández-Vásquez, and Diego Azañedo. 2023. "Socioeconomic Inequalities and Factors Associated with the Use of Modern Contraceptive Methods in Women of Childbearing Age in Ecuador, 2018" Healthcare 11, no. 16: 2293. https://doi.org/10.3390/healthcare11162293
APA StyleCallata-Cardenas, S., Peña-Cerna, F. M. d. R., Hernández-Vásquez, A., & Azañedo, D. (2023). Socioeconomic Inequalities and Factors Associated with the Use of Modern Contraceptive Methods in Women of Childbearing Age in Ecuador, 2018. Healthcare, 11(16), 2293. https://doi.org/10.3390/healthcare11162293








