Digitalization in Urology—A Multimethod Study of the Relationships between Physicians’ Technostress, Burnout, Work Engagement and Job Satisfaction
Abstract
1. Background
2. Introduction
2.1. Digitalization in Medicine
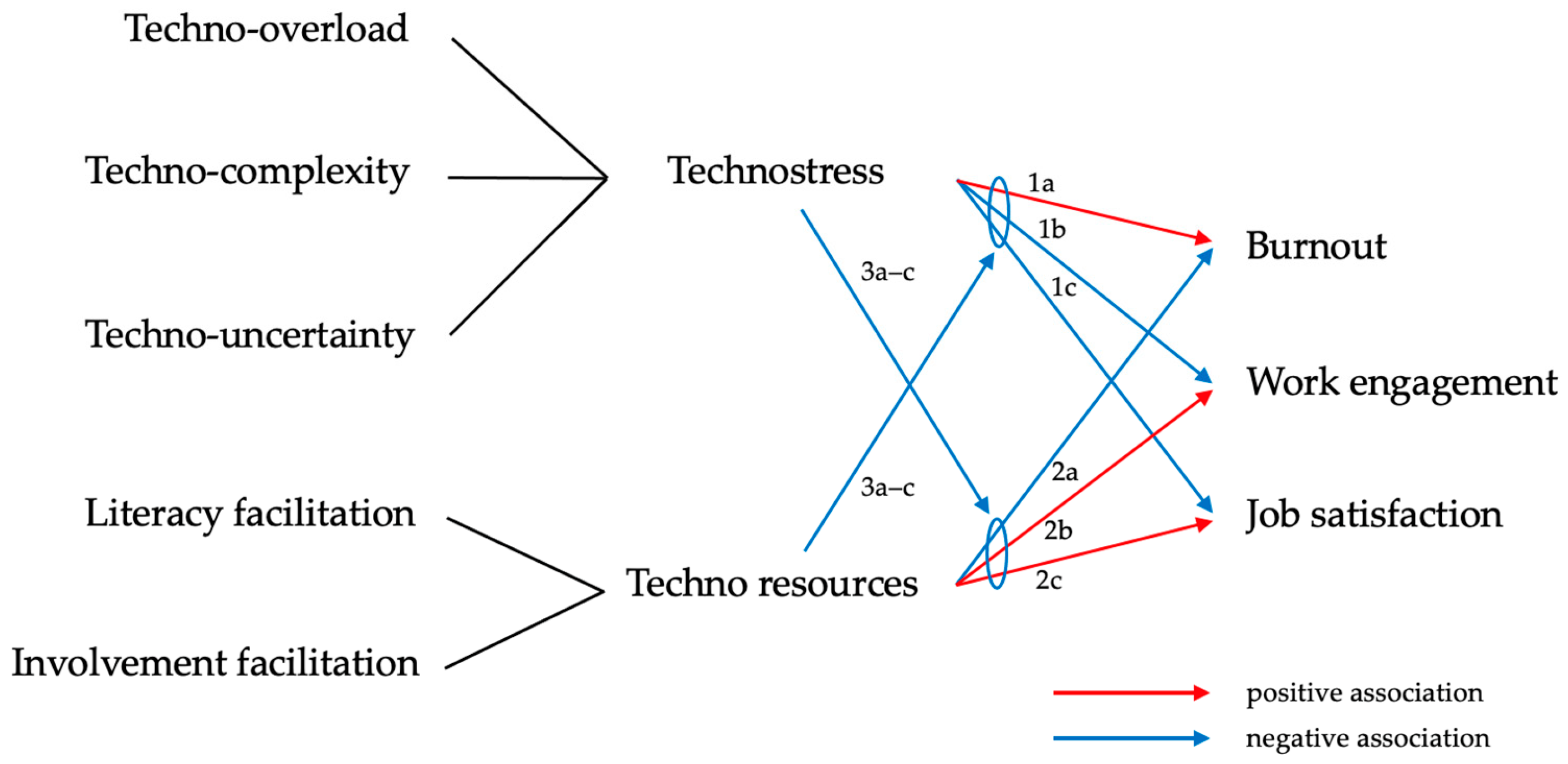
2.2. Theoretical Background and Literature Review
2.2.1. Technostress
- Techno-overload: ICT forces employees to work faster and longer [16];
- Techno-complexity: the complexity of the ICT used in companies forces users to spend a lot of time learning new technical skills [17];
- Techno-insecurity: employees fear for their jobs and experience stress due to the possibility of being replaced by ICT or other employees with better technical skills [18];
- Techno-uncertainty: employees lose confidence in their technical skills and experience stress due to constant changes and updates or the use of new technologies [16];
- Techno-invasion (techno-omnipresence): ICT “invades” the private lives of users, as users are always available everywhere [13].
2.2.2. The Job Demands–Resources Model (JD–R Model)
2.2.3. Burnout, Work Engagement and Job Satisfaction in Urology
2.3. Objectives
3. Materials and Methods
3.1. Study Design, Participant Selection and Data Collection
3.2. Variables and Measurement
3.2.1. Sociodemographic and Workplace Variables
3.2.2. ICT Use and Perceived Usefulness
3.2.3. Technostress Creators and Inhibitors
3.2.4. Burnout
3.2.5. Work Engagement and Job Satisfaction
3.2.6. Institutional Support Offers
3.3. Data Analysis
4. Results
4.1. Sociodemographic and Occupational Characteristics of the Study Participants
4.2. Descriptive Statistics
4.3. Associations between Technostress and the Outcomes Burnout, Work Engagement and Job Satisfaction
4.4. Free-Text Answer Analysis about (Dis)Advantages of ICT and Institutional Support Offers
“You have almost all the medical reports and info available on any PC anywhere in the hospital 24/7.”
“Prescribing medication and requesting nursing services, as well as documenting patient care takes about 3x as long as on paper.”
“When implemented correctly, digitization is a blessing and definitely the future. For us, this blessing is mainly called crashes and waiting times (hourglass) and is therefore more of a curse. If the software and hardware are not powerful enough, digitization is a step backwards in efficiency and regularly causes frustration.”
“Things are moving too slowly. We need better digital applications and interconnections between sectors fast.”
“There are no offers for stress reduction, it was not allowed to actually take part in the in-house exercise training during breaks.”
“1 × 15 min shoulder massage in physiotherapy due to the stress caused by the Corona pandemic; also, corporate benefits for visiting a public indoor swimming pool”
“Better hospital management, better resource management, less influence by hospital economists.”
“More competent staff in IT so that improvements are actually implemented.”
“I do not take advantage of ‘relief opportunities’ that may be offered by the employer. Partnership, friendships, spirituality, nature and exercise are essential for me.”
“Adequate workplace equipment, back-friendly seating/desk chairs, height-adjustable desk, functioning IT that is also practicable and does not constantly hang up or take forever to load; providing a second monitor etc.”
“The main problem is the lack of staff. For us, it’s more in the nursing environment. If there was more time to explain things, some things would be easier. I am much more stressed because I always must ‘iron out’ frustration and inexperience etc. among the nursing staff and residents.”
“The offer that administrative tasks coding, discharge management, surgery planning, bed planning) are taken on by other persons (physician assistant). In terms of responsibilities, more and more tasks are labelled ‘medical’ activities. This leaves little time for practicing medicine. This is compensated by working faster. We therefore no longer speak of overtime, but of ‘work density’/hour.”
“More real involvement in the development of (IT) processes that massively influence the workflow. Especially in IT, minimal changes can only ever be enforced by the group of end users (doctors, nursing) at the end of the implementation processes. Here, an earlier involvement of the users in the decision-making processes must take place.”
5. Discussion
5.1. Key Results
5.2. Strengths and Limitations
- Since urology is an operative specialty, their main workplace is the operating room rather than at a PC in an office.
- E-mails often do not get through spam filters due to increased security measures.
- In addition to the already high workload among physicians, staff shortages have become even more acute as a result of the COVID-19 pandemic in 2022. Thus, it only seems reasonable to prioritize patient care tasks above participation in an online survey.
- E-mail is not necessarily the main communication channel in many clinical teams and therefore e-mails may not be read.
- Chief physicians and secretaries did not forward the survey link, either due to lack of interest in the topic or to avoid further burdening the physicians in their team.
5.3. Implications for Research
5.4. Practical Implications
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Neuhaus, A.; Lechleiter, P.; Sonntag, K. Meausres and Recommendations for Healthy Work Practices of Tomorrow (MEgA). Available online: https://gesundearbeit-mega.de/sites/gesundearbeit-mega.de/files/u29/literaturreview.pdf (accessed on 23 March 2023).
- Mache, S.; Harth, V. Digital transformation in the world of work and mental health. Zbl. Arbeitsmed 2019, 70, 180–184. [Google Scholar] [CrossRef]
- Nohl-Deryk, P.; Brinkmann, J.K.; Gerlach, F.M.; Schreyögg, J.; Achelrod, D. Barriers to digitalisation of healthcare in Germany: A survey of experts. Gesundheitswesen 2018, 80, 939–945. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.-H.; Chen, Y.-C.; Greenes, R.A. Healthcare technology management competency and its impacts on IT–healthcare partnerships development. Int. J. Med. Inf. 2009, 78, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Sensmeier, J. Transforming nursing practice through technology and informatics. J. Nurs. Manag. 2011, 42, 20–23. [Google Scholar] [CrossRef]
- Gastaldi, L.; Corso, M. Smart healthcare digitalization: Using ICT to effectively balance exploration and exploitation within hospitals. Int. J. Eng. Bus. Manag. 2012, 4, 9. [Google Scholar] [CrossRef]
- Neumann, K. Roland Berger. Available online: https://www.rolandberger.com/de/Insights/Publications/Digitalisierung-im-Gesundheitswesen-Handeln-statt-sondieren.html (accessed on 23 March 2023).
- Venkatramani, V. Urovision 2020: The future of urology. Indian J. Urol. 2015, 31, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Loch, T.; Witzsch, U.; Reis, G. Digital transformation in urology-opportunity, risk or necessity? Urol. A 2021, 60, 1125–1140. [Google Scholar] [CrossRef]
- Bernstein, D.E.; Bernstein, B.S. Urological technology: Where will we be in 20 years’ time? Ther. Adv. Urol. 2018, 10, 235–242. [Google Scholar] [CrossRef]
- Brod, C. Managing technostress: Optimizing the use of computer technology. Pers. J. 1982, 61, 753–757. [Google Scholar]
- Struck, J.; Stahl, L.; Braun, M.; Homberg, R.; Schönberger, M.; Westphal, J.; Salem, J. The working time load of specialists and senior physicians in German urology—A critical assessment. Urol. A 2019, 58, 918–923. [Google Scholar] [CrossRef]
- Ragu-Nathan, T.; Tarafdar, M.; Ragu-Nathan, B.S.; Tu, Q. The consequences of technostress for end users in organizations: Conceptual development and empirical validation. Inf. Syst. Res. 2008, 19, 417–433. [Google Scholar] [CrossRef]
- Zuboff, S. In the Age of the Smart Machine; Butterworth-Heinemann: Oxford, UK, 1988. [Google Scholar]
- Tarafdar, M.; Cooper, C.L.; Stich, J.F. The technostress trifecta–techno eustress, techno distress and design. Inf. Syst. J. 2019, 29, 6–42. [Google Scholar] [CrossRef]
- Fuglseth, A.M.; Sørebø, Ø. The effects of technostress within the context of employee use of ICT. Comput. Hum. Behav. 2014, 40, 161–170. [Google Scholar] [CrossRef]
- Raišienė, A.G.; Jonušauskas, S. Silent issues of ICT era: Impact of techno-stress to the work and life balance of employees. Entrep. Sustain. Issues 2013, 1, 108–115. [Google Scholar] [CrossRef]
- Ahmad, U.N.U.; Amin, S.M.; Ismail, W.K.W. Moderating effect of technostress inhibitors on the relationship between technostress creators and organisational commitment. J. Teknol. 2014, 67, 51–62. [Google Scholar] [CrossRef]
- Bondanini, G.; Giorgi, G.; Ariza-Montes, A.; Vega-Muñoz, A.; Andreucci-Annunziata, P. Technostress Dark Side of Technology in the Workplace: A Scientometric Analysis. Int. J. Environ. Res. Public Health 2020, 17, 8013. [Google Scholar] [CrossRef] [PubMed]
- Al-Ansari, M.A.; Alshare, K. The impact of technostress components on the employees satisfaction and perceived performance: The case of Qatar. JGIM 2019, 27, 65–86. [Google Scholar] [CrossRef]
- Dragano, N.; Lunau, T. Technostress at work and mental health: Concepts and research results. Curr. Opin Psychiatry 2020, 33, 407–413. [Google Scholar] [CrossRef]
- Stadin, M.; Nordin, M.; Fransson, E.I.; Broström, A. Healthcare managers’ experiences of technostress and the actions they take to handle it—A critical incident analysis. BMC Med. Inf. Decis. Mak. 2020, 20, 244. [Google Scholar] [CrossRef]
- Hummert, H.; Traum, A.; Görs, P.K.; Nerdinger, F.W. Wirkungen der Digitalisierung von Arbeit auf Mitarbeiter/innen in Dienstleistungsunternehmen. Habilitationsschrift. Universität Rostock. Rostock. Beiträge Wirtsch. Organ. 2019, 20, 1–39. [Google Scholar] [CrossRef]
- Nelson, D.L. Individual adjustment to information-driven technologies: A critical review. MIS Q. 1990, 1, 79–98. [Google Scholar] [CrossRef]
- Gaudioso, F.; Turel, O.; Galimberti, C. Explaining work exhaustion from a coping theory perspective: Roles of techno-stressors and technology-specific coping strategies. Stud. Health Technol. Inf. 2015, 219, 14–20. [Google Scholar] [CrossRef]
- Ter Hoeven, C.L.; Van Zoonen, W. Flexible work designs and employee well-being: Examining the effects of resources and demands. New Technol. Work. Employ. 2015, 30, 237–255. [Google Scholar] [CrossRef]
- Brown, R.; Duck, J.; Jimmieson, N. E-mail in the workplace: The role of stress appraisals and normative response pressure in the relationship between e-mail stressors and employee strain. Int. J. Stress Manag. 2014, 21, 325–347. [Google Scholar] [CrossRef]
- Park, J.-C.; Kim, S.; Lee, H. Effect of work-related smartphone use after work on job burnout: Moderating effect of social support and organizational politics. Comput. Hum. Behav. 2020, 105, 106194. [Google Scholar] [CrossRef]
- Salanova, M.; Llorens, S.; Cifre, E. The dark side of technologies: Technostress among users of information and communication technologies. Int. J. Psychol. 2013, 48, 422–436. [Google Scholar] [CrossRef] [PubMed]
- Porter, G.; Kakabadse, N.K. HRM perspectives on addiction to technology and work. J. Manag. Dev. 2006, 25, 535–560. [Google Scholar] [CrossRef]
- Mark, G.; Gudith, D.; Klocke, U. The cost of interrupted work: More speed and stress. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, Florence, Italy, 5–10 April 2008; pp. 107–110. [Google Scholar]
- Kroth, P.J.; Morioka-Douglas, N.; Veres, S.; Babbott, S.; Poplau, S.; Qeadan, F.; Parshall, C.; Corrigan, K.; Linzer, M. Association of electronic health record design and use factors with clinician stress and burnout. JAMA Netw. Open 2019, 2, 199609. [Google Scholar] [CrossRef] [PubMed]
- Arndt, B.G.; Beasley, J.W.; Watkinson, M.D.; Temte, J.L.; Tuan, W.-J.; Sinsky, C.A.; Gilchrist, V.J. Tethered to the EHR: Primary care physician workload assessment using EHR event log data and time-motion observations. Ann. Fam. Med. 2017, 15, 419–426. [Google Scholar] [CrossRef]
- Heponiemi, T.; Hyppönen, H.; Vehko, T.; Kujala, S.; Aalto, A.-M.; Vänskä, J.; Elovainio, M. Finnish physicians’ stress related to information systems keeps increasing: A longitudinal three-wave survey study. BMC Med. Inf. Decis. Mak. 2017, 17, 147. [Google Scholar] [CrossRef]
- Janols, R.; Gôrranson, B.; Sandblad, B.L. Three Key Concerns for a Successful EPR Deployment and Usage. Stud. Health Technol. Inf. 2011, 169, 260–264. [Google Scholar] [CrossRef]
- Thomas Craig, K.J.; Willis, V.C.; Gruen, D.; Rhee, K.; Jackson, G.P. The burden of the digital environment: A systematic review on organization-directed workplace interventions to mitigate physician burnout. J. Am. Med. Inf. Assoc. 2021, 28, 985–997. [Google Scholar] [CrossRef]
- Golz, C.; Peter, K.A.; Zwakhalen, S.M.; Hahn, S. Technostress Among Health Professionals–A Multilevel Model and Group Comparisons between Settings and Professions. Inf. Health Soc. Care 2021, 46, 136–147. [Google Scholar] [CrossRef]
- Thiel, R.; Deimel, L.; Schmidtmann, D.; Piesche, K.; Hüsing, T.; Rennoch, J.; Stroetmann, V.; Stroetmann, K. Bertelsmann Stiftung. Available online: https://www.bertelsmann-stiftung.de/de/publikationen/publikation/did/smarthealthsystems-1 (accessed on 23 March 2023).
- Virone, C.; Kremer, L.; Breil, B. Which Factors of Digitisation Bias the Work-Related Stress of Healthcare Employees? A Systematic Review. Stud. Health Technol. Inf. 2021, 281, 916–920. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. The job demands-resources model: State of the art. J. Manag. Psychol. 2007, 22, 309–328. [Google Scholar] [CrossRef]
- Demerouti, E. Job Demands-Resources Theory: Taking Stock and Looking Forward. J. Occup. Health Psychol. 2016, 22, 273–285. [Google Scholar] [CrossRef]
- Chênevert, D.; Kilroy, S.; Johnson, K.; Fournier, P.-L. The determinants of burnout and professional turnover intentions among Canadian physicians: Application of the job demands-resources model. BMC Health Serv. Res 2021, 21, 993. [Google Scholar] [CrossRef] [PubMed]
- Krämer, T.; Schneider, A.; Spieß, E.; Angerer, P.; Weigl, M. Associations between job demands, work-related strain and perceived quality of care: A longitudinal study among hospital physicians. Int. J. Qual. Health Care 2016, 28, 824–829. [Google Scholar] [CrossRef]
- Zhang, S.; Shi, Y.; Liu, B.; Wang, H.; Zhao, X.; Wang, X.; Sun, T. Job demands and resources and their relationship with satisfaction and thriving at work in a sample of Chinese doctors: A cross-sectional study. BMJ Open 2021, 11, e045745. [Google Scholar] [CrossRef]
- Scheepers, R.; Silkens, M.; van den Berg, J.; Lombarts, K. Associations between job demands, job resources and patient-related burnout among physicians: Results from a multicentre observational study. BMJ Open 2020, 10, e038466. [Google Scholar] [CrossRef]
- Pastores, S.M.; Kvetan, V.; Coopersmith, C.M.; Farmer, J.C.; Sessler, C.; Christman, J.W.; D’Agostino, R.; Diaz-Gomez, J.; Gregg, S.R.; Khan, R.A. Workforce, workload, and burnout among intensivists and advanced practice providers: A narrative review. Crit. Care Med. 2019, 47, 550–557. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician burnout: Contributors, consequences and solutions. J. Intern. Med. 2018, 283, 516–529. [Google Scholar] [CrossRef] [PubMed]
- Gluschkoff, K.; Hakanen, J.; Elovainio, M.; Vänskä, J.; Heponiemi, T. The relative importance of work-related psychosocial factors in physician burnout. Occup. Med. 2022, 72, 28–33. [Google Scholar] [CrossRef] [PubMed]
- International Statistical Classification of Diseases and Related Health Problems (11th ed.). Available online: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281 (accessed on 14 March 2023).
- Shoureshi, P.; Guerre, M.; Seideman, C.A.; Callejas, D.G.; Amling, C.L.; Bassale, S.; Chouhan, J.D. Addressing Burnout in Urology: A Qualitative Assessment of Interventions. Urol. Pract. 2022, 9, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.W.; Wagner, H.; Hernandez, B.C.; Hu, B.R.; Ko, E.Y.; Ruckle, H.C. Stressors and coping mechanisms related to burnout within urology. Urology 2020, 139, 27–36. [Google Scholar] [CrossRef]
- Beschoner, P.; Limbrecht-Ecklundt, K.; Jerg-Bretzke, L. Mental health among physicians: Burnout, depression, anxiety and substance abuse in the occupational context. Nervenarzt 2019, 90, 961–974. [Google Scholar] [CrossRef]
- Nauheim, J.; North, A.C. An Updated Review on Physician Burnout in Urology. Urol. Clin. N. Am. 2021, 48, 173–178. [Google Scholar] [CrossRef]
- Böhle, A.; Baumgärtel, M.; Götz, M.L.; Müller, E.H.; Jocham, D. Burn-out of urologists in the county of Schleswig-Holstein, Germany: A comparison of hospital and private practice urologists. J. Urol. 2001, 165, 1158–1161. [Google Scholar] [CrossRef]
- Marchalik, D.; Brems, J.; Rodriguez, A.; Lynch, J.H.; Padmore, J.; Stamatakis, L.; Krasnow, R. The Impact of Institutional Factors on Physician Burnout: A National Study of Urology Trainees. Urology 2019, 131, 27–35. [Google Scholar] [CrossRef]
- Rodríguez-Socarrás, M.; Kingo, P.S.; Uvin, P.; Østergren, P.; Patruno, G.; Edison, E.; Kasivisvanathan, V.; Vásquez, J.L.; Esperto, F.; Rivas, J.G. Lifestyle among urology trainees and young urologist in the context of burn-out syndrome. Actas Urológicas Españolas 2020, 44, 19–26. [Google Scholar] [CrossRef]
- Fainberg, J.; Lee, R.K. What Is Underlying Resident Burnout in Urology and What Can Be Done to Address this? Curr. Urol. Rep. 2019, 20, 62. [Google Scholar] [CrossRef]
- Panagioti, M.; Panagopoulou, E.; Bower, P.; Lewith, G.; Kontopantelis, E.; Chew-Graham, C.; Dawson, S.; Van Marwijk, H.; Geraghty, K.; Esmail, A. Controlled interventions to reduce burnout in physicians: A systematic review and meta-analysis. JAMA Intern. Med. 2017, 177, 195–205. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Bakker, A.B. Defining and measuring work engagement: Bringing clarity to the concept. In Work Engagement: A Handbook of Essential Theory and Research; Bakker, A.B., Leitner, M.P., Eds.; Psychology Press: New York, NY, USA, 2010; Volume 12, pp. 10–24. [Google Scholar]
- García-Iglesias, J.J.; Gómez-Salgado, J.; Fagundo-Rivera, J.; Romero-Martín, M.; Ortega-Moreno, M.; Navarro-Abal, Y. Predictive factors for burnout and work engagement levels among doctors and nurses: A systematic review. Rev. Española Salud Pública 2021, 95, e202104046. [Google Scholar]
- Höge, T.; Schnell, T. Kein Arbeitsengagement ohne Sinnerfüllung. Eine Studie zum Zusammenhang von Work Engagement, Sinnerfüllung und Tätigkeitsmerkmalen. Wirtschaftspsychologie 2012, 1, 91–99. [Google Scholar]
- Mache, S.; Vitzthum, K.; Klapp, B.F.; Danzer, G. Surgeons’ work engagement: Influencing factors and relations to job and life satisfaction. Surgeon 2014, 12, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Debets, M.; Scheepers, R.; Silkens, M.; Lombarts, K. Structural equation modelling analysis on relationships of job demands and resources with work engagement, burnout and work ability: An observational study among physicians in Dutch hospitals. BMJ Open 2022, 12, e062603. [Google Scholar] [CrossRef] [PubMed]
- Van Bogaert, P.; Clarke, S.; Willems, R.; Mondelaers, M. Staff engagement as a target for managing work environments in psychiatric hospitals: Implications for workforce stability and quality of care. J. Clin. Nurs. 2013, 22, 1717–1728. [Google Scholar] [CrossRef] [PubMed]
- Locke, E.A. What is job satisfaction? Organ. Behav. Hum. Perform. 1969, 4, 309–336. [Google Scholar] [CrossRef]
- Rosta, J.; Gerber, A. Job satisfaction of hospital doctors. Results of a study of a national sample of hospital doctors in Germany. Gesundheitswesen 2008, 70, 519–524. [Google Scholar] [CrossRef]
- Himmler, M.; Schultz-Lampel, D.; Hellmis, E.; Kowalewski, K.F.; Michel, M.S.; Weinberger, S. Analysis of the impact of increasing feminization in the healthcare system on urology. Urologie 2022, 61, 1083–1092. [Google Scholar] [CrossRef]
- Laubach, W.; Fischbeck, S. Job satisfaction and the work situation of physicians: A survey at a German university hospital. Int. J. Public Health 2007, 52, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Zaresani, A.; Scott, A. Does digital health technology improve physicians’ job satisfaction and work–life balance? A cross-sectional national survey and regression analysis using an instrumental variable. BMJ Open 2020, 10, e041690. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Fujita, F. Resources, personal strivings, and subjective well-being: A nomothetic and idiographic approach. J. Pers. Soc. Psychol. 1995, 68, 926–935. [Google Scholar] [CrossRef] [PubMed]
- Kahn, R.L.; Byosiere, P. Stress in organizations. In Handbook of Industrial and Organizational Psychology; Dunette, M.D., Hough, L.M., Eds.; Consulting Psychologists Press: Palo Alto, CA, USA, 1992; Volume 3, pp. 571–650. [Google Scholar]
- German Hospital Directory. Available online: https://www.german-hospital-directory.com/app/search (accessed on 26 March 2023).
- Kristensen, T.S.; Borritz, M.; Villadsen, E.; Christensen, K.B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work Stress 2005, 19, 192–207. [Google Scholar] [CrossRef]
- Nübling, M.; Vomstein, M.; Haug, A.; Nolle, I.; Lindner, A.; Lincke, H. COPSOQ 3: Internationale Weiterentwicklung und deutsche Standardversion. PPmP Psychother. Psychosom. Med. Psychol. 2018, 68, e409. [Google Scholar] [CrossRef]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Fischer, T.; Riedl, R. Technostress research: A nurturing ground for measurement pluralism? Commun. Assoc. Inf. Syst. 2017, 40, 375–401. [Google Scholar] [CrossRef]
- Hanebuth, D.; Aydin, D.; Scherf, T. Burnout and related conditions in managers: A five-year longitudinal study. Psychol. Everyday Act. 2012, 5, 4–39. [Google Scholar]
- Lincke, H.-J.; Vomstein, M.; Lindner, A.; Nolle, I.; Häberle, N.; Haug, A.; Nübling, M. COPSOQ III in Germany: Validation of a standard instrument to measure psychosocial factors at work. J. Occup. Med. Toxicol. 2021, 16, 50. [Google Scholar] [CrossRef] [PubMed]
- Tabachnick, B.G.; Fidell, L.S.; Ullman, J.B. Using Multivariate Statistics; Pearson: Boston, MA, USA, 2007; Volume 5. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Mayring, P. Qualitative Inhaltsanalyse. In Handbuch Qualitative Forschung in der Psychologie; Mey, G., Mruck, K., Eds.; VS Verlag für Sozialwissenschaften: Wiesbaden, Germany, 2010; pp. 601–613. [Google Scholar]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson: Upper Saddle River, NJ, USA, 2009. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Califf, C.B.; Brooks, S. An empirical study of techno-stressors, literacy facilitation, burnout, and turnover intention as experienced by K-12 teachers. Comput. Educ. 2020, 157, e103971. [Google Scholar] [CrossRef]
- Berg-Beckhoff, G.; Nielsen, G.; Ladekjær Larsen, E. Use of information communication technology and stress, burnout, and mental health in older, middle-aged, and younger workers–results from a systematic review. Int. J. Occup. Environ. Health 2017, 23, 160–171. [Google Scholar] [CrossRef] [PubMed]
- Gimpel, H.; Lanzl, J.; Manner-Romberg, T.; Nüske, N. Hans Böckler Stiftung. Available online: https://www.boeckler.de/de/faust-detail.htm?sync_id=HBS-007024 (accessed on 23 March 2023).
- Gerdiken, E.; Reinwald, M.; Kunze, F. Outcomes of Technostress at Work: A Meta-Analysis. Acad. Manag. J. 2021, 2021, e11807. [Google Scholar] [CrossRef]
- Borle, P.; Reichel, K.; Niebuhr, F.; Voelter-Mahlknecht, S. How are techno-stressors associated with mental health and work outcomes? A systematic review of occupational exposure to information and communication technologies within the technostress model. Int. J. Environ. Res. Public Health 2021, 18, 8673. [Google Scholar] [CrossRef]
- Locke, T. Medscape Global Physicians’ Burnout and Lifestyle Comparisons. Available online: https://www.medscape.com/slideshow/2019-global-burnout-comparison-6011180 (accessed on 26 March 2023).
- Kasemy, Z.A.; Sharif, A.F.; Barakat, A.M.; Abdelmohsen, S.R.; Hassan, N.H.; Hegazy, N.N.; Sharfeldin, A.Y.; El-Ma’doul, A.S.; Alsawy, K.A.; Shereda, H.M.A. Technostress Creators and Outcomes Among Egyptian Medical Staff and Students: A Multicenter Cross-Sectional Study of Remote Working Environment During COVID-19 Pandemic. Front. Public Health 2022, 10, 796321. [Google Scholar] [CrossRef]
- Golz, C.; Peter, K.A.; Müller, T.J.; Mutschler, J.; Zwakhalen, S.M.; Hahn, S. Technostress and digital competence among health professionals in Swiss psychiatric hospitals: Cross-sectional study. JMIR Ment. Health 2021, 8, e31408. [Google Scholar] [CrossRef]
- Hämmig, O. Explaining burnout and the intention to leave the profession among health professionals—A cross-sectional study in a hospital setting in Switzerland. BMC Health Serv. Res. 2018, 18, 785. [Google Scholar] [CrossRef]
- Vandenbroeck, S.; Van Gerven, E.; De Witte, H.; Vanhaecht, K.; Godderis, L. Burnout in Belgian physicians and nurses. Occup. Med. 2017, 67, 546–554. [Google Scholar] [CrossRef]
- Cohen, T.N.; Jain, M.; Gewertz, B.L. Personal Communication Devices Among Surgeons—Exploring the Empowerment/Enslavement Paradox. JAMA Surg. 2021, 156, 302–304. [Google Scholar] [CrossRef]
- Borkowetz, A.; Leitsmann, M.; Baunacke, M.; Borgmann, H.; Boehm, K.; Groeben, C.; Roigas, J.; Schneider, A.W.; Speck, T.; Schroeder-Printzen, I.; et al. Acceptance and status of digitalization in clinics and practices: Current assessment in German urology. Urologie 2022, 61, 1365–1372. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. 9. The Concept of Coping. In Stress and Coping: An Anthology; Columbia University Press: New York, NY, USA, 1991; pp. 189–206. [Google Scholar]
- Bundesärztekammer. Available online: https://www.bundesaerztekammer.de/fileadmin/user_upload/downloads/pdf-Ordner/Statistik_2020/2020-Statistik.pdf (accessed on 23 March 2023).
- Cho, Y.I.; Johnson, T.P.; VanGeest, J.B. Enhancing surveys of health care professionals: A meta-analysis of techniques to improve response. Eval. Health Prof. 2013, 36, 382–407. [Google Scholar] [CrossRef] [PubMed]
| Construct (Type of Variable) | Measurement and Source | No. of Items |
|---|---|---|
| Technostress creators (IV, moderator) | Technostress Questionnaire [13] | 14 |
| Technostress inhibitors (IV, moderator) | Technostress Questionnaire [13] | 9 |
| Burnout (DV) | Copenhagen Burnout Inventory [73] | 6 |
| Work engagement (DV) | COPSOQ [74] | 3 |
| Job satisfaction (DV) | COPSOQ [61] | 7 |
| Variable | n | % | Variable | n | % |
|---|---|---|---|---|---|
| Gender | Patient beds in the department | ||||
| Female | 29 | 25.0 | 10–19 | 2 | 1.7 |
| Male | 87 | 75.0 | 20–29 | 40 | 34.5 |
| Age | 30–39 | 39 | 33.6 | ||
| 20–29 | 11 | 9.5 | 40–49 | 20 | 17.2 |
| 30–39 | 35 | 30.2 | 50 and more | 15 | 13.0 |
| 40–49 | 30 | 25.9 | Hospital ownership | ||
| 50–59 | 24 | 20.7 | Private | 26 | 22.4 |
| 60 years and older | 16 | 13.8 | Public | 22 | 19.0 |
| Mother tongue | Private non-profit | 68 | 58.6 | ||
| German | 106 | 91.4 | Federal state | ||
| Other | 10 | 8.6 | Baden-Württemberg | 17 | 14.7 |
| Position | Bavaria | 6 | 5.2 | ||
| Chief physician | 19 | 16.4 | Berlin | 6 | 5.2 |
| Senior physician | 58 | 50.0 | Brandenburg | 5 | 4.3 |
| Attending physician | 16 | 13.8 | Bremen | 3 | 2.6 |
| Resident physician | 23 | 19.8 | Hamburg | 7 | 6.0 |
| Years of professional work experience | Hesse | 13 | 11.2 | ||
| 1–9 | 36 | 31.0 | Mecklenburg Western Pomerania | 5 | 4.3 |
| 10–19 | 31 | 26.7 | Lower Saxony | 13 | 11.2 |
| 20–29 | 25 | 21.6 | North Rhine-Westphalia | 35 | 21.6 |
| 30–39 | 21 | 18.1 | Rhineland Platinate | 2 | 1.7 |
| 40 years and more | 4 | 3.4 | Saarland | 0 | 0.0 |
| Working hours in inpatient care/week | Saxony | 2 | 1.7 | ||
| 20–29 | 11 | 9.5 | Saxony-Anhalt | 4 | 3.4 |
| 30–39 | 13 | 11.2 | Schleswig Holstein | 7 | 6.0 |
| 40–49 | 42 | 36.2 | Thuringia | 1 | 0.9 |
| 50 h and more | 48 | 41.4 | |||
| HIS | EHR | Dictaphones | Patient Portals | Robots | Medication Management | Smartphone Apps | Online Knowledge Bases | Digital SOPs | Tele- Medicine | Messenger Services | Tablets | Decision Support Systems | VR/AR | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | 5.000 | 2.422 | 0.940 | 0.914 | 0.884 | 0.806 | 0.685 | 0.681 | 0.491 | 0.461 | 0.375 | 0.306 | 0.108 | 0.017 |
| Mdn. | 5.000 | 1.500 | 0.500 | 0.000 | 0.000 | 0.000 | 0.500 | 0.500 | 0.250 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| SD | 2.2660 | 2.6683 | 1.3676 | 1.9261 | 1.6102 | 1.6950 | 1.2204 | 1.1542 | 0.9041 | 0.8292 | 1.0792 | 1.2437 | 0.3217 | 0.1857 |
| Min | 1.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Max | 10.0 | 10.0 | 7.5 | 10.0 | 6.0 | 10.0 | 10.0 | 8.5 | 8.0 | 5.5 | 10.0 | 10.0 | 2.0 | 2.0 |
| Variables | M | Mdn. | SD | Min | Max | α |
|---|---|---|---|---|---|---|
| Technostress | 2.67 | 2.71 | 0.692 | 1 | 5 | |
| Techno-uncertainty | 2.82 | 2.75 | 0.776 | 1 | 5 | 0.690 |
| Techno-complexity | 2.25 | 2.00 | 1.040 | 1 | 5 | 0.867 |
| Techno-overload | 2.99 | 3.10 | 0.945 | 1 | 5 | 0.853 |
| Technostress inhibitors | 2.30 | 2.17 | 0.818 | 1 | 5 | |
| Literacy facilitation | 2.64 | 2.60 | 0.887 | 1 | 5 | 0.846 |
| Involvement facilitation | 1.97 | 1.75 | 0.920 | 1 | 5 | 0.837 |
| Job satisfaction | 3.56 | 3.57 | 0.591 | 2 | 5 | 0.793 |
| Work engagement | 3.73 | 3.67 | 0.671 | 2 | 5 | 0.790 |
| Burnout | 2.86 | 2.92 | 0.788 | 1 | 5 | 0.907 |
| Variables | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1 Technostress Techno-overload Techno-complexity Techno-uncertainty | – | ||||
| 2 Technostress inhibitors Literacy facilitation Involvement facilitation | 0.234 ** | ||||
| 3 Burnout | 0.248 ** | 0.040 | – | ||
| 0.245 ** | 0.063 * | ||||
| 0.181 ** | −0.003 | ||||
| 0.201 ** | |||||
| 4 Work engagement | −0.176 ** | 0.020 | −0.441 ** | – | |
| −0.149 ** | 0.012 | ||||
| −0.242 ** | −0.031 | ||||
| −0.094 ** | |||||
| 5 Job satisfaction | −0.170 ** | 0.203 ** | −0.560 ** | 0.437 * | – |
| −0.139 ** | 0.198 ** | ||||
| −0.184 ** | 0.118 ** | ||||
| −0.111 ** |
| Variable | Burnout | Work Engagement | Job Satisfaction | |||
|---|---|---|---|---|---|---|
| R2 = 0.073 F2,1273 = 50.231, p < 0.001 | R2 = 0.042 F2,1272 = 28.137, p < 0.001 | R2 = 0.062 F2,1273 = 42.218, p < 0.001 | ||||
| β | robust se | β | robust se | β | robust se | |
| Technostress | 0.293 p < 0.001 | 0.029 | −0.175 p < 0.001 | 0.023 | −0.206 p < 0.001 | 0.022 |
| Technostress inhibitors | 0.036 p = 0.189 | 0.028 | −0.049 p = 0.082 | 0.028 | 0.119 p < 0.001 | 0.030 |
| Intercept | 1.991 p < 0.001 | 0.091 | 4.308 p < 0.001 | 0.080 | 3.839 p < 0.001 | 0.081 |
| Variable | Burnout | Work Engagement | Job Satisfaction | |||
|---|---|---|---|---|---|---|
| R2 = 0.073 F2,1272 = 40.046, p < 0.001 | R2 = 0.048 F3,1271 = 23.899, p < 0.001 | R2 = 0.079 F3,1272 = 36.415, p < 0.001 | ||||
| β | robust se | β | robust se | β | robust se | |
| Moderation effect | −0.020 p < 0.001 | 0.462 | −0.081 p = 0.001 | 0.030 | −0.123 p = 0.001 | 0.031 |
| Disadvantages/Criticisms of ICT |
|---|
| Technical problems: lack of hardware/outdated hardware (n = 9), slow wi-fi (n = 3), technical failures/difficulties (n = 12), slow system response time (n = 11) |
| Low user-friendliness: complicated navigation (n = 3), missing coordination with clinical work processes (n = 5), lack of user-friendliness (n = 5), complexity of ICT (n = 1), lack of user motivation (n = 1) |
| Lack of interoperability (n = 8) |
| Clinical documentation: high documentation load (n = 6), double documentation (n = 3) |
| Increased workload (n = 19) |
| IT support and training: lack of IT support (n = 2), lack of training offers (n = 2) |
| Digital transformation in the hospital: delayed transformation process (n = 11), additional work and problems due to transition phase (n = 8) |
| Advantages of ICT |
| Availability of information: availability of patient data quickly and at any time in several places at the same time (n = 26), use of online knowledge databases (n = 1) |
| General reduction of workload and time savings (n = 10) |
| Transparency: transparent documentation (n = 3), better overview and readability (n = 2) |
| Desire for paperless work and digital transformation (n = 3) |
| Category | Sub-Categories |
|---|---|
| Institutional offer | Break room (n = 1), massage/physiotherapy (n = 3), sports facilities (n = 4), childcare (n = 1), communication training (n = 1), higher salary (n = 1) |
| Organizational changes | Better process management (n = 3), expansion of IT support (n = 2), individual working hours/reduction of working hours (n = 6), working time accounts (n = 1), good team atmosphere (n = 2), good communication within the team (n = 2) |
| Other | Private recreation (n = 8), none (n = 11) |
| Category | Sub-Categories |
|---|---|
| Institutional offer | Relaxation offers (n = 5), sport offers (n = 7), healthy/free food (n = 2), communication training (n = 4), individualized workplace design (n = 3), childcare (n = 1), higher salary or payment of overtime (n = 2) |
| Organizational changes | More staff, needs-based demand planning work distribution (n = 14), more ICT training offers (n = 2), personal ICT training (n = 2), expansion of IT support (n = 6), involving end-users in digitization projects (n = 5), more appreciation (n = 2), individual working hours or reduction of working hours (n = 5), adherence working hours according to the employment contract (n = 1), working time account (n = 1) |
| Other | User-friendly ICT in general (n = 1), better hardware (n = 1), faster Wi-Fi (n = 1), interoperability of ICT (n = 2), shorter loading times (n = 1), none (n = 4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bail, C.; Harth, V.; Mache, S. Digitalization in Urology—A Multimethod Study of the Relationships between Physicians’ Technostress, Burnout, Work Engagement and Job Satisfaction. Healthcare 2023, 11, 2255. https://doi.org/10.3390/healthcare11162255
Bail C, Harth V, Mache S. Digitalization in Urology—A Multimethod Study of the Relationships between Physicians’ Technostress, Burnout, Work Engagement and Job Satisfaction. Healthcare. 2023; 11(16):2255. https://doi.org/10.3390/healthcare11162255
Chicago/Turabian StyleBail, Clara, Volker Harth, and Stefanie Mache. 2023. "Digitalization in Urology—A Multimethod Study of the Relationships between Physicians’ Technostress, Burnout, Work Engagement and Job Satisfaction" Healthcare 11, no. 16: 2255. https://doi.org/10.3390/healthcare11162255
APA StyleBail, C., Harth, V., & Mache, S. (2023). Digitalization in Urology—A Multimethod Study of the Relationships between Physicians’ Technostress, Burnout, Work Engagement and Job Satisfaction. Healthcare, 11(16), 2255. https://doi.org/10.3390/healthcare11162255





