Abstract
Mental health problems of health workers are attracting increasing concerns in China and the world. A trustful relationship between health workers and patients is the foundation of quality patient care, which is currently under serious threat. This study aimed to determine the associations of social trust on subjective wellbeing and mental health of health workers. Using the survey data of 262 health workers extracted from the 2018 Chinese Family Panel Studies, a structural equation model with partial least square approach was established. The results showed that social trust was linked to both subjective wellbeing (β = 0.251, p < 0.01) and mental health (β = −0.210, p < 0.01). The effect of social trust on mental health was partially mediated by subjective wellbeing (51.87%). The association between social trust and subjective wellbeing was moderated by socioeconomic status: social trust has a stronger effect on subjective wellbeing in those with higher socioeconomic status. Erosion of social trust may present a serious risk to mental health and subjective wellbeing of health workers. High socioeconomic status can amplify the effect of social trust.
1. Introduction
Mental health problems of health workers are attracting increasing attention all over the world. High levels of work stress are common in health professionals [1]. Psychological disorders caused by work stress can affect cognitive functions such as concentration, understanding, and decision-making [2], leading to poor quality of patient care [3,4]. Maintaining mental health of health workers is also critical in response to the COVID-19 pandemic [5]. Subjective wellbeing is a crucial indicator impacting the mental health of health workers [6]. However, subjective wellbeing of Chinese health workers had a decreasing trend from 2004 to 2020 [7]. Previous research has established important positive relationships between social trust and subjective wellbeing [8]. Trustful relationships with family and relatives, friends, and neighbors are considerably related to subjective wellbeing [9]. Doctor–patient trust as a special kind of trust relationship has become discordant in recent years. Violent conflicts between doctors and patients have caused burnout syndrome and emotional exhaustion of health workers in China [10].
Health workers in China are facing unprecedented challenges in managing their relationships with patients, which has put a great deal of stress on them [3]. Since the introduction of the market mechanism in China [11], health workers have been charged with a responsibility to generate revenues through user charges for their institutions because of the declined share of governmental investment in the 1990s [12]. This has led to a public outcry on the affordability of medical care, causing a growing tension between health workers and consumers. Meanwhile, work pressure on health workers has been increasing, partly due to insufficient resources and partly due to increased consumer demands [13,14]. For example, China has 3.34 nurses per 1000 population, compared with 3.69 on average in the world, 8.34 in the US, and 7.93 in European countries [15]. There have been increasing concerns in recent years over the high prevalence of work stress and burnout in health workers in China [16]. Meanwhile, the mismatch between supply and demand has exacerbated the tension between health workers and consumers [17], eroding social trust from the public.
Social trust falls into the category of systemic trust, which refers to the expectation that individuals and groups can rely on others and the overall institutional system of the society for their interest [18]. According to Putnam [19], social trust is a manifestation of social capital. There is a paucity in the literature documenting social trust from health workers, despite speculation on its association with mental health [20]. Health workers are often expected to take social responsibilities such as fight against disease outbreaks in addition to their individual-based clinical works [21,22]. However, the deterioration of public trust in health workers is likely to jeopardize the trust of health workers in others [23], which can trigger a sense of doubt about the public appreciation for their contributions [24]. Previous studies in community settings have shown that low levels of social trust are associated with poor self-rated health [25,26].
This study aimed to address the gap in the literature by assessing social trust held by health workers and testing its associations with subjective wellbeing and mental health. Four hypotheses were proposed (Figure 1):
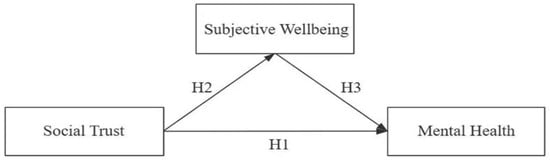
Figure 1.
Hypotheses tested in the study.
Hypothesis 1 (H1).
Higher social trust is associated with better mental health.
Hypothesis 2 (H2).
Higher social trust is associated with higher subjective wellbeing.
Hypothesis 3 (H3).
Higher subjective wellbeing is associated with better mental health.
Hypothesis 4 (H4).
Subjective wellbeing mediates the effect of social trust on mental health.
1.1. Review of the Literature and Hypothesis Development
1.1.1. Relationship between Social Trust and Mental Health
Previous studies have demonstrated a positive correlation between social trust and general health [27]. This aligns well with the theory of social determinants of health [28]. It is worth noting that social trust is not only important for individual health and wellbeing but also has an impact on various aspects of the healthcare system. Social trust encourages cooperative behaviors, social cohesion, social solidarity, and collective actions [29]. Empirical evidence shows that community residents who trust and help each other have better mental health than those who do not [30,31,32]. Social trust can help with the healing process in those who experience traumatic events [33], mitigate the negative mental health consequences of socioeconomic deprivations on children [34], and ease psychological distress of older people [35]. Low levels of trust in unknown people are associated with high levels of mental stress [36]. Research also suggests that poor mental health has a significant negative impact on social trust [37].
1.1.2. Relationship between Social Trust and Subjective Wellbeing
Subjective wellbeing reflects an individual’s affirmative attitudes and positive feelings arising from a comparison between the actual state of life and the ideal state of life [38]. Life satisfaction is one of the key elements of subjective wellbeing [39]. Many external factors such as event context and demographics can affect subjective wellbeing [40].
A growing body of the literature points to a positive connection between social trust and subjective wellbeing. Trustful relationships with family members, relatives, friends, and neighbors are more closely linked to subjective wellbeing than structural social capital [9,19]. Social trust has been found to be beneficial to the emotional wellbeing of rural people in China [41], possibly through the pathway of social networking and social support [42]. A survey of 1449 left-behind children (who did not live with their emigrated parents) in China found that social cohesion and trusting relationships with caregivers positively predict the subjective wellbeing of the left-behind children [43]. To the best of our knowledge, there has been no research into the association between social trust and subjective wellbeing of health workers.
1.1.3. Relationship between Subjective Wellbeing and Mental Health
The link between subjective wellbeing and mental health has been well documented. High levels of subjective wellbeing are associated with good health, longevity, good social relationships, high job performance, and creativity [44]. Previous studies have confirmed that the association between subjective wellbeing and health varies by age [45], but overall, high levels of subjective wellbeing are associated with lower levels of mental health problems, such as stress, depression, anxiety, and loneliness [46]. Subjective wellbeing is also closely related to long-term health behaviors [47].
1.1.4. Relationships between Social Trust, Subjective Wellbeing, and Mental Health
Given that social trust is linked to both subjective wellbeing and mental health, a mediation analysis is warranted to examine the role of subjective wellbeing in the association between social trust and mental health. A previous study showed that high subjective wellbeing can effectively reduce the impact of social trust (or a lack of) on the emotional health of older people [41]. Institutional trust has been proved to partially mediate the relationship between subjective wellbeing and mental health [48]. Social trust also partially mediates the effect of satisfaction with social security on subjective wellbeing [49].
2. Materials and Methods
2.1. Data Source
Data were extracted from the 2018 China Family Panel Studies (CFPS), which are publicly available. No ethics approval was required.
The CFPS was started in 2010 by the Institute of Social Science Survey (ISSS) at Peking University. It aims to reflect the changes of China’s society, economy, population, education, and health by tracking and collecting data at the individual, family, and community levels and focuses on the economic and non-economic wellbeing of Chinese residents, including economic activities, educational outcomes, family relations and dynamics, population migration, and health. There are four main types of CFPS questionnaires: community questionnaire, family questionnaire, adult questionnaire, and children questionnaire. Adult questionnaires were used in this study. Five waves of the survey have been completed since then, with samples drawing from 25 provinces/regions in mainland China. A probability proportional to size (PPS) sampling strategy was employed to recruit study participants. Data were collected through computer-assisted personal interviews, followed by quality audit measures such as random telephone and field checks, audio recording, interview reviews, and logical analyses [50].
We used the 2018 CFPS dataset for this study because it contains the largest sample of our target participants (health workers). The 2018 CFPS collected 37,354 records, in which 281 were completed by respondents flagged as a physician, a nurse, or an allied health professional. We adopted imputation method strategy to manage missing values. This resulted in a final sample of 262 participants for data analyses.
2.2. Measurements
2.2.1. Mental Health
Mental health was the outcome indicator in this study. It was measured using the simplified Epidemiological Studies-Depression Scale (CES-D8), which has demonstrated good reliability and validity in China [51]. In this study, 5 items were selected as outer loadings that are more than 0.65 (Appendix A Table A1). Respondents were asked to report how often in the past week they felt depressed, struggled, felt happy (score reversed), felt joyful (score reversed), and felt sad, along a scale ranging from 0 ‘none of the time’ to 3 ‘almost or all of the time’. A summed score (0–15) was calculated, with a higher score indicating worse mental health.
2.2.2. Social Trust
The effect of social trust on mental health was the major interest of this study. In the CFPS, social trust was defined as a belief in the honesty, integrity, and reliability of other people with whom one usually interacts in daily life [52]. Respondents were asked to rate their trust in parents, Americans, strangers, neighbors, physicians, and local governmental officials, respectively, along a ten-point scale ranging from 0 (strongly distrust) to 10 (strongly trust) [53]. In this study, three items (neighbors, physicians, and local governmental officials) were selected to measure social trust as outer loadings are more than 0.65 (Appendix A Table A1). A summed score (0–30) was calculated, with a higher score indicating a higher level of social trust.
2.2.3. Subjective Wellbeing
This study tested the mediating effect of subjective wellbeing on the association between social trust and mental health. Subjective wellbeing was measured based on the concept proposed by Diener [54], encompassing life satisfaction, life happiness, and future self-confidence. Diener [54] identified three features of subjective wellbeing: subjectivity, relative stability, and integrity. Respondents were asked to rate their life satisfaction and future self-confidence on a five-point Likert scale, while life happiness was rated on a ten-point scale ranging from 1 (very unhappy) to 10 (very happy). A summed score (0–20) was calculated, with a higher score indicating a higher level of subjective wellbeing.
2.2.4. Living and Working Conditions
In this study, we also tested the association between sleep time and subjective wellbeing and the moderation effect of socioeconomic status (SES) on the association between social trust and subjective wellbeing. Healthcare services often require night shifts, which can disrupt daily routines, leading to low levels of subjective wellbeing [55]. In this study, sleep time was measured by a latent variable containing two items: average daily sleep hours over workdays and average daily sleep hours over non-workdays.
Empirical evidence shows that people with low SES tend to have low social trust and poor health outcomes [56,57]. A previous study found that higher levels of public health investment appear to be associated with both higher levels of subjective wellbeing and higher levels of health outcomes [58]. In this study, SES was measured by a latent variable containing three items: average annual household income (<50,000, 50,000–100,000, >1,000,000 Yuan), individual educational attainment (with or without a university degree), and self-rated social status. Traditional SES measures usually cover income, education, and occupation [59,60]. However, self-perceived social status is a much stronger predictor of health outcomes than occupation [57]. In the CFPS, respondents were asked to rate their social status in comparison with others in the local community on a five-point scale ranging from 1 (very low) to 5 (very high), which was collapsed into three categories in data analyses: low (1–2), average (3), and high (4–5).
2.2.5. Sociodemographic Characteristics
Data in regard to age (≤35, 36–64, ≥65 years), sex (male or female), household registration (urban or rural), marital status (never married, married/cohabiting, or widowed/divorced), and profession (physician, nurse, or allied health profession) were collected in the 2018 CFPS.
2.3. Statistical Analysis
Data were analyzed using SPSS 26.0 and Smart PLS 4.0.
The sociodemographic characteristics of study participants were described using frequency distributions. The mean values and standard deviations (SDs) of social trust, mental health, and subjective wellbeing of the study participants with different sociodemographic characteristics were calculated and compared through student t tests or ANOVA.
Structural equation modeling with partial least square (PLS-SEM) was established to test the study hypotheses. We chose PLS-SEM because it does not require a large sample size nor a normal distribution of data [61,62]. The modeling started with a testing of reliability and validity of the key constructs measured. Reliability was assessed using Cronbach’s α, rho-A, and composite reliability, with a higher than 0.6 coefficient deemed acceptable [63]. Validity was assessed through convergent validity and discriminant validity. The former was reflected by the average variance extracted (AVE), with a minimum threshold value of 0.5 [64]. The latter was assessed through the Fornell–Larker criterion and heterotrait–monotrait ratio of correlations (HTMT) [65,66]. The Fornell–Larcker criterion requires that the square root of each AVE is higher than the correlation coefficients between the tested construct and other constructs [67]. The HTMT ratio measures similarity between tested constructs, which must be lower than 0.90 [65,68,69].
Once the reliability and validity of the tested constructs were confirmed, PLS-SEM was established using a 5000 bootstrapped procedure [68]. Fitness of data into the model was assessed through standardized root mean square (SRMR between 0 and 1) [67], R2 (between 0 and 1), Q2 (>0) [65], and root mean squared error (RMSE) and mean absolute error (MAE) with a naïve benchmark [69]. While R2 and Q2 reflect in-sample explanatory power of the model, RMSE and MAE indicate out-of-sample predictive power of the PLS path model estimations [69]. The naïve benchmark for RMSE and MAE was generated through linear regression modelling (LM). A high predictive power is assumed if none of the constructs in the PLS-SEM have a higher RMSE or MAE value compared to the naïve LM benchmark [69,70].
A two-side p value less than 0.05 was considered statistically significant for the path coefficients. We calculated the VAF (variance accounted for) value to determine the mediation effect: less than 20% indicates no mediation, 20–80% indicates partial mediation, and above 80% indicates full mediation [64].
3. Results
3.1. Characteristics of Respondents
The majority of study participants were female (67%), registered as an urban resident (52%), and married or cohabited with others (78%) at the time of the survey. About half were younger than 35 years. Most participants were physicians (40%) or nurses (40%) and have a university degree (70%). The average sleep time was 7.28 (SD = 1.36) hours on workdays and 7.94 (SD = 1.55) hours on non-workdays. Over 43% of participants reported an annual household income between 50,000 and 100,000 Yuan. About 58% considered their local social status as average (Table 1).

Table 1.
Sociodemographic characteristics, social trust, mental health, and subjective wellbeing of study participants.
Marriage was associated with higher levels of social trust (p = 0.003), mental health (p = 0.001), and subjective wellbeing (p = 0.025). Higher self-rated social status was associated with higher levels of social trust (p = 0.023) and subjective wellbeing (p = 0.006). Nurses had the lowest level of social trust (p = 0.029) (Table 1).
The study participants reported a mean score of 18.65 (SD = 4.45), 8.95 (SD = 2.68), and 15.49 (SD = 3.02) for social trust, mental health, and subjective wellbeing, respectively, similar to those of non-health workers (Appendix A Table A2).
3.2. PLS-SEM Results
The PLS-SEM demonstrated acceptable reliability and validity of key constructs as indicated in Table 2, Table 3 and Table 4. The reliability coefficients of mental health and subjective wellbeing were all above 0.7, despite a slightly lower but still acceptable Cronbach’s alpha and Rho-A for social trust (>0.6 in Table 2) possibly due to its low number of measurement items [64]. The AVE values for the three constructs were all above 0.5 (Table 2), demonstrating acceptable convergent validity. The discriminant validity of the three constructs was supported by the Fornell–Larcker criterion (Table 3) and the HTMT ratio (Table 4).

Table 2.
Reliability of measurement constructs.

Table 3.
Discriminant validity—Fornell–Larcker criterion.

Table 4.
Discriminant validity—Heterotait–Monotrait (HTMT) ratio.
Overall, the PLS-SEM showed good fitness of data: SRMR = 0.085; R2 = 0.286; Q2 = 0.138. The path estimations showed medium predictive power, with most RMSE and MAE values being higher than their naïve LM benchmarks (Table 5).

Table 5.
Predictive results of partial least square (PLS) and linear regression modeling (LM).
The PLS-SEM indicated a direct link between social trust and mental health: one unit increase in social trust was associated with 0.210 units of improvement in mental health (a reduction of mental health problems) (Figure 2): hypothesis one (H1) was accepted. One unit increase in social trust was also associated with a 0.251 unit increase in subjective wellbeing (Figure 2): hypothesis two (H2) was accepted. One unit increase in subjective wellbeing was associated with 0.431 units of improvement in mental health (a reduction in mental health problems) (Figure 2): hypothesis three (H3) was accepted.
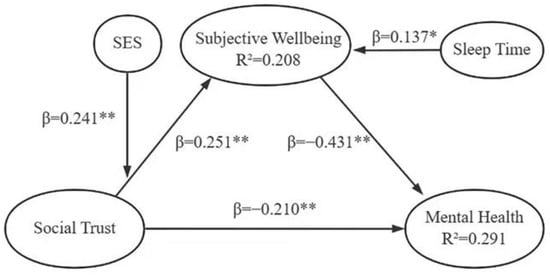
Figure 2.
Social trust, subjective wellbeing, and mental health: PLS-SEM. Note: * p < 0.05, ** p < 0.01.
Subjective wellbeing partially mediated the effect of social trust on mental health: the indirect effect accounted for 51.87% of the variance (Table 6). Hence, hypothesis four (H4) was accepted.

Table 6.
Results of hypothesis testing.
Further analyses showed that longer sleep duration was associated with higher subjective wellbeing (β = 0.173, p = 0.026). SES moderated the effect of social trust on subjective wellbeing: higher effect of social trust on subjective wellbeing was found in those with higher SES (β = 0.241, p = 0.048).
4. Discussion
Health workers have similar levels of social trust, subjective wellbeing, and mental health in comparison with their non-health counterparts in China, according to the findings of this study. There exist significant links among these three constructs in health workers. Firstly, higher social trust is associated with better mental health. This result is consistent with the findings of previous studies [31,64,71,72]. Social trust may reduce work stress of health workers through a perception of supportive work and social environments. Public and consumer engagement has been considered as a critical determinant of patient care outcomes. Social trust provides a fundamental condition for effective consumer engagement. Higher levels of social trust can make health workers feel psychologically safe to work in partnerships with their patients to achieve clinical excellence [23,73], reducing psychological distress [74].
Secondly, higher social trust is associated with higher subjective wellbeing. This finding is supported by several other studies [19,43]. The Chinese culture emphasizes kinship and “Guanxi” [75]. Those who have a large network of social connections are highly regarded and respected, and they tend to have higher levels of life satisfaction. Social connection from family members, friends, coworkers, and other adults is a known protective factor for mental health. Family and friend relationships make unique contributions to wellbeing [76,77]. High levels of social trust enable people to enjoy their daily life, reducing negative emotions such as a hostile mentality, anger, and anxiety. The association between social trust and subjective wellbeing may be bidirectional [78]. Social trust encourages people to develop and expand ties with others, increasing subjective wellbeing. Meanwhile, subjective wellbeing helps foster more trustful relationships with others. Trust is essential for health workers to maintain good relationships with patients. A study of physicians in China showed a clear connection between public trust and self-rated happiness [79]. However, public trust in health workers has been declining in China in recent years. Meanwhile, health workers have reported lower levels of social trust in comparison with their patients [80,81,82].
Thirdly, higher subjective wellbeing is associated with better mental health. This is not surprising as happiness, one of the elements of subjective wellbeing, is an indication of healthy emotion. A study of 3989 adults in Australia reported that subjective wellbeing reduces vulnerability to depression and anxiety [83]. Another study during the outbreak of COVID-19 found that lower subjective wellbeing of frontline health workers is associated with moral injury, burnout, and psychological distress [81]. In China, physicians perceived high levels of stress, burnout, and a declined sense of wellbeing as indications of poor workplace wellbeing [82]. Health workers maybe have a low level of subjective wellbeing in high stress scenarios. However, our study showed there was not significant difference between subjective wellbeing of physicians under normal working conditions and the general public. A more complex mechanism needs to be further explored.
Fourthly, subjective wellbeing partially mediates the effect of social trust on mental health. The result is consistent with the findings of previous studies of young and middle-aged adults [84,85]. The psychological burden of health workers can be exacerbated when subjective wellbeing is at a low level. Health workers are constantly exposed to stressful events such as the outbreak of COVID-19, which would undoubtedly affect their subjective wellbeing. Working under a stressful environment influences the everyday life of health workers [86]. It is important to pay increasing attention to the subjective wellbeing of health workers.
The moderation role of SES in the link between social trust and subjective wellbeing revealed in this study warrants further studies. We found a stronger effect of social trust on subjective wellbeing in those with higher SES. The underlying mechanism of such a moderation effect is unclear, but it highlights the challenges for improving the mental health of people who have a lower perceived SES. SES has been found to be a strong predictor of health outcomes [87]. Some researchers argue that poverty alleviation and wealth increase should be taken as a top priority for improving the wellbeing of people [88,89]. However, this is not enough. Individual perception of SES often involves a comparison with others. Internationally, there exists a hierarchical structure in health professionals, with medical doctors usually enjoying the top status. The vast majority of health workers such as nurses may rate their SES as lower in comparison with medical doctors. In China, health workers of tertiary hospitals often have higher qualifications and higher income and attract higher social trust than their counterparts in the primary care sector [90]. This can lead to a vicious cycle, making mental health promotion for nurses and primary care workers extremely challenging.
Sleep deprivation has been an occupational health concern for health workers [91]. We found a direct link between sleep time and subjective wellbeing. Previous studies show that health workers working long night shifts suffer higher incidence of depression, stress, and burnout [92]. Sleep latency mediates the effect of night-shift work on mental wellbeing [93]. Sleep disturbance is often associated with poor job performance, poor doctor-patient relationship, and psychosomatic symptoms [94]. Poor quality of sleep can mediate the effect of anxiety on subjective wellbeing [95].
5. Conclusions
This research revealed that the social trust and subjective wellbeing play a substantial role in promoting the mental health of health workers. Thus, it can be recommended that improving the level of social trust especially interpersonal trust is an important strategy to promote the mental health of health workers. On the contrary, erosion of social trust may present a serious risk to mental health and subjective wellbeing of health workers. Health service managers can foster a culture and service environment, in which health workers feel safe, supported, and protected. They can also promote a patient safety culture that discourages status distinction across health professions. Increasing policy attention should be paid to pay equality and work–life balance for health workers. These measures are essential for promoting the mental health and subjective wellbeing of health workers and for ensuring the safety and quality of patient care.
6. Limitations and Future Research
The present study has several limitations. The data used in this study were drawn from a Chinese context. The effect of social trust on mental health workers is likely to vary under different system contexts. We were not able to explore the occupational differences of the effect of social trust on mental health either due to limited sample size. Our study adopted a cross-sectional design, and causal conclusions should not be assumed.
Author Contributions
C.X.: drafting the manuscript, data collection and analysis, and revising the manuscript. Y.Y.: data collection and drafting the manuscript. T.H.: revising the manuscript. J.C.: drafting the manuscript and revising the manuscript. S.X.: data analysis. C.L.: conceptualization, articulation of the story line, writing, and revising. All authors have read and agreed to the published version of the manuscript.
Funding
The project was funded by a grant from National Health Commission of the People’s Republic of China (The construction of high-quality development evaluation indicators system of public hospitals, No. 3) and Doctoral Set-up Fund of Wuhan University of Science and Technology (No.1170034).
Institutional Review Board Statement
The research protocol was approved by the Peking University Biomedical Ethics Review Committee (IRB00001052-14010) as well as Wuhan University of Science and Technology Biomedical Ethics Review Committee (202-300-3).
Informed Consent Statement
All methods were carried out in accordance with the Declaration of Helsinki.
Data Availability Statement
The datasets generated during the current study are available in the Peking University Open Research Data Platform repository, https://opendata.pku.edu.cn/dataset.xhtml?persistentId=doi:10.18170/DVN/45LCSO (accessed on 15 June 2020).
Acknowledgments
We thank China Family Panel Studies (CFPS) data source conducted by Chinese Social Science Survey Center (ISSS) of Peking University in 2018.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Outer loadings of measurement constructs.
Table A1.
Outer loadings of measurement constructs.
| Construct | Outer Loadings |
|---|---|
| Social trust (ST) | |
| ST-1: Trust in neighbors. | 0.747 |
| ST-2: Trust in local government officials. | 0.658 |
| ST-3: Trust in physicians. | 0.628 |
| ST-4: Trust in parents. | 0.443 |
| ST-5: Trust in Americans. | 0.497 |
| ST-6: Trust in strangers. | 0.527 |
| Subjective wellbeing (SWB) | |
| SWB-1: What is your happiness level? | 0.843 |
| SWB-2: How satisfied are you with your life? | 0.788 |
| SWB-3: How confident do you feel about the future? | 0.762 |
| Mental health (MH) | |
| MH-1: I felt depressed. | 0.713 |
| MH-2: I struggled. | 0.740 |
| MH-3: I felt delighted. | 0.664 |
| MH-4: I felt joyful in life. | 0.658 |
| MH-5: I felt sad. | 0.715 |
| MH-6: I did not sleep well. | 0.583 |
| MH-7: I felt lonely. | 0.648 |
| MH-8: I felt life could not go on. | 0.460 |

Table A2.
Social trust, mental health, and subjective wellbeing of health workers and non-health workers.
Table A2.
Social trust, mental health, and subjective wellbeing of health workers and non-health workers.
| Participants | Sample Size (n) | Social Trust (Mean ± SD) | Mental Health (Mean ± SD) | Subjective Wellbeing (Mean ± SD) |
|---|---|---|---|---|
| Health workers | 262 | 18.65 ± 4.64 | 8.95 ± 2.68 | 15.49 ± 3.05 |
| Non-health workers | 18199 | 18.53 ± 5.59 | 9.06 ± 2.86 | 15.63 ± 3.33 |
| p | <0.001 | 0.395 | 0.676 |
References
- Zhang, X.; Zhao, K.; Zhang, G.; Feng, R.; Chen, J.; Xu, D.; Liu, X.; Ngoubene-Atioky, A.J.; Huang, H.; Liu, Y.; et al. Occupational Stress and Mental Health: A Comparison Between Frontline Medical Staff and Non-frontline Medical Staff During the 2019 Novel Coronavirus Disease Outbreak. Front. Psychiatry 2020, 11, 555703. [Google Scholar] [CrossRef]
- Zaka, A.; Shamloo, S.E.; Fiorente, P.; Tafuri, A. COVID-19 pandemic as a watershed moment: A call for systematic psychological health care for frontline medical staff. J. Health Psychol. 2020, 25, 883–887. [Google Scholar] [CrossRef]
- Sun, J.; Sun, R.; Jiang, Y.; Chen, X.; Li, Z.; Ma, Z.; Wei, J.; He, C.; Zhang, L. The relationship between psychological health and social support: Evidence from physicians in China. PLoS ONE 2020, 15, e0228152. [Google Scholar] [CrossRef]
- Su, J.-A.; Weng, H.-H.; Tsang, H.-Y.; Wu, J.-L. Mental health and quality of life among doctors, nurses and other hospital staff. Stress Health 2009, 25, 423–430. [Google Scholar] [CrossRef]
- Chen, Q.; Liang, M.; Li, Y.; Guo, J.; Fei, D.; Wang, L.; He, L.; Sheng, C.; Cai, Y.; Li, X.; et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, E15–E16. [Google Scholar] [CrossRef]
- Mache, S.; Klapp, B.F.; Groneberg, D.A. The well-being and mental health of male and female hospital doctors in Germany. World Hosp. Health Serv. 2014, 50, 17–22. [Google Scholar]
- Liang, S.; Taige, Z.; Junjie, L.; Haiyun, P.; Sufei, X. Changes of medical staffs’ subjective well-being in China (2004–2020): A cross-temporal meta-analysis. Appl. Psychol. Health Well-Being 2022, 15, 425–446. [Google Scholar]
- June, P.S.; Rui, Z.; Ki-Chul, P. The Effect of Social Trust on Subjective Well-Being: Focusing on the Moderation Effect of Individualism-Collectivism. Acad. Cust. Satisf. Manag. 2021, 23, 35–36. [Google Scholar]
- Ahn, Y.-J. Do Informal Social Ties and Local Festival Participation Relate to Subjective Well-Being? Int. J. Environ. Res. Public Health 2021, 18, 16. [Google Scholar] [CrossRef]
- Baiyu, L.; Meijia, X.; Lijuan, L.; Xiaoying, Z. Burnout syndrome, doctor-patient relationship and family support of pediatric medical staff during a COVID-19 Local outbreak in Shanghai China: A cross-sectional survey study. Front. Pediatr. 2023, 11, 1093444. [Google Scholar]
- Cai, F. Perceiving Truth and Ceasing Doubts: What Can We Learn from 40 Years of China’s Reform and Opening up? China World Econ. 2018, 26, 1–22. [Google Scholar] [CrossRef]
- Liu, G.G.; Vortherms, S.A.; Hong, X. China’s health reform update. Annu. Rev. Public Health 2017, 38, 431–438. [Google Scholar] [CrossRef]
- Yip, W.C.-M.; Hsiao, W.C.; Chen, W.; Hu, S.; Ma, J.; Maynard, A. Early appraisal of China’s huge and complex health-care reforms. Lancet 2012, 379, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Liu, L.; Wang, Y.; Gao, F.; Zhao, X.; Wang, L. Factors associated with burnout among Chinese hospital doctors: A cross-sectional study. BMC Public Health 2013, 13, 786. [Google Scholar] [CrossRef] [PubMed]
- WHO. The World Health Organization releases State of the World’s Nursing Report. AORN J. 2020, 111, 6. [Google Scholar]
- Tang, C.; Liu, C.; Fang, P.; Xiang, Y.; Min, R. Work-related accumulated fatigue among doctors in tertiary hospitals: A cross-sectional survey in six provinces of China. Int. J. Environ. Res. Public Health 2019, 16, 3049. [Google Scholar] [CrossRef]
- He, A.J.; Qian, J. Explaining medical disputes in Chinese public hospitals: The doctor-patient relationship and its implications for health policy reforms. Health Econ. Policy Law 2016, 11, 359–378. [Google Scholar] [CrossRef]
- Aurel, B.; Rozalia, K.; Ionel, B. Social Trust and Dynamics of Capitalist Economies in the Context of Clashing Managerial Factors with Risks and Severe Turbulence: A Conceptual Inquiry. Sustainability 2020, 12, 8794. [Google Scholar]
- Helliwell, J.F.; Putnam, R.D. The social context of well-being. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2004, 359, 1435–1446. [Google Scholar] [CrossRef]
- He, A.J. The doctor-patient relationship, defensive medicine and overprescription in Chinese public hospitals: Evidence from a cross-sectional survey in Shenzhen city. Soc. Sci. Med. 2014, 123, 64–71. [Google Scholar] [CrossRef]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A novel coronavirus outbreak of global health concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Ballard, M.; Bancroft, E.; Nesbit, J.; Johnson, A.; Holeman, I.; Foth, J.; Rogers, D.; Yang, J.; Nardella, J.; Olsen, H.; et al. Prioritising the role of community health workers in the COVID-19 response. BMJ Glob. Health 2020, 5, e002550. [Google Scholar] [CrossRef] [PubMed]
- Gilson, L.; Palmer, N.; Schneider, H. Trust and health worker performance: Exploring a conceptual framework using South African evidence. Soc. Sci. Med. 2005, 61, 1418–1429. [Google Scholar] [CrossRef]
- Walton, M.; Murray, E.; Christian, M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 241–247. [Google Scholar] [CrossRef]
- Kawachi, I.; Kennedy, B.P.; Glass, R. Social capital and self-rated health: A contextual analysis. Am. J. Public Health 1999, 89, 1187–1193. [Google Scholar] [CrossRef]
- Subramanian, S.V.; Kim, D.J.; Kawachi, I. Social trust and self-rated health in US communities: A multilevel analysis. J. Urban Health Bull. N. Y. Acad. Med. 2002, 79 (Suppl. S1), S21–S34. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I.; Kennedy, B.P.; Lochner, K.; Prothrow-Stith, D. Social capital, income inequality, and mortality. Am. J. Public Health 1997, 87, 1491–1498. [Google Scholar] [CrossRef]
- DeVoe, J.E.; Bazemore, A.; Cottrell, E.K.; Likumahuwa-Ackman, S.; Grandmont, J.; Spach, N.; Gold, R. Perspectives in Primary Care: A Conceptual Framework and Path for Integrating Social Determinants of Health into Primary Care Practice. Ann. Fam. Med. 2016, 14, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Habibov, N.; Cheung, A.; Auchynnikava, A. Does social trust increase willingness to pay taxes to improve public healthcare? Cross-sectional cross-country instrumental variable analysis. Soc. Sci. Med. 2017, 189, 25–34. [Google Scholar] [CrossRef]
- Buck-McFadyen, E.; Akhtar-Danesh, N.; Isaacs, S.; Leipert, B.; Strachan, P.; Valaitis, R. Social capital and self-rated health: A cross-sectional study of the general social survey data comparing rural and urban adults in Ontario. Health Soc. Care Community 2019, 27, 424–436. [Google Scholar] [CrossRef] [PubMed]
- Dai, X.; Gu, N. The Impact of Social Capital on Mental Health: Evidence from the China Family Panel Survey. Int. J. Environ. Res. Public Health 2022, 19, 190. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Schlesinger, M.; Wang, H.; Hsiao, W.C. The flip-side of social capital: The distinctive influences of trust and mistrust on health in rural China. Soc. Sci. Med. 2009, 68, 133–142. [Google Scholar] [CrossRef]
- Duren, R.; Yalcin, O. Social capital and mental health problems among Syrian refugee adolescents: The mediating roles of perceived social support and post-traumatic symptoms. Int. J. Soc. Psychiatry 2021, 67, 243–250. [Google Scholar] [CrossRef]
- Van der Linden, J.; Drukker, M.; Gunther, N.; Feron, F.; van Os, J. Children’s mental health service use, neighbourhood socioeconomic deprivation, and social capital. Soc. Psychiatry Psychiatr. Epidemiol. 2003, 38, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Forsman, A.K.; Nyqvist, F.; Wahlbeck, K. Cognitive components of social capital and mental health status among older adults: A population-based cross-sectional study. Scand. J. Public Health 2011, 39, 757–765. [Google Scholar] [CrossRef]
- Martinez, L.M.; Estrada, D.; Prada, S. Mental health, interpersonal trust and subjective well-being in a high violence context. SSM-Popul. Health 2019, 8, 100423. [Google Scholar] [CrossRef] [PubMed]
- Roychowdhury, P. Too unwell to trust? The effect of mental health on social trust in Europe. Econ. Hum. Biol. 2021, 42, 101021. [Google Scholar] [CrossRef] [PubMed]
- Diener, E. Subjective well-being. The science of happiness and a proposal for a national index. Am. Psychol. 2000, 55, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Suh, E.M.; Lucas, R.E.; Smith, H.L. Subjective well-being: Three decades of progress. Psychol. Bull. 1999, 125, 276–302. [Google Scholar] [CrossRef]
- Diener, E. Subjective Well-Being. Psychol. Bull. 1984, 95, 542–575. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Zhu, Z. Social trust and emotional health in rural older adults in China: The mediating and moderating role of subjective well-being and subjective social status. BMC Public Health 2021, 21, 556. [Google Scholar] [CrossRef] [PubMed]
- Yip, W.; Subramanian, S.V.; Mitchell, A.D.; Lee, D.T.S.; Wang, J.; Kawachi, I. Does social capital enhance health and well-being? Evidence from rural China. Soc. Sci. Med. 2007, 64, 35–49. [Google Scholar] [CrossRef]
- Chai, X.; Li, X.; Ye, Z.; Li, Y.; Lin, D. Subjective well-being among left-behind children in rural China: The role of ecological assets and individual strength. Child Care Health Dev. 2019, 45, 63–70. [Google Scholar] [CrossRef]
- Diener, E.; Oishi, S.; Tay, L. Advances in subjective well-being research. Nat. Hum. Behav. 2018, 2, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Deaton, A.; Stone, A.A. Subjective wellbeing, health, and ageing. Lancet 2015, 385, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Arslan, G.; Yildirim, M. Meaning-Based Coping and Spirituality During the COVID-19 Pandemic: Mediating Effects on Subjective Well-Being. Front. Psychol. 2021, 12, 646572. [Google Scholar] [CrossRef]
- Yang, Y.; Zhao, L.; Cui, F. How Does Public Health Investment Affect Subjective Well-Being? Empirical Evidence from China. Int. J. Environ. Res. Public Health 2022, 19, 5035. [Google Scholar] [CrossRef]
- Lee, S. Subjective Well-being and Mental Health During the Pandemic Outbreak: Exploring the Role of Institutional Trust. Res. Aging 2022, 44, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; He, M. Social Security Satisfaction and People’s Subjective Wellbeing in China: The Serial Mediation Effect of Social Fairness and Social Trust. Front. Psychol. 2022, 13, 855530. [Google Scholar] [CrossRef]
- Xie, Y.; Hu, J. An Introduction to the China Family Panel Studies (CFPS). Chin. Sociol. Rev. 2014, 47, 3–29. [Google Scholar]
- Sun, X.Y.; Li, Y.X.; Yu, C.Q.; Li, L.M. Reliability and validity of depression scales of Chinese version: A systematic review. Zhonghua Liu Xing Bing Xue Za Zhi 2017, 38, 110–116. [Google Scholar] [PubMed]
- Jen, M.H.; Sund, E.R.; Johnston, R.; Jones, K. Trustful societies, trustful individuals, and health: An analysis of self-rated health and social trust using the World Value Survey. Health Place 2010, 16, 1022–1029. [Google Scholar] [CrossRef]
- Carpiano, R.M.; Fitterer, L.M. Questions of trust in health research on social capital: What aspects of personal network social capital do they measure? Soc. Sci. Med. 2014, 116, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Wirtz, D.; Tov, W.; Kim-Prieto, C.; Choi, D.-W.; Oishi, S.; Biswas-Diener, R. New Well-being Measures: Short Scales to Assess Flourishing and Positive and Negative Feelings. Soc. Indic. Res. 2010, 97, 143–156. [Google Scholar] [CrossRef]
- Landrigan, C.P.; Rothschild, J.M.; Cronin, J.W.; Kaushal, R.; Burdick, E.; Katz, J.T.; Lilly, C.M.; Stone, P.H.; Lockley, S.W.; Bates, D.W.; et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N. Engl. J. Med. 2004, 351, 1838–1848. [Google Scholar] [CrossRef]
- Quon, E.; McGrath, J. Subjective Socioeconomic Status and Adolescent Health: A Meta-Analysis. Health Psychol. 2014, 33, 433–447. [Google Scholar] [CrossRef]
- Adler, N.E.; Epel, E.S.; Castellazzo, G.; Ickovics, J.R. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2000, 19, 586–592. [Google Scholar] [CrossRef]
- Stenlund, S.; Koivumaa-Honkanen, H.; Sillanmäki, L.; Lagström, H.; Rautava, P.; Suominen, S. Changed health behavior improves subjective well-being and vice versa in a follow-up of 9 years. Health Qual. Life Outcomes 2022, 20, 66. [Google Scholar] [CrossRef]
- Wong, C.; Tang, W.; Chang, W.; Hui, C.; Chan, S.; Lee, E.; Chen, E. Constructing socioeconomic index (SEI) in predicting mental health in young adults. Eur. Psychiatry 2021, 64, S118–S119. [Google Scholar] [CrossRef]
- Paradela, R.S.; Ferreira, N.V.; Nucci, M.P.; Cabella, B.; Martino, L.M.; Torres, L.A.; da Costa, D.I.; Consolim-Colombo, F.M.; Suemoto, C.K.; Irigoyen, M.C.; et al. Relation of a Socioeconomic Index with Cognitive Function and Neuroimaging in Hypertensive Individuals. J. Alzheimer’s Dis. 2021, 82, 815–826. [Google Scholar] [CrossRef]
- Henseler, J. Partial least squares path modeling: Quo vadis? Qual. Quant. 2018, 52, 1–8. [Google Scholar] [CrossRef]
- Schuberth, F.; Henseler, J.; Dijkstra, T.K. Confirmatory Composite Analysis. Front. Psychol. 2018, 9, 2541. [Google Scholar] [CrossRef] [PubMed]
- Sarstedt, M.; Ringle, C.M.; Cheah, J.-H.; Ting, H.; Moisescu, O.I.; Radomir, L. Structural model robustness checks in PLS-SEM. Tour. Econ. 2020, 26, 531–554. [Google Scholar] [CrossRef]
- Hair, J.F.; Risher, J.J.; Sarstedt, M.; Ringle, C.M. When to use and how to report the results of PLS-SEM. Eur. Bus. Rev. 2019, 31, 2–24. [Google Scholar] [CrossRef]
- Franke, G.; Sarstedt, M. Heuristics versus statistics in discriminant validity testing: A comparison of four procedures. Internet Res. 2019, 29, 430–447. [Google Scholar] [CrossRef]
- Dijkstra, T.K.; Henseler, J. Consistent Partial Least Squares Path Modeling. Mis Q. 2015, 39, 297–316. [Google Scholar] [CrossRef]
- Chin, W.; Cheah, J.-H.; Liu, Y.; Ting, H.; Lim, X.-J.; Cham, T.H. Demystifying the role of causal-predictive modeling using partial least squares structural equation modeling in information systems research. Ind. Manag. Data Syst. 2020, 120, 2161–2209. [Google Scholar] [CrossRef]
- Aguirre-Urreta, M.I.; Ronkko, M. Statistical Inference with Plsc Using Bootstrap Confidence Intervals. Mis Q. 2018, 42, 1001–1020. [Google Scholar] [CrossRef]
- Shmueli, G.; Sarstedt, M.; Hair, J.F.; Cheah, J.H.; Ting, H.; Vaithilingam, S.; Ringle, C.M. Predictive model assessment in PLS-SEM: Guidelines for using PLSpredict. Eur. J. Mark. 2019, 53, 2322–2347. [Google Scholar] [CrossRef]
- Sharma, P.N.; Shmueli, G.; Sarstedt, M.; Danks, N.; Ray, S. Prediction-oriented model selection in partial least squares path modeling. Decis. Sci. 2018, 52, 567–607. [Google Scholar] [CrossRef]
- Niu, Z.; Hu, L.; Jeong, D.C.; Brickman, J.; Stapleton, J.L. An Experimental Investigation into Promoting Mental Health Service Use on Social Media: Effects of Source and Comments. Int. J. Environ. Res. Public Health 2020, 17, 7898. [Google Scholar] [CrossRef]
- Sugawara, Y.; Tomata, Y.; Sekiguchi, T.; Yabe, Y.; Hagiwara, Y.; Tsuji, I. Social trust predicts sleep disorder at 6 years after the Great East Japan earthquake: Data from a prospective cohort study. BMC Psychol. 2020, 8, 69. [Google Scholar] [CrossRef]
- Ezumah, N.; Manzano, A.; Ezenwaka, U.; Obi, U.; Ensor, T.; Etiaba, E.; Onwujekwe, O.; Ebenso, B.; Uzochukwu, B.; Huss, R.; et al. Role of trust in sustaining provision and uptake of maternal and child healthcare: Evidence from a national programme in Nigeria. Soc. Sci. Med. 2022, 293, 114644. [Google Scholar] [CrossRef]
- Philayrath, P.; Tien, C.; Adrian, B.; Robert, B.; Derrick, S. Social capital, socio-economic status and psychological distress among Australian adults. Soc. Sci. Med. 2006, 63, 2546–2561. [Google Scholar]
- Olwen, B. The relation between Guanxi and Interpersonal trust in the workplace. Integr. Psychol. Behav. Sci. 2022, 56, 385–404. [Google Scholar]
- Nguyen, A.W.; Chatters, L.M.; Taylor, R.J.; Mouzon, D.M. Social Support from Family and Friends and Subjective Well-Being of Older African Americans. J. Hapniess Stud. 2016, 17, 959–979. [Google Scholar] [CrossRef] [PubMed]
- Oliver, H.; Martina, M.; Benjamin, S. Benefits of Having Friends in Older Ages: Differential Effects of Informal Social Activities on Well-Being in Middle-Aged and Older Adults. J. Gerontol. Ser. B-Psychol. Sci. Soc. Sci. 2014, 69, 366–375. [Google Scholar]
- Zhang, R.J. Social trust and satisfaction with life: A cross-lagged panel analysis based on representative samples from 18 societies. Soc. Sci. Med. 2020, 251, 112901. [Google Scholar] [CrossRef] [PubMed]
- Dahai, Z.; Zhiruo, Z. Changes i public trust in physicians: Empirical evidence from China. Front. Med. 2019, 13, 504–510. [Google Scholar]
- Han, Y.; Lie, R.K.; Li, Z.; Guo, R. Trust in the doctor-patient relationship in Chinese public hospitals: Evidence for hope. Patient Prefer. Adherence 2022, 16, 647–657. [Google Scholar] [CrossRef]
- Wang, Z.; Koenig, H.G.; Tong, Y.; Wen, J.; Sui, M.; Liu, H.; Zaben, F.A.; Liu, G. Moral injury in Chinese health professional during the COVID-19 pandemic. Psychol. Trauma Theory Res. Pract. Policy 2021, 14, 250–257. [Google Scholar] [CrossRef]
- Tao, S.; Jinghui, W.; Shu’e, Z.; Yu, S.; Bei, L.; Xiaohe, W. Status, causes and consequences of physicians’ self-perceived professional reputation damage in China: A crosssectional survey. BMC Health Serv. Res. 2021, 21, 1–3. [Google Scholar]
- Burns, R.A.; Anstey, K.J.; Windsor, T.D. Subjective well-being mediates the effects of resilience and mastery on depression and anxiety in a large community sample of young and middle-aged adults. Aust. N. Z. J. Psychiatry 2011, 45, 240–248. [Google Scholar] [CrossRef]
- Lai, C.; Mak, K.; Watanabe, H.; Jeong, J.; Kim, D.; Bahar, N.; Ramos, M.; Chen, S.; Cheng, C. The mediating role of Internet addiction in depression, social anxiety, and psychosocial well-being among adolescents in six Asian countries: A structural equation modelling approach. Public Health 2015, 129, 1224–1236. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Martin, P.; Poon, L.W.; Centenarian, S.G. Successful aging and subjective well-being among oldest-old adults. Gerontol. 2015, 55, 132–143. [Google Scholar] [CrossRef]
- Veronese, G.; Mahamid, F.A.; Bdier, D. Subjective well-being, sense of coherence, and posttraumatic growth mediate the association between COVID-19 stress, trauma, and burnout among Palestinian health-care providers. Am. J. Orthopsychiatry 2022, 92, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Zou, H.; Xiong, Q.; Xu, H. Does Subjective Social Status Predict Self-Rated Health in Chinese Adults and Why? Soc. Indic. Res. 2020, 152, 443–471. [Google Scholar] [CrossRef]
- Thomson, R.M.; Igelström, E.; Purba, A.K.; Shimonovich, M.; Thomson, H.; McCartney, G.; Reeves, A.; Leyland, A.; Pearce, A.; Katikireddi, S.V. How do income changes impact on mental health and wellbeing for working-age adults? A systematic review and meta-analysis. Lancet Public Health 2022, 7, e515–e528. [Google Scholar] [CrossRef]
- Xu, W.; Sun, H.; Zhu, B.; Bai, W.; Yu, X.; Duan, R.; Kou, C.; Li, W. Analysis of Factors Affecting the High Subjective Well-Being of Chinese Residents Based on the 2014 China Family Panel Study. Int. J. Environ. Res. Public Health 2019, 16, 2566. [Google Scholar] [CrossRef]
- Jing, Y. Research on the current situation and improvement strategy of medical prsonnel salary level in China. Chin. Health Econ. 2018, 37, 17–21. [Google Scholar]
- Hu, N.; Deng, H.; Yang, H.; Wang, C.; Cui, Y.; Chen, J.; Wang, Y.; He, S.; Chai, J.; Liu, F.; et al. The pooled prevalence of the mental problems of Chinese medical staff during the COVID-19 outbreak: A meta-analysis. J. Affect. Disord. 2022, 303, 323–330. [Google Scholar] [CrossRef]
- Melnyk, B.M.; Hsieh, A.P.; Tan, A.; Teall, A.M.; Weberg, D.; Jun, J.; Gawlik, K.; Hoying, J. Associations Among Nurses’ Mental/Physical Health, Lifestyle Behaviors, Shift Length, and Workplace Wellness Support During COVID-19: Important Implications for Health Care Systems. Nurs. Adm. Q. 2022, 46, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.C.; Hoe, V.C.W.; Darus, A.; Bhoo-Pathy, N. Association between night-shift work, sleep quality and health-related quality of life: A cross-sectional study among manufacturing workers in a middle-income setting. BMJ Open 2020, 10, e034455. [Google Scholar] [CrossRef] [PubMed]
- Xuexue, D.; Xuelian, L.; Ronghua, F. Evaluation of the correlation between job stress and sleep quality in community nurses. Medicine 2020, 99, e1882. [Google Scholar]
- Meher, K.; Mushtaq, M.; Fatima, S. Death Anxiety and WellBeing in Doctors During COVID-19: The Explanatory and Boosting Roles of Sleep Quality and Work Locality. Omega 2022, 302228221078074. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).