Abstract
This review aimed to investigate the effects of exercise and exercise with joint mobilization on shoulder range of motion (ROM) and subjective symptom recovery in patients with adhesive capsulitis (AC). Related Studies published from 2000 to 2021 that were peer-reviewed and for which pre-and post-values could be calculated were extracted from PubMed, CINAHL, SPORTDiscus, and Web of Science. Nine studies met our inclusion criteria. As a result of calculating the standard mean difference (SMD) and 95% confidence intervals (CI), both exercise and exercise with joint mobilization showed a large effect on shoulder ROM and subjective outcomes. The combination showed a more significant effect than exercise alone on shoulder flexion (SMD = −1.59 [−2.34, −0.65]), extension (SMD = −1.47 [−2.05, −0.89]), internal rotation (SMD = −1.77 [−2.17, −1.36], external rotation (SMD = −2.18 [−2.92, −1.44]), and abduction ROM (SMD = −1.99 [CI −3.86, −0.12]). Patients who performed exercise alone showed a higher effect of improvement in subjective function (SMD = 3.15 [2.06, 4.24]) and pain (SMD = 4.13 [1.86, 6.41]). Based on these results, an AC rehabilitation exercise program should be developed by adjusting the amount of exercise and joint mobilization by identifying the patient’s needs, subjective symptoms, and ROM.
1. Introduction
Adhesive capsulitis (AC), also referred to as frozen shoulder, involves progressive thickening and shrinkage of the glenohumeral joint capsule [1,2]. Approximately 2–5% of the world’s population experiences AC [3]. AC occurs more commonly in women aged 40–60 years and in sedentary workers than in manual workers [4]. AC progresses through the pre-adhesion, acute adhesive, maturation, and chronic stages [4], and symptoms vary according to the stage. Nocturnal pain occurs in the pre-adhesion stage, and there is no decrease in the shoulder range of motion (ROM); however, a loss of motion begins to appear in the acute adhesive stage. Pain decreases in the maturation stage compared to that in the previous stage within the ROM; however, the motion is further reduced as it reaches the chronic stage when adhesions have fully progressed, and pain occurs when arm movement exceeds the restricted ROM [5]. In particular, a prolonged period of limited movement of the affected shoulder can cause weakening of muscles, tendons, ligament contraction [6], impaired muscle coactivation, and proprioception of the shoulder [7]. In addition, due to thickening of the coracohumeral ligament, external rotation is limited, and, as it also affects the subscapular and supraspinatus tendons, internal rotation can also be restricted [8,9,10]. If AC is left unattended and progresses to more advanced stages, the thickening and contraction of the glenohumeral capsule ends occurs, with limited shoulder ROM in all directions [11,12]. As such, decreased ROM accompanied by pain reduces the quality of life by restricting daily living activities, such as washing the back, making the bed, pulling the car seat belt, working, and several leisure activities [13,14,15]. Therefore, recovery through appropriate intervention is necessary.
It is essential to design movements to alleviate symptoms in patients with AC. Exercise and manual therapy approaches, such as joint mobilization [16,17], have been used to reduce pain and improve patients’ ROM and function. Exercises designed to improve function and ROM can improve shoulder joint stability, mobility, and proprioception [18]. In a systematic review examining the effect of physiotherapy for AC [2], stretching along with administration of corticosteroid injection, physical therapy, and other modalities was effective in relieving pain and improving ROM and shoulder function in patients with stage 2–3 AC. Meanwhile, in a meta-analysis of the effect of joint mobilization on the recovery of shoulder ROM, conducting joint mobilization yielded an increase in ROM by 20.14° greater than that of the control group with respect to shoulder abduction and external rotation. Furthermore, a medium effect was observed, suggesting that joint mobilization was effective in restoring ROM and relieving pain [19]. In addition, mobilization of peripheral somatosensory receptors and suppression of nociceptors resulted in decreased pain and increased shoulder mobility by enhancing the exchange between synovial fluid and cartilage [20,21]. Thus, exercise and mobilization could be effective interventions in patients with AC.
However, as indicated in a few studies, the exercise and joint mobilization results for AC are contradictory to those reported in previous studies. For example, [22] indicated that stretching with glenohumeral joint distraction and glide toward caudal, posterior, and anterior directions significantly improved the range of shoulder flexion and abduction in patients with AC compared to stretching alone. In contrast, [23] reported decreased pain but no significant group difference between exercise and exercise with Maitland mobilization technique in grade II and III. Likewise, posterior gliding improves shoulder ROM in all directions except abduction, and the mechanism of elevation of the humeral head and the increase in the thickness of the inferior fibers of the joint capsule has been elucidated, but, compared to the control group, a significant increase in abduction ROM of 20.14 degrees has also been reported [21,24,25]. Therefore, joint mobilization may be effective for ROM recovery and pain reduction, but several studies have revealed that the evidence is not conclusive [19]. These conflicting results suggest the importance of establishing an evidence-based decision on whether to intervene only with exercise or to add joint mobilization.
Because exercise can be easily performed in daily life, it is desirable to prevent financial waste by judging when joint mobilization is unnecessary. Therefore, to make efficient clinical decisions, analysis of the effects of exercise alone versus exercise combined with other interventions is essential.
This review aimed to present a comprehensive conclusion considering AC patients’ objective indicators, such as shoulder ROM, subjective function measured by a questionnaire, and degree of pain. In addition, this study aimed to present a more generalized conclusion on the impact of an exercise intervention on symptom improvement by analyzing previous studies on the effects of exercise and joint mobilization in patients with AC. By comparing the effects of exercise and exercise plus joint mobilization, implications for efficient intervention in the field of exercise prescription can be presented.
2. Methods
A systematic search was conducted to investigate the effects of exercise and a combination of exercise and joint mobilization in patients with AC according to the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [26]. In this review, the following research questions were set: 1. Investigation of the effect of exercise and exercise with joint mobilization on shoulder ROM and subjective function in AC patients. 2. Comparison of effects according to whether or not joint mobilization is applied to exercise.
2.1. Literature Search Strategy
A comprehensive literature search was performed to identify peer-reviewed articles. We systematically searched PubMed, CINAHL, SPORTDiscus, and Web of Science electronic databases for papers published from January 2000 to November 2021. The period of collection and screening of papers was from June to November 2021. We used a keyword search and the medical subject headings vocabulary. The search was limited to studies involving humans, written in English, and reported in peer-reviewed journals. The search terms were as follows: adhesive capsulitis, frozen shoulder, frozen shoulders, adhesive capsulitides, shoulder, periarthritis, stiff, shoulder stiffness, contracted, restricted, peri capsulitis, shoulder pain, fibrosis, irritative, AND exercise, sport, sports, training, stretching, rehabilitation, intervention; NOT calcific tendinitis, rotator cuff tear, rotator cuff rupture, SLAP, labral tear, labral rupture, biceps tendinitis, Bankart, impingement, tear, and rupture. We limited the scope of the search to the case where the full text was retrieved from each database. In addition, while using PubMed, we searched by setting “Article Type” to “Randomized controlled trial” and “Clinical Trial”, and “Books and Documents”, “Meta-Analysis”, “Review”, and “Systematic review” set to exclude. In CINAHL and SPORTDiscus, we set “Source Types” to “Academic Journals”, in Web of Science we set “Document Types” to “Articles”, and in “Quick Filters” we set “Review Article” and “Early Access” to exclude. A manual search for relevant references was performed on all systematically retrieved studies, and the identified articles were screened by two independent authors (J.H.L. and H.G.J) who specialize in sports rehabilitation.
2.2. Eligibility Criteria
The inclusion and exclusion criteria described in the following paragraphs were assessed by the investigators using the eligibility of the articles identified in the systematic search.
2.2.1. Inclusion Criteria
The inclusion criteria used to select and screen studies were as follows:
- A peer-reviewed study published in English between 2000 and 2021 investigating the effect of exercise and joint mobilization in patients with AC;
- Outcome variables including shoulder ROM, subjective function, and pain;
- Studies in which the results were described or converted to mean and standard deviation.
2.2.2. Exclusion Criteria
The exclusion criteria used to screen out studies were as follows:
- Case studies using a single-subject design;
- Studies that did not definitively establish that the participants were patients with AC;
- Studies in which interventions other than exercise and/or exercise with joint mobilization were added and applied as confounding variables (e.g., injection, operation, drug, ultrasound).
2.3. Assessment of Methodologic Quality
The authors assessed the quality of included studies using the National Heart, Lung, and Blood Institute Quality Assessment Tool (NHLBI-QAT, https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools, accessed on 15 February 2022). The checklist includes 11 questions and indicates the total score as a percentage. Two authors independently reviewed the full text of the selected studies for quality analysis. Discrepancies in screening and scoring were addressed through collaboration between the authors until a consensus was reached. If a consensus could not be reached, any conflicts of opinion were resolved by a third reviewer (corresponding author of this review who is an expert in meta-analysis and other research methodologies). The screened studies were classified into levels 1–3 according to the study quality. In this present review, NHLBI scores ≥ 70%, 40% < NHLBI scores < 70%, and ≤40% were considered levels of evidence 1, 2, and 3, respectively.
2.4. Assessment of Publication Bias
After reviewing the meta-analysis data using a forest plot, the asymmetry of the effect size was visually assessed using a funnel plot. In addition, the relationship between effect size and standard error was verified using Egger’s regression to determine whether the funnel plot was asymmetric. In the case of asymmetry, we calculated the average effect size obtained by adjusting the asymmetry using the trim-and-fill method and compared it with the original average effect size [27].
2.5. Data Synthesis and Extraction
To calculate the standard mean difference (SMD) and 95% confidence intervals (CIs), means, standard deviations pre-and post-intervention, and numbers were extracted from each study. The review process was performed by assessing the aims and quality of the studies, characteristics, inclusion and exclusion criteria of the subjects, intervention procedures, and outcome variables. The significance of heterogeneity varied depending on the I2 value: high (≥75%), medium (≥25%, <75%), and low (<25%). A random-effects model was used in the meta-analysis to generalize the results of the independent studies. We used R-Studio software (Version 4.0.2, R-Studio, Boston, MA, USA) with the “metafor” package to calculate SMD and assess publication bias through forest and funnel plots. Cohen’s d was used to calculate and determine the effect size [28]; the CIs for the effect size was 95%, and the significance level was 0.05. A fixed-effects model was used to estimate the overall effect when homogeneity test statistics were insignificant. When the heterogeneity was p ≤ 0.05, a random-effects model was used, including the restricted maximum likelihood estimation method.
3. Results
3.1. Study Selection
The flowchart presented in Figure 1 follows the PRISMA guidelines. The first search identified 5136 relevant studies. After screening, nine studies were included in the meta-analysis. However, no additional studies were identified after examining the references of the pooled studies. Table 1 and Table 2 present methodological summaries of the included studies.
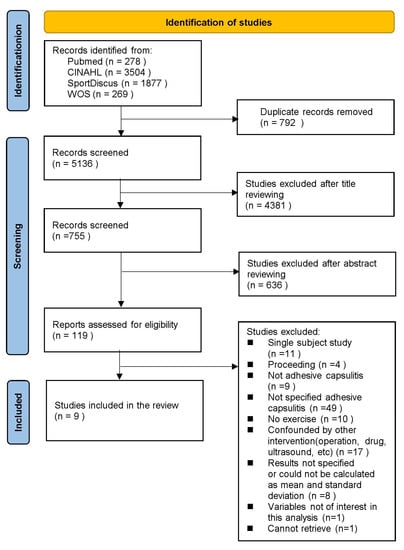
Figure 1.
Flow chart of the selection process for studies.

Table 1.
Characteristics of studies with exercise intervention.

Table 2.
Characteristics of studies with exercise intervention and joint mobilization.
3.2. Level of Evidence and Strength of Recommendation
The average methodological quality of the included studies was 8.8 out of a possible 11 (range 6–10; Table 3). Seven studies [22,29,31,32,34,35,36] were classified as Level 1 with an average NHLBI score of 9.4, while 2 studies [30,33] were classified as Level 2 with an average NHLBI score of 6.5 (Table 3). Regarding grading according to variables, grade A was assigned when consistent results were obtained in most pooled studies with high-quality RCT designs. Grade B was assigned if most of the studies included in each variable had case-control or comparative experimental research designs. Therefore, only the pain variable was classified as grade A based on the effects of exercise. In contrast, flexion, extension, internal rotation, external rotation, abduction ROM, and subjective function variables were classified as grade B. The effects of a combination of exercise and joint mobilization, flexion, extension, internal rotation, external rotation ROM, and pain variables were graded as A, whereas abduction ROM and subjective function were graded as B.

Table 3.
Quality assessment of studies.
3.3. Publication Bias
Egger’s regression analysis, which was conducted to determine the symmetry of the funnel plot (Figure 2 and Figure 3), confirmed that flexion (p = 0.14), extension (p = 0.62), and internal rotation (p = 0.24) ROM variables in studies investigating the effects of exercise showed symmetry, indicating no publication error.
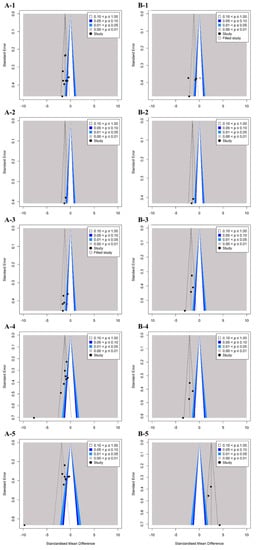
Figure 2.
Funnel plots of standard error by each shoulder range of motion for the studies included in the meta-analysis. Funnel plots of exercise effect on flexion (A-1), extension (A-2), internal rotation (A-3), external rotation (A-4), and abduction range of motion (A-5). Funnel plots combination effect on flexion (B-1), extension (B-2), internal rotation (B-3), external rotation (B-4), and abduction range of motion (B-5).
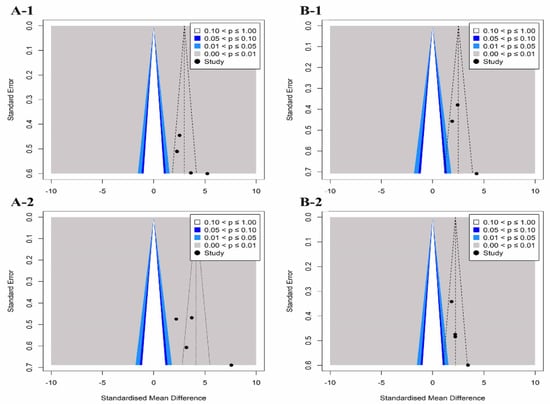
Figure 3.
Funnel plots of standard error by each patient-oriented outcome for the studies included in the meta-analysis. Funnel plots of exercise effect on subjective function (A-1) and pain (A-2). Funnel plots of combination effect on subjective function (B-1) and pain (B-2).
In studies exploring the effects of a combination of exercise and joint mobilization, extension (p = 0.56), internal rotation (p = 0.07), ROM, and pain (p = 0.12) had no publication errors.
In contrast, in studies investigating the effects of exercise, asymmetry of external rotation (p < 0.01), abduction ROM (p < 0.01), subjective function (p < 0.01), and pain (p < 0.01) were noted, and publication errors were confirmed. Studies exploring the effects of a combination of exercise and joint mobilization, flexion and abduction ROM, and subjective function variables have shown asymmetry and publication errors. Therefore, we applied the trim-and-fill method to these variables and confirmed the effect of publication errors on the research results. When comparing the existing SMD with the adjusted SMD, the difference was <10%. Therefore, it can be concluded that publication errors had less effect on the results of this study.
3.4. Data Synthesis
The analysis effect size showed that both exercise and exercise combined with joint mobilization showed a large effect on shoulder ROM, subjective function, and pain recovery. The pooled effect size for each variable is summarized in Figure 4.
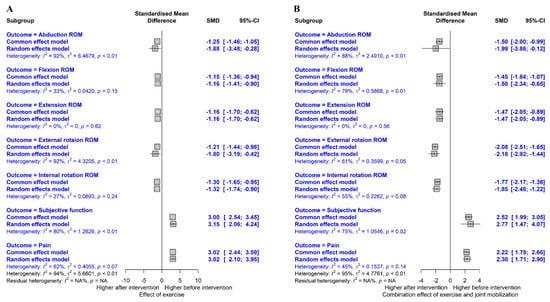
Figure 4.
Summary of meta-analysis results. Effect of exercise (A) and combination effect of exercise and joint mobilization (B).
3.4.1. Flexion ROM
Figure 5A shows the overall effect size measures for the effect of exercise on flexion ROM in patients with AC using a forest plot (k = 9, Q(8) = 11.96, p = 0.153, I2 = 33%). Under the fixed-effects model, the overall difference in exercise on flexion ROM was statistically significant (SMD = −1.15, 95% CIs = −1.36 to −0.94), indicating that exercise significantly improved flexion ROM in patients with AC compared to pre-exercise (large effect size).
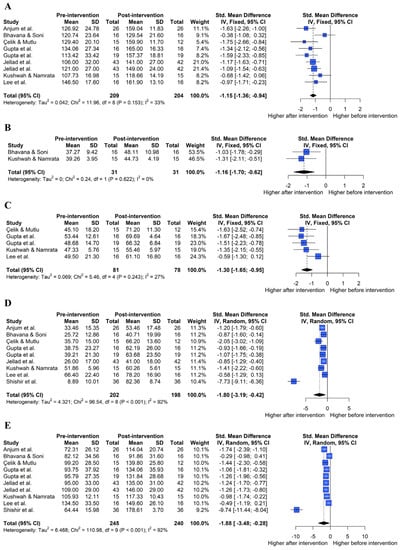
Figure 5.
Effect of exercise on shoulder range of motion in forest plots of the meta-analysis. Flexion (A), extension (B), internal rotation (C), external rotation (D), and abduction range of motion (E) [22,29,30,31,32,33,34,36].
The effect of the combination of exercise and joint mobilization on flexion ROM was assessed (Figure 6A; k = 4, Q(3) = 14.35, p = 0.002, I2 = 79%). Under the random-effects model, the overall effect of a combination of exercise and joint mobilization on flexion ROM was statistically significant (SMD = −1.50, 95% CIs = −2.34 to −0.65), indicating that a combination of the two interventions led to the improvement of flexion ROM in patients with AC compared with pre-intervention (large effect size).
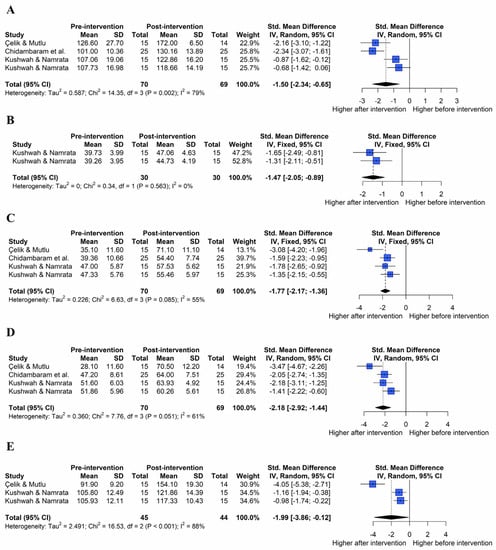
Figure 6.
Effect of a combination of exercise and joint mobilization on shoulder range of motion in forest plots of the meta-analysis. Flexion (A), extension (B), internal rotation (C), external rotation (D), and abduction range of motion (E) [22,35,36].
3.4.2. Extension ROM
Figure 5B shows the overall effect size measures of the effect of exercise on extension ROM in patients with AC (k = 2, Q(1) = 0.24, p = 0.622, I2 = 0%). Under the fixed-effects model, the overall difference in exercise on extension ROM was statistically significant (SMD = −1.16, 95% Cis = −1.70 to −0.62), indicating that exercise led to the improvement of extension ROM in patients with AC compared to pre-exercise (large effect size).
The effect of the combination of exercise and joint mobilization on extension ROM was assessed (Figure 6B; k = 2, Q(1) = 0.34, p = 0.563, I2 = 0%). Under the fixed-effects model, the overall effect of a combination of exercise and joint mobilization on extension ROM was statistically significant (SMD = −1.47, 95% CIs = −2.05 to −0.89), indicating that a combination of the two interventions improved extension ROM in patients with AC compared with pre-intervention (large effect size).
3.4.3. Internal Rotation ROM
Figure 5C shows the overall effect size measures of the effect of exercise on internal rotation ROM in patients with AC (k = 5, Q(4) = 5.46, p = 0.243, I2 = 27%). Under the fixed-effects model, the overall difference in exercise on internal rotation ROM was statistically significant (SMD = −1.30, 95% CIs = −1.65 to −0.95), indicating that exercise improved the internal rotation ROM in patients with AC compared to pre-exercise (large effect size).
The effect of the combination of exercise and joint mobilization on internal rotation ROM was assessed (Figure 6C; k = 4, Q(3) = 6.63, p = 0.085, I2 = 55%). Under the fixed-effects model, the overall effect of a combination of exercise and joint mobilization on internal rotation ROM was statistically significant (SMD = −1.77, 95% CIs = −2.17 to −1.36), indicating that a combination of the two interventions improved internal rotation ROM in patients with AC compared with pre-intervention (large effect size).
3.4.4. External Rotation ROM
Figure 5D shows the overall effect size measures for the effect of exercise on external rotation ROM in patients with AC (k = 9, Q(8) = 96.54, p < 0.001, I2 = 92%). Under the random-effects model, the overall difference in exercise on external rotation ROM was statistically significant (SMD = −1.80, 95% CIs = −3.19, −0.42), indicating that exercise improved external rotation ROM in patients with AC compared to pre-exercise (large effect size).
The effect of the combination of exercise and joint mobilization on external rotation ROM was assessed (Figure 6D; k = 4, Q(3) = 7.76, p = 0.051, I2 = 61%). Under the random-effects model, the overall effect of the combined exercise and joint mobilization on external rotation ROM was statistically significant (SMD = −2.18, 95% CIs = −2.92 to −1.44), indicating that a combination of the two interventions improved external rotation ROM in patients with AC compared with pre-intervention (large effect size).
3.4.5. Abduction ROM
Figure 5E shows the overall effect size measures of the effect of exercise on abduction ROM in patients with AC (k = 10, Q(9) = 110.98, p < 0.001, I2 = 92%). Under the random-effects model, the overall difference in exercise on abduction ROM was statistically significant (SMD = −1.88, 95% CIs = −3.48, −0.28), indicating that exercise improved abduction ROM in patients with AC compared to pre-exercise (large effect size).
The effect of the combination of exercise and joint mobilization on abduction ROM was assessed (Figure 6E; k = 3, Q(2) = 16.53, p < 0.001, I2 = 88%). Under the random-effects model, the overall effect of a combination exercise and joint mobilization on abduction ROM was statistically significant (SMD = −1.99, 95% CIs = −3.86, −0.12), indicating that a combination of the two interventions improved abduction ROM in patients with AC compared to pre-intervention (large effect size).
3.4.6. Subjective Function
Figure 7A shows the overall effect size measures of the effect of exercise on subjective function in patients with AC (k = 5, Q(4) = 20.15, p < 0.001, I2 = 80%). Under the random-effects model, the overall effect of exercise on subjective function was statistically significant (SMD = 3.15, 95% CIs = 2.06 to 4.24), indicating that exercise improved subjective function in patients with AC compared to pre-exercise (large effect size).
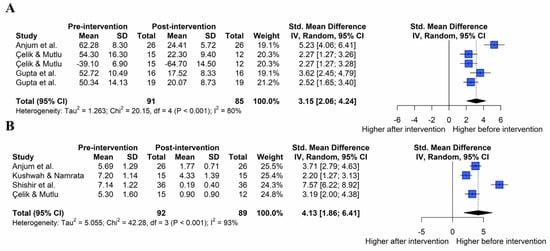
Figure 7.
Effect of exercise on patient-oriented outcome in forest plots of the meta-analysis. Subjective function (A) and pain (B) [22,29,31,34,36].
The effect of the combination of exercise and joint mobilization on subjective function was assessed (Figure 8A; k = 3, Q(2) = 8.10, p = 0.017, I2 = 75%). Under the random-effects model, the overall effect of a combination of exercise and joint mobilization on subjective function was statistically significant (SMD = 2.22, 95% CIs = 1.47 to 4.07), indicating that a combination of the two interventions improved subjective function in patients with AC compared to pre-intervention (large effect size).
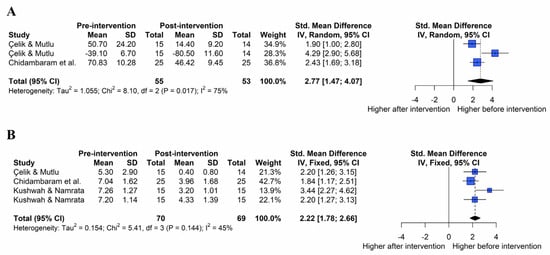
Figure 8.
Effect of a combination of exercise and joint mobilization on patient-oriented outcome in forest plots of the meta-analysis. Subjective function (A) and pain (B) [22,35,36].
3.4.7. Pain
Figure 7B shows the overall effect size measures of the effect of exercise on pain in patients with AC (k = 4, Q(3) = 42.28, p < 0.001, I2 = 93%). Under the random-effects model, the overall effect of exercise on pain was statistically significant (SMD = 4.13, 95% CIs = 1.86 to 6.41), indicating that exercise improved pain in patients with AC compared with pre-exercise (large effect size).
The effect of the combination of exercise and joint mobilization on pain was assessed (Figure 8B; k = 4, Q(3) = 5.41, p = 0.144, I2 = 45%). Under the fixed-effects model, the overall effect of a combination of exercise and joint mobilization on pain was statistically significant (SMD = 2.22, 95% CIs = 1.78 to 2.66), indicating that a combination of the two interventions improved pain in patients with AC compared to pre-intervention (large effect size).
4. Discussion
This study aimed to suggest an integrated conclusion on the effect of exercise and exercise with joint mobilization on patients with AC by performing a systematic review and meta-analysis. Nine studies were analyzed, and, as the overall effect size was >0.8, we concluded that exercise and exercise combined with mobilization could be effective interventions to recover function and ROM and relieve pain. In addition, a greater effect on shoulder ROM recovery was shown when joint mobilization was added to exercise. On the contrary, subjective function (shoulder pain and disability index (SPADI), disabilities of arm, shoulder, and hand (DASH), and constant shoulder score) and pain were further improved with exercise without joint mobilization. The results are as follows.
4.1. Effect on Shoulder ROM
AC causes a reduction in external shoulder rotation ROM, which indicates that the inter-rotator cuff and the coracohumeral ligament are aggravated; therefore, exercises including joint stretching should be applied [37]. In this review, a study [30] that applied the CHL stretch, while grabbing a dowel with adducted and hyperextended humerus and forearm supinated in the side-lying position on the unaffected arm, showed a significant effect size (0.87). In particular, previous studies [22,29] have shown that the effect was greater when strength exercises were combined. These results contradict those of previous studies [38], which inferred that strength exercises were unnecessary. Alternatively, the necessity of concurrent strength exercises to recover external rotation ROM was highlighted. In addition, a previous study [22] showed that the addition of glenohumeral joint distraction, caudal glide, posterior glide, and anterior glide to scapulothoracic and rotator cuff muscular strength exercise were ideal intervention methods for restoring external shoulder rotation and abduction ROM (grade I or II rhythmic oscillations were used in the first 2 weeks, and grade III and IV oscillation techniques were used in the following week.) These effects are thought to be due to not only securing PROM through joint mobilization but also the recovery of the dynamic musculoskeletal system through active muscle strength exercise. However, active-ROM and passive-ROM restriction of the glenohumeral joint due to AC is often multidirectional in practice [11,12]. Although this review showed that all three axes of shoulder ROM improved, it is difficult for this to be explained by a functional anatomical viewpoint based on this evidence. Since studies on connective tissues involved in ROM other than external rotation remain scarce, follow-up studies are deemed necessary.
4.2. Effect on Shoulder Subjective Function and Pain
If the cost-effectiveness of AC patients is considered, the importance of autonomy may increase; in fact, several studies have reported that participants who exercised showed better results regardless of whether other treatments were combined [39]. A previous study reviewing AC [5] showed that the recovery of AC yields better subjective results than objective indicators. In this study, exercise without joint mobilization had a greater effect on subjective function (SPADI, DASH, and constant shoulder score) and pain relief. Unlike passive exercises, such as mobilization by a therapist, the patient could recognize pain-free ROM well through active exercise, and the patient was self-aware and actively created motion by contracting and relaxing the muscles, thus restoring proprioception and kinesthesia. Therefore, these results could be explained by the feeling of being liberated from discomfort in daily life. In fact, AC patients in the ‘frozen’ phase had satisfactory results after applying stretching in the direction of external rotation, internal rotation, and horizontal adduction with tolerable intensity [40]. However, in a state where pain remains due to AC, the stretching intensity should be adjusted according to the degree of pain, and, for this, the stimulation sensitivity of each patient should be considered [39]. Low sensitivity to stimuli means that stiffness of the joint is felt relatively more strongly than pain, so it responds better to more intense movements or stretching. For AC patients with this type, more aggressive exercise interventions could be implemented so there is a possibility of better recovery. However, in the case of high stimulation sensitivity, since pain is felt more strongly than stiffness, exercise intervention is considered to be performed cautiously, and there are no guidelines based on solid evidence. Therefore, ultrasound, iontophoresis, and phonophoresis may be recommended, and it has been found that when these patients received ultrasound treatment, ROM improved, but there was no improvement in pain or function [41,42]. Therefore, a cognitive improvement program that can lower stimuli sensitivity should be developed and applied so that patients can better accept exercise interventions.
4.3. Implications of Virtual Reality Training and Coracohumeral Ligament Stretching
High adherence should be induced to maximize the efficiency of the prescribed exercise program for AC. In one study [40], participants were instructed to exercise five times a day but actually showed compliance with an average of two times a day. Hence, a sufficient dose of exercise intervention could be applied when patient interest is aroused. As such, virtual reality (VR) training could be an enjoyable and interesting approach for AC patients. However, analyzing the research of applying VR training [33] in this review showed that the effect sizes of internal rotation, external rotation, and abduction were small compared to those in other studies and were not statistically significant. Hence, developing and modifying the existing VR program is necessary to pique the interest of patients with AC and drive better ROM recovery. Furthermore, when coracohumeral ligament stretching, which was found to improve external shoulder rotation ROM [37,43], was applied, the effect size for the recovery of shoulder flexion and abduction ROM was not significant [30]. Since shoulder flexion and abduction play an essential role in picking up objects overhead or enjoying leisure activities requiring considerable overhead movement (e.g., racquet sports), joint stretching in various directions besides the CHL should be applied to AC patients. Accordingly, a study that performed stretching of the anterior, posterior, and antero-inferior capsules [36] was analyzed, but the effect size was not significant in shoulder flexion ROM recovery. If restoration of the shoulder flexion ROM is given priority, the proportion of exercises not directly related to the shoulder, such as sit-to-stand, must be reduced, and, in addition to the joint capsule, treatment for shoulder flexor muscles such as the anterior deltoid, pectoralis major, serratus anterior, and upper and lower trapezius muscles [44] seems necessary.
4.4. Overall Implications and Limitations
This study aimed to create a framework for a protocol that enables efficient treatment by selectively applying exercises and joint mobilization, which can be used conservatively.
Exercise does not generally incur any cost and for most individuals can be easily practiced in daily life. This review indicates the significant effectiveness of exercise for patients with AC. In addition, by comprehensively investigating the ROM of the shoulders of patients with AC and subjective indices, data for an evidence-based exercise program were presented. Based on the results of this review, interventions including exercise should be preferentially performed, particularly for pain relief. However, they can be more effective in improving ROM when combined with joint mobilization by clinicians. However, a limitation of this study is that it is difficult to analyze subgroups according to the type of exercise performed, as all types of exercises are based on a certain protocol, and a comparative study on the effect according to the stage of frozen shoulder and the presence or absence of comorbidities is required. In addition, as shown from the quality assessment of the studies presented in Table 3, information on adherence to exercise intervention was not found in the studies included in this review. Therefore, further research is required to determine the degree of exercise program practice in patients with AC. In addition, there are several interventions, such as injection and transcutaneous electric nerve stimulation, in addition to exercise, for the treatment of AC. However, since this review only investigated the net effect of exercise, it could not explain the case when interventions other than exercise and joint mobilization were additionally applied. Furthermore, since the focus was on presenting the integrated viewpoint, low-score studies were also included in the analysis in the risk of bias evaluation process, and blindness of individual studies was also not considered; therefore, caution is required when interpreting the results. In addition, since the literature published before 2000 was not included in the analysis, the possibility of bias in the process of deriving the pooled effect size cannot be excluded. Finally, since the literature search protocol of this study was conducted in an unregistered state, it is suggested that follow-up research proceeds after registering the research protocol with an institution such as PROSPERO.
Dogru, Basaran, and Sarpel [41] reported that when patients with AC received ultrasound treatment, their ROM improved, but there was no pain or functional improvement. Moreover, Jewell, Riddle, and Thacker [42] reported that the ion transfer-phonophoresis method and ultrasonic therapy massage reduced the improvement in function in 19–32% of patients. Therefore, it is suggested that interventions other than exercise can vary, but exercise and joint mobilization should be included in the rehabilitation of patients with AC. Therefore, as future comparisons between various intervention strategies are required, individual studies should be conducted to gather sufficient evidence. In addition, the characteristics of the participants, such as racial differences and comorbidities, were not considered. An epidemiological study showed that the Black/African American and Hispanic/Latino populations are more likely to develop AC [45]. In addition, as AC occurs more frequently in patients with cerebrovascular accidents, myocardial infarction, and diabetes mellitus [46,47,48], it is necessary to consider the characteristics of these patients. Regarding ROM, many studies in our meta-analysis did not specify the measurement method; hence, they were integrated and analyzed. However, the difference between active and passive ROM was reported by Jellad et al. [32]; hence, caution is warranted when interpreting the results. In addition, the progression stage of AC was not considered, and the exercise protocol and dose of mobilization were not specified; thus, considering these limitations, analysis was not possible.
5. Conclusions
In this study, we aimed to comprehensively investigate the effects of exercise combined with joint mobilization, a conservative rehabilitation method, on ROM and subjective symptom recovery in patients with frozen shoulder. The following conclusions were drawn (by comparing the differences) to provide evidence for the selection of an effective intervention method. First, exercise and exercise with joint mobilization both had significant effects on the recovery of shoulder flexion, extension, internal rotation, external rotation, abduction ROM, pain, and subjective function improvement in patients with AC. Second, our results indicate that, to recover ROM, the effect increases only when joint motion therapy is applied to exercise therapy. To eliminate subjective discomfort in daily life, including pain, it is desirable to configure the rehabilitation protocol to include only exercise. Therefore, it is appropriate to construct an AC rehabilitation exercise program by identifying all patient symptoms and objective indicators and adjusting the weight of exercise and joint mobilization to reflect patient-specific needs.
Author Contributions
Conceptualization, J.H.L. and Y.J.Y.; methodology, H.G.J. and Y.J.Y.; software, H.G.J.; validation, J.H.L., H.G.J. and Y.J.Y.; formal analysis, J.H.L. and H.G.J.; funding acquisition, J.H.L. and Y.J.Y.; data curation, J.H.L.; manuscript preparation, J.H.L. and H.G.J.; supervision, Y.J.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the BK21 FOUR (Fostering Outstanding Universities for Research) funded by the Ministry of Education (MOE, Korea) and National Research Foundation of Korea (NRF); and Yonsei Signature Research Cluster Program of 2023-20-0010.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data can be directed to the corresponding author.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
References
- Codman, E.A. Rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. In The Shoulder; Thomas Todd Company: Boston, MA., USA, 1934; p. 514. [Google Scholar]
- Nakandala, P.; Nanayakkara, I.; Wadugodapitiya, S.; Gawarammana, I. The efficacy of physiotherapy interventions in the treatment of adhesive capsulitis: A systematic review. J. Back Musculoskelet. Rehabil. 2021, 34, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Hsu, J.E.; Anakwenze, O.A.; Warrender, W.J.; Abboud, J.A. Current review of adhesive capsulitis. J. Shoulder Elb. Surg. 2011, 20, 502–514. [Google Scholar] [CrossRef] [PubMed]
- Neviaser, R.J.; Neviaser, T.J. The frozen shoulder. Diagnosis and management. Clin. Orthop. Relat. Res. 1987, 223, 59–64. [Google Scholar] [CrossRef]
- Neviaser, A.S.; Neviaser, R.J. Adhesive capsulitis of the shoulder. J. Am. Acad. Orthop. Surg. 2011, 19, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Mao, C.Y.; Jaw, W.C.; Cheng, H.C. Frozen shoulder: Correlation between the response to physical therapy and follow-up shoulder arthrography. Arch. Phys. Med. Rehabil. 1997, 78, 857–859. [Google Scholar] [CrossRef]
- Ballantyne, B.T.; O’Hare, S.J.; Paschall, J.L.; Pavia-Smith, M.M.; Pitz, A.M.; Gillon, J.F.; Soderberg, G.L. Electromyographic activity of selected shoulder muscles in commonly used therapeutic exercises. Phys. Ther. 1993, 73, 668–677. [Google Scholar] [CrossRef]
- De la Serna, D.; Navarro-Ledesma, S.; Alayón, F.; López, E.; Pruimboom, L. A comprehensive view of frozen shoulder: A mystery syndrome. Front. Med. 2021, 8, 663703. [Google Scholar] [CrossRef]
- Hollmann, L.; Halaki, M.; Kamper, S.J.; Haber, M.; Ginn, K.A. Does muscle guarding play a role in range of motion loss in patients with frozen shoulder? Musculoskelet. Sci. Pract. 2018, 37, 64–68. [Google Scholar] [CrossRef]
- Hagiwara, Y.; Ando, A.; Kanazawa, K.; Koide, M.; Sekiguchi, T.; Hamada, J.; Itoi, E. Arthroscopic coracohumeral ligament release for patients with frozen shoulder. Arthrosc. Tech. 2017, 7, e1–e5. [Google Scholar] [CrossRef]
- Cho, C.H.; Song, K.S.; Kim, B.S.; Kim, D.H.; Lho, Y.M. Biological aspect of pathophysiology for frozen shoulder. Biomed. Res. Int. 2018, 2018, 7274517. [Google Scholar] [CrossRef]
- Harryman, D.T., 2nd; Sidles, J.A.; Clark, J.M.; McQuade, K.J.; Gibb, T.D.; Matsen, F.A., 3rd. Translation of the humeral head on the glenoid with passive glenohumeral motion. J. Bone Jt. Surg. Am. 1990, 72, 1334–1343. [Google Scholar] [CrossRef]
- Neviaser, J.S. Adhesive capsulitis of the shoulder: A study of the pathological findings in periarthritis of the shoulder. J. Bone Jt. Surg. 1945, 27, 211–222. [Google Scholar]
- Reeves, B. The natural history of the frozen shoulder syndrome. Scand. J. Rheumatol. 1975, 4, 193–196. [Google Scholar] [CrossRef] [PubMed]
- Vastamäki, H.; Kettunen, J.; Vastamäki, M. The natural history of idiopathic frozen shoulder: A 2- to 27-year followup study. Clin. Orthop. Relat. Res. 2012, 470, 1133–1143. [Google Scholar] [CrossRef]
- Kaltenborn, F.M. Specializad techniques: Tests and joint-mobilisation. In Manual Therapy for the Extremity Joints; Olaf Norlis Bokhandel: Oslo, Norway, 1976. [Google Scholar]
- Yaver, J. Maitland’s Peripheral Manipulation, ed 4. Phys. Ther. 2007, 87, 118–119. [Google Scholar] [CrossRef]
- Nicholson, G.G. The effects of passive joint mobilization on pain and hypomobility associated with adhesive capsulitis of the shoulder. J. Orthop. Sport. Phys. Ther. 1985, 6, 238–246. [Google Scholar] [CrossRef]
- Zavala-González, J.; Pavez-Baeza, F.; Gutiérrez-Espinoza, H.; Olguín-Huerta, C. The effectiveness of joint mobilization techniques for range of motion in adult patients with primary adhesive capsulitis of the shoulder: A systematic review and meta-analysis. Medwave 2018, 18, e7265. [Google Scholar] [CrossRef]
- Mangus, B.C.; Hoffman, L.A.; Hoffman., M.A.; Altenburger, P. Basic principles of extremity joint mobilization using a Kaltenborn approach. J. Sport Rehabil. 2002, 11, 235–250. [Google Scholar] [CrossRef]
- Vermeulen, H.M.; Rozing, P.M.; Obermann, W.R.; Le Cessie, S.; Vliet Vlieland, T.P. Comparison of high-grade and low-grade mobilization techniques in the management of adhesive capsulitis of the shoulder: Randomized controlled trial. Phys. Ther. 2006, 86, 355–368. [Google Scholar] [CrossRef]
- Çelik, D.; Kaya Mutlu, E.K. Does adding mobilization to stretching improve outcomes for people with frozen shoulder? A randomized controlled clinical trial. Clin. Rehabil. 2016, 30, 786–794. [Google Scholar] [CrossRef]
- Ali, S.A.; Khan, M. Comparison for efficacy of general exercises with and without mobilization therapy for the management of adhesive capsulitis of shoulder-An interventional study. Pak. J. Med. Sci. 2015, 31, 1372–1376. [Google Scholar] [CrossRef] [PubMed]
- Sirajuddin, M.; Quddus, N.; Grover, D. Comparison of anterior versus posterior glide mobilization techniques for improving internal rotation range of motion in shoulder adhesive capsulitis. Indian J. Physiother. Occup. 2010, 4, 152–157. [Google Scholar]
- Chan, S.; Hill, R.; Kerr, J. Passive joint mobilisation: Does it enhance outcome of adhesive capsulitis of the shoulder following corticosteroid injection? Int. Musculoskelet. Med. 2010, 32, 58–67. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and fill: A simple funnel-plot–based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Anjum, R.; Aggarwal, J.; Gautam, R.; Pathak, S.; Sharma, A. Evaluating the outcome of two different regimes in adhesive capsulitis: A prospective clinical study. Med. Princ. Pract. 2020, 29, 225–230. [Google Scholar] [CrossRef]
- Bhavana, D.R.; Soni, S. Immediate effects of positional stretching of coracohumeral ligament in individuals with adhesive capsulitis. Indian J. Physiother. Occup. Ther. 2017, 11, 107–111. [Google Scholar] [CrossRef]
- Gupta, D.; Desai, O.P.; Rastogi, S. To compare the effect of home based program and supervised occupational therapy program in adhesive capsulitis patients with diabetes mellitus. Indian J. Physiother. Occup. Ther. 2019, 13, 48–53. [Google Scholar] [CrossRef]
- Jellad, A.; May, W.; Zrig, A.; Kalai, A.; Jguirim, M.; Frih, Z.B.S.; Golli, M. Intra-articular distension preceded by physical therapy versus intra-articular distension followed by physical therapy for treating adhesive capsulitis of the shoulder. J. Back Musculoskelet. Rehabil. 2020, 33, 443–450. [Google Scholar] [CrossRef]
- Lee, S.H.; Yeh, S.C.; Chan, R.C.; Chen, S.; Yang, G.; Zheng, L.-R. Motor ingredients derived from a wearable sensor-based virtual reality system for frozen shoulder rehabilitation. BioMed Res. Int. 2016, 2016, 7075464. [Google Scholar] [CrossRef]
- Shishir, M.S.; Abraham, M.M.; Kanagasabai, R.; Najimudeen, S.; Gnanadoss, J.J. Home based exercise program for frozen shoulder-follow-up of 36 idiopathic frozen shoulder patients. Indian J. Physiother. Occup. Ther. 2013, 7, 221–226. [Google Scholar] [CrossRef]
- Chidambaram, R.; Muruganandam, P.; Bhandure, K.S. The efficacy of sleeper’s stretch and movement with mobilization on pain, range of motion & functional capacity in patients with adhesive capsulitis. Indian J. Physiother. Occup. Ther. 2020, 14, 149–155. [Google Scholar] [CrossRef]
- Kushwah, S.S.; Srivastava, N. Comparison between effectiveness of active release technique and capsular stretch along with conventional therapy in the management of frozen shoulder. Indian J. Physiother. Occup. Ther. 2018, 12, 85–90. [Google Scholar] [CrossRef]
- Hand, C.; Clipsham, K.; Rees, J.L.; Carr, A.J. Long-term outcome of frozen shoulder. J. Shoulder Elb. Surg. 2008, 17, 231–236. [Google Scholar] [CrossRef]
- van den Hout, W.B.; Vermeulen, H.M.; Rozing, P.M.; Vlieland, T.P.V. Impact of adhesive capsulitis and economic evaluation of high-grade and low-grade mobilisation techniques. Aust. J. Physiother. 2005, 51, 141–149. [Google Scholar] [CrossRef]
- Brotzman, S.D.; Manske, R.D. Clinical Orthopaedic Rehabilitation: An Evidence-Based Approach, 3rd ed.; Mosby: Maryland, MO, USA, 2011. [Google Scholar]
- Griggs, S.M.; Ahn, A.; Green, A. Idiopathic adhesive capsulitis: A prospective functional outcome study of nonoperative treatment. JBJS 2000, 82, 1398. [Google Scholar] [CrossRef]
- Dogru, H.; Basaran, S.; Sarpel, T. Effectiveness of therapeutic ultrasound in adhesive capsulitis. Jt. Bone Spine 2008, 75, 445–450. [Google Scholar] [CrossRef]
- Jewell, D.V.; Riddle, D.L.; Thacker, L.R. Interventions associated with an increased or decreased likelihood of pain reduction and improved function in patients with adhesive capsulitis: A retrospective cohort study. Phys. Ther. 2009, 89, 419–429. [Google Scholar] [CrossRef]
- Ruiz, J.O. Positional stretching of the coracohumeral ligament on a patient with adhesive capsulitis: A case report. J. Man Manip. Ther. 2009, 17, 58–63. [Google Scholar] [CrossRef]
- Wattanaprakornkul, D.; Halaki, M.; Boettcher, C.; Cathers, I.; Ginn, K.A.A. Comprehensive analysis of muscle recruitment patterns during shoulder flexion: An electromyographic study. Clin. Anat. 2011, 24, 619–626. [Google Scholar] [CrossRef]
- Kingston, K.; Curry, E.J.; Galvin, J.W.; Li, X. Shoulder adhesive capsulitis: Epidemiology and predictors of surgery. J. Shoulder Elb. Surg. 2018, 27, 1437–1443. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.D.; Wirth, M.A.; Rockwood, C.A. Thawing the frozen shoulder: The “patient” patient. Orthopedics 1996, 19, 849–853. [Google Scholar] [CrossRef] [PubMed]
- Minter, W.T., 3rd. The shoulder-hand syndrome in coronary disease. J. Med. Assoc. GA 1967, 56, 45–49. [Google Scholar] [PubMed]
- Ogilvie-Harris, D.J.; Myerthall, S. The diabetic frozen shoulder: Arthroscopic release. Arthroscopy 1997, 13, 1–8. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).