Abstract
Endometriosis is a disease that is often diagnosed late and that may lead to significant reduction in quality of life and serious complications (e.g., infertility). We aimed to assess the prevalence and the annual, nationwide health insurance treatment cost of endometriosis in Hungary using a quantitative, descriptive, cross-sectional method, focusing on the year 2019. We used claims data obtained from the Hungarian National Health Insurance Fund Administration (NHIFA). Patient numbers, total and age-specific prevalence, annual health insurance expenditure, and the distribution of costs across age groups were determined. The NHIFA spent a total of HUF 619.95 million (EUR 1.91 million) on endometriosis treatment. The highest number of patients and prevalence (10,058 women, 197.3 per 100,000) were found in outpatient care. In acute inpatient care, prevalence was substantially lower (23.5 per 100,000). Endometriosis, regardless of its type, affects 30–39-year-olds in the highest number: 4397 women (694.96 per 100,000) in this age group were affected in 2019. The average annual health insurance expenditure per capita was EUR 189.45. In addition to early detection and diagnosis of endometriosis, it is of pivotal importance to provide adequate therapy to reduce costs and reduce the burden on the care system.
1. Introduction
Endometriosis is a chronic, estrogen-dependent gynecological disease that is associated with severe pelvic pain and infertility and increases the risk of developing other malignant lesions, as well as immunological and atopic diseases [1,2,3,4]. In addition to the causes of the development and spread of this disease, with its varied clinical presentation, its full impact on the body and its possible manifestations outside the reproductive tract are still not fully understood. Diagnosing and treating this possibly systemic and multidisciplinary disease can therefore be challenging [5] and can take years [6]. The average time from first symptoms to diagnosis among Canadian women was estimated to be approximately 5.4 years [7]. According to another study, more than 50% of US patients waited longer than 6 years for a diagnosis [8]. In Europe, an average wait of 10.4 years was reported among women in Austria and Germany, where 74% of women were misdiagnosed at least once [9]. In Hungary, the average diagnostic delay was 2.01–3.9 years [10,11].
Many factors can contribute to diagnostic delays [12], such as the lack of reliable non-invasive tests, misleading symptoms, and late arrival to care centers with the appropriate diagnostical tools—of which laparoscopic surgery is considered to be the most correct form [5,13]. The stage of the disease must also be taken into consideration when choosing the best treatment method. The classification system of the American Society of Reproductive Medicine (ASRM) distinguishes four stages of endometriosis. In Stage I (minimal) and Stage II (mild), deep lesions and thin adhesions are absent or rare, while in Stage III (moderate) and Stage IV (severe), larger adhesions and endometrioma can occur and possibly spread to other organs, further decreasing the patient’s quality of life [14].
Considering the above facts, the prevalence of endometriosis in women of reproductive age ranges widely and is difficult to determine. A recent study estimates the prevalence of the disease at 18% globally, 17% in Europe, 19% in the Americas, 26% in Africa, and 36% in Asia [15]. Regarding its incidence, most new cases are found among 25–45-year-olds [16,17,18,19].
Diagnostic delay can have a negative impact not only on quality of life and thus productivity [20,21,22,23,24], but can also increase the cost of treatment. A US study with 11,793 participants set the average diagnostic delay to 763.9 days and the total cost per capita related to endometriosis to USD 3553. Among women who took the longest to be diagnosed (1505.9 days), this was USD 4794, while among those who took the shortest time (90.2 days), it was less than half (USD 2082). The greatest cost drivers were ambulatory care (59.1%) and pharmaceutical reimbursement (17.7%) [25].
Studies measuring the burden of the disease and quality of life associated with endometriosis among Hungarian women are scarce, and their results vary [10,11,26,27].
The Hungarian Health Care and Health Insurance System
The Hungarian compulsory health insurance system is based on a single payer (National Health Insurance Fund Administration, NHIFA) which covers 98–99% of the population. Any healthcare provider, regardless of ownership (public, non-profit, church, private, etc.), can initiate a financing contract with the NHIFA. These providers send monthly data on the volume of care and services covered by the contract and the patient population served, which forms the basis for reimbursement.
It is mandatory to be a member of the health insurance risk pool in Hungary. The insured will be entitled to health insurance benefits by right if they pay contributions (a percentage of their monthly income) to the NHIFA, while those without income (pensioners, schoolchildren, etc.) are insured by contributions from the central budget. The role of private health insurance companies is supplementary and covers mainly amenities (single room, LCD television, etc.). Only a small proportion of the Hungarian population has private health insurance.
The regulation and functioning of the Hungarian health care system and its structural characteristics have been described in detail elsewhere [28,29].
We aimed to assess the prevalence and the annual health insurance treatment cost of endometriosis in Hungary.
2. Materials and Methods
The epidemiological and health insurance disease burden of different types of endometrioses were analyzed using a quantitative, descriptive, cross-sectional method in Hungary, focusing on the year 2019.
The research used a nationwide database of real-world data from the sole publicly funded health insurance organization of Hungary, the National Health Insurance Fund Administration (NHIFA) [30], as it contains claims data for all Hungarian, publicly funded healthcare providers. We identified endometriosis according to the following ICD codes (10th Revision): endometriosis of the uterus (N80.0), ovary (N80.1), fallopian tube (N80.2), pelvic peritoneum (N80.3), rectovaginal septum, and vagina (N80.4), as well as other (N80.8) and unspecified endometriosis (N80.9).
The utilization and reimbursement of 14 treatment types were assessed: general practitioner care; home (nursing) care; care in care centers; outpatient care; acute and chronic inpatient care; medical imaging (CT, MRI); laboratory diagnostics; pharmaceuticals; medical aids; disposable instruments, implantations and medicaments falling under itemized accounts; ambulance service; patient transportation. (For ambulance service, data on patient numbers were available and thus analyzed only.) Regarding acute and chronic inpatient care, cases reported with a primary diagnosis of endometriosis were evaluated only.
To determine the health insurance burden—from the health insurer’s viewpoint—of the diseases included in the study, annual health insurance expenditure and the distribution of costs by age group were determined. Expenditures are given in EUR (at the average EUR to HUF exchange rate from 2019).
For epidemiological analysis, we also examined the annual patient and case numbers, as well as the total and age-specific prevalence per 100,000 female population. To calculate the prevalence, we obtained age-specific data from the Hungarian Central Statistical Office for the female population in 2019.
We also estimated the average length of stay as the ratio of the number of patients to the number of days of care provided in acute inpatient care. To avoid duplication between different treatment types and to ensure comparability between different ICD codes, the number of patients receiving outpatient care was selected to calculate the prevalence for all disease subgroups. The annual case numbers per patient were also determined to further analyze the utilization of each care type. For that, we divided the case numbers of all 14 care types assessed with the corresponding patient numbers for all ICD codes.
3. Results
3.1. Epidemiology
In Hungary, the highest number of patients (10,058 women) was found in outpatient care in 2019. A total of 8174 women consulted their general practitioner about some form of endometriosis, and 4372 women used reimbursed pharmaceuticals (Table 1).

Table 1.
Annual patient numbers according to different types of endometriosis (capita).
Out of the different disease types assessed, the largest ratio belonged to unspecified endometriosis (N80.9) in outpatient care (67.88%). Ovarian endometriosis also occurred in a significant proportion (15.99%), while all the other types accounted for 16.14%. In addition, almost half (39.12%) of the acute inpatient population was found to have ovarian endometriosis.
The mean age across the three types of care with the highest patient numbers was roughly the same: outpatients average 37.5 years, those receiving reimbursed medication 38.8 years, and women in general practice 38.4 years. Patients attending laboratory diagnostics and acute inpatient care tended to be younger (36.6 and 35.8 years, respectively).
The prevalence defined for the different types of care varied considerably. The highest prevalence was observed in outpatient care (197.3 per 100,000 women), followed by the prevalence based on general practice (160.4 per 100,000 women), while in acute inpatient care it was substantially lower (23.5 per 100,000 women), and the prevalence based on the number of patients using prescribed medicaments was about half that calculated based on general practitioner care (85.8 per 100,000 women) (Figure 1).
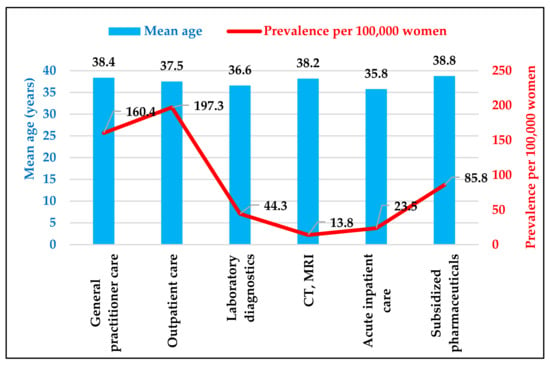
Figure 1.
Average age and prevalence of women with endometriosis by different types of care. Source: NHIFA, 2019.
Figure 2 shows the annual outpatient numbers and the prevalence per 100,000 women of each age group. Endometriosis, regardless of its type, affected 30–39-year-olds in the highest number: 4397 women (694.96 per 100,000) in 2019. This was followed by the 40–49 age group (3422 patients, 438.94 per 100,000), and then the 20–29 age group (1586 patients, 275.27 per 100,000). For two disease types, we observed a higher proportion of women aged 40–49 years: endometriosis of the uterus (40.71%) and endometriosis of the fallopian tube (44.26%). The rates for women aged 20–29 years were highest for ovarian (17.04%) and peritoneal endometriosis (16.28%).
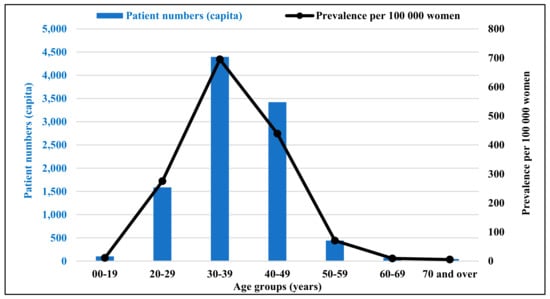
Figure 2.
The number of patients in outpatient care and prevalence per 100,000 women of each age group. Source: NHIFA, 2019.
3.2. Health Insurance Costs
The National Health Insurance Fund Administration of Hungary spent a total of HUF 619.95 million (EUR 1.91 million) on the treatment of endometriosis in 2019. The exact health insurance expenditure for each type of care is shown in Table 2. The largest share of expenditure was for the reimbursement of pharmaceuticals (48.20%), acute inpatient care (31.63%), and outpatient care (6.25%).

Table 2.
Annual health insurance treatment cost of endometriosis according to the type of care (EUR).
Out of the different subgroups analyzed, the largest expenditure share and patient numbers belonged to unspecified cases (67.07%; EUR 1.28 million), followed by ovarian endometriosis (21.47%; EUR 409,160). Every other form added up to 11.46% of total expenditure in 2019 (Table 2).
For the relevant cost drivers, we examined the differences in the distribution of expenditure between the different anatomical locations. The share of pharmaceutical reimbursement for each form of endometriosis ranged from 8.58% (fallopian tube) to 62.28% (unspecified), whereas the treatment of the ovary (70.70%) and fallopian tube (63.32%) was associated more with acute inpatient care. The lowest proportion of inpatient care costs was observed for the rectovaginal septum and vagina (11.69%) and the unspecified cases (17.07%). Apart from the latter, the costs associated with general practitioner care ranked third for each of these conditions (fallopian tubes: 5.08%; uterus: 13.53%). It is also worth highlighting the distribution of costs for rectovaginal septum and vaginal endometriosis, where the proportion of chronic inpatient care (10.78%) was much higher than for the other ICD codes (elsewhere, this type of care accounted for an average of only 1.38%).
The total and per capita expenditures of different age groups are shown in Figure 3. The highest expenditure belongs to those aged 30–39 years (45.44%; EUR 865,780). For the treatment of 40–49-year-olds, EUR 639,110 (33.54%) was reimbursed, while for the 20–29 age group, EUR 328,500 (7.24%) was reimbursed by the NHIFA. In contrast to the total expenditure, the 40–49-year-olds demonstrated the highest expenditure for endometriosis of the uterus (47.40%) and fallopian tubes (42.91%).
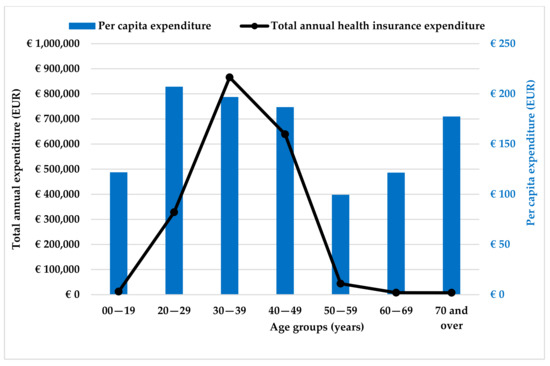
Figure 3.
Total annual health insurance expenditure and average annual expenditure per patient by age group (in EUR). Source: NHIFA, 2019.
Based on the data for outpatient care, we also calculated the average annual health insurance expenditure per capita, which averaged EUR 189.45 in 2019. The lowest per capita health insurance expenditure was for treating endometriosis of the rectovaginal septum and vagina (EUR 114.58), while the highest was for treating ovarian endometriosis (EUR 254.45), but the expenditure for treatment of the pelvic peritoneum (EUR 192.25) was also significant compared to the other types of diseases studied. This indicator was much higher, however, for hospitalized patients, where the annual cost per patient was EUR 502.74 in 2019.
The average length of stay when endometriosis was the main diagnosis in acute inpatient care was 2.8 days. The lowest length of stay recorded was for patients with endometriosis of the rectovaginal septum and vagina (1.6 days), while the longest was for endometriosis of the uterus (5.33 days).
Correlation analysis was used to examine the relationship between per capita expenditure (expenditure for a given type of care divided by the number of patients recorded for each ICD code) and average age (also for a given type for each ICD code). The detailed results can be seen in Table 3.

Table 3.
Results of correlation analyses.
We found a negative relationship between laboratory diagnostics (r = −0.503; p = 0.020) and subsidized medicaments (r = −0.356; p = 0.097), although the latter was not statistically significant. These results mean that with younger age comes a higher per capita cost among endometriosis patients.
However, we found a moderate, positive, although not significant, relationship between the per capita cost of acute inpatient specialist care (r = 0.405; p = 0.060) and average age. In conclusion, acute inpatient care, including treatments requiring higher expenditure, tends to affect older patients in NHIFA-funded hospitals.
We also examined the existence of relationships between age and the annual number of cases per patient. For patient transportation (r = 0.649; p = 0.002), ambulatory service care (r = 0.879; p < 0.001), home care (r = 0.981; p < 0.001), and chronic inpatient specialty care (r = 0.995; p < 0.001), older women typically present more than once a year. In contrast, an inverse relationship was found for outpatient care (r = −0.453; p = 0.036), where women of younger ages return more than once a year more so than older patients.
Additionally, we also detected a statistically significant, strong, and positive association between mean age and mean length of stay in acute inpatient care, suggesting that older patients typically require longer hospital stays (r = 0.877; p < 0.001).
4. Discussion
Our analysis aimed to determine the epidemiological and annual health insurance cost of endometriosis in Hungary; therefore, we performed our analysis on a nationwide dataset covering the whole Hungarian population covered by the only health care financing agency in a single-payer system. We found that the prevalence of endometriosis is 275.27 per 100,000 among 20–29-year-olds, 694.96 per 100,000 in 30–39-year-olds, and 438.94 per 100,000 in 40–49-year-olds, based on outpatient data. Our results are in line with those based on real-life data from France (0.90% for 15–49-year-olds) [31].
Epidemiologic studies assessing endometriosis show different levels of prevalence, with a large variance influenced by the number of patients and their methodological specificities. In a literature review and meta-analysis of 69 studies, the prevalence of endometriosis was estimated to be between 0.2% and 71.4%, with prevalence typically lower in population-based analyses with the largest number of items (2.4%), and 4.3% in national/regional questionnaire surveys (10,000 population: 2.4%, over 10,000 population: 4.4%), while the highest prevalence (and variance) was found in studies that took place in a hospital/clinical setting (15.9%) [32].
In addition to outpatient specialist care, a significant proportion of Hungarian women also visited their general practitioners about their illnesses, and a large proportion of them also received subsidized medications—the latter being the area with the highest health insurance expenditure. Although general practitioners have a gatekeeping role in Hungary, specialized gynecological services available at the outpatient level can be used without a GP referral. Our results show that more women go straight to specialist care with their symptoms. The use of specialist care as the first place where a patient presents with a problem may also be explained by the fact that women tend to seek help only for more serious complaints and pain. The direct and indirect costs associated with the care of endometriosis can be a significant burden for individuals and society [33]. In our analysis, we found the cost per patient of treating endometriosis to have been EUR 189.45 in 2019, based on the outpatient specialty care element number. In contrast, the cost per capita of hospital care is already higher, at EUR 502.74. This is still well below the average per capita expenditure found in the literature. For instance, a study on 10 countries found the per capita expenditure to be EUR 9579 in 2008, of which indirect costs linked to productivity loss produced the largest proportion (66%, EUR 6298), whereas direct costs amounted to EUR 3281 per capita [34]. Annual per capita expenditure was EUR 8768 in Sweden in 2010 (based on 2019 prices), of which direct costs amounted to EUR 4282 and indirect expenditure was EUR 4486 [35]. In Austria, the average annual cost per person was EUR 7712 in 2011, with 73% of this being direct cost [36]. In Germany, for example, the direct cost of treatment is USD 4846.99, in Canada it is USD 1109.45, and in the US it is up to ten to fifteen times higher (up to USD 16,574, according to Gao et al.). There are several possible reasons for this phenomenon. For example, there were significant differences between the income levels of doctors in Hungary and in other countries (in 2019), which were then reduced by a reform of the Hungarian health care and human resources system [37]. Due to the different natures of the health insurance systems, administrative costs can also be significantly higher in countries such as the US, where private insurers dominate. Differences in the pharmaceutical market (e.g., price regulation) can also lead to significant differences in health expenditure on endometriosis between countries.
According to the available studies on expenditure, the direct public expenditure per capita for endometriosis—as we have also assessed—can be significant, with differences of up to ten times between countries. However, the methodologies used to determine the costs show at least as much variation, meaning that the data reported must be treated with caution. One should keep in mind that the health systems of the countries also differ (e.g., the USA, where the annual per capita cost in the year following diagnosis is USD 13,199, which is equivalent to EUR 9046.8 at the exchange rate in the year of the study) [38]. In addition, the indirect costs often tend to be even higher. Although we have not been able to measure them, we can assume that there may be significant indirect costs associated with endometriosis in Hungary [33].
In general, we have also observed that in most publications, acute inpatient care accounts for the largest share of direct costs [38,39], whereas we have identified pharmaceutical reimbursement as the primary cost driver. The discrepancy may be due to methodological differences in international studies (no drug costs were examined), but it may also be due to differences in care protocols.
In the US, the average length of acute inpatient stay in the year following diagnosis was found to be 1.6 days [39], while another study found that it was 2.6 days in 2014–2015 [40]. In the national context, similar values were obtained (2.8 days (1.6–5.33)).
Despite the relatively low number of patients, acute inpatient care still involved a significant amount of health insurance expenditure in our study. To reduce costs, it may be important to support innovative, more cost-effective therapies, or those that can be delivered at lower levels of care, for those conditions for which higher than average inpatient admission rates have been found. For example, there have been significant technological advances in medical imaging technologies such as transvaginal ultrasound or MRI in recent years, which is why Chapron et al. suggest that exploratory laparoscopy is no longer always justified for the diagnosis of endometriotic lesions. The authors base the diagnosis on a structured process combining patient interviews, clinical examination, and imaging [41].
We found a negative relationship between laboratory care (r = −0.503; p = 0.020) and pharmaceutical reimbursement (r = −0.356; p = 0.097). This means that the younger age group incur a higher per capita cost. In conclusion, efforts should be made on the part of both the patient and the care provider to diagnose the disease as early as possible in life. In addition to early detection and diagnosis of endometriosis, it is of pivotal importance to provide therapy at the lowest possible level of care to reduce costs and reduce the burden on the care system, in terms of allocative effectiveness. One study showed that 76.8% of general practitioners were visited by women with typical symptoms of endometriosis, but only 36% of them diagnosed them with endometriosis when confronted with these symptoms. Thus, in addition to patient education, the early recognition of symptoms should also be emphasized in the training of health professionals. Our analysis shows that Hungarian women visit their general practitioners in high numbers, with the second highest prevalence in Hungary being found in this type of care [42].
We also found that older endometriosis patients typically use patient transportation, ambulatory care, home care, and chronic inpatient care more often. In contrast, an inverse relationship was found in outpatient care (r = −0.453; p = 0.036), where younger women return more than once a year more so than older patients. A similar result was found by Grundström et al. in a study of Swedish women, where they found that those under 30 years of age also had a higher rate of use of general practitioner’s care and gynecological specialist services [35]. The likely reason behind this result is the higher level of health literacy, health awareness, and perception of the importance of fertility among younger women. In addition, we also found a significant, strong, positive association between mean age and mean length of stay in active inpatient care. This finding suggests that older female patients typically need to be treated for a longer period (r = 0.877; p < 0.001), suggesting that older age is associated with a higher risk of surgery and longer recovery times. Therefore, it is also more beneficial for the patient and the health insurer to have these procedures performed at a younger age.
In our research, some levels of care had very low or no utilization at all regarding endometriosis. For example, the use of medical aids, home (nursing) care, and patient transport is not common in the treatment of endometriosis. Among the ICD codes, the high use of the code without a specific name (N80.9) compared to the other codes shows that the coding does not specify the location of endometriosis (uterus, ovary, etc.), especially in cases where it is not essential to record the exact diagnosis for a given treatment (e.g., prescription of painkillers)—which may lead to data bias. The use of an ICD code independent of the localization may also be explained by the need to classify the disease in the appropriate homogeneous disease groups (HDGs) (e.g., ovarian endometriosis, coded N80.1), or even for people with certain diseases to claim the personal income tax benefit, which has been available in Hungary since 2019 [43].
Knowing the severity of endometriosis is also of key importance, as each stage differs and causes various symptoms and clinical manifestations, requiring different treatment plans. The 11th Revision of the ICD already contains much more detailed codes for identifying location and severity than the 10th, and the “Endometriosis Severity Scale Value” has been developed, which allows the disease to be coded separately according to its severity (three categories) [44]. An appropriate coding system that makes it possible to locate and describe severity accurately will greatly facilitate research into the disease and help to identify any unknown influences and risk factors and the likely outcome of treatment [45]. The success of surgical interventions is also greatly enhanced when patients (in the more severe stages) are treated in endometriosis centers or assisted reproduction centers, where the most effective treatment of this disease can be guaranteed.
At the time of this study, there is no valid clinical guideline for the treatment of endometriosis in Hungary. The European Society of Human Reproduction and Embryology (ESHRE) renewed its guidelines in 2022, and it is necessary that their application and incorporation into the Hungarian health care system be promoted [46].
5. Conclusions
The strength of our analysis is that we present national endometriosis-related utilization and expenditure data through real-world, routinely collected claims data. Understanding these indicators is key for health policymakers, as we can better understand the burden of each type of care and identify where allocative and technical efficiency needs to be increased. A suitable patient population can be managed at a lower level of care through the introduction and promotion of innovative diagnostic and therapeutic procedures. Modern endometriosis management should be personalized through a patient-centered, multimodal, and interdisciplinary approach.
However, our research also has some limitations. We have not been able to investigate indirect costs, which can impose significant costs on patients and their families (e.g., cost of care, travel, absence from work, etc.). We also did not have data on other socio-demographic characteristics of the patient population that are likely to cause significant differences in individual cost, quality of life, and prevalence between subgroups (such as marital status, number of children, urban-rural location, and education). We do not have data on private health care utilization, neither regarding expenditure nor the indirect costs patients have to pay regarding their illness.
We also could not determine the exact length of diagnostic delay among Hungarian women with endometriosis. However, it was important to describe the problem of delay, even though no such data were available for our research. Delay negatively affects the quality of life of the individual, as it puts a burden on the health care system, especially on the more costly specialist care. For an efficient healthcare system, it is of pivotal importance to diagnose diseases promptly and to treat them at the lowest possible level, if possible. This can be achieved, among other things, through appropriate patient education and access to services and modern, effective/efficient diagnostic tools. The main aim of our analysis was (also) to draw attention to the significant burden of endometriosis, which provides the basis for ensuring the above-mentioned solutions and health policy decisions.
Based on our results, our main conclusion is to call for the adequate diagnosis of endometriosis patients at an earlier stage of life, as timely treatment can improve the quality of life of the individual and reduce the burden on health insurance as well.
Author Contributions
Conceptualization–study design: T.C., J.B. and I.B.; methodology: T.C., L.F.K., Á.V., K.K., J.B. and I.B.; literature search: T.C., D.P.-K., L.F.K., D.E., R.P., B.K., Á.V., K.K., J.B. and I.B.; data curation, validation, and analysis: T.C., L.F.K., D.E. and I.B.; data interpretation: T.C., D.P.-K., L.F.K., D.E., R.P., B.K., Á.V., K.K., J.B. and I.B.; statistical analysis: T.C., L.F.K., D.E., J.B. and I.B.; writing the manuscript–drafting: T.C., D.P.-K., L.F.K., D.E., R.P., B.K. and I.B.; writing–review and editing: Á.V., K.K., J.B. and I.B.; visualization: T.C., D.P.-K., L.F.K., D.E., R.P. and B.K.; supervision: J.B. and I.B.; funding acquisition: J.B. All authors have read and agreed to the published version of the manuscript.
Funding
This study was financed by the project RRF-2.3.1-21-2022-00012 “National Laboratory on Human Reproduction”.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Restrictions apply to the availability of these data. Data were obtained from the National Health Insurance Fund Administration (NHIFA) of Hungary and are available from the authors with the permission of the NHIFA.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Giudice, L.C.; Kao, L.C. Endometriosis. Lancet 2004, 364, 1789–1799. [Google Scholar] [CrossRef] [PubMed]
- Kvaskoff, M.; Mahamat-Saleh, Y.; Farland, L.V.; Shigesi, N.; Terry, K.L.; Harris, H.R.; Roman, H.; Becker, C.M.; As-Sanie, S.; Zondervan, K.T.; et al. Endometriosis and cancer: A systematic review and meta-analysis. Hum. Reprod. Updat. 2021, 27, 393–420. [Google Scholar] [CrossRef]
- Szegedi, S.; Koppan, M.; Varga, T.; Kovacs, K.; Tinneberg, H.R.; Bodis, J. Endometrioid adenocarcinoma arising from adenomyosis: A case report. Eur. J. Gynaecol. Oncol. 2016, 37, 858–860. [Google Scholar] [PubMed]
- Vigh, É.; Molnár, V.; Garai, J.; Varga, T.; Koppán, M.; Bódis, J. Endometriosis: Damage to ectopically surviving tissue. Part 1: Pathomechanism of endometriosis. (Endometriózis: Az ektópiásan túlélő szövet ártalma I.: Az endometriózis patomechanizmusa.). Magy Nőorv L 2009, 72, 79–97. (In Hungarian) [Google Scholar]
- Taylor, H.S.; Kotlyar, A.M.; Flores, V.A. Endometriosis is a chronic systemic disease: Clinical challenges and novel innovations. Lancet 2021, 397, 839–852. [Google Scholar] [CrossRef] [PubMed]
- Hadfield, R.; Mardon, H.; Barlow, D.; Kennedy, S. Delay in the diagnosis of endometriosis: A survey of women from the USA and the UK. Hum. Reprod. 1996, 11, 878–880. [Google Scholar] [CrossRef]
- Singh, S.; Soliman, A.M.; Rahal, Y.; Robert, C.; Defoy, I.; Nisbet, P.; Leyland, N. Prevalence, Symptomatic Burden, and Diagnosis of Endometriosis in Canada: Cross-Sectional Survey of 30000 Women. J. Obstet. Gynaecol. Can. 2020, 42, 829–838. [Google Scholar] [CrossRef]
- Lamvu, G.; Antunez-Flores, O.; Orady, M.; Schneider, B. Path to diagnosis and women’s perspectives on the impact of endometriosis pain. J. Endometr. Pelvic Pain Disord. 2020, 12, 16–25. [Google Scholar] [CrossRef]
- Hudelist, G.; Fritzer, N.; Thomas, A.; Niehues, C.; Oppelt, P.; Haas, D.; Tammaa, A.; Salzer, H. Diagnostic delay for endometriosis in Austria and Germany: Causes and possible consequences. Hum. Reprod. 2012, 27, 3412–3416. [Google Scholar] [CrossRef]
- Bokor, A.; Koszorús, E.; Brodszky, V.; D’hooghe, T.; WERF EndoCost Consortium; Rigó, J. The impact of endometriosis on the quality of life in Hungary. (Az endometriosis hatása az életminőségre Magyarországon). Orvosi Hetil. 2013, 154, 1426–1434. (In Hungarian) [Google Scholar] [CrossRef]
- Márki, G.; Vásárhelyi, D.; Rigó, A.; Kaló, Z.; Ács, N.; Bokor, A. Challenges of and possible solutions for living with endometriosis: A qualitative study. BMC Women’s Health 2022, 22, 20. [Google Scholar] [CrossRef] [PubMed]
- Van Der Zanden, M.; Teunissen, D.A.M.; Van Der Woord, I.W.; Braat, D.D.M.; Nelen, W.L.D.M.; Nap, A.W. Barriers and facilitators to the timely diagnosis of endometriosis in primary care in the Netherlands. Fam. Pract. 2020, 37, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Hsu, A.L.; Khachikyan, I.; Stratton, P. Invasive and Noninvasive Methods for the Diagnosis of Endometriosis. Clin. Obstet. Gynecol. 2010, 53, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Canis, M.; Donnez, J.G.; Guzick, D.S.; Halme, J.K.; Rock, J.A.; Schenken, R.S.; Vernon, M.W. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil. Steril. 1997, 67, 817–821. [Google Scholar]
- Moradi, Y.; Shams-Beyranvand, M.; Khateri, S.; Gharahjeh, S.; Tehrani, S.; Varse, F.; Tiyuri, A.; Najmi, Z. A systematic review on the prevalence of endometriosis in women. Indian J. Med. Res. 2021, 154, 446–454. [Google Scholar] [CrossRef]
- Houston, D.E.; Noller, K.L.; Melton, I.L.J.; Selwyn, B.J.; Hardy, R.J. Incidence of pelvic endometriosis in rochester, minnesota, 1970–1979. Am. J. Epidemiol. 1987, 125, 959–969. [Google Scholar] [CrossRef]
- Eisenberg, V.H.; Weil, C.; Chodick, G.; Shalev, V. Epidemiology of endometriosis: A large population-based database study from a healthcare provider with 2 million members. BJOG 2018, 125, 55–62. [Google Scholar] [CrossRef]
- Missmer, S.A.; Hankinson, S.E.; Spiegelman, D.; Barbieri, R.L.; Marshall, L.M.; Hunter, D.J. Incidence of Laparoscopically Confirmed Endometriosis by Demographic, Anthropometric, and Lifestyle Factors. Am. J. Epidemiol. 2004, 160, 784–796. [Google Scholar] [CrossRef]
- Muhaidat, N.; Saleh, S.; Fram, K.; Nabhan, M.; Almahallawi, N.; Alryalat, S.A.; Elfalah, M.; Elfalah, M. Prevalence of endometriosis in women undergoing laparoscopic surgery for various gynaecological indications at a Jordanian referral centre: Gaining insight into the epidemiology of an important women’s health problem. BMC Women’s Health 2021, 21, 381. [Google Scholar] [CrossRef]
- Ruszała, M.; Dłuski, D.F.; Winkler, I.; Kotarski, J.; Rechberger, T.; Gogacz, M. The State of Health and the Quality of Life in Women Suffering from Endometriosis. J. Clin. Med. 2022, 11, 2059. [Google Scholar] [CrossRef]
- Kalfas, M.; Chisari, C.; Windgassen, S. Psychosocial factors associated with pain and health-related quality of life in Endometriosis: A systematic review. Eur. J. Pain 2022, 26, 1827–1848. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, B.; Zhou, Y.; Wang, Y.; Han, X.; Zhang, S.; He, Z.; Ouyang, L. Does Endometriosis Disturb Mental Health and Quality of Life? A Systematic Review and Meta-Analysis. Gynecol. Obstet. Investig. 2021, 86, 315–335. [Google Scholar] [CrossRef] [PubMed]
- Becker, K.; Heinemann, K.; Imthurn, B.; Marions, L.; Moehner, S.; Gerlinger, C.; Serrani, M.; Faustmann, T. Real world data on symptomology and diagnostic approaches of 27,840 women living with endometriosis. Sci. Rep. 2021, 11, 20404. [Google Scholar] [CrossRef] [PubMed]
- Koppan, Á.; Frank, O.; Hámori, J.; Krisbacher, I.; Vranics, I.; Garai, J.; Bódis, J.; Tinneberg, H.R.; Koppán, M. The effect of lifestyle factors on pelvic pain and quality of life in endometriosis. (Életmódbeli faktorok hatása a kismedencei fájdalomra és életminőségre endometriózisban.). Magy. Epidemiol. 2010, 7, 17–26. (In Hungarian) [Google Scholar]
- Surrey, E.; Soliman, A.M.; Trenz, H.; Blauer-Peterson, C.; Sluis, A. Impact of Endometriosis Diagnostic Delays on Healthcare Resource Utilization and Costs. Adv. Ther. 2020, 37, 1087–1099. [Google Scholar] [CrossRef]
- Szendei, G.A. Endometriosis in Hungary. Gynecol. Endocrinol. 2009, 25, 694–700. [Google Scholar] [CrossRef]
- Csákvári, T.; Elmer, D.; Kajos, L.; Pónusz, R.; Pónusz-Kovács, D.; Kovács, B.; Endrei, D.; Boncz, I.; Bódis, J. Epidemiological Disease Burden of Ovarian Endometriosis Based on Real-World Health Insurance Claims Data. Value Health 2022, 25, S451. [Google Scholar] [CrossRef]
- Boncz, I.; Evetovits, T.; Dózsa, C.; Sebestyén, A.; Gulácsi, L.; Ágoston, I.; Endrei, D.; Csákvári, T.; Getzen, T.E. The Hungarian Care Managing Organization Pilot Program. Value Health Reg Issues 2015, 7, 27–33. [Google Scholar] [CrossRef]
- National Health Insurance Fund Administration (NEAK). Data Request nr. I043/24-2/2021; National Health Insurance Fund Administration (NEAK): Budapest, Hungary, 29 September 2021. [Google Scholar]
- Boncz, I.; Nagy, J.; Sebestyén, A.; Kőrösi, L. Financing of health care services in Hungary. Eur. J. Health Econ. 2004, 5, 252–258. [Google Scholar] [CrossRef]
- Von Theobald, P.; Cottenet, J.; Iacobelli, S.; Quantin, C. Epidemiology of Endometriosis in France: A Large, Nation-Wide Study Based on Hospital Discharge Data. BioMed Res. Int. 2016, 2016, 3260952. [Google Scholar] [CrossRef]
- Ghiasi, M.; Kulkarni, M.T.; Missmer, S.A. Is Endometriosis More Common and More Severe Than It Was 30 Years Ago? J. Minim. Invasive Gynecol. 2020, 27, 452–461. [Google Scholar] [CrossRef] [PubMed]
- Soliman, A.M.; Yang, H.; Du, E.X.; Kelley, C.; Winkel, C. The direct and indirect costs associated with endometriosis: A systematic literature review. Hum. Reprod. 2016, 31, 712–722. [Google Scholar] [CrossRef] [PubMed]
- Simoens, S.; Dunselman, G.; Dirksen, C.; Hummelshoj, L.; Bokor, A.; Brandes, I.; Brodszky, V.; Canis, M.; Colombo, G.L.; DeLeire, T.; et al. The burden of endometriosis: Costs and quality of life of women with endometriosis and treated in referral centres. Hum. Reprod. 2012, 27, 1292–1299. [Google Scholar] [CrossRef] [PubMed]
- Grundström, H.; Hammar Spagnoli, G.; Lövqvist, L.; Olovsson, M. Healthcare Consumption and Cost Estimates Concerning Swedish Women with Endometriosis. Gynecol. Obstet. Investig. 2020, 85, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Prast, J.; Oppelt, P.; Shamiyeh, A.; Shebl, O.; Brandes, I.; Haas, D. Costs of endometriosis in Austria: A survey of direct and indirect costs. Arch. Gynecol. Obstet. 2013, 288, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Gaal, P.; Velkey, Z.; Szerencses, V.; Webb, E. The 2020 reform of the employment status of Hungarian health workers: Will it eliminate informal payments and separate the public and private sectors from each other? Health Policy 2021, 125, 833–840. [Google Scholar] [CrossRef]
- Fuldeore, M.; Yang, H.; Du, E.X.; Soliman, A.M.; Wu, E.Q.; Winkel, C. Healthcare utilization and costs in women diagnosed with endometriosis before and after diagnosis: A longitudinal analysis of claims databases. Fertil. Steril. 2014, 103, 163–171. [Google Scholar] [CrossRef]
- Soliman, A.M.; Taylor, H.S.; Bonafede, M.; Nelson, J.K.; Castelli-Haley, J. Incremental direct and indirect cost burden attributed to endometriosis surgeries in the United States. Fertil. Steril. 2017, 107, 1181–1190.e2. [Google Scholar] [CrossRef]
- Estes, S.J.; Soliman, A.M.; Epstein, A.J.; Bond, J.C.; Gordon, K.; Missmer, S.A. National trends in inpatient endometriosis admissions: Patients, procedures and outcomes, 2006−2015. PLoS ONE 2019, 14, e0222889. [Google Scholar] [CrossRef]
- Chapron, C.; Marcellin, L.; Borghese, B.; Santulli, P. Rethinking mechanisms, diagnosis and management of endometriosis. Nat. Rev. Endocrinol. 2019, 15, 666–682. [Google Scholar] [CrossRef]
- Ducarme, G.; Planche, L.; Lebœuf, A. Screening and management of endometriosis by primary care physicians. (Repérage et prise en charge de l’endométriose en soins primaires par les médecins généralistes.). Gynecol. Obstet. Fertil. Senol. 2021, 49, 672–676. [Google Scholar] [CrossRef] [PubMed]
- The Governmental Decree no. 335/2009. (XII. 29.) on Diseases Classified as Severe Disability. Available online: https://net.jogtar.hu/jogszabaly?docid=a0900335.kor (accessed on 28 February 2023). (In Hungarian).
- World Health Organization. Endometriosis Severity Scale Value. In International Classification of Diseases for Mortality and Morbidity Statistics; 11th Revision; World Health Organization: Geneva, Switzerland, 2019; Available online: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/331649528 (accessed on 30 January 2023).
- Whitaker, L.H.R.; Byrne, D.; Hummelshoj, L.; Missmer, S.A.; Saraswat, L.; Saridogan, E.; Tomassetti, C.; Horne, A.W. Proposal for a new ICD-11 coding classification system for endometriosis. Eur. J. Obstet. Gynecol. 2019, 241, 134–135. [Google Scholar] [CrossRef] [PubMed]
- Becker, C.M.; Bokor, A.; Heikinheimo, O.; Horne, A.; Jansen, F.; Kiesel, L.; King, K.; Kvaskoff, M.; Nap, A.; Petersen, K.; et al. ESHRE guideline: Endometriosis. Hum. Reprod. Open 2022, 2022, hoac009. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).