Significance of Post-Traumatic Growth and Mental Health for Coping in Multiple Sclerosis Caregivers
Abstract
1. Introduction
2. Materials and Methods
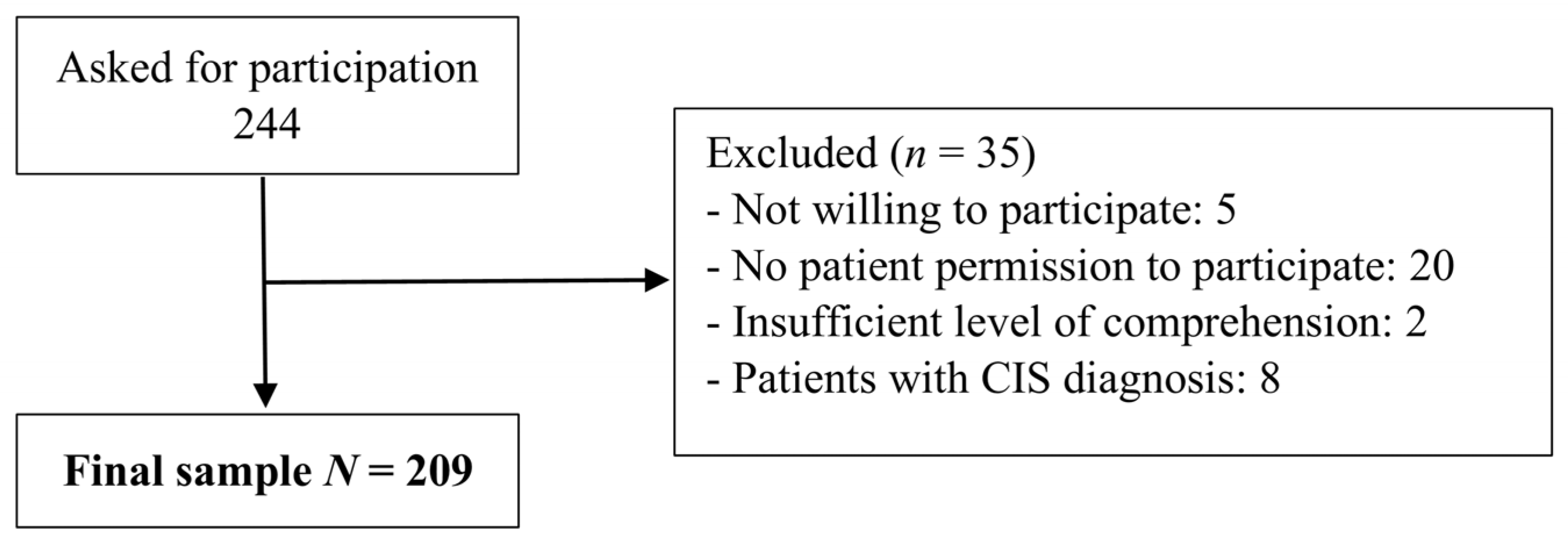
2.1. Sample and Procedure
2.2. Instruments
2.2.1. Health-Related Quality of Life
2.2.2. Mental Health Questionnaire (GHQ-28)
2.2.3. Post-Traumatic Growth
2.2.4. Coping Strategies
2.2.5. Social Support
2.3. Data Analysis
3. Results
3.1. Influence of Post-Traumatic Growth and Mental Health on Coping Strategies
3.2. Coping Strategies Predictors
4. Discussion
4.1. Influence of Post-Traumatic Growth and Mental Health on Coping Strategies
4.2. Coping Strategies Predictors
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- García-López, F.J.; García-Merino, A.; Alcalde-Cabero, E.; de Pedro-Cuesta, J. Incidence and prevalence of multiple sclerosis in Spain: A systematic review. Neurologia 2022, S2173–S5808. [Google Scholar] [CrossRef] [PubMed]
- Atlas of MS. Available online: https://www.atlasofms.org/map/united-kingdom/epidemiology/number-of-people-with-ms (accessed on 17 April 2023).
- Kavaliunas, A.; Karrenbauer, V.D.; Hillert, J. Socioeconomic consequences of multiple sclerosis. A systematic literature review. Acta Neurol. Scand. 2021, 143, 587–601. [Google Scholar] [CrossRef] [PubMed]
- Rajachandrakumar, R.; Finlayson, M. Multiple sclerosis caregiving: A systematic scoping review to map current state of knowledge. Health Soc. Care Commun. 2022, 30, e874–e897. [Google Scholar] [CrossRef]
- Di Cara, M.; Bonanno, L.; Rifici, C.; Sessa, E.; D’Aleo, G.; Corallo, F.; Lo Buono, V.; Venuti, G.; Bramanti, P.; Marino, S. Quality of life in patients with multiple sclerosis and caregivers predictive factors: An observational study. J. Clin. Neurosci. 2020, 78, 242–245. [Google Scholar] [CrossRef] [PubMed]
- Hlabangana, V.; Hearn, J.H. Depression in partner caregivers of people with neurological conditions: Associations with self-compassion and quality of life. J. Ment. Health 2020, 29, 176–181. [Google Scholar] [CrossRef]
- Merali, S.; Cameron, J.I.; Barclay, R.; Salbach, N.M. Experiences of people with stroke and multiple sclerosis and caregivers of a community exercise programme involving a healthcare-recreation partnership. Disabil. Rehabil. 2020, 42, 1220–1226. [Google Scholar] [CrossRef]
- Gafari, S.; Khoshknab, M.; Nourozi, K.; Mohamadi, E. Informal caregivers’ experiences of caring of multiple sclerosis patients: A qualitative study. Iran. J. Nurs. Midwifery Res. 2017, 22, 243–247. [Google Scholar]
- Maguire, R.; Maguire, P. Caregiver burden in multiple sclerosis: Recent trends and future directions. Curr. Neurol. Neurosci. Rep. 2020, 20, 18. [Google Scholar] [CrossRef]
- Kivi, M.S.; Jamei-Moghadam, M.; Khoshlahni, H.; Heidarzadeh, M.; Kamran, A.; Shahabi, H. Psychological changes in patients with multiple sclerosis. J. Holist. Nurs. Midwifery 2019, 29, 308–313. [Google Scholar]
- O’Brien, M.T. Multiple Sclerosis: Stressors and coping strategies in spousal caregivers. J. Community Health Nurs. 1993, 3, 123–135. [Google Scholar] [CrossRef]
- Montel, S.R.; Bungener, C. Coping and quality of life in 135 subjects with multiple sclerosis. Mult. Scler. 2007, 13, 393–401. [Google Scholar] [CrossRef]
- Courts, N.; Newton, A.; McNeal, L. Husbands and wives living with multiple sclerosis. J. Neurosci. Nurs. 2005, 37, 20–27. [Google Scholar] [CrossRef]
- Kouzoupis, A.B.; Paparrigopoulos, T.; Soldatos, M.; Papadimitriou, G.N. The family of the multiple sclerosis patient: A psychosocial perspective. Int. Rev. Psychiatry 2010, 22, 83–89. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Bassi, M.; Falautano, M.; Cilia, S.; Goretti, B.; Grobberio, M.; Pattini, M.; Pietrolongo, E.; Viterbo, R.G.; Amato, M.P.; Benin, M.; et al. Illness perception and well-being among persons with multiple sclerosis and their caregivers. J. Clin. Psychol. Med. Settings 2016, 23, 33–52. [Google Scholar] [CrossRef]
- Aspinwall, L.G. Future-oriented thinking, proactive coping, and the management of potential threats to health and well-being. In Oxford Handbook of Stress, Health, and Coping; Folkman, S., Ed.; Oxford University Press: Oxford, UK, 2010; Online edition; pp. 334–365. [Google Scholar]
- Martindale-Adams, J.; Zuber, J.; Levin, M.; Burns, R.; Graney, M.; Nichols, L.O. Integrating caregiver support into multiple sclerosis care. Mult. Scler. Int. 2020, 2020, 3436726. [Google Scholar] [CrossRef]
- Penwell-Waines, L.; Goodworth, M.R.; Casillas, R.S.; Rahn, R.; Stepleman, L. Perceptions of caregiver distress, health behaviors, and provider health-promoting communication and their relationship to stress management in MS caregivers. Health Commun. 2016, 31, 478–484. [Google Scholar] [CrossRef]
- Dȩbska, G.; Milaniak, I.; Skorupska-Król, A. The quality of life as a predictor of social support for multiple sclerosis patients and caregivers. J. Neurosci. Nurs. 2020, 52, 106–111. [Google Scholar] [CrossRef]
- Treder-Rochna, N. Adaptation to the disease—The psychological resources of families struggling with multiple sclerosis. Health Psychol. Rep. 2020, 8, 136–144. [Google Scholar] [CrossRef]
- van der Hiele, K.; van Gorp, D.A.M.; Heerings, M.A.P.; Jongen, P.J.; van der Klink, J.J.L.; Beenakker, E.A.C.; van Eijk, J.J.J.; Frequin, S.T.F.M.; van Geel, B.M.; Hengstman, G.J.D.; et al. Caregiver strain among life partners of persons with mild disability due to relapsing-remitting multiple sclerosis. Mult. Scler. Relat. Disord. 2019, 31, 5–11. [Google Scholar] [CrossRef]
- Vilagut, G.; Valderas, J.M.; Ferrer, M.; Garin, O.; López-García, E.; Alonso, J. Interpretation of SF-36 and SF-12 questionnaires in Spain: Physical and mental components. Med. Clin. 2008, 130, 726–735. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Turner-Bowker, D.M.; Gandek, B. How to Score Version 2 of the SF-12 Health Survey (with a Supplement Documenting Version 1); QualityMetric Incorporated: Lincoln, RI, USA, 2002. [Google Scholar]
- Maruish, M.E. User’s Manual for the SF-12v2 Health Survey, 3rd ed.; QualityMetric Incorporated: Lincoln, RI, USA, 2012. [Google Scholar]
- Goldberg, D.; Gater, R.; Sartorius, N.; Ustun, T.; Piccinelli, M.; Gureje, O.; Rutter, C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 1997, 27, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Willmott, S.; Boardman, J.; Henshaw, C.A.; Jones, P.W. Understanding general health questionnaire (GHQ-28) score and its threshold. Soc. Psychiatry Psychiatr. Epidemiol. 2004, 39, 613–617. [Google Scholar] [CrossRef] [PubMed]
- Lobo, A.; Pérez-Echeverría, M.J.; Artal, J. Validity of the scaled version of the general health questionnaire (GHQ-28) in a Spanish population. Psychol. Med. 1986, 16, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Vallejo, M.Á.; Rivera, J.; Esteve-Vives, J.; Rodríguez-Muñoz, M.D.; Icaf, G. The general health questionnaire (GHQ-28) in patients with fibromyalgia: Psychometric characteristics and adequacy. Clin. Salud 2014, 25, 105–110. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. The posttraumatic growth inventory: Measuring the positive legacy of trauma. J. Trauma Stress 1996, 9, 455–471. [Google Scholar] [CrossRef]
- Weiss, T.; Berger, R. Reliability and validity of a Spanish version of the posttraumatic growth inventory. Res. Soc. Work. Pract. 2006, 16, 191–199. [Google Scholar] [CrossRef]
- Carver, C.S. You want to measure coping but your protocol’s too long: Consider the brief COPE. Int. J. Behav. Med. 1997, 4, 92–100. [Google Scholar] [CrossRef]
- Morán, C.; Landero, R.; González, M.T. COPE-28: A psychometric analysis of the Spanish version of the brief COPE. Univ. Psychol. 2010, 9, 543–552. [Google Scholar] [CrossRef]
- Arechabala-Mantuliz, M.C.; Miranda-Castillo, C. Validation of a scale of perceived social support in a group of elders under control in a hypertension program in the metropolitan region. Cienc. Enferm. 2002, 208, 49–55. [Google Scholar]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The multidimensional scale of perceived social support. J. Pers. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates Publishers: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Henson, C.; Truchot, D.; Canevello, A. What promotes post traumatic growth? A systematic review. Eur. J. Trauma Dissoc. 2021, 5, 100195. [Google Scholar] [CrossRef]
- Neate, S.L.; Taylor, K.L.; Jelinek, G.A.; de Livera, A.M.; Simpson, S.; Bevens, W.; Weiland, T.J. On the path together: Experiences of partners of people with multiple sclerosis of the impact of lifestyle modification on their relationship. Health Soc. Care Community 2019, 27, 1515–1524. [Google Scholar] [CrossRef]
- Pérez-San-Gregorio, M.Á.; Martín-Rodríguez, A.; Borda-Mas, M.; Avargues-Navarro, M.L.; Pérez-Bernal, J.; Gómez-Bravo, M.Á. Coping strategies in liver transplant recipients and caregivers according to patient posttraumatic growth. Front Psychol. 2017, 8, 18. [Google Scholar] [CrossRef]
- Martin, L.; Rea, S.; Wood, F. A quantitative analysis of the relationship between posttraumatic growth, depression and coping styles after burn. Burns 2021, 47, 1748–1755. [Google Scholar] [CrossRef]
- Azimian, M.; Arian, M.; Shojaei, S.F.; Doostian, Y.; Barmi, B.E.; Khanjani, M.S. The effectiveness of group hope therapy training on the quality of life and meaning of life in patients with multiple sclerosis and their family caregivers. Iran. J. Psychiatry 2021, 16, 260–270. [Google Scholar] [CrossRef]
- Pakenham, K.I. Relations between coping and positive and negative outcomes in carers of persons with multiple sclerosis (MS). J. Clin. Psychol. Med. Settings 2005, 12, 25–38. [Google Scholar] [CrossRef]
- Wawrziczny, E.; Corrairie, A.; Antoine, P. Relapsing-remitting multiple sclerosis: An interpretative phenomenological analysis of dyadic dynamics. Disabil. Rehabil. 2021, 43, 76–84. [Google Scholar] [CrossRef]
- Kunz, S.; Joseph, S.; Geyh, S.; Peter, C. Coping and posttraumatic growth: A longitudinal comparison of two alternative views. Rehab. Psychol. 2018, 63, 240–249. [Google Scholar] [CrossRef]
- Calhoun, L.G.; Tedeschi, R.G. The foundations of posttraumatic growth: An expanded framework. In Handbook of Posttraumatic Growth: Research & Practice; Calhoun, L.G., Tedeschi, R.G., Eds.; Lawrence Erlbaum Associates Publishers: Hillsdale, NJ, USA, 2006; pp. 3–23. [Google Scholar]
- Treder-Rochna, N. Marital life and family adjustment to multiple sclerosis. Pol. Psychol. Bull. 2020, 51, 139–148. [Google Scholar]
- Santos, M.; Sousa, C.; Pereira, M.; Pereira, M.G. Quality of life in patients with multiple sclerosis: A study with patients and caregivers. Disabil. Health J. 2019, 12, 628–634. [Google Scholar] [CrossRef]
- Neate, S.L.; Taylor, K.L.; Jelinek, G.A.; de Livera, A.M.; Brown, C.R.; Weiland, T.J. Psychological shift in partners of people with multiple sclerosis who undertake lifestyle modification: An interpretive phenomenological study. Front. Psychol. 2018, 9, 15. [Google Scholar] [CrossRef] [PubMed]
- Gil-González, I.; Martín-Rodríguez, A.; Conrad, R.; Pérez-San-Gregorio, M.Á. Coping with multiple sclerosis: Reconciling significant aspects of health-related quality of life. Psychol. Health Med. 2022, 16, 1167–1180. [Google Scholar] [CrossRef] [PubMed]
- Gil-González, I.; Pérez-San-Gregorio, M.Á.; Conrad, R.; Martín-Rodríguez, A. Beyond the boundaries of disease-significant post-traumatic growth in multiple sclerosis patients and caregivers. Front. Psychol. 2022, 13, 903508. [Google Scholar] [CrossRef] [PubMed]
- Gil-González, I.; Martín-Rodríguez, A.; Conrad, R.; Pérez-San-Gregorio, M.Á. Quality of life in adults with multiple sclerosis: A systematic review. BMJ Open 2020, 10, e041249. [Google Scholar] [CrossRef]
| Post-Traumatic Growth Level | Intergroup Comparison | Effect Size | ||||
|---|---|---|---|---|---|---|
| Low (n = 69) | Medium (n = 69) | High (n = 71) | χ2 | p | Cohen’s w | |
| Gender n (%) | 1.67 | 0.433 | (N) | |||
| Male | 28 (40.57) | 35 (50.72) | 35 (49.29) | |||
| Female | 41 (59.43) | 34 (49.28) | 36 (50.70) | |||
| Partnership n (%) | 1.104 | 0.576 | (N) | |||
| No partner | 12 (17.39) | 8 (11.59) | 12 (16.90) | |||
| Partner | 57 (82.61) | 61 (88.41) | 59 (83.09) | |||
| Occupation n (%) | 7.569 | 0.053 | (S) | |||
| Employed/In education | 33 (47.82) | 48 (69.56) | 46 (64.78) | |||
| Unemployed | 36 (52.18) | 21 (30.44) | 25 (35.22) | |||
| Educational level n (%) | 9.449 | 0.051 | (S) | |||
| Primary education | 24 (34.78) | 11 (15.94) | 19 (26.76) | |||
| Secondary education | 24 (34.78) | 21 (30.43) | 23 (32.39) | |||
| University or higher | 21 (30.44) | 37 (53.63) | 29 (40.85) | |||
| MS subtype n (%) | 3.630 | 0.163 | (N) | |||
| Remittent | 50 (7.25) | 57 (82.61) | 60 (84.51) | |||
| Progressive | 19 (92.75) | 12 (17.39) | 11 (15.49) | |||
| Family Relation | 4.087 | 0.130 | (N) | |||
| Partners | 38 (55.07) | 48 (69.57) | 49 (69) | |||
| Others | 31 (44.93) | 21 (30.43) | 22 (31) | |||
| Cohabitation | 2.333 | 0.311 | (N) | |||
| Yes | 50 (72.46) | 51 (73.91) | 59 (83.10) | |||
| No | 19 (27.54) | 16 (26.09) | 12 (16.90) | |||
| F (2, 206) | p | Cohen’s d | ||||
| Age (M ± SD) | 49.97 ± 13.19 | 44.64 ± 12.46 | 47.87 ± 14.13 | 2.817 | 0.062 | (S) |
| EDSS (M ± SD) | 3.36 ± 2.08 | 3.84 ± 2.07 | 3.67 ± 2.34 | 1.046 | 0.353 | (N) |
| Months since diagnosis (M ± SD) | 153.96 ± 97.41 | 1.34.49 ± 89.16 | 158.23 ± 88.29 | 1.324 | 0.268 | (N) |
| Months since outbreak (M ± SD) | 195.16 ± 114.13 | 165.99 ± 102.33 | 201.76 ± 120.87 | 1.981 | 0.141 | (N) |
| Mental Health Level | Intergroup Comparison | Effect Size | ||||
|---|---|---|---|---|---|---|
| Low (n = 66) | Medium (n = 73) | High (n = 70) | χ2 | p | Cohen’s w | |
| Gender n (%) | 17.359 | <0.0001 | (M) | |||
| Male | 44 (66.67) | 32 (43.84) | 22 (31.43) | |||
| Female | 22 (33.33) | 41 (56.16) | 48 (68.57) | |||
| Partnership n (%) | 0.775 | 0.679 | (N) | |||
| No partner | 11 (16.67) | 9 (12.33) | 12 (17.14) | |||
| Partner | 55 (83.33) | 64 (87.67) | 58 (82.86) | |||
| Occupation n (%) | 1.862 | 0.397 | (N) | |||
| Employed/In education | 42 (63.64) | 47 (64.38) | 38 (54.29) | |||
| Unemployed | 24 (36.36) | 26 (35.62) | 32 (45.71) | |||
| Educational level n (%) | 5.265 | 0.261 | (N) | |||
| Primary education | 16 (24.24) | 17 (23.30) | 21 (30) | |||
| Secondary education | 16 (24.24) | 28 (38.35) | 24 (34.29) | |||
| University or higher | 34 (51.52) | 28 (38.35) | 25 (35.71) | |||
| MS subtype n (%) | 0.090 | 0.956 | (N) | |||
| Remittent | 52 (78.79) | 59 (80.82) | 56 (80) | |||
| Progressive | 14 (21.21) | 14 (19.18) | 14 (20) | |||
| Family Relation | 3.099 | 0.212 | (N) | |||
| Partners | 48 (72.73) | 46 (63) | 41 (58.57) | |||
| Others | 18 (27.27) | 27 (37) | 29 (41.43) | |||
| Cohabitation | 0.498 | 0.780 | (N) | |||
| Yes | 53 (80.30) | 55 (75.34) | 54 (77.14) | |||
| No | 13 (19.70) | 18 (24.66) | 16 (22.86) | |||
| F(2, 206) | p | Cohen’s d | ||||
| Age (M ± SD) | 50.39 ± 12.64 | 47.21 ± 13.33 | 45.03 ± 13.83 | 2.794 | 0.063 | (S) |
| EDSS (M ± SD) | 3.69 ± 2.32 | 3.68 ± 2.14 | 3.67 ± 2.11 | 0.491 | 0.613 | (N) |
| Months since diagnosis (M ± SD) | 151.23 ± 71.21 | 140.70 ± 86.09 | 155.50 ± 113.07 | 0.400 | 0.400 | (N) |
| Months since outbreak (M ± SD) | 184.82 ± 88.94 | 181.15 ± 116.23 | 197.46 ± 130.42 | 0.001 | 0.999 | (N) |
| Main Effects (Cohen’s f) | Interactive Effects | ||
|---|---|---|---|
| COPE-28 | Post-Traumatic Growth | Mental Health | F (2, 200) p |
| F (2, 200) | F (2, 200) | ||
| Acceptance | 2.410 0.157 S | 4.593 * 0.215 S | 0.463 0.763 |
| Emotional support | 13.691 ** 0.369 M | 2.616 0.160 S | 0.327 0.859 |
| Humor | 2.531 0.160 S | 0.188 0.044 N | 0.558 0.693 |
| Positive reframing | 8.035 ** 0.282 M | 0.778 0.089 N | 0.514 0.726 |
| Religion | 13.671 ** 0.368 M | 0.957 0.095 N | 1.087 0.364 |
| Active coping | 5.506 * 0.234 S | 0.382 0.063 N | 0.239 0.916 |
| Instrumental support | 5.306 * 0.229 S | 0.006 0.031 N | 0.215 0.930 |
| Planning | 3.267 * 0.181 S | 0.424 0.063 N | 0.545 0.703 |
| Behavioral disengagement | 3.069 0.175 S | 4.023 * 0.201 S | 0.871 0.482 |
| Denial | 3.361 * 0.176 S | 3.128 0.185 S | 1.224 0.302 |
| Self-distraction | 5.339 * 0.232 S | 3.521 * 0.188 S | 0.410 0.802 |
| Self-blaming | 9.636 ** 0.311 M | 1.997 0.142 S | 0.245 0.912 |
| Substance use | 2.040 0.142 S | 1.038 0.100 S | 1.402 0.235 |
| Venting | 3.554 * 0.188 S | 2.363 0.153 S | 1 0.409 |
| Post-Traumatic Growth Level M (SD) | Comparisons p (Cohen’s d) | |||||
|---|---|---|---|---|---|---|
| Low (a) n = 69 | Medium (b) n = 69 | High (c) n = 71 | Group Levels | |||
| a-b | a-c | b-c | ||||
| Acceptance | 2.03 (0.72) | 2.01 (0.63) | 2.23 (0.74) | 1 0.029 N | 0.157 −0.274 S | 0.201 −0.320 S |
| Emotional support | 0.86 (0.68) | 1.18 (0.76) | 1.58 (0.94) | 0.084 −0.443 S | <0.001 ** −0.877 L | 0.009 * −0.468 S |
| Humor | 0.81 (0.95) | 0.81 (0.90) | 1.12 (0.99) | 1 0 N | 0.135 −0.319 S | 0.191 −0.327 S |
| Positive reframing | 1.32 (0.74) | 1.53 (0.77) | 1.82 (0.78) | 0.290 −0.278 S | <0.001 ** −0.658 M | 0.062 −0.374 S |
| Religion | 0.59 (0.83) | 0.56 (0.80) | 1.27 (1.15) | 1 0.037 N | <0.001 ** −0.678 M | <0.001 ** −0.716 M |
| Active coping | 1.78 (0.75) | 1.95 (0.61) | 2.16 (0.65) | 0.394 −0.249 S | 0.003 * −0.541 M | 0.216 −0.333 S |
| Instrumental support | 1.04 (0.70) | 1.19 (0.63) | 1.45 (0.83) | 0.681 −0.225 S | 0.004 * −0.534 M | 0.134 −0.353 M |
| Planning | 1.40 (0.82) | 1.48 (0.70) | 1.71 (0.84) | 1 −0.577 M | 0.042 * −0.807 L | 0.237 −0.297 S |
| Behavioral disengagement | 0.22 (0.47) | 0.23 (0.42) | 0.44 (0.66) | 1 −0.022 N | 0.164 −0.384 S | 0.067 −0.377 S |
| Denial | 0.25 (0.46) | 0.47 (0.58) | 0.51 (0.73) | 0.158 −0.420 S | 0.044 * −0.426 S | 0.158 −0.061 N |
| Self-distraction | 0.96 (0.72) | 1.36 (0.85) | 1.42 (0.83) | 0.023 * −0.508 M | 0.010 * −0.592 M | 0.023 * −0.071 N |
| Self-blaming | 0.52 (0.57) | 0.79 (0.73) | 1.14 (0.92) | 0.176 −0.412 S | <0.001 * −0.810 L | 0.041 * −0.421 S |
| Substance use | 0.06 (0.24) | 0.09 (0.27) | 0.21 (0.58) | 1 −0.117 N | 0.456 −0.337 S | 1 −0.265 S |
| Venting | 0.63 (0.684) | 0.75 (0.59) | 0.97 (0.70) | 1 −0.188 N | 0.034 * −0.491 S | 0.162 −0.339 S |
| Mental Health Level M (SD) | Comparisons p (Cohen’s d) | |||||
|---|---|---|---|---|---|---|
| Low (a) n = 66 | Medium (b) n = 73 | High (c) n = 70 | Group Levels | |||
| a-b | a-c | b-c | ||||
| Acceptance | 2.28 (0.63) | 2 (0.64) | 1.99 (0.80) | 0.043 * 0.441 S | 0.018 * 0.403 S | 1 0.013 N |
| Emotional support | 1 (0.80) | 1.31 (0.82) | 1.30 (0.90) | 0.073 −0.383 S | 0.472 −0.352 S | 1 0.011 N |
| Humor | 0.95 (0.96) | 0.86 (0.88) | 0.94 (1) | 1 0.097 N | 1 0.010 N | 1 −0.084 N |
| Positive reframing | 1.63 (0.77) | 1.49 (0.71) | 1.55 (0.88) | 0.817 0.189 N | 0.135 0.096 N | 0.132 −0.075 N |
| Religion | 0.88 (1.11) | 0.80 (0.95) | 0.75 (0.94) | 1 0.077 N | 0.583 0.126 N | 0.865 0.053 N |
| Active coping | 1.96 (0.71) | 1.99 (0.56) | 1.96 (0.78) | 1 −0.046 N | 1 0 N | 1 0.044 N |
| Instrumental support | 1.21 (0.73) | 1.20 (0.63) | 1.27 (0.85) | 1 0.015 N | 1 −0.075 N | 1 −0.093 N |
| Planning | 1.58 (0.83) | 1.53 (0.66) | 1.51 (0.90) | 1 0.066 N | 1 0.080 N | 1 0.025 N |
| Behavioral disengagement | 0.18 (0.50) | 0.27 (0.47) | 0.44 (0.59) | 0.934 −0.186 S | 0.017 * −0.475 S | 0.200 −0.318 S |
| Denial | 0.25 (0.46) | 0.46 (0.66) | 0.50 (0.66) | 0.117 −0.369 S | 0.074 −0.439 S | 1 −0.060 N |
| Self-distraction | 1.04 (0.87) | 1.21 (0.68) | 1.47 (0.87) | 0.708 −0.217 S | 0.026 * −0.494 S | 0.392 −0.332 S |
| Self-blaming | 0.71 (0.84) | 0.73 (0.69) | 1 (0.83) | 1 −0.026 N | 0.247 −0.347 S | 0.258 −0.353 S |
| Substance use | 0.06 (0.27) | 0.10 (0.34) | 0.19 (0.53) | 1 −0.130 N | 0.456 −0.309 S | 1 −0.202 S |
| Venting | 0.64 (0.59) | 0.78 (0.63) | 0.92 (0.76) | 0.630 −0.229 S | 0.94 −0.411 S | 1 −0.200 S |
| F | R2 | B | SE.B | β | 1-β | f2 | |
|---|---|---|---|---|---|---|---|
| Proactive coping strategies | |||||||
| Model | 17.831 (6, 202) | 0.346 | 0.203 | 0.189 | 0.99 | 0.529 (L) | |
| Relating to others | 0.102 | 0.032 | 0.263 * | ||||
| Cohabitation | 0.289 | 0.070 | 0.244 ** | ||||
| Partner or other support | 0.062 | 0.021 | 0.171 * | ||||
| New possibilities | 0.076 | 0.033 | 0.186 * | ||||
| Physical role | 0.005 | 0.002 | 0.257 * | ||||
| Emotional role | 0.004 | 0.002 | 0.223 * | ||||
| Reactive coping strategies | |||||||
| Model | 24.718 (7, 201) | 0.463 | 0.319 | 0.119 | 0.99 | 0.862 (L) | |
| Relating to others | 0.097 | 0.016 | 0.327 ** | ||||
| Severe depression | 0.029 | 0.007 | 0.228 ** | ||||
| Mental health | −0.006 | 0.001 | −0.289 ** | ||||
| Vitality | 0.005 | 0.001 | 0.293 ** | ||||
| Emotional role | −0.004 | 0.001 | −0.241 * | ||||
| Other than partner relation | 0.107 | 0.043 | 0.134 * | ||||
| Physical role | 0.002 | 0.001 | 0.158 * | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gil-González, I.; Pérez-San-Gregorio, M.Á.; Funuyet-Salas, J.; Conrad, R.; Martín-Rodríguez, A. Significance of Post-Traumatic Growth and Mental Health for Coping in Multiple Sclerosis Caregivers. Healthcare 2023, 11, 1390. https://doi.org/10.3390/healthcare11101390
Gil-González I, Pérez-San-Gregorio MÁ, Funuyet-Salas J, Conrad R, Martín-Rodríguez A. Significance of Post-Traumatic Growth and Mental Health for Coping in Multiple Sclerosis Caregivers. Healthcare. 2023; 11(10):1390. https://doi.org/10.3390/healthcare11101390
Chicago/Turabian StyleGil-González, Irene, María Ángeles Pérez-San-Gregorio, Jesús Funuyet-Salas, Rupert Conrad, and Agustín Martín-Rodríguez. 2023. "Significance of Post-Traumatic Growth and Mental Health for Coping in Multiple Sclerosis Caregivers" Healthcare 11, no. 10: 1390. https://doi.org/10.3390/healthcare11101390
APA StyleGil-González, I., Pérez-San-Gregorio, M. Á., Funuyet-Salas, J., Conrad, R., & Martín-Rodríguez, A. (2023). Significance of Post-Traumatic Growth and Mental Health for Coping in Multiple Sclerosis Caregivers. Healthcare, 11(10), 1390. https://doi.org/10.3390/healthcare11101390






