Analysis of Patient Satisfaction through the Effect of Healthcare Spending on Waiting Times for Consultations and Operations
Abstract
1. Introduction
- The extraordinary development of Spanish public health care. Between 1984 and 2000, the number of public health accounts rose from 5800 million to 29,121 million.
- Its progressive decentralization, culminating in the total territorialization of public health care in 2002 and the assumption of complete authority over their own healthcare systems by the different autonomous communities [4].
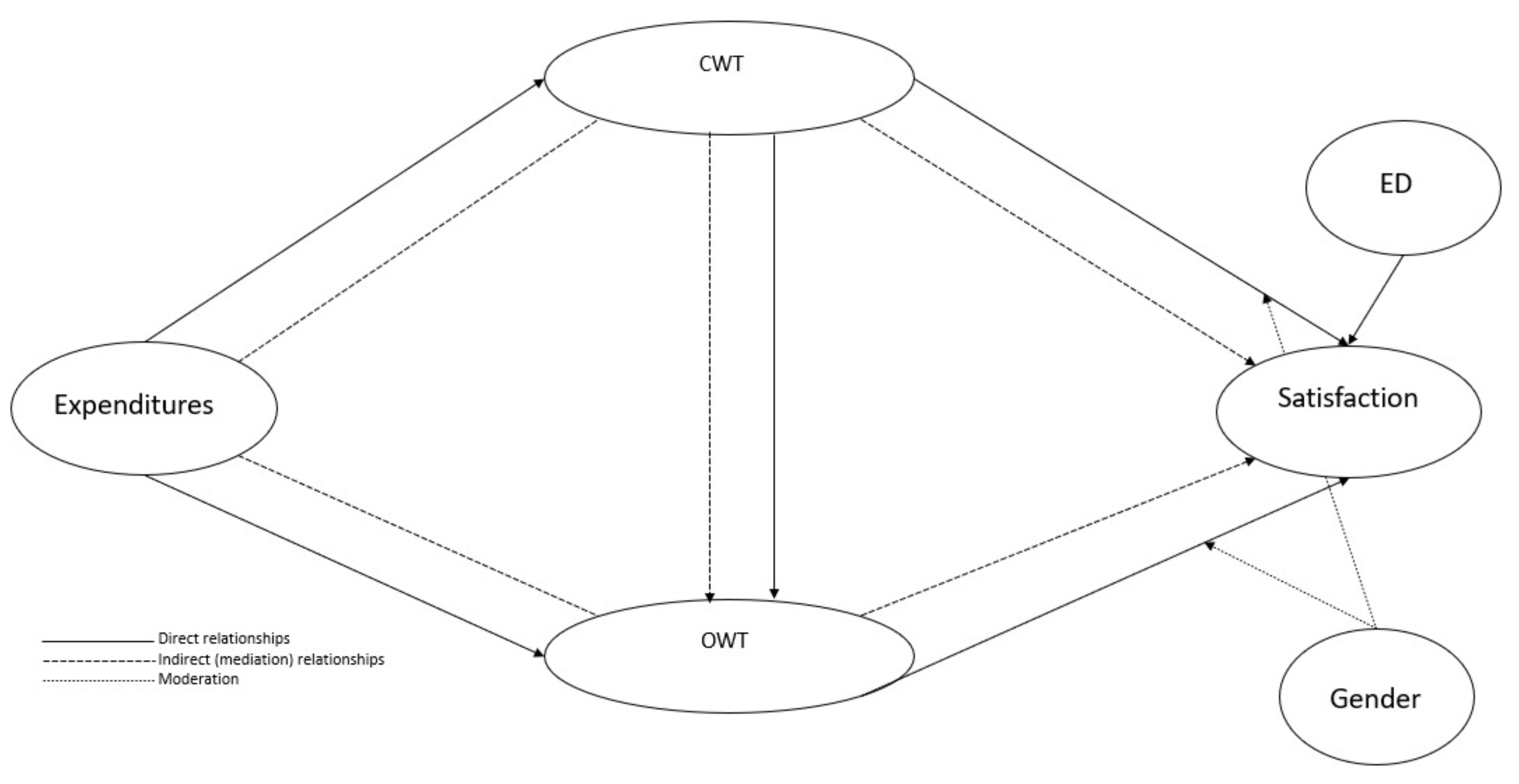
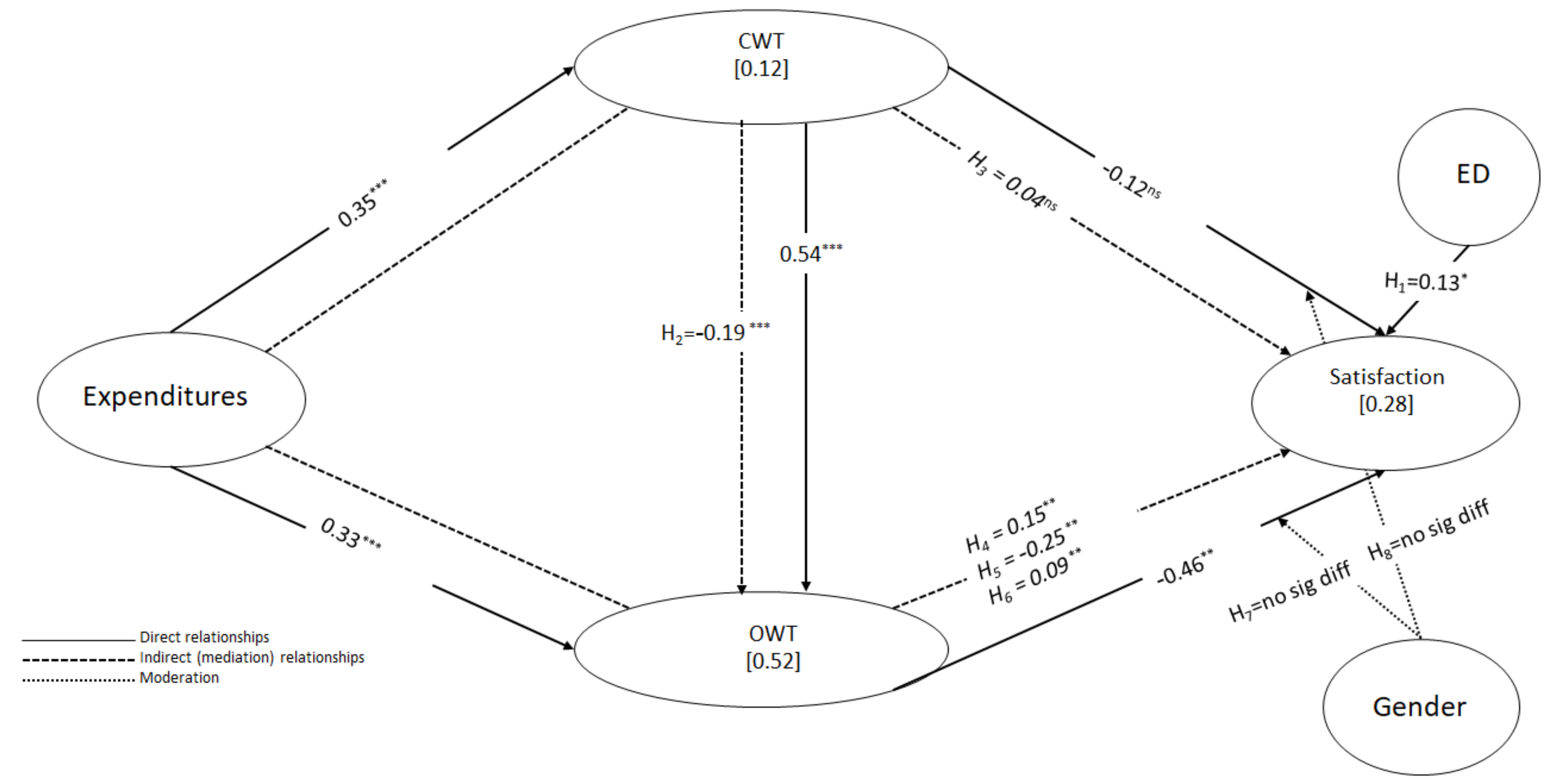
- Does consultant waiting time influence operation waiting time?
- Do waiting times for consultations and surgical procedures influence patient satisfaction?
- Does public healthcare expenditure influence waiting times and indirectly affect patient satisfaction?
- Does gender play a role in these relationships?
2. Methodology
2.1. Sample and Data Collection
2.2. Variables
2.3. Analytical Procedure
3. Results
3.1. Descriptive Analysis
3.2. Measurement Model
3.2.1. Mode A Composites
3.2.2. Composites Mode B
3.3. Structural Model Analysis
3.4. Further Analysis
3.5. Moderation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| MEN | Path | SD | T-Value | f2 | 95 CI | H | Supported | |
|---|---|---|---|---|---|---|---|---|
| Direct effects | VIF | |||||||
| Expenses -> CWT | −0.352 | 0.050 | 7.032 *** | 0.141 | [−0.452; −0.287] | 1.000 | ||
| Expenses -> OWT | −0.331 | 0.054 | 6.141 *** | 0.201 | [−0.423; −0.246] | 1.142 | ||
| ED -> Satisfaction | 0.08 | 0.12 | 0.667 ns | 0.008 | [−0.103; −0.292] | 1.14 | ||
| CWT -> Satisfaction | −0.066 | 0.165 | 0.399 ns | 0.003 | [−0.356; 0.190] | 1.878 | ||
| CWT -> OWT | 0.537 | 0.047 | 11.435 *** | 0.528 | [0.454; 0.609] | 1.142 | ||
| OWT -> Satisfaction | −0.500 | 0.258 | 1.937 * | 0.199 | [−0.693; −0.109] | 1.743 | H1 | Yes |
| Indirect effects | VAF | |||||||
| Individual indirect effects | ||||||||
| Expenses -> CWT -> OWT | −0.189 | 0.032 | 5.823 *** | [−0.252; −0.145] | 36.34 | H2 | Yes | |
| Expenses -> CWT -> Satisfaction | 0.023 | 0.065 | 0.355 ns | [−0.076; 0.137] | 8.15 | H3 | No | |
| CWT -> OWT -> Satisfaction | −0.268 | 0.14 | 1.910 * | [−0.406; −0.005] | 80.24 | H4 | Yes | |
| Expenses -> CWT -> OWT-> Satisfaction | 0.094 | 0.058 | 1.621 ns | [−0.020; 0.175] | 33.33 | H5 | No | |
| Expenses -> OWT -> Satisfaction | 0.166 | 0.097 | 1.707 * | [0.048; 0.255] | 58.86 | H6 | Yes | |
| Global indirect effects | ||||||||
| Expenses -> Satisfaction | 0.282 | 0.127 | 2.231 ** | [0.231; 0.345] | 100.00 | |||
| Expenses -> OWT | −0.189 | 0.032 | 5.823 *** | [−0.222; −0.132] | 36.34 | |||
| CWT -> Satisfaction | −0.268 | 0.140 | 1.910 * | [−0.406; −0.005] | 80.24 | |||
| Total effect | ||||||||
| Expenses -> Satisfaction | 0.282 | 0.127 | 2.231 ** | [0.231; 0.345] | ||||
| Expenses -> OWT | −0.520 | 0.041 | 12.611 *** | [−0.600; −0.465] | ||||
| CWT -> Satisfaction | −0.334 | 0.152 | 2.194 *** | [−0.515; −0.041] | ||||
| OWT -> Satisfaction | −0.500 | 0.258 | 1.937 * | [−0.693; −0.002] |
Appendix B
| WOMEN | Path | SD | T-Value | f2 | 95 CI | H | Supported | |
|---|---|---|---|---|---|---|---|---|
| Direct effects | VIF | |||||||
| Expenses -> CWT | −0.352 | 0.050 | 7.032 *** | 0.142 | [−0.452; −0.287] | 1.000 | ||
| Expenses -> OWT | −0.331 | 0.054 | 6.141 *** | 0.201 | [−0.423; −0.246] | 1.142 | ||
| ED -> Satisfaction | 0.148 | 0.122 | 1.217 ns | 0.027 | [−0.114; 0.301] | 1.139 | ||
| CWT -> Satisfaction | −0.137 | 0.139 | 0.979 ns | 0.014 | [−0.345; 0.118] | 1.876 | ||
| CWT -> OWT | 0.537 | 0.047 | 11.435 *** | 0.529 | [0.454; 0.609] | 1.142 | ||
| OWT -> Satisfaction | −0.463 | 0.354 | 1.310 ns | 0.173 | [−0.618; −0.569] | 1.746 | H1 | No |
| Indirect effects | VAF | |||||||
| Individual indirect effects | ||||||||
| Expenses -> CWT -> OWT | −0.189 | 0.032 | 5.823 *** | [−0.252; −0.145] | 36.27 | H2 | Yes | |
| Expenses -> CWT -> Satisfaction | 0.048 | 0.054 | 0.894 ns | [−0.045; 0.135] | 16.61 | H3 | No | |
| CWT -> OWT -> Satisfaction | −0.249 | 0.188 | 1.322 ns | [−0.364; 0.283] | 64.67 | H4 | No | |
| Expenses -> CWT -> OWT-> Satisfaction | 0.088 | 0.075 | 1.666 ns | [−0.106; 0.156] | 30.45 | H5 | No | |
| Expenses -> OWT -> Satisfaction | 0.153 | 0.129 | 1.188 ns | [−0.215; 0.228] | 52.94 | H6 | No | |
| Global indirect effects | ||||||||
| Expenses -> Satisfaction | 0.289 | 0.212 | 1.366 ns | [−0.321; 0.381] | 100.00 | |||
| Expenses -> OWT | −0.189 | 0.032 | 5.823 *** | [−0.222; −0.132] | 36.27 | |||
| CWT -> Satisfaction | −0.249 | 0.188 | 1.322 ns | [−0.364; 0.283] | 64.67 | |||
| Total effect | ||||||||
| Expenses -> Satisfaction | 0.289 | 0.212 | 1.366 ns | [−0.321; 0.381] | ||||
| Expenses -> OWT | −0.521 | 0.057 | 9.172 *** | [−0.638; −0.451] | ||||
| CWT -> Satisfaction | −0.385 | 0.247 | 1.558 ns | [−0.536; 0.319] | ||||
| OWT -> Satisfaction | −0.463 | 0.354 | 1.310 ns | [−0.618; 0.569] |
References
- Baril, C.; Gascon, V.; Vadeboncoeur, D. Discrete-event simulation and design of experiments to study ambulatory patient waiting time in an emergency department. J. Oper. Res. Soc. 2019, 70, 2019–2038. [Google Scholar] [CrossRef]
- World Health Organization. Global Expenditure on Health: Public Spending on the Rise? World Health Organization: New York, NY, USA, 2021. [Google Scholar]
- Valls Martínez, M.; Ramírez-Orellana, A. Patient Satisfaction in the Spanish National Health Service: Partial Least Squares Structural Equation Modeling. Int. J. Environ. Res. Public Health 2019, 16, 4886. [Google Scholar] [CrossRef] [PubMed]
- Moyano, M.C. Gasto público en sanidad y estado del bienestar. Rev. Adm. Sanit. 2003, 1, 619–656. [Google Scholar]
- Vieira, E.W.R.; Lima, T.M.N.; Gazzinelli, A. The waiting time for specialized medial consultations in a small municipality fo Minas Gerais, Brazil. REME Rev. Min. Enferm. 2015, 19. [Google Scholar] [CrossRef]
- Fun, W.H.; Tan, E.H.; Khalid, R.; Sararaks, S.; Tang, K.F.; Ab Rahim, I.; Md. Sharif, S.; Jawahir, S.; Sibert, R.M.Y.; Nawawi, M.K.M. Applying Discrete Event Simulation to Reduce Patient Wait Times and Crowding: The Case of a Specialist Outpatient Clinic with Dual Practice System. Healthcare 2022, 10, 189. [Google Scholar] [CrossRef]
- Laut, K.G.; Hjort, J.; Engstrøm, T.; Jensen, L.O.; Tilsted Hansen, H.-H.; Jensen, J.S.; Pedersen, F.; Jørgensen, E.; Holmvang, L.; Pedersen, A.B.; et al. Impact of Health Care System Delay in Patients With ST-Elevation Myocardial Infarction on Return to Labor Market and Work Retirement. Am. J. Cardiol. 2014, 114, 1810–1816. [Google Scholar] [CrossRef]
- Sauceda-Valenzuela, A.L.; Wirtz, V.J.; Santa-Ana-Téllez, Y.; de la Luz Kageyama-Escobar, M. Ambulatory health service users’ experience of waiting time and expenditure and factors associated with the perception of low quality of care in Mexico. BMC Health Serv. Res. 2010, 10, 1–11. [Google Scholar] [CrossRef]
- Fun, W.H.; Tan, E.H.; Sararaks, S.; Md. Sharif, S.; Ab Rahim, I.; Jawahir, S.; Eow, V.H.Y.; Sibert, R.M.Y.; Fadzil, M.M.; Mahmud, S.H. Implications of Dual Practice on Cataract Surgery Waiting Time and Rescheduling: The Case of Malaysia. Healthcare 2021, 9, 653. [Google Scholar] [CrossRef]
- Valls Martínez, M.d.C.; Ramírez-Orellana, A.; Grasso, M.S. Health Investment Management and Healthcare Quality in the Public System: A Gender Perspective. Int. J. Environ. Res. Public Health 2021, 18, 2304. [Google Scholar] [CrossRef]
- Atalan, A. A cost analysis with the discrete-event simulation application in nurse and doctor employment management. J. Nurs. Manag. 2022, 30, 733–741. [Google Scholar] [CrossRef]
- Knight, H.E.; Self, A.; Kennedy, S.H. Why are women dying when they reach hospital on time? A systematic review of the ‘third delay.’ . PLoS ONE 2013, 8, e63846. [Google Scholar]
- Carrière, G.; Sanmartin, C. Waiting time for medical specialist consultations in Canada, 2007. Health Rep. 2010, 21, 7. [Google Scholar]
- Chen, P.-S.; Chen, G.Y.-H.; Liu, L.-W.; Zheng, C.-P.; Huang, W.-T. Using Simulation Optimization to Solve Patient Appointment Scheduling and Examination Room Assignment Problems for Patients Undergoing Ultrasound Examination. Healthcare 2022, 10, 164. [Google Scholar] [CrossRef] [PubMed]
- Sanmartin, C.; Pierre, F.; Tremblay, S. Waiting for care in Canada: Findings from the health services access survey. Healthc. Policy 2006, 2, 43. [Google Scholar] [CrossRef][Green Version]
- Taimen, K.; Mustonen, A.; Pirilä, L. The Delay and Costs of Diagnosing Systemic Vasculitis in a Tertiary-Level Clinic. Rheumatol. Ther. 2021, 8, 233–242. [Google Scholar] [CrossRef]
- Palter, V.N.; Simpson, A.N.; Yeung, G.; Lee, J.Y.; Grantcharov, T.P.; Shore, E.M. Operating Room Utilization: A Retrospective Analysis of Perioperative Delays. J. Gynecol. Surg. 2020, 36, 109–114. [Google Scholar] [CrossRef]
- Kreindler, S.A. Policy strategies to reduce waits for elective care: A synthesis of international evidence. Br. Med. Bull. 2010, 95, 7–32. [Google Scholar] [CrossRef]
- Conill, E.M.; Giovanella, L.; Almeida, P.F. de Listas de espera em sistemas públicos: Da expansão da oferta para um acesso oportuno? Considerações a partir do Sistema Nacional de Saúde espanhol. Cien. Saude Colet. 2011, 16, 2783–2794. [Google Scholar] [CrossRef]
- Leddin, D.; Bridges, R.J.; Morgan, D.G.; Fallone, C.; Render, C.; Plourde, V.; Gray, J.; Switzer, C.; McHattie, J.; Singh, H. Survey of access to gastroenterology in Canada: The SAGE wait times program. Can. J. Gastroenterol. 2010, 24, 20–25. [Google Scholar] [CrossRef]
- Jaraiz, E.; Lagares, N.; Pereira, M. The components of patient satisfaction and their usefulness for hospital management. Rev. Esp. Cienc. Polit. 2013, 161–181. [Google Scholar]
- Manzoor, F.; Wei, L.; Hussain, A.; Asif, M.; Shah, S.I.A. Patient satisfaction with health care services; an application of physician’s behavior as a moderator. Int. J. Environ. Res. Public Health 2019, 16, 3318. [Google Scholar] [CrossRef] [PubMed]
- Barrasa, J.I.; Aibar, C. Revisión sistemática de los estudios de satisfacción realizados en España en el período 1986-2001. Rev. Calid. Asist. 2003, 18, 580–590. [Google Scholar] [CrossRef]
- Huynh, H.P.; Sweeny, K.; Miller, T. Transformational leadership in primary care: Clinicians’ patterned approaches to care predict patient satisfaction and health expectations. J. Health Psychol. 2018, 23, 743–753. [Google Scholar] [CrossRef] [PubMed]
- González, N.; Quintana, J.M.; Bilbao, A.; Esteban, C.; San Sebastián, J.A.; de la Sierra, E.; Aizpuru, F.; Escobar, A. Patient satisfaction in 4 hospitals of the Basque Health Service. Gac. Sanit. 2008, 22, 210–217. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mori, N.L.; Olbrich Neto, J.; Spagnuolo, R.S. Resolution, access and waiting time for specialties in different models of care. Rev. De Saude Publica 2015, 54. [Google Scholar] [CrossRef]
- Mira, J.J.; Aranaz, J. La satisfacción del paciente como una medida del resultado de la atención sanitaria. Med. Clin. 2000, 114, 26–33. [Google Scholar]
- Leon, M. Perceptions of health care quality in Central America. Int. J. Qual. Health Care 2003, 15, 67–71. [Google Scholar] [CrossRef]
- Gattinara, B.C.; Lbacache, J.; Puente, C.T.; Giaconi, J.; Caprara, A. Community perception on the quality of public health services delivery in the Norte and Ichilo districts of Bolivia. Cad. Saude Publica 1995, 11, 425–438. [Google Scholar] [CrossRef][Green Version]
- Cabrera-Arana, G.A.; Bello-Parías, L.D.; Londoño-Pimienta, J.L. Quality as perceived by people using hospitals in the Colombian health service network restructuring programme. Rev. Salud Pública 2008, 10, 593–604. [Google Scholar] [CrossRef][Green Version]
- Chaganty, S.S.; Sharma, H. Factors influencing peri-operative delays in neurosurgery operating theatres: A prospective study. Perioper. Care Oper. Room Manag. 2021, 23, 100160. [Google Scholar] [CrossRef]
- Hicks, K.B.; Glaser, K.; Scott, C.; Sparks, D.; McHenry, C.R. Enumerating the causes and burden of first case operating room delays. Am. J. Surg. 2020, 219, 486–489. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.; Khu, K.J.; Kaderali, Z.; Bernstein, M. Delays in the operating room: Signs of an imperfect system. Can. J. Surg. 2010, 53, 189. [Google Scholar] [PubMed]
- LeGrand, J. The distribution of public expenditure: The case of health care. Economica 1978, 45, 125–142. [Google Scholar] [CrossRef]
- Pérez-Romero, S.; Gascón-Cánovas, J.J.; Salmerón-Martínez, D.; Parra-Hidalgo, P.; Monteagudo-Piqueras, O. Relevance of the socioeconomic and health context in patient satisfaction. Gac. Sanit. 2017, 31, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Bleich, S.N.; Özaltin, E.; Murray, C.J.L. How does satisfaction with the health-care system relate to patient experience? Bull. World Health Organ. 2009, 87, 271–278. [Google Scholar] [CrossRef]
- Pérez-Romero, S.; Gascón-Cánovas, J.J.; Salmerón-Martínez, D.; Parra-Hidalgo, P.; Monteagudo-Piqueras, O. Sociodemographic characteristics and geographic variability associated with patient satisfaction in Primary Care. Rev. Calid. Asist. Organo la Soc. Esp. Calid. Asist. 2016, 31, 300–308. [Google Scholar] [CrossRef]
- Fernández-Pérez, Á.; Sánchez, Á. Improving people’s self-reported experience with the health services: The role of non-clinical factors. Int. J. Environ. Res. Public Health 2020, 17, 178. [Google Scholar] [CrossRef]
- Vodă, A.I.; Bostan, I.; Țigănaș, C.G. Impact of macroeconomic and healthcare provision factors on patient satisfaction. Curr. Sci. 2018, 115, 43–48. [Google Scholar] [CrossRef]
- Chang de la Rosa, M.; Alemán Lage, M.; Cañizares Pérez, M.; Ibarra, A.M. Satisfacción de los pacientes con la atención médica. Rev. Cuba. Med. Gen. Integr. 1999, 15, 541–547. [Google Scholar]
- Valls Martínez, M.d.C.; Santos-Jaén, J.M.; Soriano Román, R.; Martín-Cervantes, P.A. Are gender and cultural diversities on board related to corporate CO2 emissions? J. Clean. Prod. 2022, 363, 132638. [Google Scholar] [CrossRef]
- Panezai, S.; Ahmed, M.M.; Saqib, S.E. Gender differences in client satisfaction and its relationship with utilization of primary health care services in Pakistan. J Geogr. Soc. Sci 2019, 1, 30–43. [Google Scholar]
- Kolodinsky, J. Gender Differences in Satisfaction with Primary Care Physicians in a Managed Care Health Plan. Women Health 1998, 26, 67–86. [Google Scholar] [CrossRef]
- Kuosmanen, L.; Hätönen, H.; Jyrkinen, A.R.; Katajisto, J.; Välimäki, M. Patient satisfaction with psychiatric inpatient care. J. Adv. Nurs. 2006, 55, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Martínez, C.V.; Oller, I.M.P. Health investment management based on patient satisfaction with the primary care doctor in the Spanish national health service context. A gender perspective. MOJ Gerontol. Geriatr. 2019, 4, 204–211. [Google Scholar] [CrossRef]
- Indicadores clave del Sistema Nacional de Salud. Available online: http://inclasns.msssi.es/main.html (accessed on 7 May 2022).
- Bener, A.; Ghuloum, S. Gender difference on patients’ satisfaction and expectation towards mental health care. Niger. J. Clin. Pract. 2013, 16, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.-H.; Tran, D.-V.; Vo, H.-L.; Nguyen Si Anh, H.; Doan, T.-N.-H.; Nguyen, T.-H.-T. Outpatient Waiting Time at Vietnam Health Facilities: Policy Implications for Medical Examination Procedure. Healthcare 2020, 8, 63. [Google Scholar] [CrossRef]
- Sarstedt, M.; Hair, J.F.; Ringle, C.M.; Thiele, K.O.; Gudergan, S.P. Estimation issues with PLS and CBSEM: Where the bias lies! J. Bus. Res. 2016, 69, 3998–4010. [Google Scholar] [CrossRef]
- Hair, J.F.J.; Hult, G.T.M.; Ringle, C.M.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM), 3rd ed.; SAGE Publications Inc: Thousand Oaks, CA, USA, 2022. [Google Scholar]
- Rigdon, E.E. Choosing PLS path modeling as analytical method in European management research: A realist perspective. Eur. Manag. J. 2016, 34, 598–605. [Google Scholar] [CrossRef]
- Cepeda-Carrion, G.; Cegarra-Navarro, J.G.; Cillo, V. Tips to use partial least squares structural equation modelling (PLS-SEM) in knowledge management. J. Knowl. Manag. 2019, 23, 67–89. [Google Scholar] [CrossRef]
- Chin, W.W.; Dibbern, J. Handbook of Partial Least Squares; Springer: Berlin, Germany, 2010; pp. 171–193. [Google Scholar] [CrossRef]
- Sarstedt, M.; Henseler, J.; Ringle, C.M. Multigroup analysis in partial least squares (PLS) path modeling: Alternative methods and empirical results. Adv. Int. Mark. 2011, 22, 195–218. [Google Scholar] [CrossRef]
- Hair, J.F.; Risher, J.J.; Sarstedt, M.; Ringle, C.M. When to use and how to report the results of PLS-SEM. Eur. Bus. Rev. 2019, 31, 2–24. [Google Scholar] [CrossRef]
- Faul, F.; Buchner, A.; Erdfelder, E.; Mayr, S. A short tutorial of GPower. Tutor. Quant. Methods Psychol. 2007, 3, 51–59. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Earlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Ringle, C.M.; Wende, S.; Becker, J.-M. SmartPLS 3; SmartPSL GmbH: Boenningstedt, Germany, 2015. [Google Scholar]
- Streukens, S.; Leroi-Werelds, S. Bootstrapping and PLS-SEM: A step-by-step guide to get more out of your bootstrap results. Eur. Manag. J. 2016, 34, 618–632. [Google Scholar] [CrossRef]
- Hair, J.F.; Ringle, C.M.; Sarstedt, M. PLS-SEM: Indeed a silver bullet. J. Mark. Theory Pract. 2011, 19, 139–152. [Google Scholar] [CrossRef]
- Chin, W.W. The Partial Least Squares Approach to Structural Modeling. Mod. Methods Bus. Res. 1998, 295–336. [Google Scholar]
- Dijkstra, T.K.; Henseler, J. Consistent Partial Least Squares Path Modeling. MIS Q. 2015, 39, 297–316. [Google Scholar] [CrossRef]
- Henseler, J. Bridging Design and Behavioral Research With Variance-Based Structural Equation Modeling. J. Advert. 2017, 46, 178–192. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. Testing measurement invariance of composites using partial least squares. Int. Mark. Rev. 2016, 33, 405–431. [Google Scholar] [CrossRef]
- Falk, R.F.; Miller, N.B. A Primer for Soft Modeling; University of Akron Press: Akron, UK, 1992; ISBN 0962262846. [Google Scholar]
- Chin, W.W. How to write up and report PLS analyses. In Handbook of Partial Least Squares; Springer: Berlin, Germany, 2010; pp. 655–690. [Google Scholar]
- Palos-Sanchez, P.; Saura, J.R.; Velicia-Martin, F.; Cepeda-Carrion, G. A business model adoption based on tourism innovation: Applying a gratification theory to mobile applications. Eur. Res. Manag. Bus. Econ. 2021, 27, 100149. [Google Scholar] [CrossRef]
- Tenenhaus, M.; Vinzi, V.E.; Chatelin, Y.M.; Lauro, C. PLS path modeling. Comput. Stat. Data Anal. 2005, 48, 159–205. [Google Scholar] [CrossRef]
- Hu, L.-T.; Bentler, P.M. Fit indices sensitivity to misspecification. Psychol. Methods 1998, 3, 424–453. [Google Scholar] [CrossRef]
- Claver-Cortés, E.; Molina-Azorín, J.F.; Pereira-Moliner, J. The impact of strategic behaviours on hotel performance. Int. J. Contemp. Hosp. Manag. 2007. [Google Scholar] [CrossRef]
- Felipe, C.M.; Roldán, J.L.; Leal-Rodríguez, A.L. Impact of organizational culture values on organizational agility. Sustainability 2017, 9, 2354. [Google Scholar] [CrossRef]
- Hair, J.F.; Sarstedt, M.; Ringle, C.M.; Gudergan, S.P. Advanced Issues in Partial Least Squares Structural Equation Modeling; Sage Publications Sage CA: Los Angeles, CA, USA, 2017; ISBN 1483377385. [Google Scholar]
- Henseler, J.; Ringle, C.M.; Sinkovics, R.R. The use of partial least squares path modeling in international marketing. Adv. Int. Mark. 2009, 20, 277–319. [Google Scholar] [CrossRef]
- Zimmerman, D.W. A note on preliminary tests of equality of variances. Br. J. Math. Stat. Psychol. 2004, 57, 173–181. [Google Scholar] [CrossRef]
- Alfonso, C.M.; Roldán, J.L.; Sánchez-Franco, M.; O, M. De The moderator role of Gender in the Unified Theory of Acceptance and Use of Technology (UTAUT): A study on users of Electronic Document Management Systems. In Proceedings of the 7th International Conference Partial Least Squares and Related Methods, Houston, TX, USA, 19–22 May 2012; pp. 1–8. [Google Scholar]
| Expenditure (EXP) | |
| EXP_1 | Percentage of expenditure on specialized care services |
| EXP_2 | Percentage of spending on primary care services |
| EXP_3 | Percentage of expenditure on public–private contracts |
| EXP_4 | Percentage of spending on intermediate consumption |
| EXP_5 | Percentage of public health spending on staff remuneration for resident training |
| EXP_6 | Public health spending per capita |
| Consultant Waiting Time (CWT) | |
| CWT_1 | Waiting times for Gynecology consultations |
| CWT_2 | Waiting times for Ophthalmology consultations |
| CWT_3 | Waiting times for Traumatology consultations |
| CWT_4 | Waiting times for Dermatology consultations |
| CWT_5 | Otorhinolaryngology office waiting times |
| CWT_6 | General surgery office waiting times |
| CWT_7 | Waiting times for Urology consultations |
| CWT_8 | Waiting times for Digestive System consultations |
| CWT_9 | Waiting times for Cardiology consultations |
| Operation Waiting Time (OWT) | |
| OWT_1 | Waiting times for Gynecology procedures |
| OWT_2 | Waiting times for Ophthalmology procedures |
| OWT_3 | Waiting times for Traumatology procedures |
| OWT_4 | Waiting times for Dermatology procedures |
| OWT_5 | Waiting times for Otolaryngology procedures |
| OWT_6 | Waiting times for Cardiac surgery procedures |
| Satisfaction (SAS) | |
| SAS_1 | Degree of citizen satisfaction with the functioning of the public health system. |
| SAS_2 | Degree of citizen satisfaction with the family physician or pediatrician’s knowledge of the patient’s medical history, as well as any possible follow-up care. |
| SAS_3 | Degree of citizen satisfaction with the information received from the specialist regarding their health problems. |
| Economic Driver (ED) | |
| ED1 | Gross Domestic Product (GDP) per capita |
| Variables | Mean | SD | Variables | Mean | SD |
|---|---|---|---|---|---|
| CWT | Satisfaction (Total) | ||||
| CWT_1 | 57.366 | 43.188 | SAS_1 | 6.635 | 0.520 |
| CWT_2 | 68.968 | 34.453 | SAS_2 | 7.638 | 0.390 |
| CWT_3 | 71.645 | 29.724 | SAS_3 | 7.380 | 0.470 |
| CWT_4 | 59.008 | 23.465 | Satisfaction (Men) | ||
| CWT_5 | 40.855 | 20.109 | SAS_1 | 6.643 | 0.399 |
| CWT_6 | 42.468 | 27.079 | SAS_2 | 7.598 | 0.271 |
| CWT_7 | 52.629 | 30.701 | SAS_3 | 7.391 | 0.371 |
| CWT_8 | 54.452 | 29.301 | Satisfaction (Women) | ||
| CWT_9 | 50.573 | 24.697 | SAS_1 | 6.627 | 0.389 |
| OWT | SAS_2 | 7.684 | 0.242 | ||
| OWT_1 | 72.227 | 25.614 | SAS_3 | 7.364 | 0.365 |
| OWT_2 | 87.667 | 35.819 | Economic driver (ED) | ||
| OWT_3 | 114.107 | 47.078 | ED_1 | 23.101 | 4.765 |
| OWT_4 | 80.265 | 45.061 | |||
| OWT_5 | 57.254 | 28.053 | |||
| OWT_6 | 87.409 | 40.505 | |||
| Expenditure | |||||
| EXP_1 | 62.184 | 3.361 | |||
| EXP_2 | 13.976 | 1.636 | |||
| EXP_3 | 25.542 | 3.871 | |||
| EXP_4 | 3.649 | 0.841 | |||
| EXP_5 | 47.715 | 4.644 | |||
| EXP_6 | 1464.31 | 156.27 | |||
| Loading | t-Student *** | Q2 | α | ρA | ρC | AVE | |
|---|---|---|---|---|---|---|---|
| CWT | 0.065 | 0.907 | 0.925 | 0.924 | 0.578 | ||
| CWT_1 | 0.705 | 24.486 | 0.119 | ||||
| CWT_2 | 0.829 | 33.925 | 0.039 | ||||
| CWT_3 | 0.752 | 22.809 | 0.050 | ||||
| CWT_4 | 0.806 | 30.042 | 0.090 | ||||
| CWT_5 | 0.859 | 42.276 | 0.057 | ||||
| CWT_6 | 0.486 | 7.238 | 0.034 | ||||
| CWT_7 | 0.701 | 19.345 | -0.003 | ||||
| CWT_8 | 0.794 | 26.787 | 0.090 | ||||
| CWT_9 | 0.843 | 21.615 | 0.107 | ||||
| OWT | 0.300 | 0.850 | 0.906 | 0.892 | 0.594 | ||
| OWT_1 | 0.899 | 54.603 | 0.474 | ||||
| OWT_2 | 0.889 | 85.233 | 0.451 | ||||
| OWT_3 | 0.448 | 6.746 | 0.019 | ||||
| OWT_4 | 0.801 | 21.466 | 0.316 | ||||
| OWT_5 | 0.546 | 12.146 | 0.121 | ||||
| OWT_6 | 0.907 | 64.808 | 0.418 |
| CWT | OWT | |
|---|---|---|
| CWT | 0.760 | 0.676 |
| OWT | 0.653 | 0.770 |
| Variables | Weights | t | CI 2.5% | CI 97.5% | Loadings | VIF | Q2 |
|---|---|---|---|---|---|---|---|
| Expenditure | |||||||
| EXP_1 | 0.730 *** | 4.177 | 0.367 | 1.049 | 0.707 *** | 2.989 | |
| EXP_2 | 0.130 ns | 0.631 | −0.275 | 0.536 | −0.500 *** | 3.236 | |
| EXP_3 | 0.344 * | 2.169 | 0.009 | 0.628 | 0.621 *** | 2.338 | |
| EXP_4 | 0.463 *** | 3.983 | 0.226 | 0.678 | 0.639 *** | 2.151 | |
| EXP_5 | 0.414 ** | 2.737 | 0.094 | 0.688 | 0.013 ns | 1.618 | |
| EXP_6 | 0.229 ns | 1.842 | −0.023 | 0.464 | 0.147 *** | 1.581 | |
| Patient satisfaction (Total) | 0.038 | ||||||
| SAS_1 | 1.238 *** | 4.146 | 1.114 | 1.321 | 0.751 *** | 1.547 | 0.131 |
| SAS_2 | −0.357 *** | 2.249 | −0.610 | −0.036 | −0.052 ns | 1.677 | 0.003 |
| SAS_3 | −0.557 *** | 2.334 | −0.868 | −0.144 | −0.093 ns | 1.760 | 0.014 |
| Patient satisfaction (Men) | 0.023 | ||||||
| SAS_1 | 1.247 *** | 2.65 | −1.013 | 1.375 | 0.743 *** | 1.676 | 0.105 |
| SAS_2 | −0.131 ns | 0.501 | −0.680 | 0.374 | 0.110 * | 1.914 | 0.008 |
| SAS_3 | −0.747 ns | 1.526 | −1.167 | 1.182 | −0.120 * | 1.876 | 0.029 |
| Patient satisfaction (Women) | 0.030 | ||||||
| SAS_1 | 1.174 ns | 1.550 | −1.163 | 1.295 | 0.719 * | 1.448 | 0.104 |
| SAS_2 | −0.528 ns | 1.337 | −0.786 | 0.704 | −0.217 * | 1.597 | 0.001 |
| SAS_3 | −0.403 ns | 1.083 | −0.717 | 0.755 | −0.101 * | 1.713 | 0.012 |
| GLOBAL | Path | SD | T-Value | f2 | 95 CI | H | Supported | |
|---|---|---|---|---|---|---|---|---|
| Direct effects | VIF | |||||||
| Expenditure -> CWT | −0.352 | 0.050 | 7.032 *** | 0.142 | [−0.452; −0.287] | 1.000 | Yes | |
| Expenditure -> OWT | −0.331 | 0.054 | 6.141 *** | 0.201 | [−0.423; −0.246] | 1.142 | Yes | |
| CWT -> Satisfaction | −0.122 | 0.098 | 1.236 ns | 0.011 | [−0.280; 0.045] | 1.877 | No | |
| OWT -> Satisfaction | −0.461 | 0.143 | 3.228 ** | 0.168 | [−0.590; −0.316] | 1.745 | Yes | |
| CWT -> OWT | 0.537 | 0.047 | 11.435 *** | 0.529 | [0.454; 0.609] | 1.142 | Yes | |
| ED -> Satisfaction | 0.129 | 0.073 | 1.759 * | 0.020 | [0.005; −0.245] | 1.140 | H1 | Yes |
| Indirect effects | VAF | |||||||
| Individual indirect effects | ||||||||
| Expenditure -> CWT -> OWT | −0.189 | 0.032 | 5.823 *** | [−0.252; −0.145] | 36.34 | H2 | Yes | |
| Expenditure -> CWT -> Satisfaction | 0.043 | 0.036 | 1.176 ns | [−0.017; 0.103] | 15.14 | H3 | No | |
| Expenditure -> OWT -> Satisfaction | 0.153 | 0.054 | 2.804 ** | [0.097; 0.213] | 54.15 | H4 | Yes | |
| CWT -> OWT -> Satisfaction | −0.247 | 0.079 | 3.113 ** | [−0.335; −0.160] | 66.93 | H5 | Yes | |
| Expenditure -> CWT -> OWT-> Satisfaction | 0.087 | 0.033 | 2.676 ** | [0.053; 0.134] | 30.71 | H6 | Yes | |
| Global indirect effects | ||||||||
| Expenditure -> Satisfaction | 0.282 | 0.077 | 3.677 *** | [0.231; 0.345] | 100.00 | |||
| Expenditure -> OWT | −0.189 | 0.032 | 5.823 *** | [−0.252; −0.145] | 36.34 | |||
| CWT -> Satisfaction | −0.247 | 0.079 | 3.113 ** | [−0.335; −0.160] | 66.93 | |||
| Total effect | ||||||||
| Expenditure -> Satisfaction | 0.282 | 0.077 | 3.677 *** | [0.231; 0.345] | ||||
| Expenditure -> OWT | −0.52 | 0.041 | 12.611 *** | [−0.600; −0.465] | ||||
| CWT -> Satisfaction | −0.369 | 0.104 | 3.554 *** | [−0.481; −0.234] | ||||
| OWT -> Satisfaction | −0.461 | 0.143 | 3.228 ** | [−0590; −0.316] |
| Configuration Invariance (Same Algorithms for Both Groups) | Compositional Invariance | P-permutation Values | Partial Measurement Invariance Established | Equal Mean Assessment | Equal Variance Assessment | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Construct | Correlation original | 5.0% | Difference | CI 2.5% | CI 97.5% | Equal | Difference | CI 2.5% | CI 97.5% | Equal | Full Measurement Invariance Established | |||
| Expenses | Yes | 1.000 | 0.760 | 1.000 | Yes | −0.233 | 0.223 | −0.407 | 0.369 | |||||
| ED | Yes | 1.000 | 1.000 | 0.148 | Yes | −0.222 | 0.249 | −0.263 | 0.303 | |||||
| Satisfaction | Yes | 0.942 | 0.835 | 0.314 | Yes | 0.125 | −0.248 | 0.213 | Yes | −0.095 | −0.434 | 0.381 | Yes | Yes |
| CWT | Yes | 1.000 | 0.996 | 1.000 | Yes | −0.218 | 0.227 | −0.415 | 0.389 | |||||
| OWT | Yes | 1.000 | 0.995 | 0.996 | Yes | −0.219 | 0.251 | −0.346 | 0.356 | |||||
| PERMUTATION | TEST W-S | PARAMETRIC | ||||||
|---|---|---|---|---|---|---|---|---|
| Path Coefficients (Women) | Path Coefficients (Women) | Diff | p Value | T | p Value | T | p Value | |
| ED -> Satisfaction | 0.080 | 0.148 | −0.068 | 0.650 | 0.397 | 0.346 | 0.397 | 0.346 |
| CWT -> Satisfaction | −0.066 | −0.137 | 0.070 | 0.728 | 0.328 | 0.372 | 0.328 | 0.372 |
| OWT -> Satisfaction | −0.500 | −0.463 | −0.036 | 0.792 | 0.084 | 0.467 | 0.084 | 0.467 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos-Jaén, J.M.; Valls Martínez, M.d.C.; Palacios-Manzano, M.; Grasso, M.S. Analysis of Patient Satisfaction through the Effect of Healthcare Spending on Waiting Times for Consultations and Operations. Healthcare 2022, 10, 1229. https://doi.org/10.3390/healthcare10071229
Santos-Jaén JM, Valls Martínez MdC, Palacios-Manzano M, Grasso MS. Analysis of Patient Satisfaction through the Effect of Healthcare Spending on Waiting Times for Consultations and Operations. Healthcare. 2022; 10(7):1229. https://doi.org/10.3390/healthcare10071229
Chicago/Turabian StyleSantos-Jaén, José Manuel, María del Carmen Valls Martínez, Mercedes Palacios-Manzano, and Mayra Soledad Grasso. 2022. "Analysis of Patient Satisfaction through the Effect of Healthcare Spending on Waiting Times for Consultations and Operations" Healthcare 10, no. 7: 1229. https://doi.org/10.3390/healthcare10071229
APA StyleSantos-Jaén, J. M., Valls Martínez, M. d. C., Palacios-Manzano, M., & Grasso, M. S. (2022). Analysis of Patient Satisfaction through the Effect of Healthcare Spending on Waiting Times for Consultations and Operations. Healthcare, 10(7), 1229. https://doi.org/10.3390/healthcare10071229








