Comparison of the Injury Mechanism between Pregnant and Non-Pregnant Women Vehicle Passengers Using Car Crash Test Dummies
Abstract
:1. Introduction
2. Materials and Methods
3. Results
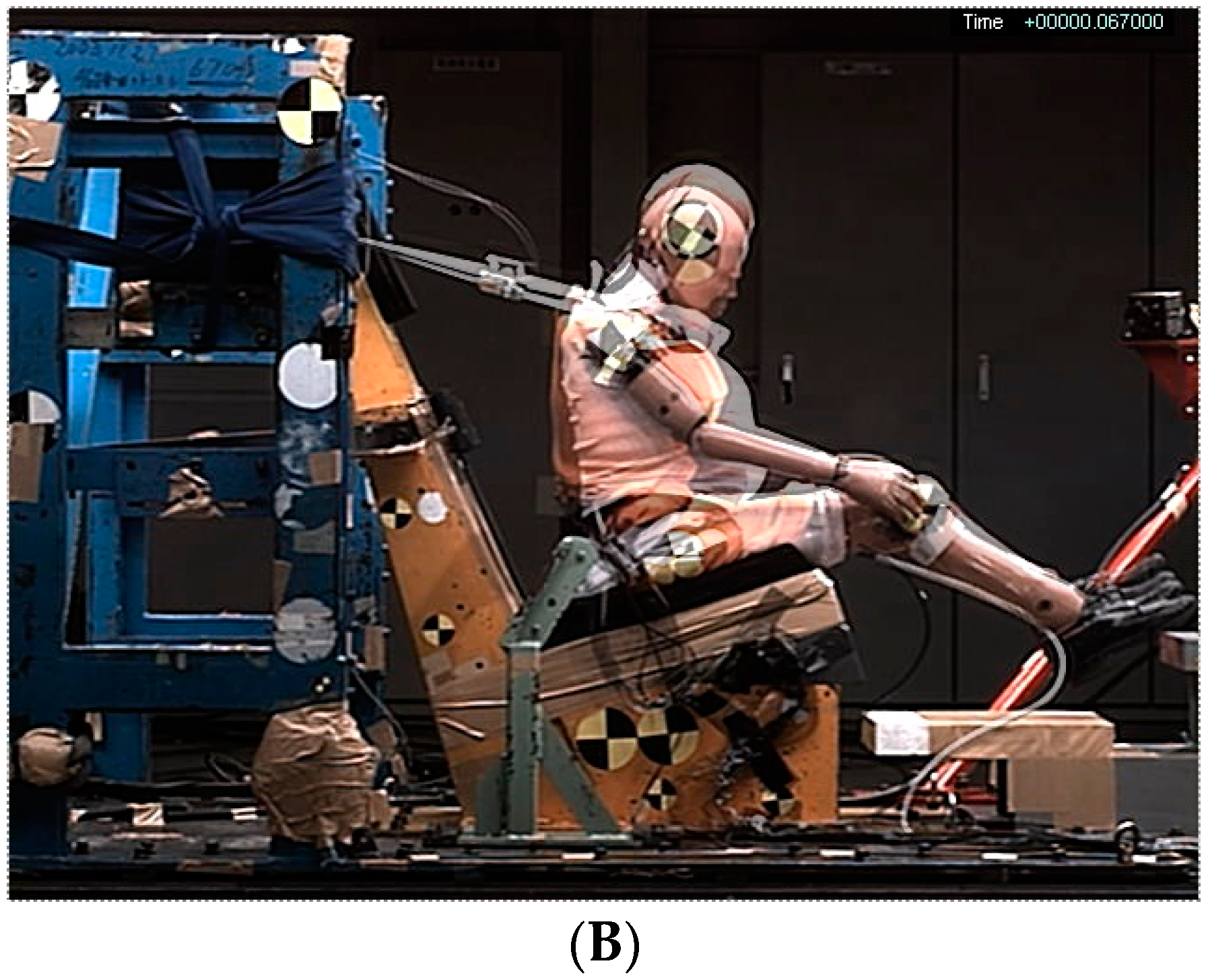
3.1. Kinematics of the Dummy
3.2. Resultant Acceleration of the Chest
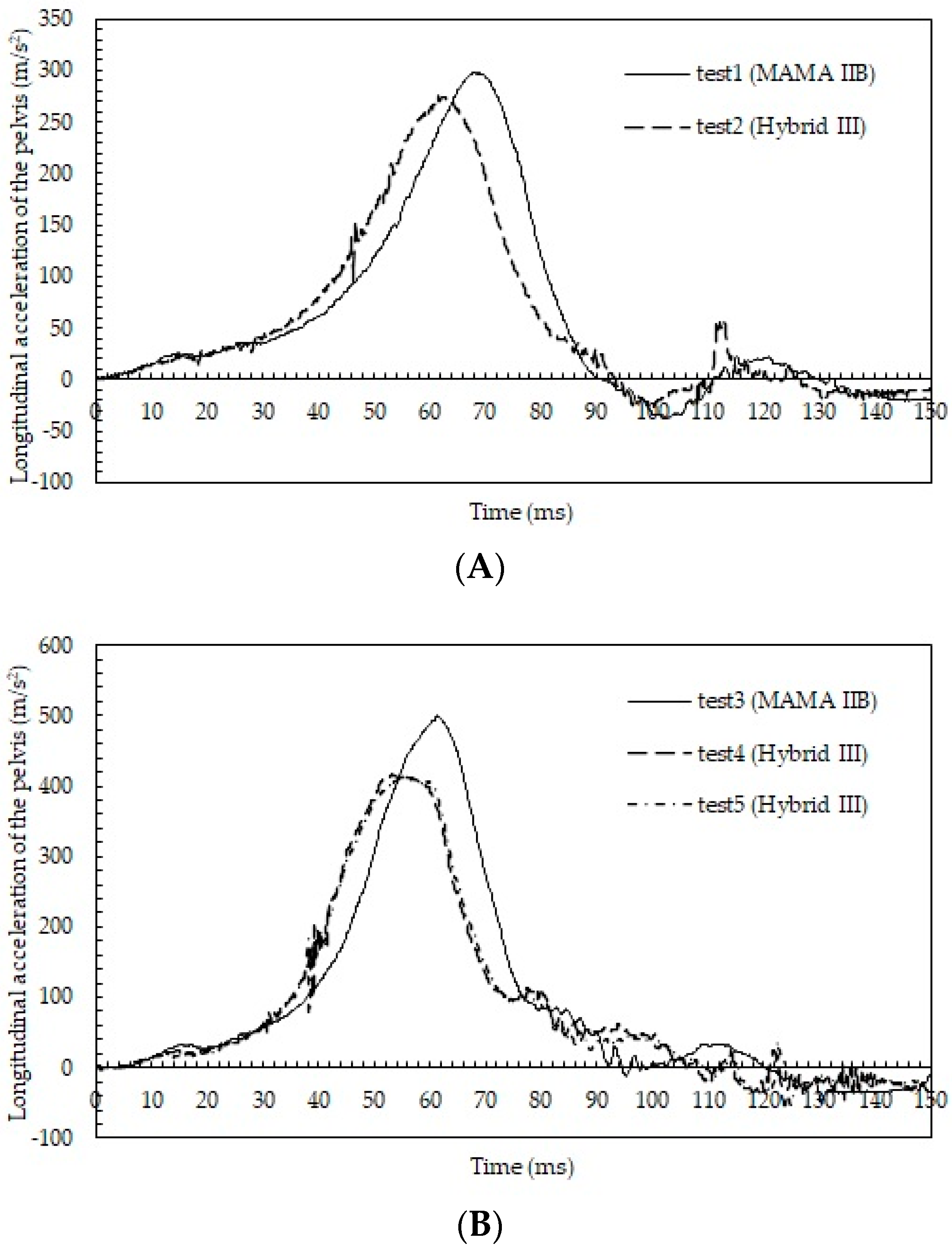
3.3. Longitudinal Acceleration of the Pelvis
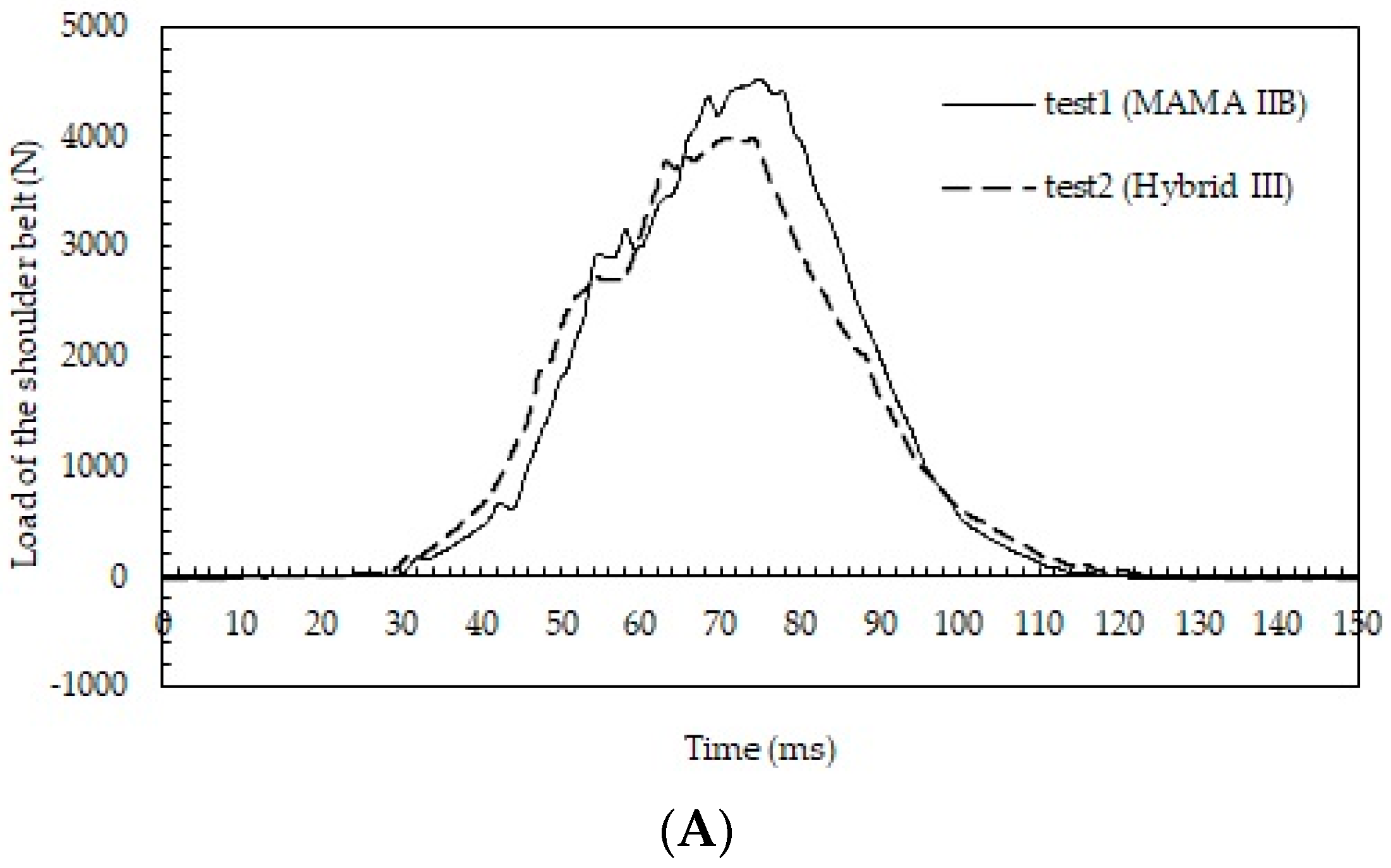
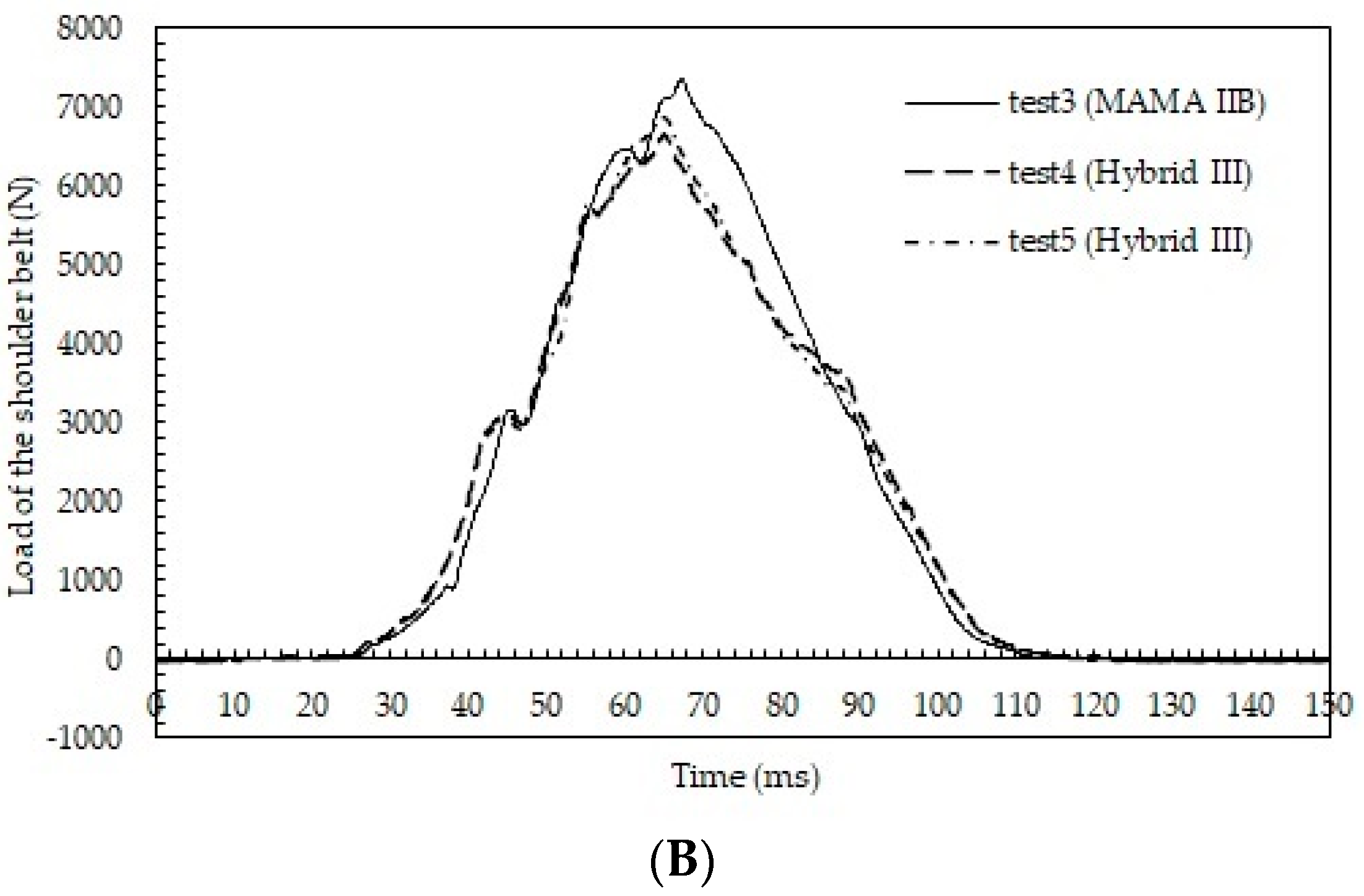
3.4. Belt Loads
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hill, C.C.; Pickinpaugh, J. Trauma and surgical emergencies in the obstetric patient. Surg. Clin. N. Am. 2008, 88, 421–440. [Google Scholar] [CrossRef] [PubMed]
- Oxford, C.M.; Ludmir, J. Trauma in pregnancy. Clin. Obstet. Gynecol. 2009, 52, 611–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petrone, P.; Jiménez-Morillas, P.; Axelrad, A.; Marini, C.P. Traumatic injuries to the pregnant patient: A critical literature review. Eur. J. Trauma Emerg. Surg. 2019, 45, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Duma, S.M. Pregnant Occupant Biomechanics—Advances in Automobile Safety Research; SAE: Warrendale, PA, USA, 2011. [Google Scholar]
- Klinich, K.D.; Schneider, L.W.; Eby, B.; Rupp, J.D.; Pearlman, M.D. Seated Anthropometry During Pregnancy; UMTRI: Ann Arbor, MI, USA, 1999; Report No.: UMTRI-99-16. [Google Scholar]
- Klinich, K.D.; Schneider, L.W.; Moore, J.L.; Pearlman, M.D. Investigations of Crashes Involving Pregnant Occupants: Final Report; UMTRI: Ann Arbor, MI, USA, 1999; Report No.: UMTRI-99-29. [Google Scholar]
- Pearlman, M.D. Motor vehicle crashes, pregnancy loss and preterm labor. Int. J. Gynaecol. Obstet. 1997, 57, 127–132. [Google Scholar] [CrossRef]
- Weiss, H.B. The Epidemiology of Perinatal Traumatic Fetal Injury Mortality. Ph.D. Dissertation, University of Pittsburgh, Pittsburgh, PA, USA, 1999. [Google Scholar]
- Miller, N.; Shental, T.B.; Peleg, K.; Fishman, A.; Olsha, O.; Givon, A.; Kessel, B. Are pregnant women safer in motor vehicle accidents? J. Perinat. Med. 2016, 44, 329–332. [Google Scholar] [CrossRef] [PubMed]
- Azar, T.; Longo, C.; Oddy, L.; Abenhaim, H.A. Motor vehicle collision-related accidents in pregnancy. J. Obstet. Gynecol. Res. 2015, 41, 1370–1376. [Google Scholar] [CrossRef]
- Manoogian, S. Comparison of pregnant and non-pregnant occupant crash and injury characteristics based on national crash data. Accid. Anal. Prev. 2015, 74, 69–76. [Google Scholar] [CrossRef]
- Owattanapanich, N.; Lewis, M.R.; Benjamin, E.R.; Wong, M.D.; Demetriades, D. Motor vehicle crashes in pregnancy: Maternal and fetal outcomes. J. Trauma Acute Care Surg. 2021, 90, 861–865. [Google Scholar] [CrossRef]
- Koh, S.; Hitosugi, M.; Moriguchi, S.; Baba, M.; Tsujimura, S.; Takeda, A.; Takaso, M.; Nakamura, M. Comparison of Motor Vehicle Collision Injuries between Pregnant and Non-Pregnant Women: A Nationwide Collision Data-Based Study. Healthcare 2021, 9, 1414. [Google Scholar] [CrossRef]
- Foster, C.D.; Hardy, W.N.; Yang, K.H.; King, A.I.; Hashimoto, S. High-speed seatbelt pretensioner loading of the abdomen. Stapp Car Crash J. 2006, 50, 27–51. [Google Scholar]
- Hitosugi, M.; Koseki, T.; Hariya, T.; Maeda, G.; Moriguchi, S.; Hiraizumi, S. Shorter pregnant women restrained in the rear seat of a car are at risk for serious neck injuries: Biomechanical analysis using a pregnant crash test dummy. Forensic Sci. Int. 2018, 291, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Klinich, K.D.; Flannagan, C.A.C.; Rupp, J.D.; Sochor, M.; Schneider, L.W.; Pearlman, M.D. Fetal outcome in motor-vehicle crashes: Effects of crash characteristics and maternal restraint. Am. J. Obstet. Gynecol. 2008, 198, 450.e1–450.e9. [Google Scholar] [CrossRef] [PubMed]
- Takeda, A.; Motozawa, Y.; Takaso, M.; Nakamura, M.; Hattori, S.; Hitosugi, M. Mechanisms of Negative Fetal Outcome in Frontal Vehicle Collisions Involving Unbelted Pregnant Drivers. Healthcare 2021, 9, 25. [Google Scholar] [CrossRef] [PubMed]
- Motozawa, Y.; Abe, T.; Hitosugi, M.; Tokudome, S. Analysis of Overall Kinematics and Abdominal Response of Pregnant Drivers during Frontal Vehicle Collisions; 09-01-0380; SAE Paper: Warrendale, PA, USA, 2009; pp. 1–10. [Google Scholar]
- Motozawa, Y.; Hitosugi, M.; Abe, T.; Tokudome, S. Analysis of the kinematics of pregnant drivers during low-speed frontal vehicle collisions. Int. J. Crashworthiness 2010, 15, 235–239. [Google Scholar] [CrossRef]
- Motozawa, Y.; Hitosugi, M.; Abe, T.; Tokudome, S. Effects of seat belts worn by pregnant drivers during low-impact collisions. Am. J. Obstet. Gynecol. 2010, 203, 62.e1–62.e8. [Google Scholar] [CrossRef]
- Hitosugi, M.; Tokudome, S. The effect of seatbelt tensioner for pregnant female drivers involved in rear-end vehicle collisions. Int. J. Crashworthiness 2009, 14, 483–487. [Google Scholar] [CrossRef]
- Rupp, J.D.; Klinich, K.D.; Moss, S.; Zhou, J.; Pearlman, M.D.; Schneider, L.W. Development and Testing of a Prototype Pregnant Abdomen for the Small-Female Hybrid III ATD. Stapp Car Crash J. 2001, 45, 61–78. [Google Scholar]
- Klinich, K.D.; Schneider, L.W.; Rupp, J.D.; Eby, B.; Pearlman, M.D. Challenges in Frontal Crash Protection of Pregnant Drivers Based on Anthropometric Considerations; No. 1999-01-0711; SAE Paper: Warrendale, PA, USA, 1999. [Google Scholar]
- Morikawa, M.; Yamada, T.; Kogo, H.; Sugawara, M.; Nishikawa, A.; Fukushi, Y.; Hirayama, E.K.; Ishioka, S.I.; Watari, H. Effect of an educational leaflet on the frequency of seat belt use and the rate of motor vehicle accidents during pregnancy in Japan in 2018: A prospective, non-randomised control trial with a questionnaire survey. BMJ Open 2019, 9, e031839. [Google Scholar] [CrossRef] [Green Version]
- Hitosugi, M.; Kido, M.; Maegawa, M.; Nagai, T.; Tokudome, S.; Motozawa, Y. The benefits of seatbelt use in pregnant women drivers. Forensic Sci. Int. 2007, 169, 274–275. [Google Scholar] [CrossRef]
- Motozawa, Y.; Hitosugi, M.; Tokudome, S. Analysis of seating position and anthropometric parameters of pregnant Japanese drivers. Traffic Inj. Prev. 2008, 9, 77–82. [Google Scholar] [CrossRef]
- Ichikawa, M.; Nakahara, S.; Okubo, T.; Wakai, S. Car seatbelt use during pregnancy in Japan: Determinants and policy implications. Inj Prev. 2003, 9, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, S.; Shinozaki, H.; Hayashi, K.; Itoh, M.; Soda, M.; Kameda, T.; Ozawa, K.; Yokota, H.; Kamioka, K.; Minegishi, T. Prevalence of rear seat belt use among pregnant women in a suburban area of Japan. J Obstet. Gynaecol. Res. 2018, 44, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Collins, A.C.; Miller, L.E.; Seeley, A.; Telehowski, P.M.; Atkinson, T.S. Analysis of restraint use in pregnant versus non-pregnant populations involved in motor vehicle collisions. Am. J. Surg. 2020, 220, 1304–1307. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, M. Pregnant women should wear seat belts. BMJ 1995, 311, 1501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hanahara, K.; Hitosugi, M.; Tateoka, Y. Education for appropriate seatbelt use required for early-phase pregnant women drivers. Sci. Rep. 2020, 10, 17609. [Google Scholar] [CrossRef] [PubMed]
- Ishiko, A.; Hitosugi, M.; Takaso, M.; Mizuno, K.; Tsuji, S.; Ono, T.; Kimura, F.; Murakami, T. Chest compression of a pregnant woman by a seatbelt might affect fetal outcome, even in minor to moderate frontal vehicle collisions. Forensic Sci. Int. 2019, 302, 109888. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuwahara, A.; Hitosugi, M.; Takeda, A.; Tsujimura, S.; Miyata, Y. Comparison of the Injury Mechanism between Pregnant and Non-Pregnant Women Vehicle Passengers Using Car Crash Test Dummies. Healthcare 2022, 10, 884. https://doi.org/10.3390/healthcare10050884
Kuwahara A, Hitosugi M, Takeda A, Tsujimura S, Miyata Y. Comparison of the Injury Mechanism between Pregnant and Non-Pregnant Women Vehicle Passengers Using Car Crash Test Dummies. Healthcare. 2022; 10(5):884. https://doi.org/10.3390/healthcare10050884
Chicago/Turabian StyleKuwahara, Ayumu, Masahito Hitosugi, Arisa Takeda, Seiji Tsujimura, and Yasuhito Miyata. 2022. "Comparison of the Injury Mechanism between Pregnant and Non-Pregnant Women Vehicle Passengers Using Car Crash Test Dummies" Healthcare 10, no. 5: 884. https://doi.org/10.3390/healthcare10050884
APA StyleKuwahara, A., Hitosugi, M., Takeda, A., Tsujimura, S., & Miyata, Y. (2022). Comparison of the Injury Mechanism between Pregnant and Non-Pregnant Women Vehicle Passengers Using Car Crash Test Dummies. Healthcare, 10(5), 884. https://doi.org/10.3390/healthcare10050884






