Preliminary Outcomes of Cervical Cerclage for Shortened Cervix with Decidual Polyp
Abstract
:1. Introduction
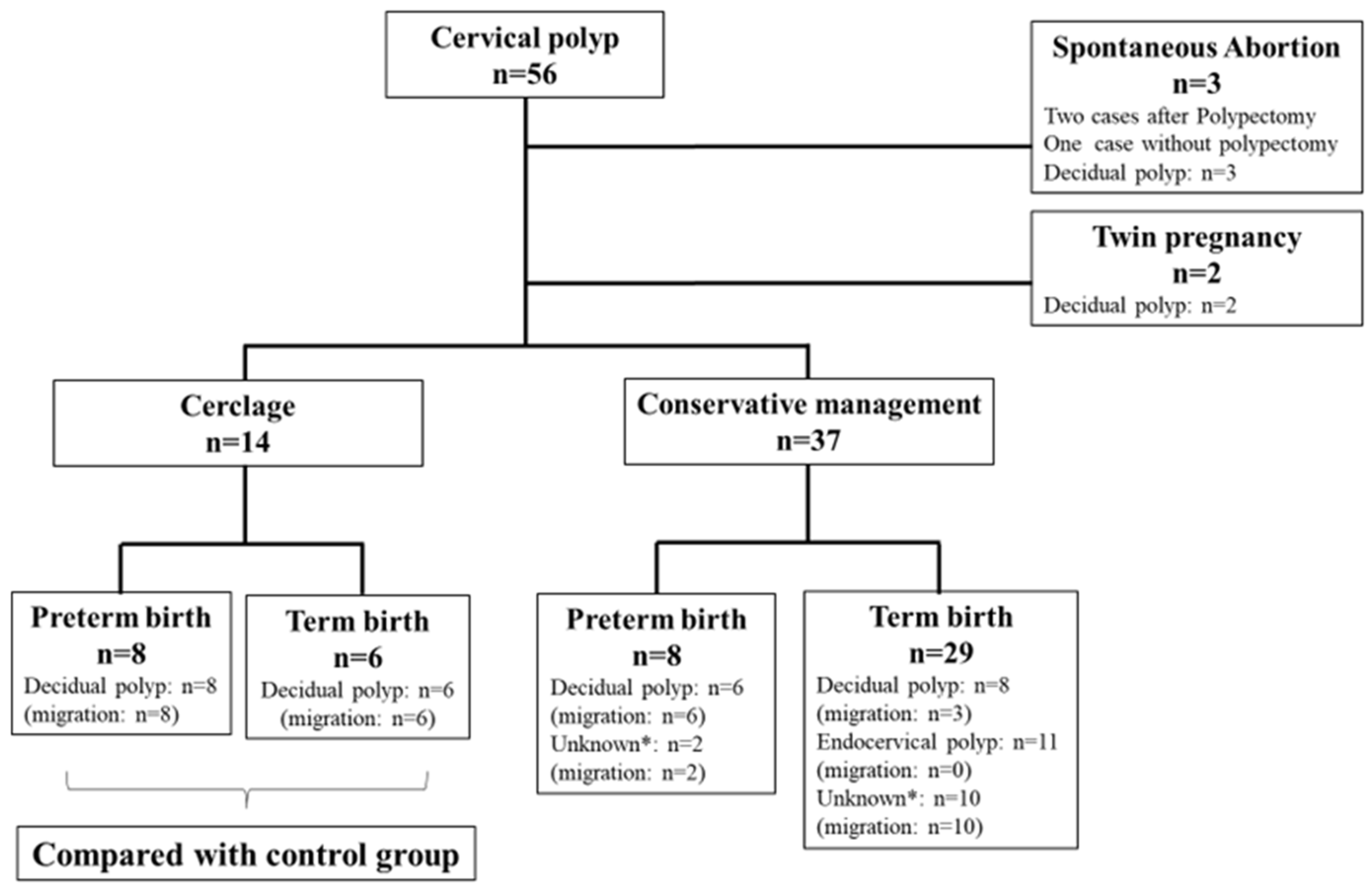
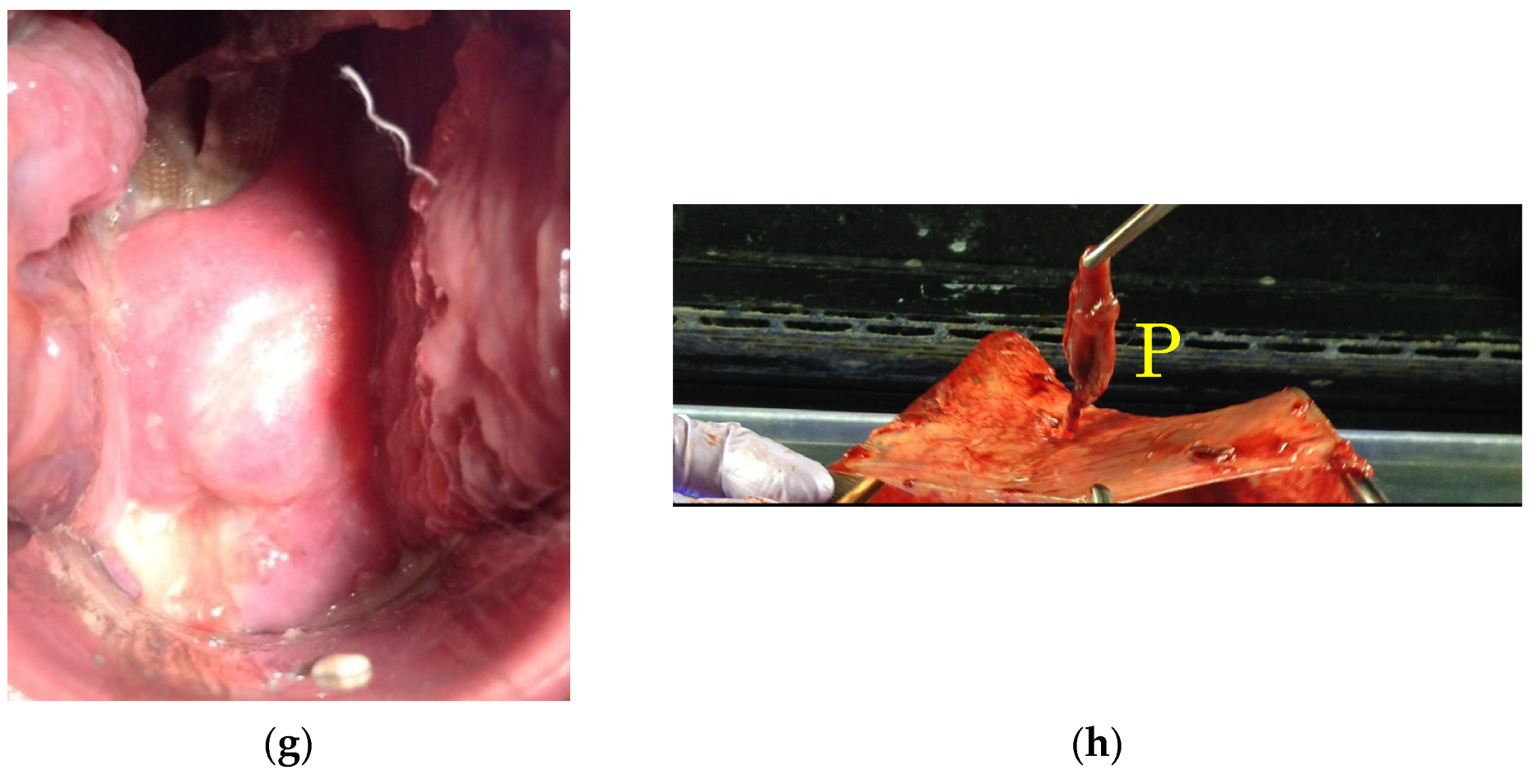
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Female Genital Tumors, 5th ed.; WHO Classification of Tumors: Lyon, France, 2020; p. 352. [Google Scholar]
- Tanos, V.; Berry, K.E.; Seikkula, J.; Abi Raad, E.; Stavroulis, A.; Sleiman, Z.; Campo, R.; Gordts, S. The management of polyps in female reproductive organs. Int. J. Surg. 2017, 43, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Younis, M.T.; Iram, S.; Anwar, B.; Ewies, A.A. Women with asymptomatic cervical polyps may not need to see a gynaecologist or have them removed: An observational retrospective study of 1126 cases. Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 150, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Berzolla, C.E.; Schnatz, P.F.; O’Sullivan, D.M.; Bansal, R.; Mandavilli, S.; Sorosky, J.I. Dysplasia and malignancy in endocervical polyps. J. Womens Health 2007, 16, 1317–1321. [Google Scholar] [CrossRef] [PubMed]
- Schnatz, P.F.; Ricci, S.; O’Sullivan, D.M. Cervical polyps in postmenopausal women: Is there a difference in risk? Menopause 2009, 16, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Tokunaka, M.; Hasegawa, J.; Oba, T.; Nakamura, M.; Matsuoka, R.; Ichizuka, K.; Otsuki, K.; Okai, T.; Sekizawa, A. Decidual polyps are associated with preterm delivery in cases of attempted uterine cervical polypectomy during the first and second trimester. J. Matern. Fetal Neonatal Med. 2015, 28, 1061–1063. [Google Scholar] [CrossRef] [PubMed]
- Levin, G.; Rottenstreich, A. 2nd trimester miscarriage following decidual polypectomy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 225, 262–263. [Google Scholar] [CrossRef] [PubMed]
- Fukuta, K.; Yoneda, S.; Yoneda, N.; Shiozaki, A.; Nakashima, A.; Minamisaka, T.; Imura, J.; Saito, S. Risk factors for spontaneous miscarriage above 12 weeks or premature delivery in patients undergoing cervical polypectomy during pregnancy. BMC Pregnancy Childbirth 2020, 20, 27. [Google Scholar] [CrossRef] [PubMed]
- Seo, N.; Tachibana, D.; Misugi, T.; Koyama, M.; Tanaka, S. First trimester findings of decidual polyp: Caution to avoid polypectomy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 249, 109–110. [Google Scholar] [CrossRef] [PubMed]
- Robertson, M.; Scott, P.; Ellwood, D.A.; Low, S. Endocervical polyp in pregnancy: Gray scale and color Doppler images and essential considerations in pregnancy. Ultrasound Obstet. Gynecol. 2005, 26, 583–584. [Google Scholar] [CrossRef] [PubMed]
- Conde-Agudelo, A.; Romero, R.; da Fonseca, E.; O’Brien, J.M.; Cetingoz, E.; Creasy, G.W.; Hassan, S.S.; Erez, O.; Pacora, P.; Nicolaides, K.H. Vaginal progesterone is as effective as cervical cerclage to prevent preterm birth in women with a singleton gestation, previous spontaneous preterm birth, and a short cervix: Updated indirect comparison meta-analysis. Am. J. Obstet. Gynecol. 2018, 219, 10–25. [Google Scholar] [CrossRef] [PubMed]


| DP Group (n = 14) | Control Group (n = 46) | p Value | |
|---|---|---|---|
| Age (year) | 36.0 (27–42) | 35.0 (20–49) | 0.982 a |
| Body mass index (kg/m2) | 22.8 (17.8–36.9) | 20.9 (16.2–34.2) | 0.393 a |
| Gravida | 2 (1–5) | 2 (1–6) | 0.42 a |
| Parity | 1 (0–3) | 1 (0–4) | 0.575 a |
| ART (n) | 2 (14.3%) | 10 (16.9 %) | 1 b |
| Cervical length at cerclage | 15 (9–24) | 17.3 (4.0–24.0) | 0.624 a |
| WBC at cerclage (/μL) | 8500 (7300–13,300) | 8700 (5200–16,000) | 0.259 a |
| CRP at cerclage (mg/dL) | 0.14 (0.02–0.75) | 0.13 (0.01–1.99) | 0.988 a |
| Gestational week at cerclage (week) | 18.4 (13.0–22.9) | 21.4 (17.0–24.9) | <0.001 a |
| Duration of tocolysis (day) | 8 (4–119) | 8 (1–92) | 0.375 a |
| Duration from cerclage to delivery (week) | 19.0 (8.7–23.4) | 14.9 (2.7–22.0) | 0.004 a |
| Gestational week at delivery (week) | 36.9 (27.6–41.9) | 37.1 (24.3–41.1) | 0.982 a |
| DP Group (n = 14) | Control Group (n = 46) | p Value | |
|---|---|---|---|
| Birthweight (g) | 2530 (884–3425) | 2815 (600–3780) | 0.197 a |
| Apgar score at 1 min | 8 (1–9) | 8 (1–9) | 0.088 a |
| Apgar score at 5 min | 9 (4–10) | 9 (1–10) | 0.64 a |
| pH of Umbilical artery | 7.29 (7.18–7.36) | 7.29 (7.09–7.41) | 0.812 a |
| Patient | Age | Parity | Diagnosis (Week) | Migration (Week) | Cerclage (Week) | CL at Cerclage (mm) | Delivery (Week) | CAM |
|---|---|---|---|---|---|---|---|---|
| 1 | 37 | 0 | 7.3 | 21.4 | 21.4 | 24 | 35.1 | Non |
| 2 | 34 | 0 | 7.3 | 19.0 | 19.0 | 13 | 36.0 | Stage1 |
| 3 | 30 | 2 | 7.4 | 20.1 | 20.1 | 20 | 36.9 | N/A |
| 4 | 40 | 1 | 7.7 | 17.6 | 17.6 | 16 | 39.1 | Stage2 |
| 5 a | 36 | 0 | 8.0 | 15.6 | 15.6 | 14 | 37.9 | Non |
| 6 | 28 | 0 | 8.6 | 34.4 | 14.9 | 22 | 38.3 | Stage2 |
| 7 b | 42 | 3 | 9.4 | 13.0 | 13.0 | 22 | 35.0 | Non |
| 8 | 37 | 1 | 10.1 | 14.1 | 18.1 | 0 c | 36.7 | Stage2 |
| 9 | 34 | 0 | 10.3 | 14.6 | 18.7 | 10 | 37.7 | Stage3 |
| 10 | 37 | 1 | 10.6 | 20.7 | 20.7 | 24 | 39.9 | N/A |
| 11 | 37 | 1 | 12.0 | 32.9 | 18.4 | 18 | 41.9 | Stage2 |
| 12 b | 27 | 0 | 17.9 | 21.1 | 18.0 | 9.0 | 33.0 | Stage2 |
| 13 | 36 | 0 | 19.1 | 19.1 | 19.1 | 10 | 28.0 | Non |
| 14 | 28 | 0 | 22.7 | 25.7 | 22.9 | 14 | 27.6 | Non |
| Median | 36 | 1 | 9.8 | 19.6 | 18.6 | 16 | 36.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Misugi, T.; Kitada, K.; Fudaba, M.; Tanaka, S.; Kurihara, Y.; Tahara, M.; Hamuro, A.; Nakano, A.; Koyama, M.; Tachibana, D. Preliminary Outcomes of Cervical Cerclage for Shortened Cervix with Decidual Polyp. Healthcare 2022, 10, 1312. https://doi.org/10.3390/healthcare10071312
Misugi T, Kitada K, Fudaba M, Tanaka S, Kurihara Y, Tahara M, Hamuro A, Nakano A, Koyama M, Tachibana D. Preliminary Outcomes of Cervical Cerclage for Shortened Cervix with Decidual Polyp. Healthcare. 2022; 10(7):1312. https://doi.org/10.3390/healthcare10071312
Chicago/Turabian StyleMisugi, Takuya, Kohei Kitada, Megumi Fudaba, Sayaka Tanaka, Yasushi Kurihara, Mie Tahara, Akihiro Hamuro, Akemi Nakano, Masayasu Koyama, and Daisuke Tachibana. 2022. "Preliminary Outcomes of Cervical Cerclage for Shortened Cervix with Decidual Polyp" Healthcare 10, no. 7: 1312. https://doi.org/10.3390/healthcare10071312
APA StyleMisugi, T., Kitada, K., Fudaba, M., Tanaka, S., Kurihara, Y., Tahara, M., Hamuro, A., Nakano, A., Koyama, M., & Tachibana, D. (2022). Preliminary Outcomes of Cervical Cerclage for Shortened Cervix with Decidual Polyp. Healthcare, 10(7), 1312. https://doi.org/10.3390/healthcare10071312







