Assessing Psychological Impact of COVID-19 among Parents of Children Returning to K-12 Schools: A U.S. Based Cross-Sectional Survey
Abstract
:1. Introduction
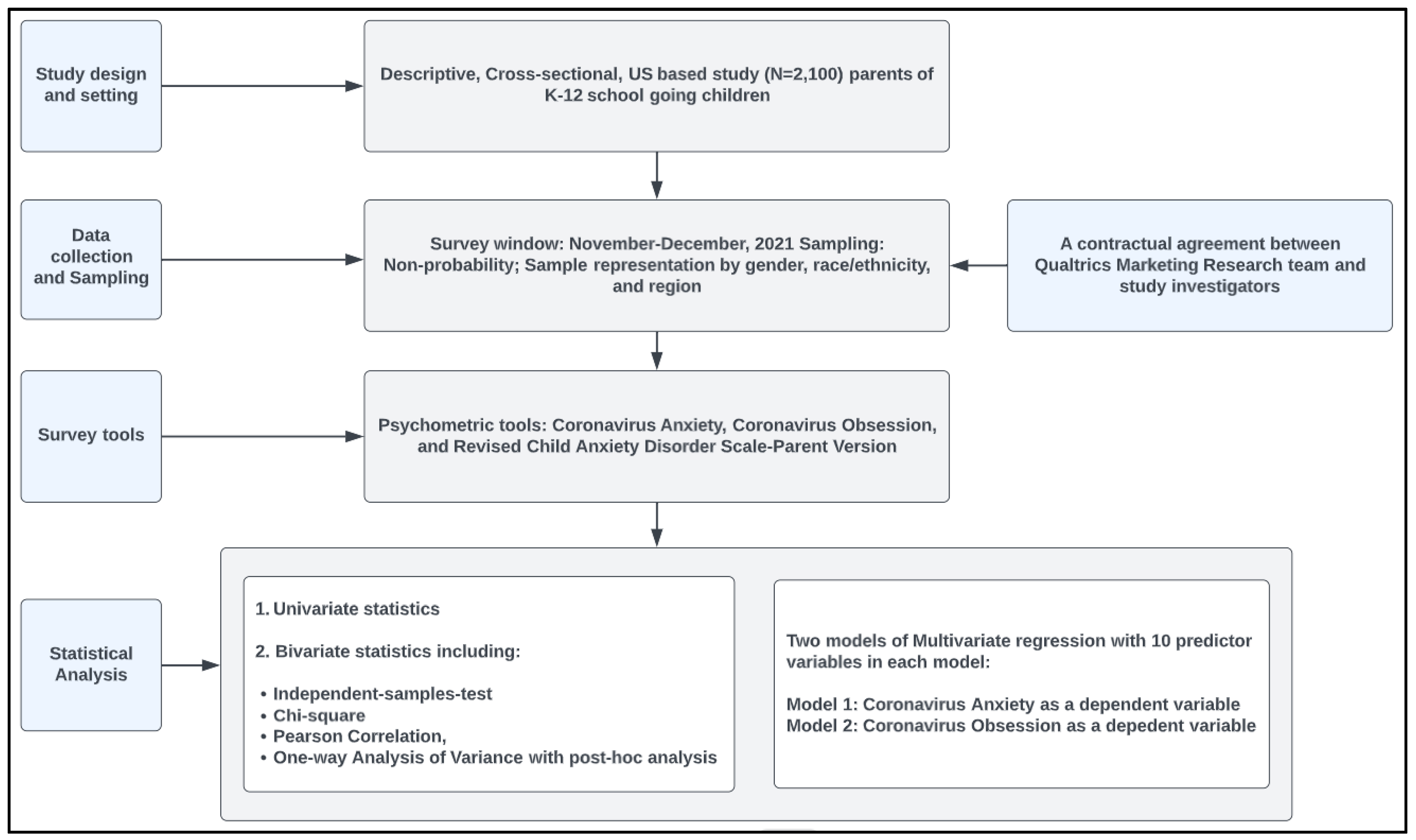
2. Materials and Methods
2.1. Study Design and Eligibility Criteria
2.2. Data Collection and Sampling Procedure
2.3. Ethical Considerations
2.4. Quality Assurance of Data
2.5. Survey Instrument
2.6. Sample Size Justification
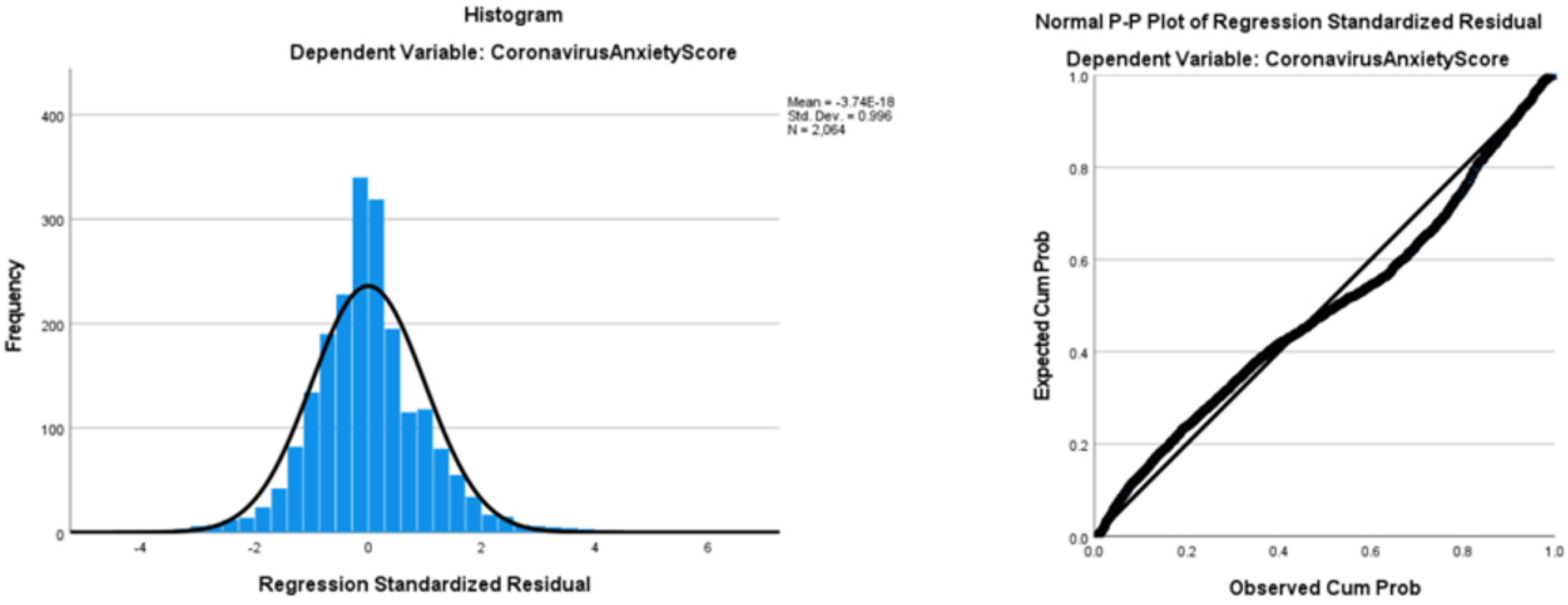
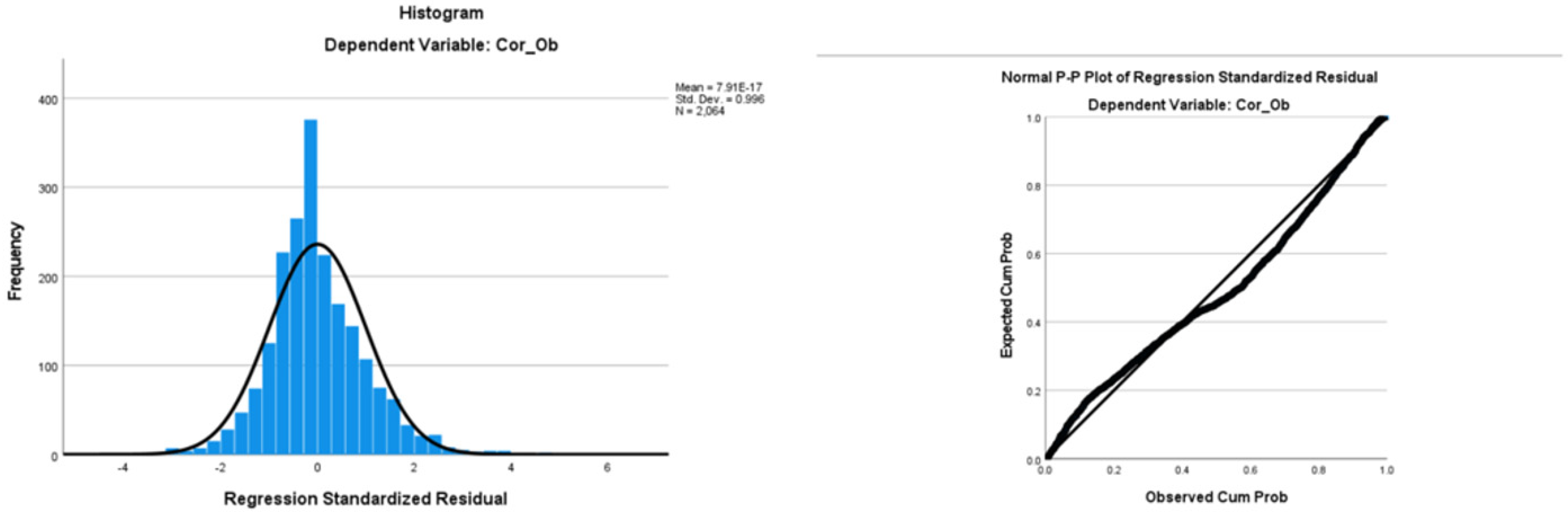
2.7. Data Analysis
3. Results
3.1. Univariate Statistics
3.2. Bivariate Statistics
3.3. Multiple Linear Regression
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
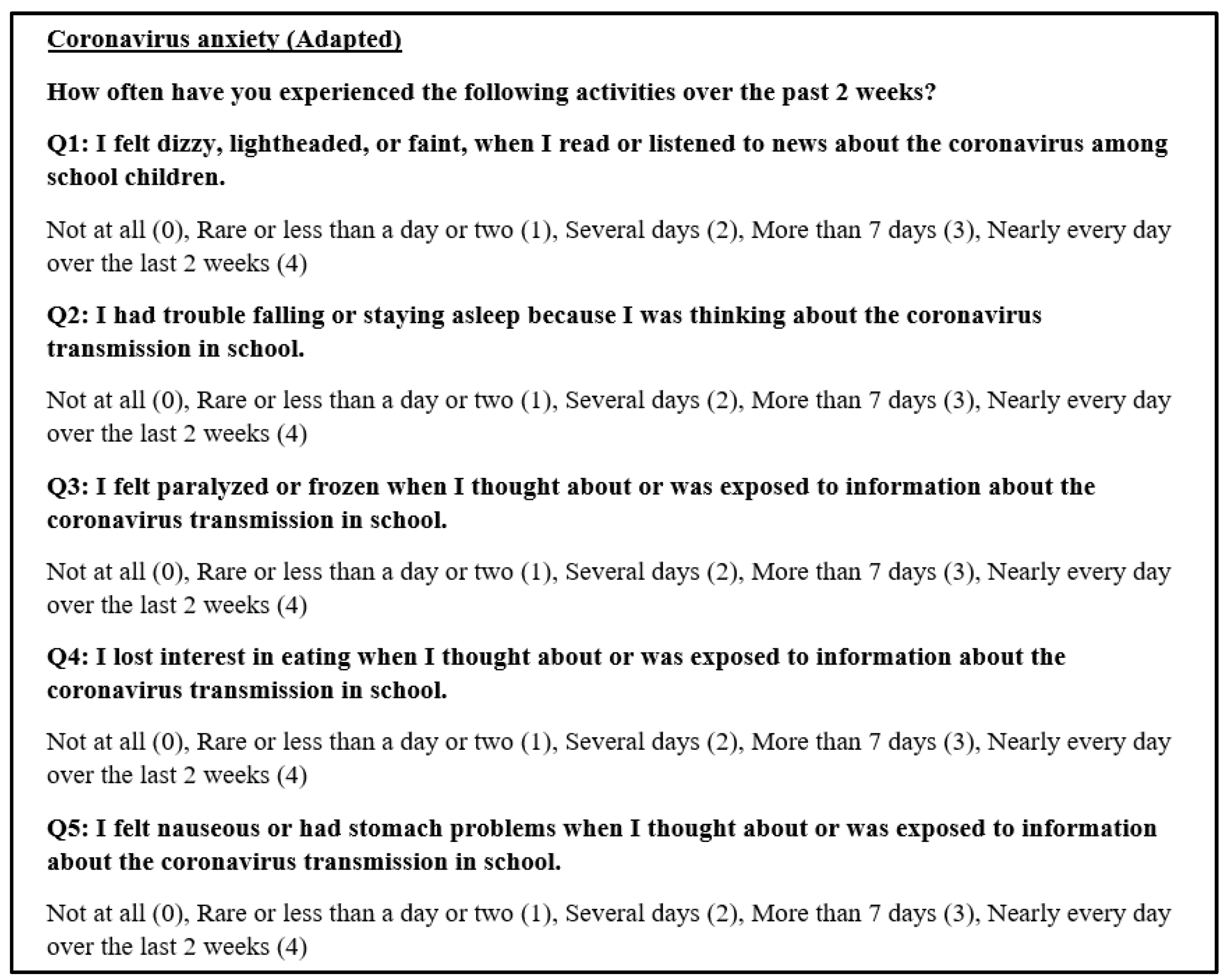
Appendix A.1. Coronavirus Anxiety Scale
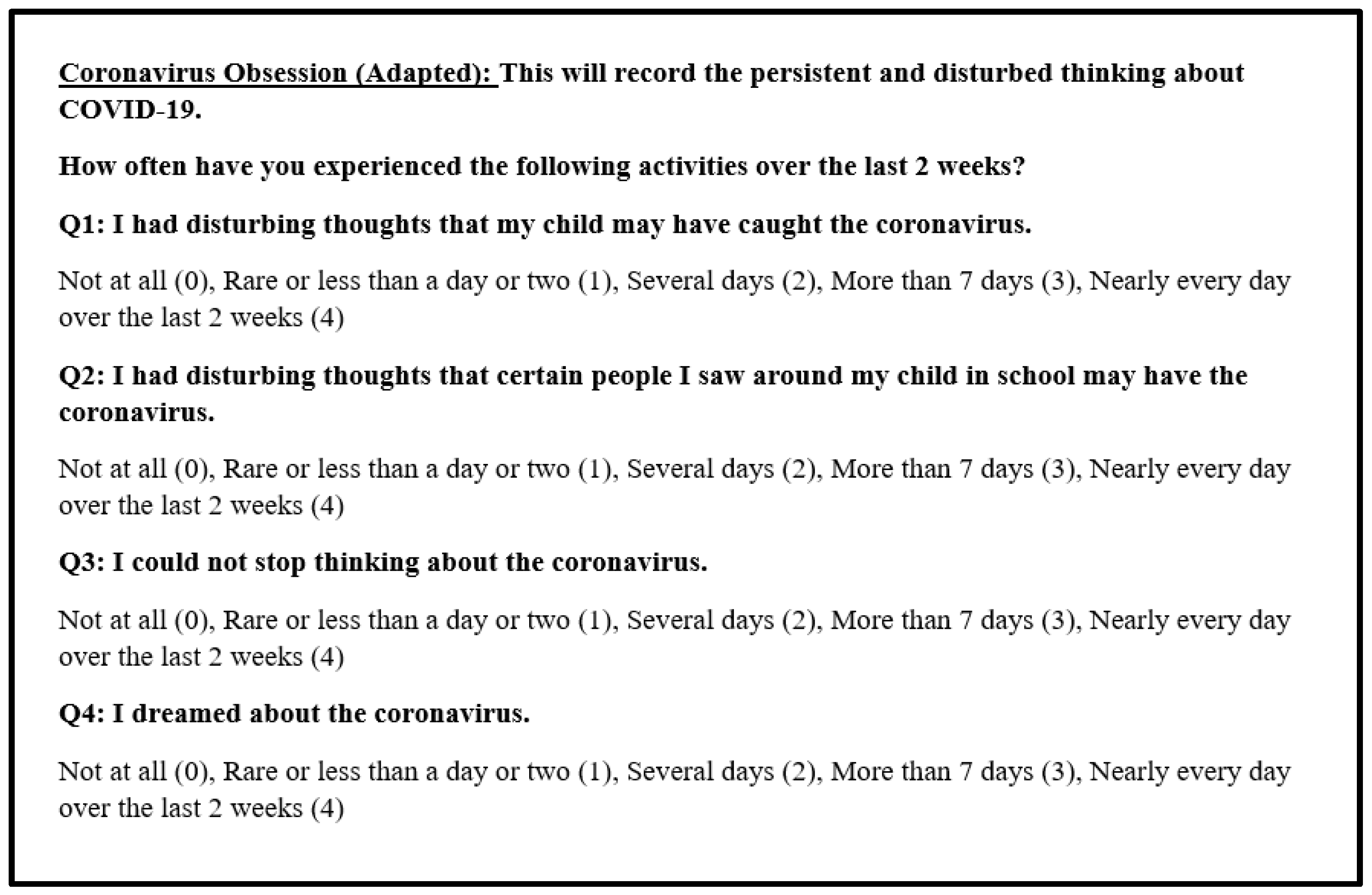
Appendix A.2. Coronavirus Obsession Scale
Appendix B
Appendix B.1
Appendix B.2
References
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. COVID-19 Disrupting Mental Health Services in Most Countries, WHO Survey. 2020. Available online: https://www.who.int/news/item/05-10-2020-covid-19-disrupting-mental-health-services-in-most-countries-who-survey (accessed on 3 February 2022).
- World Health Organization. (n.d.). Mental Health. Available online: https://www.who.int/health-topics/mental-health#tab=tab_1 (accessed on 3 February 2022).
- UNICEF. Impact of COVID-19 on Poor Mental Health in Children and Young People ‘Tip of the Iceberg’. [Press Release]. 4 October 2021. Available online: https://www.unicef.org/press-releases/impact-covid-19-poor-mental-health-children-and-young-people-tip-iceberg#:~:text=According%20to%20early%20findings%20from,little%20interest%20in%20doing%20things (accessed on 3 February 2022).
- Fitzpatrick, K.M.; Harris, C.; Drawve, G. Fear of COVID-19 and the mental health consequences in America. Psychol. Trauma 2020, 12, S17–S21. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Zhang, E.; Wong, G.T.F.; Hyun, S.; Hahm, H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020, 290, 113172. [Google Scholar] [CrossRef] [PubMed]
- Kamal, R.; Panchal, N.; Cox, C.; Garfield, R. The Implications of COVID-19 for Mental Health and Substance Use. KFF. 20 July 2021. Available online: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/ (accessed on 2 February 2022).
- Czeisler, M.É.; Wiley, J.F.; Facer-Childs, E.R.; Robbins, R.; Weaver, M.D.; Barger, L.K.; Czeisler, C.A.; Howard, M.E.; Rajaratnam, S.M.W. Mental health, substance use, and suicidal ideation during a prolonged COVID-19-related lockdown in a region with low SARS-CoV-2 prevalence. J. Psychiatr. Res. 2021, 140, 533–544. [Google Scholar] [CrossRef]
- Twenge, J.M.; Joiner, T.E. Mental distress among U.S. adults during the COVID-19 pandemic. J. Clin. Psychol. 2020, 76, 2170–2182. [Google Scholar] [CrossRef]
- American Psychological Association. Mothers-and Fathers-report Mental, Physical Health Declines. American Psychological Association. 11 March 2021. Available online: https://www.apa.org/news/press/releases/stress/2021/one-year-pandemic-stress-parents (accessed on 13 April 2022).
- Kerr, M.L.; Rasmussen, H.F.; Fanning, K.A.; Braaten, S.M. Parenting During COVID-19: A Study of Parents’ Experiences Across Gender and Income Levels. Fam. Relat. 2021, 70, 1327–1342. [Google Scholar] [CrossRef]
- Valero-Moreno, S.; Lacomba-Trejo, L.; Tamarit, A.; Pérez-Marín, M.; Montoya-Castilla, I. Psycho-emotional adjustment in parents of adolescents: A cross-sectional and longitudinal analysis of the impact of the COVID pandemic. J. Pediatr. Nurs. 2021, 59, e44–e51. [Google Scholar] [CrossRef]
- University of Oregon RAPID-EC Project. How Long Can the Levee Hold? 10 September 2020. Available online: https://medium.com/rapid-ec-project/how-long-can-the-levee-hold-2a2cd0779914 (accessed on 7 February 2022).
- He, Y.; Ortiz, R.; Kishton, R.; Wood, J.; Fingerman, M.; Jacobs, L.; Sinko, L. In their own words: Child and adolescent perceptions of caregiver stress during early COVID-19. Child Abuse Negl. 2022, 124, 105452. [Google Scholar] [CrossRef]
- Chawla, N.; Tom, A.; Sen, M.S.; Sagar, R. Psychological impact of COVID-19 on children and adolescents: A systematic review. Indian J. Psychol. Med. 2021, 43, 294–299. [Google Scholar] [CrossRef]
- Schwartz, K.D.; Exner-Cortens, D.; McMorris, C.A.; Makarenko, E.; Arnold, P.; Van Bavel, M.; Williams, S.; Canfield, R. COVID-19 and student well-being: Stress and mental health during return-to-school. Can. J. Sch. Psychol. 2021, 36, 166–185. [Google Scholar] [CrossRef]
- Gazmararian, J.; Weingart, R.; Campbell, K.; Cronin, T.; Ashta, J. Impact of COVID-19 Pandemic on the Mental Health of Students From 2 Semi-Rural High Schools in Georgia. J. Sch. Health 2021, 91, 356–369. [Google Scholar] [CrossRef] [PubMed]
- Murray, L.; Creswell, C.; Cooper, P.J. The development of anxiety disorders in childhood: An integrative review. Psychol. Med. 2009, 39, 1413–1423. [Google Scholar] [CrossRef] [PubMed]
- Qualtrics Panels Project. Available online: https://www.qualtrics.com/panels-project/ (accessed on 31 December 2021).
- Lee, S.A. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Stud. 2020, 44, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.A. How much “Thinking” about COVID-19 is clinically dysfunctional? Brain Behav. Immun. 2020, 87, 97–98. [Google Scholar] [CrossRef]
- Chorpita, B.F.; Yim, L.; Moffitt, C.; Umemoto, L.A.; Francis, S.E. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behav. Res. Ther. 2000, 38, 835–855. [Google Scholar] [CrossRef]
- Ebesutani, C.; Bernstein, A.; Nakamura, B.J.; Chorpita, B.F.; Weisz, J.R.; Research Network on Youth Mental Health. A psychometric analysis of the revised child anxiety and depression scale—Parent version in a clinical sample. J. Abnorm. Child Psychol. 2010, 38, 249–260. [Google Scholar] [CrossRef] [Green Version]
- Chen, J.H.; Tong, K.K.; Su, X.; Yu, E.W.; Wu, A.M.S. Measuring COVID-19 related anxiety and obsession: Validation of the Coronavirus Anxiety Scale and the Obsession with COVID-19 Scale in a probability Chinese sample. J. Affect. Disord. 2021, 295, 1131–1137. [Google Scholar] [CrossRef]
- Daniel, W.W. Biostatistics: A Foundation for Analysis in the Health Sciences, 7th ed.; John Wiley & Sons: New York, NY, USA, 1999. [Google Scholar]
- Patrick, S.W.; Henkhaus, L.E.; Zickafoose, J.S.; Lovell, K.; Halvorson, A.; Loch, S.; Letterie, M.; Davis, M.M. Well-being of Parents and Children During the COVID-19 Pandemic: A National Survey. Pediatrics 2020, 146, e2020016824. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Department of Psychology, New York University: New York, NY, USA, 1988; Available online: http://utstat.toronto.edu/~brunner/oldclass/378f16/readings/CohenPower.pdf (accessed on 18 January 2022).
- Mansournia, M.A.; Collins, G.S.; Nielsen, R.O.; Nazemipour, M.; Jewell, N.P.; Altman, D.G.; Campbell, M.J. Checklist for statistical Assessment of Medical Papers: The CHAMP statement. Br. J. Sports Med. 2021, 55, 1002–1003. [Google Scholar] [CrossRef]
- Gilbert, L.K.; Strine, T.W.; Szucs, L.E.; Crawford, T.N.; Parks, S.E.; Barradas, D.T.; Njai, R.; Ko, J.Y. Racial and Ethnic Differences in Parental Attitudes and Concerns About School Reopening During the COVID-19 Pandemic—United States, July 2020. MMWR Morb. Mortal. Wkly Rep. 2020, 69, 1848–1852. [Google Scholar] [CrossRef]
- The Centers for Disease Control and Prevention. Risk for COVID-19 Infection, Hospitalization, and Death by Race/Ethnicity. 1 February 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/investigations-discovery/hospitalization-death-by-race-ethnicity.html (accessed on 19 February 2022).
- Domenech Rodríguez, M.M.; Donovick, M.R.; Crowley, S.L. Parenting styles in a cultural context: Observations of “protective parenting” in first-generation Latinos. Fam. Process 2009, 48, 195–210. [Google Scholar] [CrossRef] [PubMed]
- Ayón, C.; Williams, L.R.; Marsiglia, F.F.; Ayers, S.; Kiehne, E. A Latent Profile Analysis of Latino Parenting: The Infusion of Cultural Values on Family Conflict. Fam. Soc. 2015, 96, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Sotomayor-Peterson, M.; Figueredo, A.J.; Christensen, D.H.; Taylor, A.R. Couples’ cultural values, shared parenting, and family emotional climate within Mexican American families. Fam. Process 2012, 51, 218–233. [Google Scholar] [CrossRef] [PubMed]
- The New York Times. (n.d.). COVID-19 Updates. Available online: https://www.nytimes.com/interactive/2021/us/covid-cases.html (accessed on 19 February 2022).
- CNN Politics. The Northeast Leads the Country in Mask Wearing. 2020. Available online: https://www.cnn.com/2020/06/26/politics/maskwearing-coronavirus-analysis/index.html (accessed on 12 February 2022).
- Coronavirus Resource Center. Understanding Vaccination Process. Available online: https://coronavirus.jhu.edu/vaccines/us-states/ (accessed on 19 February 2022).
- Henderson, M.B.; Peterson, P.E.; West, M.R. Pandemic parent survey finds perverse pattern: Students are more likely to be attending school in person where Covid is spreading more rapidly. Educ. Next 2021, 21, 34–48. Available online: https://link.gale.com/apps/doc/A658584616/AONE?u=unlv_main&sid=googleScholar&xid=a895985 (accessed on 18 January 2022).
- U.S. News. Private School vs. Public School. 2021. Available online: https://www.usnews.com/education/k12/articles/private-school-vs-public-school (accessed on 19 February 2022).
- Burstein, M.; Ginsburg, G.S.; Tein, J.Y. Parental anxiety and child symptomatology: An examination of additive and interactive effects of parent psychopathology. J. Abnorm. Child Psychol. 2010, 38, 897–909, Erratum in J. Abnorm. Child Psychol. 2010, 38, 895. [Google Scholar] [CrossRef] [Green Version]
- Ehrler, M.; Werninger, I.; Schnider, B.; Eichelberger, D.A.; Naef, N.; Disselhoff, V.; Kretschmar, O.; Hagmann, C.F.; Latal, B.; Wehrle, F.M. Impact of the COVID-19 pandemic on children with and without risk for neurodevelopmental impairments. Acta Paediatr. 2021, 110, 1281–1288. [Google Scholar] [CrossRef]
- Woodruff-Borden, J.; Morrow, C.; Bourland, S.; Cambron, S. The behavior of anxious parents: Examining mechanisms of transmission of anxiety from parent to child. J. Clin. Child Adolesc. Psychol. 2002, 31, 364–374. [Google Scholar] [CrossRef]
- Borelli, J.L.; Rasmussen, H.F.; John, H.; West, J.L.; Piacentini, J.C. Parental reactivity and the link between parent and child anxiety symptoms. J. Child Fam. Stud. 2015, 24, 3130–3144. [Google Scholar] [CrossRef]
| Variable | Categories | n (%) | 95% CI (LCL, UCL) |
|---|---|---|---|
| Age (Mean ± SD) | - | 49.9 ± 11.2 | 49.4, 50.4 |
| Gender | Female | 1065 (50.7) | 48.5, 52.9 |
| Male | 999 (47.6) | 45.4, 49.7 | |
| Other, including non-binary, Transgender | 29 (1.4) | 0.93, 2.0 | |
| Race/ethnicity | Non-Hispanic White | 1197 (57.0) | 54.9, 59.1 |
| Non-Hispanic Black | 273 (13.0) | 11.6, 14.5 | |
| Hispanic | 378 (18.0) | 16.4, 19.7 | |
| Asian or Pacific Islanders | 126 (6.0) | 5.0, 7.1 | |
| Other | 126 (6.0) | 5.0, 7.1 | |
| Education | Some high school | 54 (2.6) | 1.9, 3.3 |
| High school diploma or GED | 417 (19.9) | 18.2, 21.6 | |
| Some College | 560 (26.7) | 24.8, 28.6 | |
| 4-year college degree | 656 (31.2) | 29.3, 33.3 | |
| Graduate level degree | 383 (18.2) | 16.6, 19.9 | |
| Other | 30 (1.4) | 1.0, 2.0 | |
| Marital status | Married | 1294 (61.6) | 59.5, 63.7 |
| Single, never married | 364 (17.3) | 15.7, 19.0 | |
| Divorced or Separated | 192 (9.1) | 7.9, 10.5 | |
| Widowed | 42 (2.0) | 1.4, 2.7 | |
| A member of an unmarried couple | 208 (9.9) | 8.6, 11.3 | |
| Employment status | Full-time paid job | 1390 (66.2) | 64.1, 68.2 |
| Part-time paid job | 175 (8.3) | 7.2, 9.6 | |
| Self-employed | 146 (7.0) | 5.9, 8.1 | |
| Unable to work | 103 (4.9) | 4.0, 5.9 | |
| Unemployed and looking for work | 104 (5.0) | 4.1, 5.9 | |
| Unemployed but not looking for work (e.g., retired, homemaker, student, etc.) | 182 (8.7) | 7.5, 10.0 | |
| Annual Gross Income | 0 to $10,000 | 153 (7.3) | 6.2, 8.5 |
| $10,001 to $25,000 | 202 (9.6) | 8.4, 11.0 | |
| $25,001 to $50,000 | 473 (22.5) | 20.8, 24.4 | |
| $50,001 to $100,000 | 606 (28.9) | 26.9, 30.9 | |
| $100,001 to $250,000 | 528 (25.1) | 23.3, 27.1 | |
| >$250,001 | 111 (5.3) | 4.4, 6.3 | |
| Region | Midwest | 448 (21.3) | 19.6, 23.2 |
| Northeast | 358 (17.0) | 15.5, 18.7 | |
| South | 819 (39.0) | 36.9, 41.1 | |
| West | 475 (22.6) | 20.8, 24.5 |
| Variable | Categories | n (%) | 95% CI (LCL, UCL) |
|---|---|---|---|
| Age of the youngest child (Mean ± SD) | - | 9.10 ± 4.11 | 8.93, 9.27 |
| Gender of the youngest child | Female | 983 (46.8) | 44.7, 49.0 |
| Male | 1077 (51.3) | 49.1, 53.4 | |
| Other, including non-binary, transgender | 26 (1.2) | 0.8, 1.8 | |
| School type of the youngest child | Private | 349 (16.6) | 15.1, 18.3 |
| Public | 1751 (83.4) | 81.7, 85.0 | |
| School level of the youngest child | Kindergarten | 536 (25.5) | 23.7, 27.5 |
| Elementary | 852 (40.6) | 38.5, 42.7 | |
| Middle school | 357 (17.0) | 15.4, 18.7 | |
| High school | 355 (16.9) | 15.3, 18.6 | |
| Vulnerability of the youngest child to infections | Yes | 741 (35.3) | 33.2, 37.4 |
| No | 1094 (52.1) | 50.0, 54.3 | |
| Not sure | 265 (12.6) | 11.2, 14.1 | |
| Living with vulnerable family member | Yes | 755 (36.0) | 33.9, 38.1 |
| No | 1345 (64.0) | 62.0, 66.1 | |
| Friends/family tested positive for COVID-19 | Yes | 955 (45.5) | 43.3, 47.6 |
| No | 1129 (53.8) | 51.6, 55.9 | |
| COVID-19 information source | Local health department | 1194 (56.9) | 54.7, 58.9 |
| School administration | 367 (17.5) | 15.9, 19.2 | |
| Parent association | 205 (9.8) | 8.5, 11.1 | |
| Superintendent or official district communications | 166 (7.9) | 6.8, 9.1 |
| Variable | Groups | Coronavirus Anxiety | Coronavirus Obsession | Separation Anxiety | Social Phobia | Generalized Anxiety | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M ± SD p Value | M ± SD p Value | M ± SD p Value | M ± SD p Value | M ± SD p Value | |||||||
| Gender of the parent | Male | 4.64 ± 5.42 | 0.8 | 4.60 ± 4.66 | 0.3 | 6.21 ± 5.61 | 0.2 | 8.93 ± 6.68 | 0.6 | 5.22 ± 4.73 | 0.8 |
| Female | 4.60 ± 4.93 | 4.39 ± 4.23 | 5.93 ± 4.98 | 9.07 ± 6.55 | 5.19 ± 4.43 | ||||||
| Race/ethnicity of the parent | White | 4.60 ± 5.24 | <0.001 | 4.37 ± 4.48 | <0.001 | 6.12 ± 5.36 | <0.001 | 9.18 ± 6.46 | <0.001 | 5.33 ± 4.54 | <0.001 |
| Black | 4.20 ± 4.96 | 4.38 ± 4.39 | 5.62 ± 5.26 | 8.34 ± 7.03 | 4.45 ± 4.31 | ||||||
| Hispanic | 6.00 ± 5.32 | 5.51 ± 4.51 | 7.07 ± 5.31 | 10.09 ± 6.89 | 6.27 ± 4.87 | ||||||
| Other | 3.30 ± 4.37 | 3.89 ± 4.01 | 4.91 ± 4.68 | 7.46 ± 6.07 | 4.06 ± 4.26 | ||||||
| Region | Northeast | 5.05 ± 5.30 | 0.05 * | 4.93 ± 4.43 | 0.02 | 6.37 ± 5.62 | 0.08 | 9.37 ± 7.08 | 0.3 | 5.53 ± 4.94 | 0.09 |
| South | 4.74 ± 5.15 | 4.67 ± 4.52 | 6.12 ± 5.16 | 8.89 ± 6.48 | 5.13 ± 4.48 | ||||||
| West | 4.66 ± 5.29 | 4.44 ± 4.48 | 6.31 ± 5.50 | 9.33 ± 6.90 | 5.53 ± 4.84 | ||||||
| Midwest | 4.07 ± 4.94 | 3.99 ± 4.24 | 5.54 ± 4.99 | 8.66 ± 6.11 | 4.88 ± 4.16 | ||||||
| School type | Public | 4.40 ± 5.06 | <0.001 | 4.38 ± 4.39 | 0.002 | 5.85 ± 5.19 | <0.001 | 8.84 ± 6.50 | 0.005 | 5.10 ± 4.46 | 0.006 |
| Private | 5.81 ± 5.53 | 5.21 ± 4.63 | 7.25 ± 5.64 | 9.98 ± 7.04 | 5.91 ± 5.12 | ||||||
| School level | Kindergarten | 5.05 ± 5.25 | 0.2 | 4.75 ± 4.45 | 0.4 | 7.05 ± 5.19 | <0.001 | 8.48 ± 6.66 | 0.09 | 4.90 ± 4.59 | 0.2 |
| Elementary | 4.53 ± 5.00 | 4.47 ± 4.27 | 6.17 ± 5.00 | 9.14 ± 6.25 | 5.28 ± 4.33 | ||||||
| Middle school | 4.63 ± 5.30 | 4.55 ± 4.61 | 5.81 ± 5.78 | 9.59 ± 6.97 | 5.56 ± 4.89 | ||||||
| High school | 4.25 ± 5.28 | 4.24 ± 4.57 | 4.67 ± 5.29 | 9.00 ± 6.95 | 5.30 ± 4.83 | ||||||
| Gender of the youngest child | Male | 4.77 ± 5.20 | <0.001 | 4.58 ± 4.50 | 0.03 | 6.27 ± 5.44 | 0.04 | 9.20 ± 6.65 | 0.003 | 5.45 ± 4.64 | <0.001 |
| Female | 4.37 ± 5.07 | 4.38 ± 4.33 | 5.82 ± 5.11 | 8.74 ± 6.55 | 4.91 ± 4.47 | ||||||
| Other | 8.35 ± 6.01 | 6.62 ± 4.64 | 7.73 ± 5.30 | 12.96 ± 5.62 | 9.23 ± 4.65 | ||||||
| Variables | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Coronavirus anxiety of parents | 1 | 0.83 ** | 0.71 ** | 0.62 ** | 0.66 ** | −0.14 ** |
| 2. Coronavirus obsession of parents | 0.83 ** | 1 | 0.70 ** | 0.62 ** | 0.64 ** | −0.13 ** |
| 3. Separation anxiety of child | 0.71 ** | 0.70 | 1 | 0.75 ** | 0.76 ** | −0.19 ** |
| 4. Social phobia of child | 0.62 ** | 0.62 ** | 0.75 ** | 1 | 0.82 ** | −0.12 ** |
| 5. Generalized anxiety of child | 0.66 ** | 0.64 ** | 0.76 ** | 0.82 ** | 1 | −0.11 ** |
| 6. Parental age | −0.14 ** | −0.14 ** | −0.19 ** | −0.12 ** | −0.11 ** | 1 |
| Cronbach’s Alpha | 0.915 | 0.895 | 0.901 | 0.925 | 0.918 | - |
| Variables | B | 95% CI for B | SE B | β | R2 | ΔR2 | |
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Model | - | 0.553 | 0.550 ** | ||||
| Constant | −0.020 | −0.826 | 0.785 | 0.411 | - | ||
| Parental gender (ref: female) | −0.157 | −0.494 | 0.179 | 0.172 | −0.015 | ||
| Parental age | −0.007 | −0.023 | 0.010 | 0.009 | −0.012 | ||
| Race/ethnicity of the parent, white (ref: black) | 0.016 | −0.454 | 0.486 | 0.240 | 0.002 | ||
| Race/ethnicity of the parent, Hispanic (ref: black) | 0.540 | −0.016 | 1.096 | 0.283 | 0.040 | ||
| Race/ethnicity of the parent, other (ref: black) | −0.379 | −0.985 | 0.226 | 0.309 | −0.024 | ||
| Child gender, male (ref: female) | 0.070 | −0.257 | 0.397 | 0.167 | 0.007 | ||
| Child gender, other (ref: female) | 1.870 | −0.044 | 3.784 | 0.976 | 0.029 | ||
| Child’s vulnerability to infections (ref: No) | 0.768 | 0.433 | 0.999 | 0.171 | 0.071 ** | ||
| School type (ref: public) | 0.460 | 0.051 | 0.869 | 0.209 | 0.028 * | ||
| School level, elementary (ref: kindergarten) | −0.128 | −0.517 | 0.260 | 0.198 | −0.012 | ||
| School level, middle (ref: kindergarten) | 0.052 | −0.436 | 0.541 | 0.249 | 0.004 | ||
| School level, high (ref: kindergarten) | 0.312 | −0.194 | 0.819 | 0.258 | 0.023 | ||
| Social phobia of child | 0.042 * | 0.002 | −0.084 | 0.022 | 0.053 | ||
| Generalized anxiety of child | 0.25 ** | 0.19 | 0.32 | 0.032 | 0.22 ** | ||
| Separation anxiety of the child | 0.467 ** | 0.417 | 0.52 | 0.025 | 0.48 ** | ||
| Variables | B | 95% CI for B | SE B | β | R2 | Δ R2 | |
|---|---|---|---|---|---|---|---|
| LL | UL | ||||||
| Model | - | 0.525 | 0.522 ** | ||||
| Constant | 0.731 | 0.018 | 1.444 | 0.364 | |||
| Parental gender (ref: female) | 0.166 | −0.132 | 0.464 | 0.152 | 0.019 | ||
| Parental age | −0.008 | −0.023 | 0.007 | 0.008 | −0.018 | ||
| Race/ethnicity of the parent, white (ref: black) | −0.325 | −0.741 | 0.091 | 0.212 | −0.036 | ||
| Race/ethnicity of the parent, Hispanic (ref: black) | 0.139 | −0.353 | 0.631 | 0.251 | 0.012 | ||
| Race/ethnicity of the parent, other (ref: black) | 0.013 | −0.523 | 0.549 | 0.273 | 0.001 | ||
| Child gender, male (ref: female) | −0.174 | −0.464 | 0.116 | 0.148 | −0.020 | ||
| Child gender, other (ref: female) | −0.145 | −1.839 | 1.550 | 0.864 | −0.003 | ||
| Child’s vulnerability to infections (Ref: No) | 0.653 ** | 0.357 | 0.950 | 0.151 | 0.070 ** | ||
| School type (ref: public) | 0.053 | −0.310 | 0.415 | 0.185 | 0.004 | ||
| School level, elementary (ref: kindergarten) | 0.009 | −0.335 | 0.353 | 0.175 | 0.001 | ||
| School level, middle (ref: kindergarten) | 0.126 | −0.306 | 0.559 | 0.221 | 0.011 | ||
| School level, high (ref: kindergarten) | 0.357 | −0.092 | 0.805 | 0.229 | 0.030 | ||
| Social phobia of child | 0.086 ** | 0.048 | 0.123 | 0.019 | 0.128 ** | ||
| Generalized anxiety of child | 0.176 ** | 0.120 | 0.232 | 0.029 | 0.181 ** | ||
| Separation anxiety of the child | 0.369 ** | 0.326 | 0.413 | 0.022 | 0.440 ** | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Batra, K.; Pharr, J.R.; Terry, E.; Labus, B. Assessing Psychological Impact of COVID-19 among Parents of Children Returning to K-12 Schools: A U.S. Based Cross-Sectional Survey. Healthcare 2022, 10, 775. https://doi.org/10.3390/healthcare10050775
Batra K, Pharr JR, Terry E, Labus B. Assessing Psychological Impact of COVID-19 among Parents of Children Returning to K-12 Schools: A U.S. Based Cross-Sectional Survey. Healthcare. 2022; 10(5):775. https://doi.org/10.3390/healthcare10050775
Chicago/Turabian StyleBatra, Kavita, Jennifer R. Pharr, Emylia Terry, and Brian Labus. 2022. "Assessing Psychological Impact of COVID-19 among Parents of Children Returning to K-12 Schools: A U.S. Based Cross-Sectional Survey" Healthcare 10, no. 5: 775. https://doi.org/10.3390/healthcare10050775
APA StyleBatra, K., Pharr, J. R., Terry, E., & Labus, B. (2022). Assessing Psychological Impact of COVID-19 among Parents of Children Returning to K-12 Schools: A U.S. Based Cross-Sectional Survey. Healthcare, 10(5), 775. https://doi.org/10.3390/healthcare10050775








