Oral Cavity Status of Type 1 Diabetic Patients Who Underwent an Oral Hygiene Tuition
Abstract
1. Introduction
2. Materials and Methods
2.1. Subject
2.1.1. Treatment Group
Inclusion Criteria
Exclusion Criteria
Control Group
Inclusion Criteria
Exclusion Criteria
2.2. Methods
- First dental appointment during which medical interview and the questionnaire examination were done as well as the analysis of the oral cavity status of the participants. At the end of the first appointment patients from both groups were given oral hygiene instructions. The proper technique of teeth brushing was presented and each patient trained the procedure with the dentist. Patients were given all the instructions in the written form (information regarding the proper technique of teeth brushing and additional products used in oral hygiene procedures as: dental floss, interdental brushes and mouthwashes was included).
- Second dental appointment-calculation of oral hygiene indices was carried out. It took place 6 months after the first appointment.
Questionnaire Examination
- How often do you visit a dentist? (every month/every three months/every six months/once a year/occasionally)
- What are the reasons for your dental appointments? (toothache/problems with gingiva/check-up/other-what?)
- Were you given any instructions regarding oral hygiene by a dentist or dental hygienist? (yes/no)
- Did you have scaling, sandblasting and fluoridation done? If yes, when?
- Do you observe bleeding while teeth brushing? (yes/no)
- How often do you brush your teeth? (once a day/twice a day/three times a day/four times a day and more)
- What kind of toothbrush do you use? (manual- soft/medium/hard; electric)
- Do you use any additional products to maintain the proper oral hygiene? (mouthwash/interdental toothbrush/irrigator/dental floss/tongue brush’ other- what kind?)
- Do you eat or drink (liquids other than water?) after evening teeth brushing?
- How many meals do you eat during the day (including snacks)? (1/2/3/4/5/6/7/8)
- DMFT (Decayed-Missing-Filled Teeth Index)
- D-a tooth with one or more cavities (primary or secondary)
- M-a tooth lost due to caries
- F-a tooth with one or more fillings but with no secondary caries, a tooth with a prosthetic crown (that was applied because of caries)
- Dental Treatment Index
- Frequency of caries
- API (Approximal Plaque Index) by Lange [12]
- 100–70%—poor oral hygiene,
- 69–40%—insufficient oral hygiene,
- 39–25%—pretty good oral hygiene,
- <25%—optimum hygiene.
- OHI-S (Oral Hygiene Index-Simplified) by Green and Vermillion [12]
- 0-
- No debris or calculus,
- 1-
- Soft debris or supragingival calculus, covering not more than one third of the exposed surface,
- 2-
- Soft debris or supragingival calculus, covering not more than two thirds of the exposed tooth surface, or presence of flecks of subgingival calculus around the cervical portion of the tooth, or both,
- 3-
- Soft debris or supragingival calculus covering more than two thirds of the exposed tooth surface, or a continuous heavy band of subgingival calculus around the cervical portion of the tooth, or both.
- 0-
- No bleeding on probing
- 1-
- Isolated bleeding spots
- 2-
- Blood formed a red line along the gingival margin
- 3-
- Heavy bleeding [11].
2.3. Statistical Analysis
3. Results
3.1. Patients Characteristics and Their Hygiene Habits
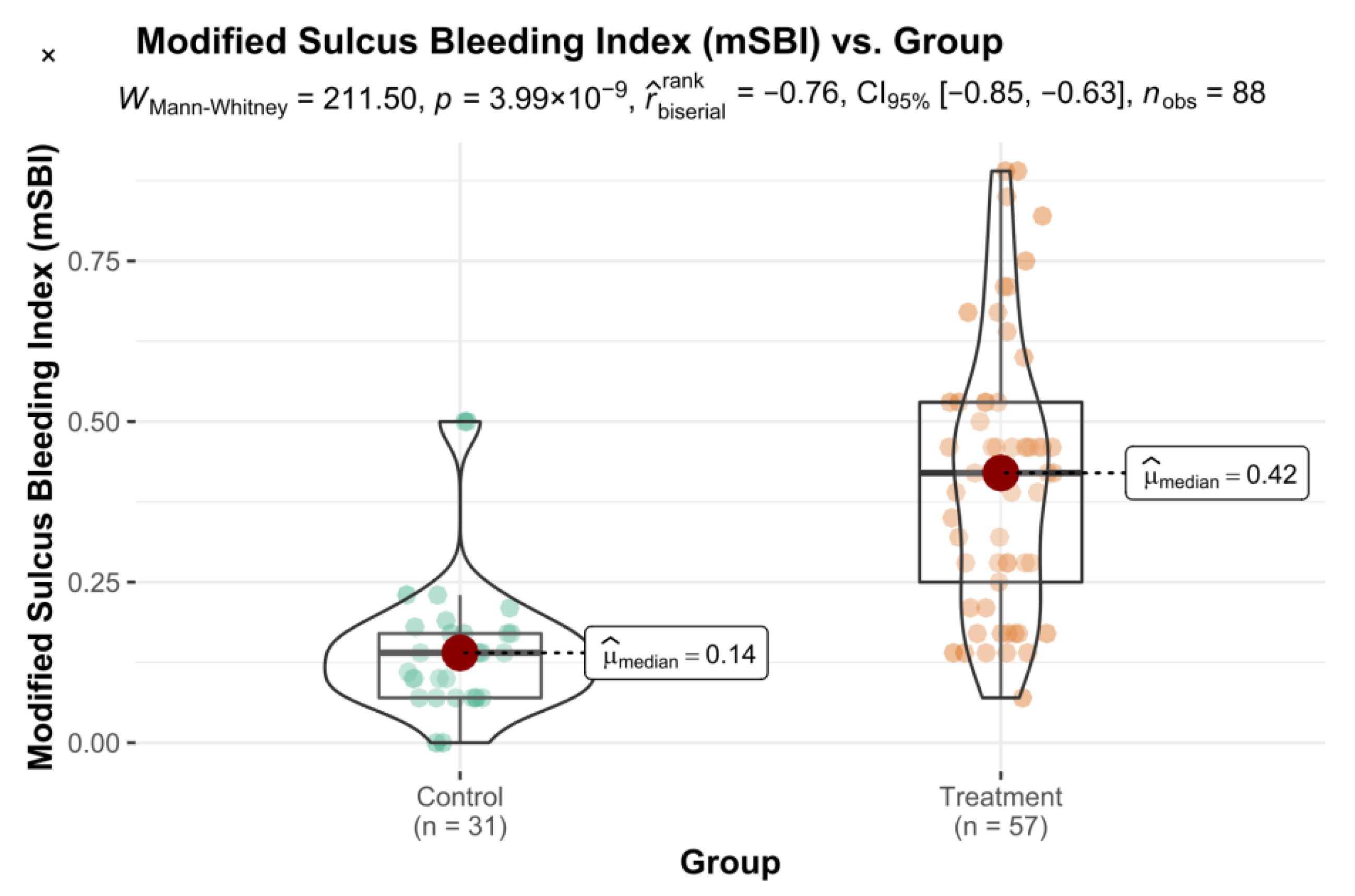
3.2. Control Group (Visit 1) vs. Treatment Group (Visit 1)
3.3. Control Group (Visit 2) vs. Treatment Group (Visit 2)
3.4. Control Group (Visit 1) vs. Control Group (Visit 2)
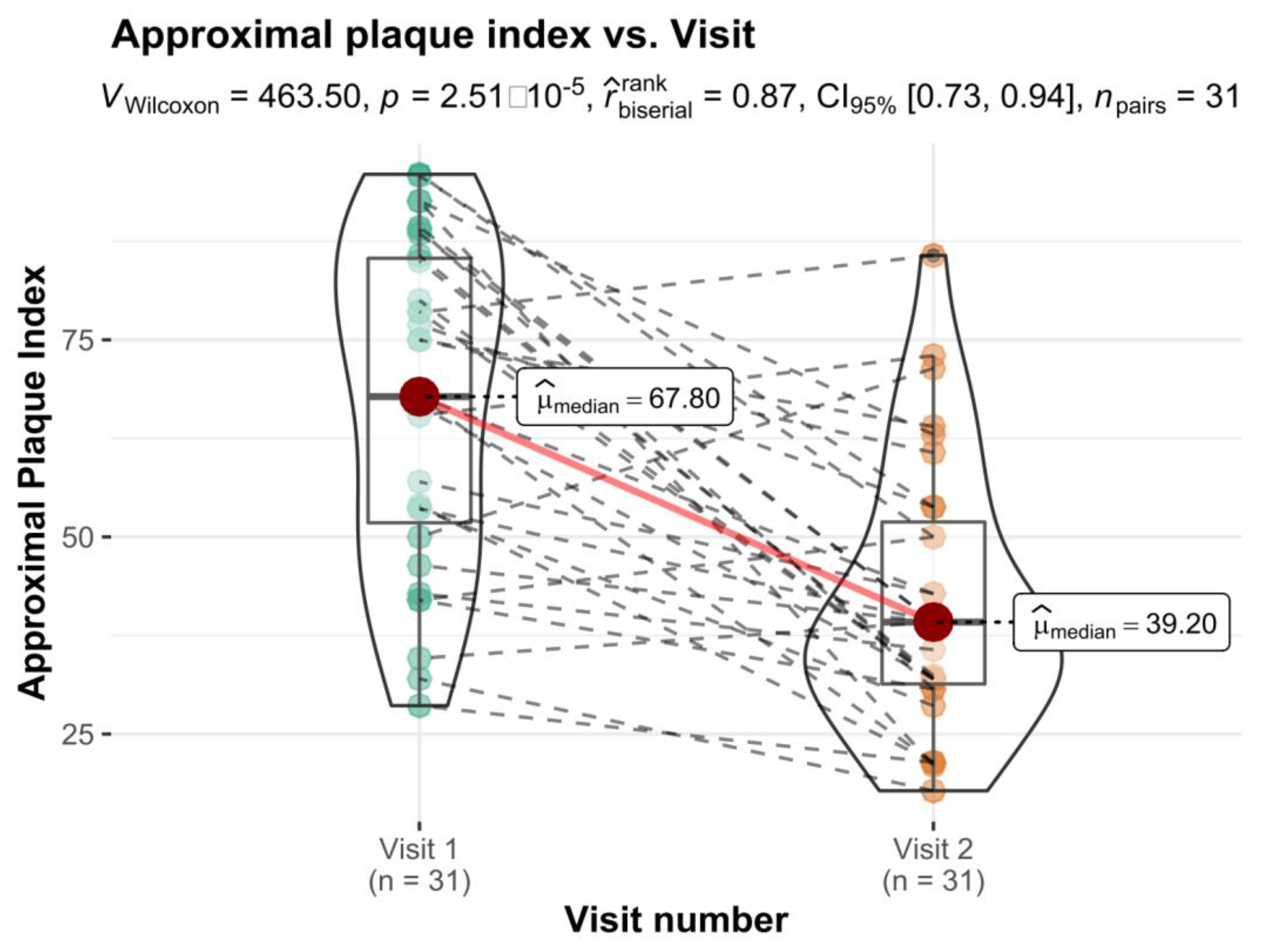
3.5. Treatment Group (Visit 1) vs. Treatment Group (Visit 2)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Poudel, P.; Griffiths, R.; Arora, A.; Wong, V.W.; Flack, J.F.; Barker, J.; George, A. Oral Health Status, Knowledge, and Behaviours of People with Diabetes in Sydney, Australia. Int. J. Environ. Res. Public Health 2021, 18, 3464. [Google Scholar] [CrossRef] [PubMed]
- Bissong, M.; Azodo, C.C.; Agbor, M.A.; Nkuo-Akenji, T.; Nde Fon, P. Oral health status of diabetes mellitus patients in Southwest Cameroon. Odonto-Stomatol. Trop. 2015, 38, 49–57. [Google Scholar]
- Coelho, A.S.; Amaro, I.F.; Caramelo, F.; Paula, A.; Marto, C.M.; Ferreira, M.M.; Botelho, M.F.; Carrilho, E.V. Dental caries, diabetes mellitus, metabolic control and diabetes duration: A systematic review and meta-analysis. J. Esthet. Restor. Dent. 2020, 32, 291–309. [Google Scholar] [CrossRef] [PubMed]
- De Lima, A.K.A.; Dos Santos, J.A.; Stefani, C.M.; de Lima, A.D.; Damé-Teixeira, N. Diabetes mellitus and poor glycemic control increase the occurrence of coronal and root caries: A systematic review and meta-analysis. Clin. Oral. Investig. 2020, 24, 3801–3812. [Google Scholar] [CrossRef]
- Latti, B.R.; Kalburge, J.V.; Birajdar, S.B.; Latti, R.G. Evaluation of relationship between dental caries, diabetes mellitus and oral microbiota in diabetics. J. Oral. Maxillofac. Pathol. 2018, 22, 282–290. [Google Scholar] [CrossRef]
- Moore, P.A.; Weyant, R.J.; Mongelluzzo, M.B.; Myers, D.E.; Rossie, K.; Guggenheimer, J.; Block, H.M.; Huber, H.; Orchard, T. Type 1 diabetes mellitus and oral health: Assessment of periodontal disease. J. Periodontol. 1999, 70, 409–417. [Google Scholar] [CrossRef]
- Kunert, J.; Bołtacz-Rzepkowska, E. Próchnica zębów u chorych na cukrzycę. Dent. Med. Probl. 2007, 4, 495–500. [Google Scholar]
- Gandara, B.; Morton, T. Objawy cukrzycy w jamie ustnej występujące poza przyzębiem: Podstawowe informacje dla personelu medycznego. Diabetol. Dypl. 2012, 9, 18–31. [Google Scholar]
- Carrera-Bastos, P.; Fontes-Vilalba, M.; O’Keefe, J.H.; Cordain, L. The western diet and lifestyle and diseases of civilization. Res. Rep. Clin. Cardiol. 2011, 2, 15–35. [Google Scholar] [CrossRef]
- Çankaya, H.; Güneri, P.; Epstein, J.B.; Boyacioğlu, H. Awareness of oral complications and oral hygiene habits of subjects with diagnosed Diabetes Mellitus. Balk. J. Dent. Educ. 2018, 22, 138–145. [Google Scholar] [CrossRef][Green Version]
- Katarzyńska-Konwa, M.; Obersztyn, I.; Trzcionka, A.; Mocny-Pachońska, K.; Mosler, B.; Tanasiewicz, M. Oral status in pregnant women from post-industrial areas of Upper Silesia in reference of: Preterm labors, low birth weight and type of labor. Healthcare 2020, 8, 528. [Google Scholar] [CrossRef] [PubMed]
- Ramanarayanan, V.; Karuveettil, V.; Sanjeevan, V.; Antony, B.K.; Varghese, N.J.; Pandamadan, H.J.; Janakiram, C. Measuring dental diseases: A critical review of indices in dental practice and research. Amirta. J. Med. 2020, 16, 152–158. [Google Scholar]
- Trzcionka, A.; Twardawa, H.; Mocny-Pachońska, K.; Tanasiewicz, M. Oral cavity status of long-term hemodialized patients vs. their socio-economic status. Med. Pr. 2020, 71, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Machado, D.; Coelho, A.; Paula, A.; Caramelo, F.; Carriliho, F.; Barros, L.; Batista, C.; Melo, M.; Ferreira, M.M.; Carrilho, E. Prevalence of dental caries in patients with type 1 diabetes mellitus treated with multiple insulin injections and that of individuals without diabetes. Acta Med. Port. 2017, 30, 402–408. [Google Scholar] [CrossRef][Green Version]
- Banyai, D.; Vegh, D.; Vegh, A.; Ujpal, M.; Payer, M.; Biczo, Z.; Triebl, Z.; Mukaddam, K.; Herber, V.; Jakse, N.; et al. Oral Health Status of Children Living with Type 1 Diabetes Mellitus. Int. J. Environ. Res. Public Health 2022, 19, 545. [Google Scholar] [CrossRef]
- Vegh, A.; Banyai, D.; Ujpal, M.; Somogyi, K.S.; Biczo, Z.; Kammerhofer, G.; Nemeth, Z.; Hermann, P.; Payer, M.; Vegh, D. Prevalence of Diabetes and Impaired Fasting Glycemia in Patients with Oral Cancer: A Retrospective Study in Hungary. Anticancer Res. 2022, 42, 109–113. [Google Scholar] [CrossRef]
- Kuźmiuk, A.; Marczuk-Kolada, G.; Łuczaj-Cepowicz, E. Znaczenie opieki stomatologicznej w utrzymaniu zdrowia jamy ustnej u dzieci i młodzieży z cukrzycą typu 1. Med. Pr. 2018, 69, 37–44. [Google Scholar] [CrossRef]
- Roy, M.; Gastaldi, G.; Courvoisier, D.S.; Mombelli, A.; Giannopoulou, C. Periodontal care in a cohort of subjects with type 1 diabetes mellitus. Clin. Exp. Dent. Res. 2019, 5, 243–249. [Google Scholar] [CrossRef]
- Kanjirath, P.P.; Kim, S.E.; Inglegart, M.R. Diabetes and oral health: The importance of oral health-related behavior. J. Dent. Hyg. 2011, 85, 264–272. [Google Scholar]
- Moore, P.A.; Orchard, T.; Guggenheimer, J.; Weyant, R.J. Promotion: A survey of disease prevention behaviors. JADA 2000, 131, 1333–1341. [Google Scholar] [CrossRef]
- Al Amassi, B.Y.; Al Dakheel, R.S. Oral hygiene practice of adult diabetic patients and their awareness about oral health problems related to diabetes. JDOH 2017, 9, 8–14. [Google Scholar] [CrossRef]
- Bowyer, V.; Sutcliffe, P.; Ireland, R.; Lindenmeyer, A.; Gadsby, R.; Graveney, M.; Sturt, J.; Dale, J. Oral health awareness in adult patients with diabetes: A questionnaire study. Br. Dent. J. 2011, 211, e12. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xing, L.; Yu, H.; Zhao, L. Prevalance of dental caries in children and adolescents with type 1 diabetes: A systematic review and metha-analysis. BMC Oral. Health 2019, 19, 213. [Google Scholar] [CrossRef] [PubMed]
- Chwalba, A.; Otto-Buczkowska, E. Oral health problems among diabetic patients- part of dental professionals in diagnostic and therapy. J. Oral. Hyg. Health 2014, 2, 167. [Google Scholar] [CrossRef]
- Barylo, O.S.; Kanishyna, T.M.; Shkilniak, L.I. The effects of diabetes mellitus on patients’ oral health. Wiad. Lek. 2018, 72, 1026–1031. [Google Scholar]


| Factor | Test | Visit 1 | Test Statistics | p | ||
|---|---|---|---|---|---|---|
| Control Group (SD) | Treatment Group (SD) | |||||
| Oral Hygiene Index (DI) | np | 1.60 (0.70) | 2.00 (0.70) | 573.00 | 0.006 | −0.35 |
| Oral Hygiene Index (CI) | np | 1.10 (0.65) | 1.50 (0.70) | 594.00 | 0.011 | −0.33 |
| Oral Hygiene Index (CI + DI) | p | 2.88 (0.93) | 3.43 (0.96) | −2.61 | 0.011 | −0.57 * |
| modified Sulcus Bleeding Index | np | 0.17 (0.16) | 0.52 (0.37) | 277.50 | <0.001 | −0.69 |
| Factor | Test | Visit 2 | Test Statistics | p | ||
|---|---|---|---|---|---|---|
| Control Group (SD) | Treatment Group (SD) | |||||
| Oral Hygiene Index (DI) | np | 1.50 (0.85) | 1.00 (0.70) | 1400.00 | <0.001 | 0.58 |
| Oral Hygiene Index (CI) | np | 1.30 (0.80) | 1.80 (0.40) | 534.00 | 0.002 | −0.40 |
| Oral Hygiene Index (CI + DI) | p | 2.83 (0.92) | 2.66 (0.66) | 0.89 | 0.379 | 0.20 * |
| Factor | Test | Treatment Group | Test Statistics | p | ||
|---|---|---|---|---|---|---|
| Visit 1 (SD) | Visit 2 (SD) | |||||
| Approximal Plaque Index | np | 75.00 (27.80) | 68.20 (25.00) | 1200.00 | <0.001 | 0.82 |
| Oral Hygiene Index (DI) | np | 2.00 (0.70) | 1.00 (0.7) | 1600.00 | <0.001 | 1.00 |
| Oral Hygiene Index (CI) | np | 1.50 (0.70) | 1.80 (0.40) | 445.50 | 0.017 | −0.38 |
| Oral Hygiene Index (CI + DI) | p | 3.43 (0.95) | 2.66 (0.66) | 8.58 | <0.001 | 1.12 |
| Modified Sulcus Bleeding Index | np | 0.52 (0.37) | 0.42 (0.28) | 120.00 | <0.001 | 0.51 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mosler, B.; Twardawa, H.; Trzcionka, A.; Korkosz, R.; Rahnama, M.; Tanasiewicz, M. Oral Cavity Status of Type 1 Diabetic Patients Who Underwent an Oral Hygiene Tuition. Healthcare 2022, 10, 606. https://doi.org/10.3390/healthcare10040606
Mosler B, Twardawa H, Trzcionka A, Korkosz R, Rahnama M, Tanasiewicz M. Oral Cavity Status of Type 1 Diabetic Patients Who Underwent an Oral Hygiene Tuition. Healthcare. 2022; 10(4):606. https://doi.org/10.3390/healthcare10040606
Chicago/Turabian StyleMosler, Bartosz, Henryk Twardawa, Agata Trzcionka, Rafał Korkosz, Mansur Rahnama, and Marta Tanasiewicz. 2022. "Oral Cavity Status of Type 1 Diabetic Patients Who Underwent an Oral Hygiene Tuition" Healthcare 10, no. 4: 606. https://doi.org/10.3390/healthcare10040606
APA StyleMosler, B., Twardawa, H., Trzcionka, A., Korkosz, R., Rahnama, M., & Tanasiewicz, M. (2022). Oral Cavity Status of Type 1 Diabetic Patients Who Underwent an Oral Hygiene Tuition. Healthcare, 10(4), 606. https://doi.org/10.3390/healthcare10040606






