Examining Psychosocial Factors and Community Mitigation Practices to Limit the Spread of COVID-19: Evidence from Nigeria
Abstract
:1. Introduction
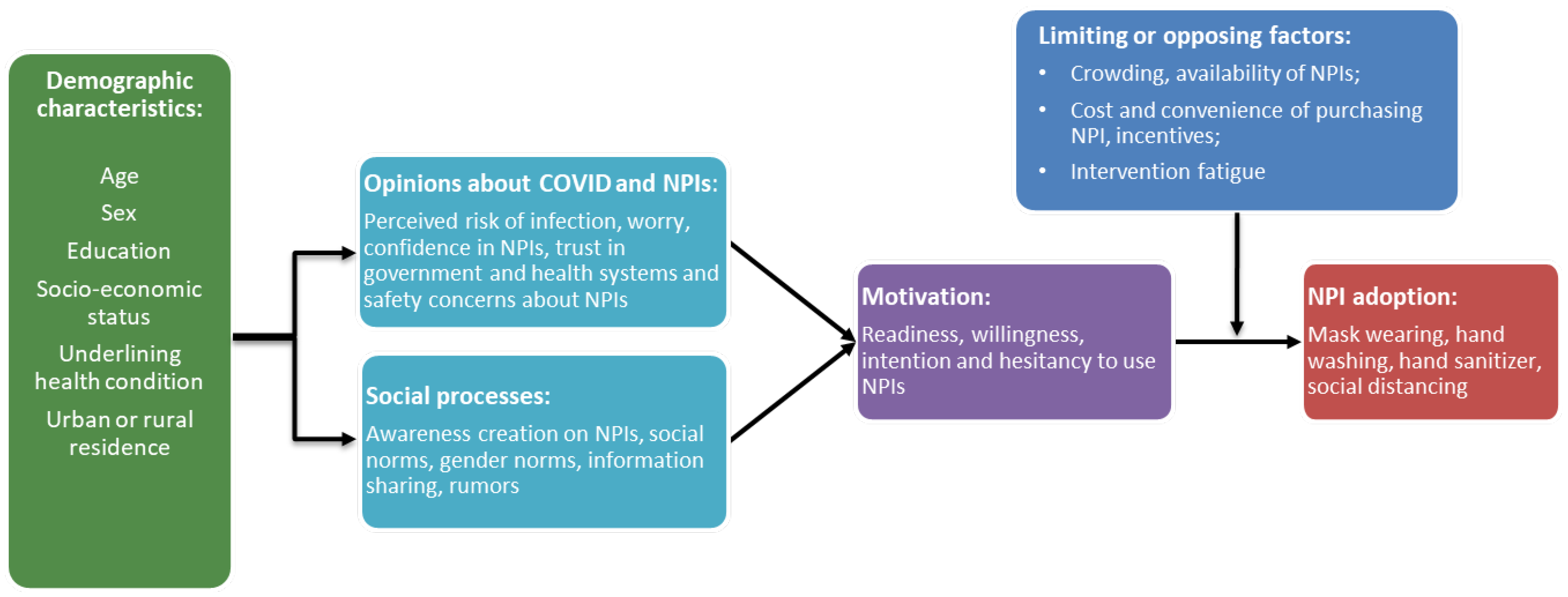
2. Theoretical Framework
3. Methods and Materials
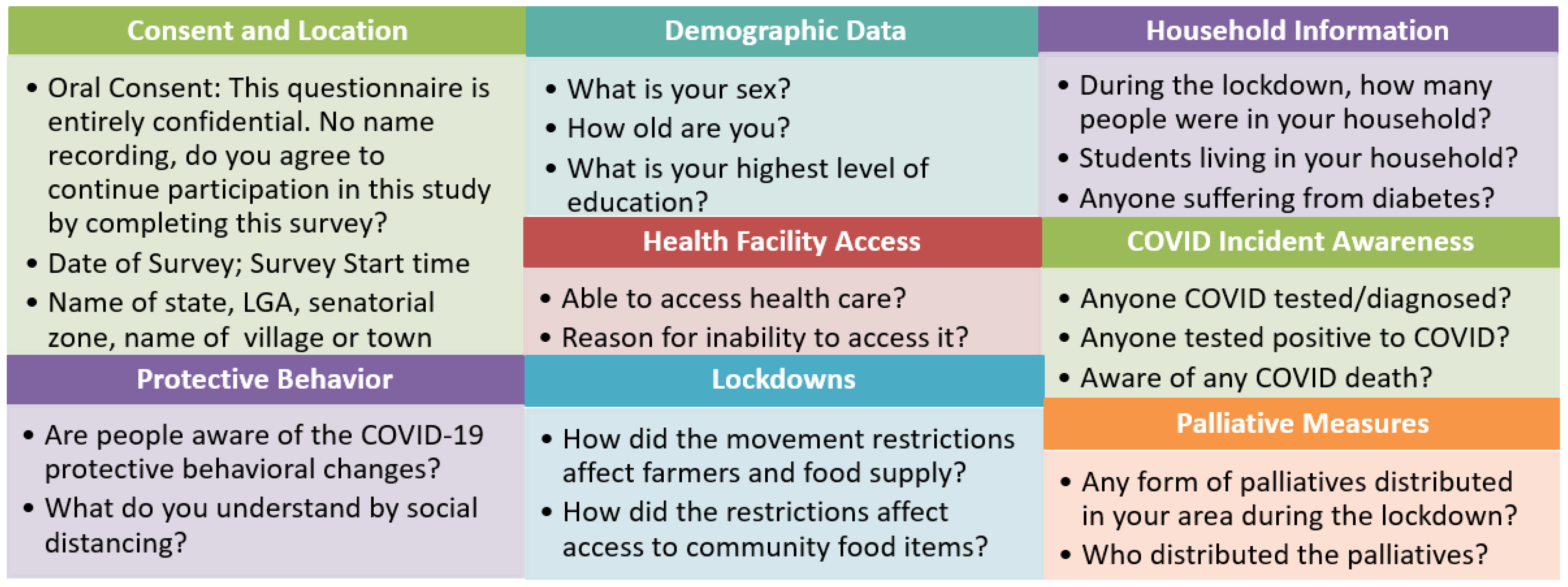
3.1. Data and Data Collection
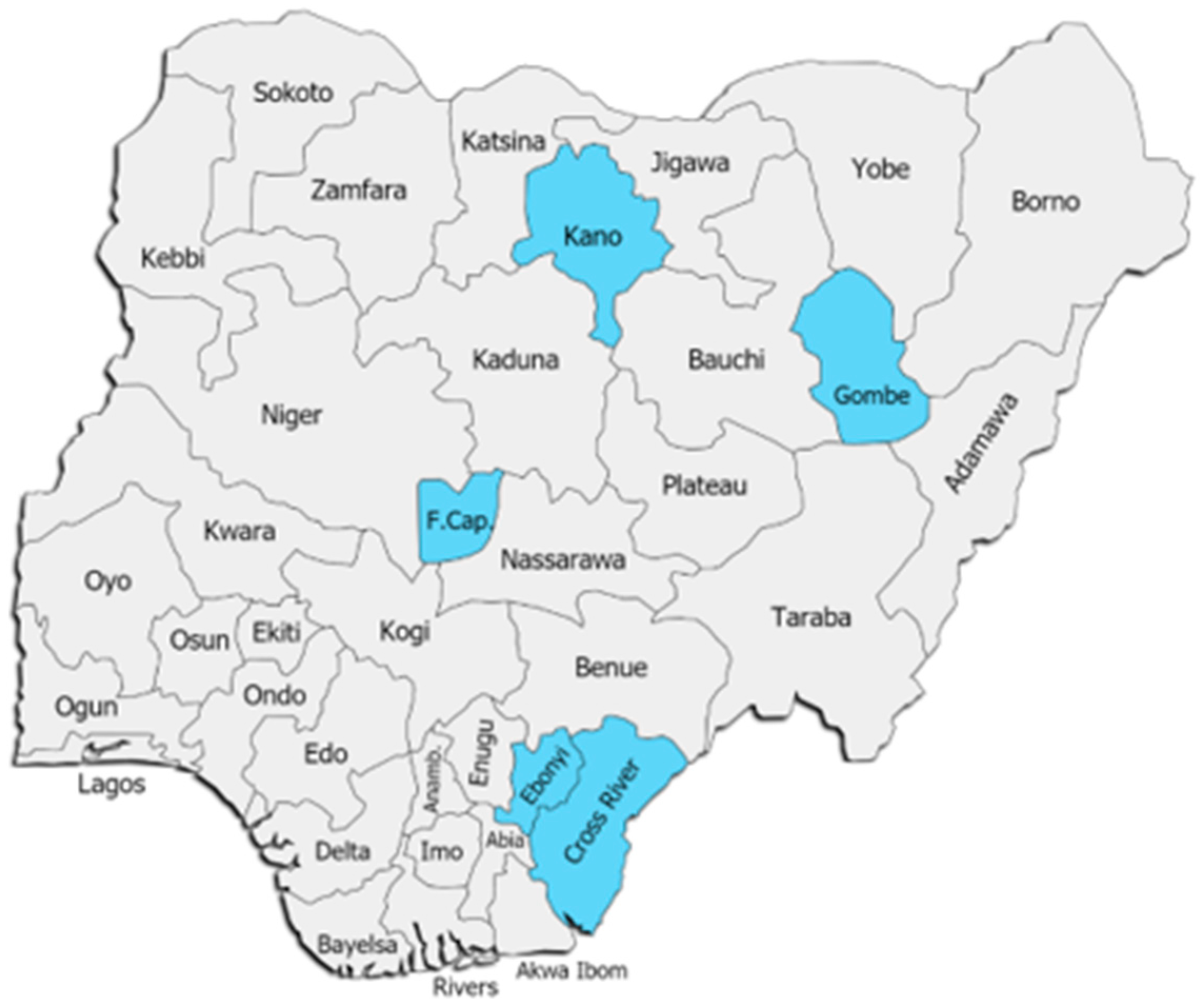
3.1.1. Study Area
3.1.2. Sample Population
3.2. Dependent Variables
3.3. Independent Variables
3.4. Control Variables
3.5. Estimation Method
4. Results
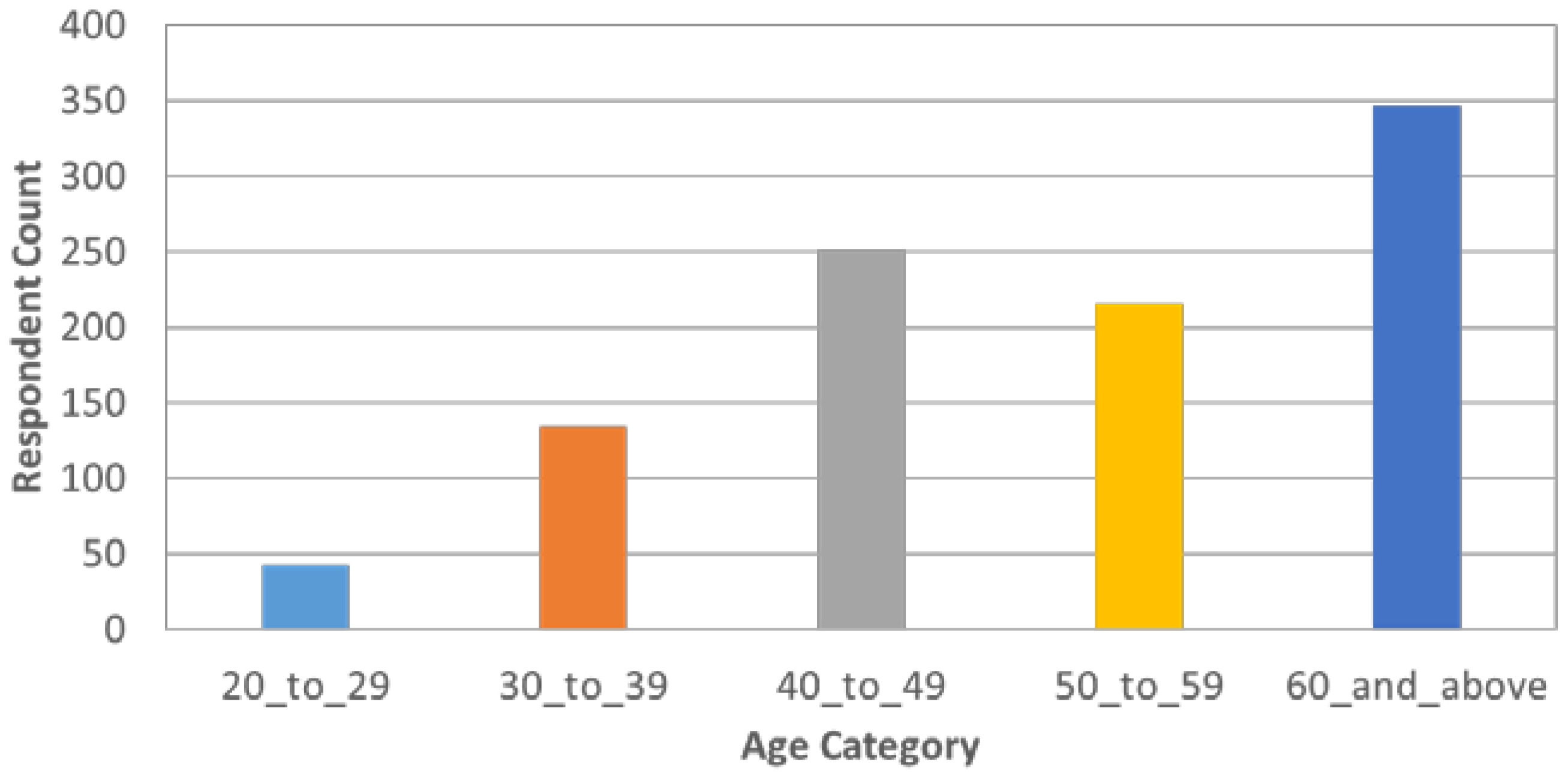
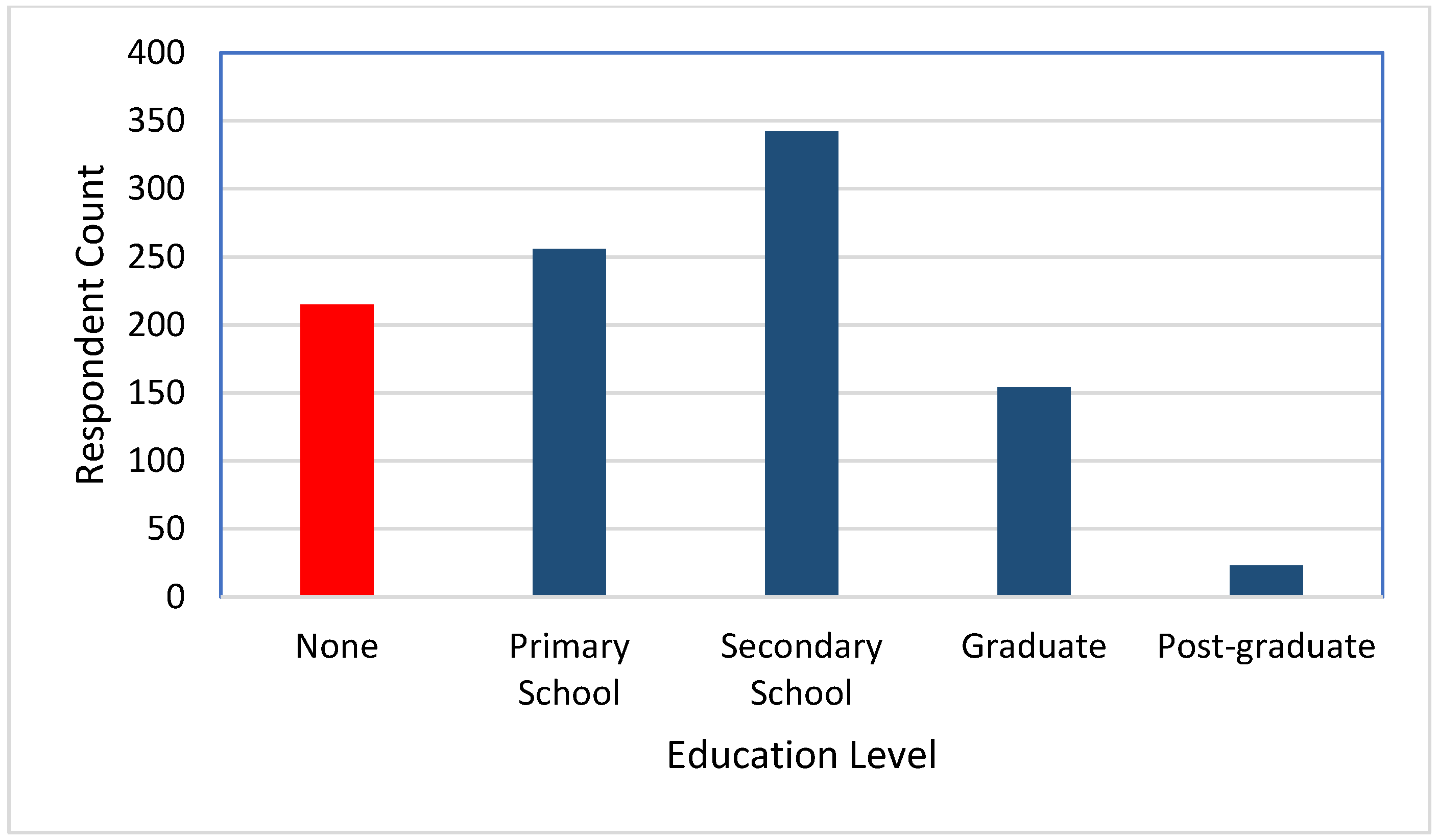
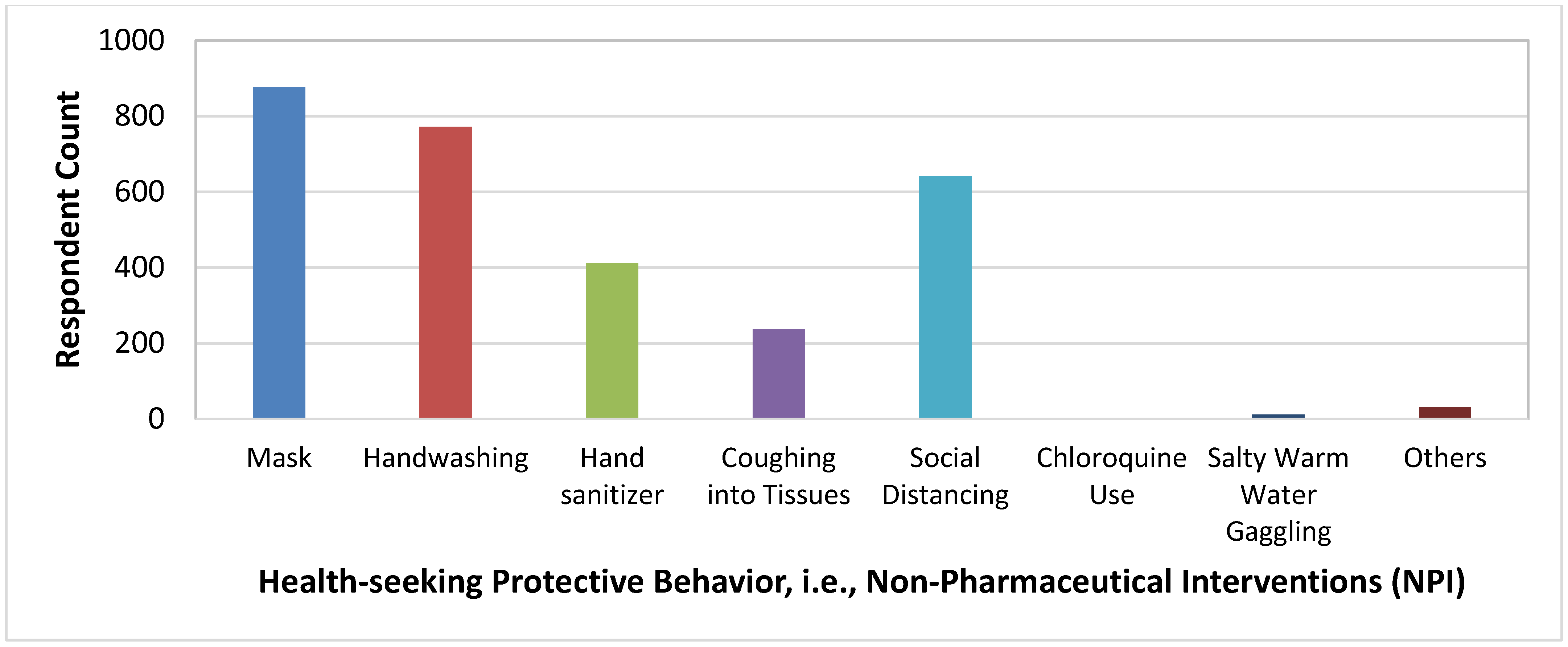
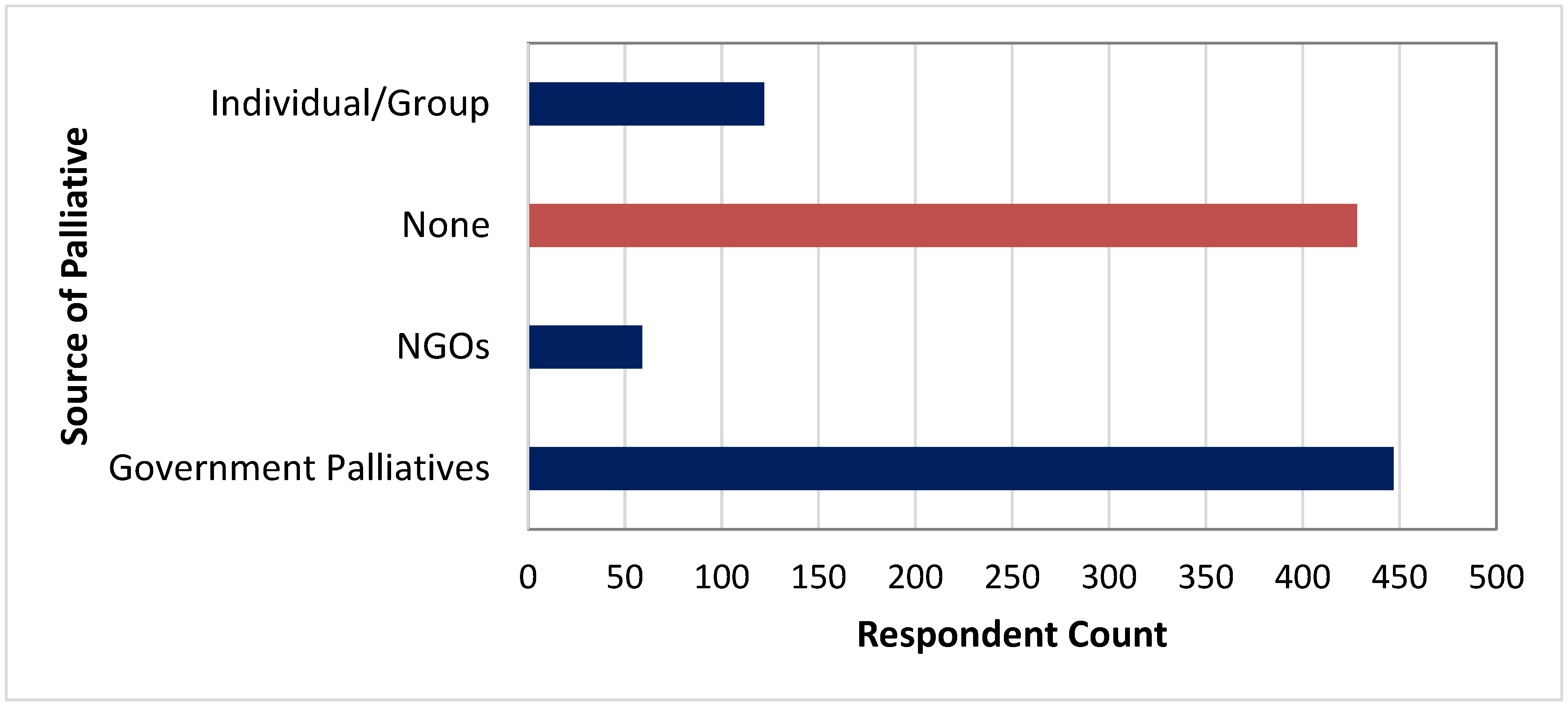
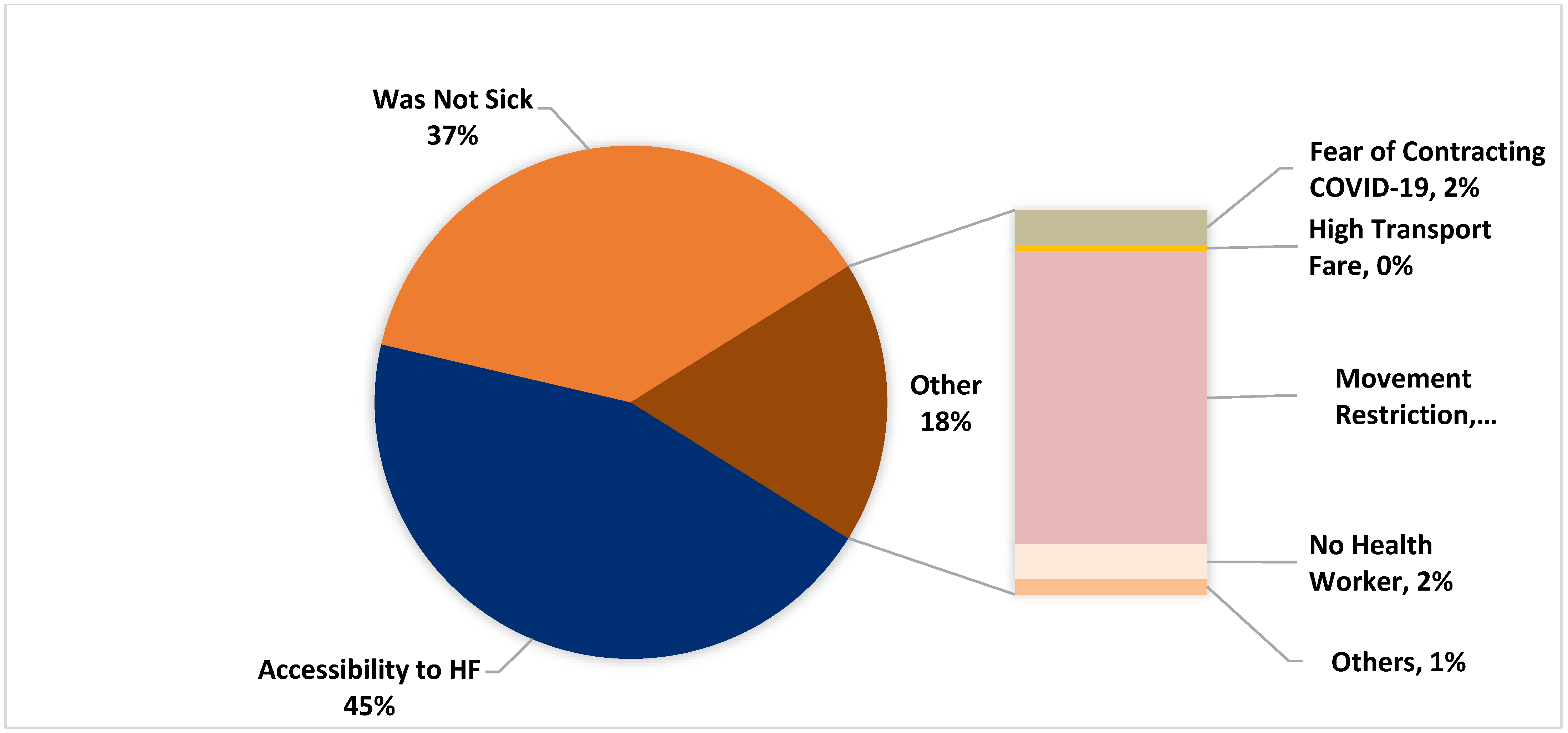
Descriptive Statistics
5. Model Diagnostics
6. Robustness Tests
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AIC | Akaike Information Criterion |
| BIC | Bayesian Information Criterion |
| COMCiRIN | Coordinating and Mobilizing Civil Society Response in Nigeria |
| COVID-19 | SARS-CoV-2 pandemic |
| CSO | Civil Society Organizations |
| FCT | Federal Capital Territory |
| LGA | Local Government Areas |
| LQAS | Lots Quality Assessment Survey |
| NPI | Non-Pharmaceutical Intervention |
| ODK | Open Data Kit |
| PPS | Probability of Proportional to Sample size |
| PTF | Presidential Task Force |
| SPHCDA | State Primary Health Care Development Agency |
| VIF | Variance Inflation Factors |
| WAVA | Women Advocates for Vaccine Access |
| WHO | World Health Organization |
References
- World Health Organization. Non-Pharmaceutical Public Health Measures for Mitigating the Risk and Impact of Epidemic and Pandemic Influenza: Annex: Report of Systematic Literature Reviews; World Health Organization: Geneva, Swizerland, 2019.
- Fong, M.W.; Gao, H.; Wong, J.Y.; Xiao, J.; Shiu, E.Y.; Ryu, S.; Cowling, B.J. Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Social Distancing Measures. Emerg. Infect. Dis. 2020, 26, 976. [Google Scholar] [CrossRef] [PubMed]
- Wiley, L.F. Public Health Law and Science in the Community Mitigation Strategy for COVID-19. J. Law Biosci. 2020, 7, lsaa019. [Google Scholar] [CrossRef] [PubMed]
- Trabelsi, K.; Ammar, A.; Masmoudi, L.; Boukhris, O.; Chtourou, H.; Bouaziz, B.; Brach, M.; Bentlage, E.; How, D.; Ahmed, M. Globally Altered Sleep Patterns and Physical Activity Levels by Confinement in 5056 Individuals: ECLB COVID-19 International Online Survey. Biol. Sport 2021, 38, 495. [Google Scholar] [CrossRef] [PubMed]
- Romdhani, M.; Rae, D.E.; Nédélec, M.; Ammar, A.; Chtourou, H.; Al Horani, R.; Ben Saad, H.; Bragazzi, N.; Dönmez, G.; Driss, T. COVID-19 Lockdowns: A Worldwide Survey of Circadian Rhythms and Sleep Quality in 3911 Athletes from 49 Countries, with Data-Driven Recommendations. Sports Med. 2021, 1–16. [Google Scholar] [CrossRef]
- Washif, J.A.; Farooq, A.; Krug, I.; Pyne, D.B.; Verhagen, E.; Taylor, L.; Wong, D.P.; Mujika, I.; Cortis, C.; Haddad, M. Training during the COVID-19 Lockdown: Knowledge, Beliefs, and Practices of 12,526 Athletes from 142 Countries and Six Continents. Sports Med. 2021; 1–16, online ahead of print. [Google Scholar]
- Imai, N.; Gaythorpe, K.A.; Abbott, S.; Bhatia, S.; van Elsland, S.; Prem, K.; Liu, Y.; Ferguson, N.M. Adoption and Impact of Non-Pharmaceutical Interventions for COVID-19. Wellcome Open Res. 2020, 5, 59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brauner, J.M.; Mindermann, S.; Sharma, M.; Johnston, D.; Salvatier, J.; Gavenčiak, T.; Stephenson, A.B.; Leech, G.; Altman, G.; Mikulik, V. Inferring the Effectiveness of Government Interventions against COVID-19. Science 2021, 371, eabd9338. [Google Scholar] [CrossRef]
- Pan, A.; Liu, L.; Wang, C.; Guo, H.; Hao, X.; Wang, Q.; Huang, J.; He, N.; Yu, H.; Lin, X. Association of Public Health Interventions with the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA 2020, 323, 1915–1923. [Google Scholar] [CrossRef] [Green Version]
- Lai, S.; Ruktanonchai, N.W.; Zhou, L.; Prosper, O.; Luo, W.; Floyd, J.R.; Wesolowski, A.; Santillana, M.; Zhang, C.; Du, X. Effect of Non-Pharmaceutical Interventions to Contain COVID-19 in China. Nature 2020, 585, 410–413. [Google Scholar] [CrossRef]
- Chowdhury, R.; Heng, K.; Shawon, M.S.R.; Goh, G.; Okonofua, D.; Ochoa-Rosales, C.; Gonzalez-Jaramillo, V.; Bhuiya, A.; Reidpath, D.; Prathapan, S. Dynamic Interventions to Control COVID-19 Pandemic: A Multivariate Prediction Modelling Study Comparing 16 Worldwide Countries. Eur. J. Epidemiol. 2020, 35, 389–399. [Google Scholar] [CrossRef]
- Davies, N.G.; Kucharski, A.J.; Eggo, R.M.; Gimma, A.; Edmunds, W.J.; Jombart, T.; O’Reilly, K.; Endo, A.; Hellewell, J.; Nightingale, E.S. Effects of Non-Pharmaceutical Interventions on COVID-19 Cases, Deaths, and Demand for Hospital Services in the UK: A Modelling Study. Lancet Public Health 2020, 5, e375–e385. [Google Scholar] [CrossRef]
- Flaxman, S.; Mishra, S.; Gandy, A.; Unwin, H.J.T.; Mellan, T.A.; Coupland, H.; Whittaker, C.; Zhu, H.; Berah, T.; Eaton, J.W. Estimating the Effects of Non-Pharmaceutical Interventions on COVID-19 in Europe. Nature 2020, 584, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Michener, L.; Aguilar-Gaxiola, S.; Alberti, P.M.; Castaneda, M.J.; Castrucci, B.C.; Harrison, L.M.; Hughes, L.S.; Richmond, A.; Wallerstein, N. Peer Reviewed: Engaging with Communities—Lessons (Re) Learned from COVID-19. Prev. Chronic Dis. 2020, 17, E65. [Google Scholar] [CrossRef]
- Rana, I.A.; Bhatti, S.S.; Aslam, A.B.; Jamshed, A.; Ahmad, J.; Shah, A.A. COVID-19 Risk Perception and Coping Mechanisms: Does Gender Make a Difference? Int. J. Disaster Risk Reduct. 2021, 55, 102096. [Google Scholar] [CrossRef] [PubMed]
- Rajpal, A.; Rahimi, L.; Ismail-Beigi, F. Factors Leading to High Morbidity and Mortality of COVID-19 in Patients with Type 2 Diabetes. J. Diabetes 2020, 12, 895–908. [Google Scholar] [CrossRef] [PubMed]
- Finer, N.; Garnett, S.P.; Bruun, J.M. COVID-19 and Obesity. Clin. Obes. 2020, 10, e12365. [Google Scholar] [CrossRef]
- Lippi, G.; Wong, J.; Henry, B.M. Hypertension and Its Severity or Mortality in Coronavirus Disease 2019 (COVID-19): A Pooled Analysis. Pol. Arch. Intern. Med. 2020, 130, 304–309. [Google Scholar] [CrossRef] [Green Version]
- Vahidy, F.S.; Pan, A.P.; Ahnstedt, H.; Munshi, Y.; Choi, H.A.; Tiruneh, Y.; Nasir, K.; Kash, B.A.; Andrieni, J.D.; McCullough, L.D. Sex Differences in Susceptibility, Severity, and Outcomes of Coronavirus Disease 2019: Cross-Sectional Analysis from a Diverse US Metropolitan Area. PLoS ONE 2021, 16, e0245556. [Google Scholar] [CrossRef]
- Dan-Nwafor, C.; Ochu, C.L.; Elimian, K.; Oladejo, J.; Ilori, E.; Umeokonkwo, C.; Steinhardt, L.; Igumbor, E.; Wagai, J.; Okwor, T. Nigeria’s Public Health Response to the COVID-19 Pandemic: January to May 2020. J. Glob. Health 2020, 10, 020399. [Google Scholar] [CrossRef]
- WAVA. COMCiRIN Pulse Survey Consolidated Report Summary: August–December 2020; Women Advocates for Vaccine Access (WAVA): Maitama, Nigeria, 2020. [Google Scholar]
- WAVA. COMCiRIN Rapid Situational Analysis of COVID-19 Government Response Efforts in Nigeria Phase Ii February–October 2020; Women Advocates for Vaccine Access (WAVA): Maitama, Nigeria, 2020. [Google Scholar]
- Brewer, N.T.; Chapman, G.B.; Rothman, A.J.; Leask, J.; Kempe, A. Increasing Vaccination: Putting Psychological Science into Action. Psychol. Sci. Public Interest 2017, 18, 149–207. [Google Scholar] [CrossRef] [Green Version]
- Oseni, G.; Palacios-Lopez, A.; Mcgee, K.; Amankwah, A. Tracking the Socioeconomic Impacts of the Pandemic in Nigeria: Results from the First Three Rounds of the Nigeria COVID-19 National Longitudinal Phone Survey. World Bank Blog. 2020, 16. Available online: https://blogs.worldbank.org/opendata/tracking-socioeconomic-impacts-pandemic-nigeria-results-first-three-rounds-nigeria-covid (accessed on 19 February 2022).
- Greene, W.H. Econometric Analysis; Pearson Education India: London, UK, 2003. [Google Scholar]
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013; Volume 398. [Google Scholar]
- Pagano, M.; Gauvreau, K. Principles of Biostatistics; CRC Press: Boca Raton, FL, USA, 2018. [Google Scholar]
- Kleinbaum, D.G.; Klein, M. Introduction to Logistic Regression. In Logistic Regression; Springer: New York, NY, USA, 2010; pp. 1–39. [Google Scholar]
- Pampel, F.C. Logistic Regression: A Primer; Sage Publications: Thousand Oaks, CA, USA, 2020; Volume 132. [Google Scholar]
- Spagnolo, P.A.; Manson, J.E.; Joffe, H. Sex and Gender Differences in Health: What the COVID-19 Pandemic Can Teach Us. Ann. Intern. Med. 2020, 173, 385–386. [Google Scholar] [CrossRef]
- Halcoussis, D. Understanding Econometrics; South-Western: Aberdeen, UK, 2005. [Google Scholar]
- Greenhill, B.; Ward, M.D.; Sacks, A. The Separation Plot: A New Visual Method for Evaluating the Fit of Binary Models. Am. J. Political Sci. 2011, 55, 991–1002. [Google Scholar] [CrossRef]
- King, G. How Not to Lie with Statistics: Avoiding Common Mistakes in Quantitative Political Science. Am. J. Political Sci. 1986, 30, 666–687. [Google Scholar] [CrossRef]
- Bianco, A.M.; Martínez, E. Robust Testing in the Logistic Regression Model. Comput. Stat. Data Anal. 2009, 53, 4095–4105. [Google Scholar] [CrossRef]
- Cramer, J.S. Robustness of Logit Analysis: Unobserved Heterogeneity and Mis-Specified Disturbances. Oxf. Bull. Econ. Stat. 2007, 69, 545–555. [Google Scholar] [CrossRef]
- Wiersema, M.F.; Bowen, H.P. The Use of Limited Dependent Variable Techniques in Strategy Research: Issues and Methods. Strateg. Manag. J. 2009, 30, 679–692. [Google Scholar] [CrossRef]
- Bowen, H.P. Testing Moderating Hypotheses in Limited Dependent Variable and Other Nonlinear Models: Secondary versus Total Interactions. J. Manag. 2012, 38, 860–889. [Google Scholar] [CrossRef]
- Brooks, J.T.; Butler, J.C. Effectiveness of Mask Wearing to Control Community Spread of SARS-CoV-2. JAMA 2021, 325, 998–999. [Google Scholar] [CrossRef]
- Shittu, E.; Parker, G.; Mock, N. Improving Communication Resilience for Effective Disaster Relief Operations. Environ. Syst. Decis. 2018, 38, 1–19. [Google Scholar] [CrossRef]
- Shittu, E.; Harnly, M.; Whitaker, S.; Miller, R. Reorganizing Nigeria’s Vaccine Supply Chain Reduces Need for Additional Storage Facilities, but More Storage Is Required. Health Aff. 2016, 35, 293–300. [Google Scholar] [CrossRef] [Green Version]
- Gai, D.H.B.; Graybill, Z.; Voevodsky, P.; Shittu, E. Evaluating Scenarios of Locations and Capacities for Vaccine Storage in Nigeria. Vaccine 2018, 36, 3505–3512. [Google Scholar]

| Variables | Mean | Std Dev. | Mask | Sex | Age | Education | Household Size | Student in Household | COVID Incident | Diabetes | Health Access | Palliatives | Food & Supplies |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mask | 0.89 | 0.32 | 1 | ||||||||||
| Sex | 0.62 | 0.49 | –0.08 *** | 1 | |||||||||
| Age | 42.55 | 16.08 | –0.04 | 0.21 *** | 1 | ||||||||
| Education | 0.78 | 0.41 | 0.10 *** | 0.01 | –0.23 *** | 1 | |||||||
| Household Size | 11.57 | 9.00 | –0.08 ** | 0.18 *** | 0.12 *** | –0.15 *** | 1 | ||||||
| Student in HH | 0.89 | 0.32 | 0.07 ** | –0.01 | 0.02 | 0.17 *** | 0.19 *** | 1 | |||||
| COVID Incident | 0.10 | 0.30 | 0.08 ** | 0.04 | –0.01 | 0.06 ** | 0.14 *** | 0.004 | 1 | ||||
| Diabetes | 0.08 | 0.27 | –0.01 | 0.09 *** | 0.05 * | –0.03 | 0.22 *** | 0.02 | 0.16 *** | 1 | |||
| Health Access | 0.45 | 0.50 | 0.09 *** | 0.07 ** | 0.12 *** | 0.11 *** | 0.002 | 0.08 *** | 0.09 *** | 0.04 | 1 | ||
| Palliatives | 0.48 | 0.50 | 0.14 *** | 0.13 *** | 0.08 *** | –0.11 *** | 0.1 *** | –0.06 ** | 0.08 ** | 0.03 | 0.07 ** | 1 | |
| Food & Supplies | 0.73 | 0.45 | –0.08 ** | 0.021 | –0.14 *** | –0.04 | 0.04 | 0.05 * | 0.06 ** | 0.09 *** | –0.16 *** | –0.01 | 1 |
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | |
|---|---|---|---|---|---|---|---|
| Sex | –0.505 * | –0.515 * | –0.515 * | –0.519 * | –0.523 * | –0.658 ** | –0.624 ** |
| (0.23) | (0.23) | (0.23) | (0.23) | (0.23) | (0.24) | (0.23) | |
| Age | –0.000372 | –0.000361 | –0.00037 | 0.00329 | –0.00237 | –0.00369 | –0.00607 |
| (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | |
| Education | 0.547 * | 0.487 * | 0.487 * | 0.490 * | 0.408 | 0.544 * | 0.505 * |
| (0.23) | (0.24) | (0.24) | (0.24) | (0.24) | (0.25) | (0.25) | |
| Household Size | –0.0184 | –0.0250 * | –0.0251 * | –0.0246 * | –0.0247 * | –0.0314 ** | –0.0321 ** |
| (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | (0.01) | |
| Students in Household | 0.569 * | 0.648 * | 0.649 * | 0.619 * | 0.607 * | 0.737 * | 0.814 ** |
| (0.29) | (0.29) | (0.29) | (0.29) | (0.29) | (0.30) | (0.31) | |
| COVID Incident | 1.396 ** | 1.393 ** | 1.379 * | 1.316 * | 1.200 * | 1.242 * | |
| (0.54) | (0.54) | (0.54) | (0.54) | (0.54) | (0.54) | ||
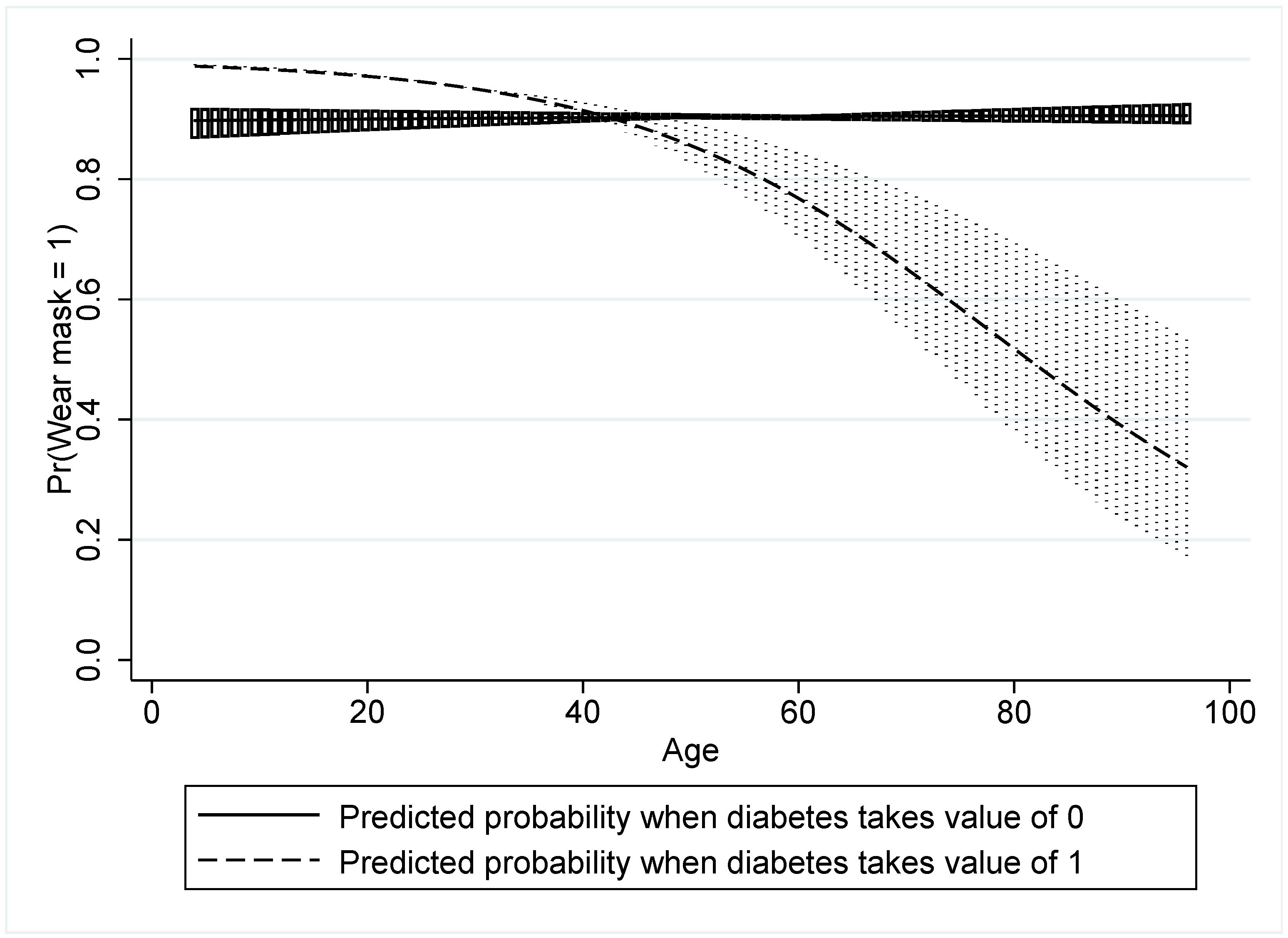
| Diabetes in Hh | 0.015 | 2.152 | 0.0132 | 0.102 | 0.198 | ||
| (0.39) | (1.31) | (0.39) | (0.40) | (0.41) | |||
| Diabetes in Hh X Age | –0.0423 | ||||||
| (0.02) | |||||||
| Health Access | 0.480 * | 0.476 * | 0.377 | ||||
| (0.22) | (0.22) | (0.23) | |||||
| Palliatives | 1.172 *** | 1.160 *** | |||||
| (0.23) | (0.23) | ||||||
| Food and Supplies | –0.597 * | ||||||
| (0.28) | |||||||
| Constant | 1.739 *** | 1.711 *** | 1.711 *** | 1.571 *** | 1.707 *** | 1.278 ** | 1.821 *** |
| (0.42) | (0.42) | (0.42) | (0.43) | (0.42) | (0.44) | (0.51) | |
| AIC | 692.7 | 684.8 | 686.8 | 685.3 | 683.9 | 658 | 654.9 |
| BIC | 722 | 719.1 | 726 | 729.3 | 728 | 707 | 708.8 |
| N | 990 | 990 | 990 | 990 | 990 | 990 | 990 |
| Variable | VIF | Tolerance | R–Squared |
|---|---|---|---|
| Mask | 1.07 | 0.93 | 0.07 |
| Sex | 1.11 | 0.90 | 0.10 |
| Age | 1.17 | 0.86 | 0.14 |
| Education | 1.18 | 0.85 | 0.15 |
| Household Size | 1.19 | 0.84 | 0.16 |
| Student in Household | 1.11 | 0.90 | 0.10 |
| COVID Incident | 1.07 | 0.94 | 0.06 |
| Diabetes | 1.08 | 0.92 | 0.08 |
| Health Access | 1.08 | 0.92 | 0.08 |
| Palliatives | 1.08 | 0.93 | 0.07 |
| Food and Supplies | 1.08 | 0.93 | 0.07 |
| Mean VIF | 1.11 |
| Mask Wearing | Coefficient | St. Err. | t-Value | p-Value | [95% Conf. Interval] | Sig | |
|---|---|---|---|---|---|---|---|
| Sex | –0.495 | 0.225 | –2.200 | 0.028 | –0.935 | –0.055 | ** |
| Age | 0.009 | 0.005 | 1.680 | 0.092 | –0.002 | 0.020 | * |
| Education | 0.901 | 0.212 | 4.250 | 0.000 | 0.485 | 1.318 | *** |
| Household Size | –0.027 | 0.012 | –2.33 | 0.020 | –0.05 | –0.004 | ** |
| Student in Hh | 1.100 | 0.274 | 4.010 | 0.000 | 0.562 | 1.637 | *** |
| COVID Incident | 1.230 | 0.544 | 2.260 | 0.024 | 0.164 | 2.296 | ** |
| Diabetes | 0.115 | 0.407 | 0.280 | 0.778 | –0.682 | 0.912 | |
| Health Access | 0.439 | 0.226 | 1.950 | 0.052 | –0.003 | 0.881 | * |
| Palliatives | 1.307 | 0.231 | 5.640 | 0.000 | 0.853 | 1.760 | *** |
| Food and Supplies | –0.127 | 0.222 | –0.570 | 0.568 | –0.561 | 0.308 | |
| Number of obs | 990 | ||||||
| Chi–square | 350 | ||||||
| Prob > chi2 | 0 | ||||||
| Akaike crit. (AIC) | 667 | ||||||
| Hand Washing | Hand Sanitizer | Social Distancing | |
|---|---|---|---|
| Sex | –0.789 *** | –0.540 *** | 0.098 |
| (0.18) | (0.15) | (0.15) | |
| Age | 0.01 | –0.016 *** | –0.006 |
| (0.01) | (0.01) | (0.00) | |
| Education | 0.463 * | 0.149 | –0.581 ** |
| (0.20) | (0.18) | (0.19) | |
| Household Size | –0.001 | 0.030 *** | –0.012 |
| (0.01) | (0.01) | (0.01) | |
| Students in Household | –0.023 | –0.006 | –0.267 |
| (0.25) | (0.23) | (0.24) | |
| COVID Incident | 0.517 | 0.565 * | 0.047 |
| (0.31) | (0.23) | (0.24) | |
| Diabetes | 0.371 | 0.434 | 0.288 |
| (0.34) | (0.26) | (0.28) | |
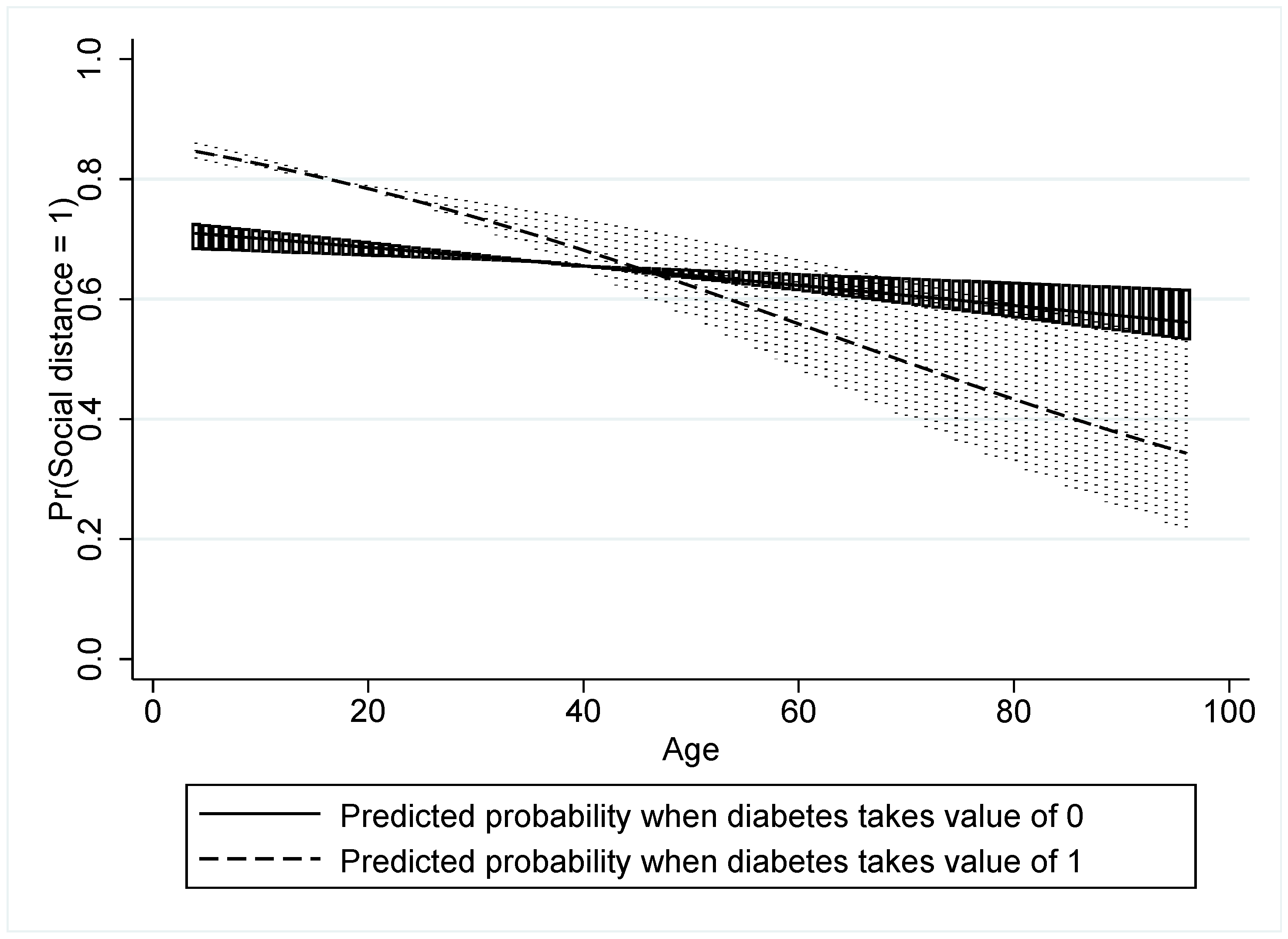
| Diabetes X Age | –0.014 | –0.179 | 0.631 *** |
| (0.17) | (0.14) | (0.15) | |
| Health Access | 0.152 | 0.037 | 0.423 ** |
| (0.16) | (0.14) | (0.14) | |
| Palliatives | 0.651 *** | 0.725 *** | 0.553 *** |
| (0.17) | (0.16) | (0.16) | |
| Food & Supplies | 0.457 | –0.384 | 0.772 * |
| (0.39) | (0.35) | (0.36) | |
| AIC | 1023.1 | 1277.6 | 1253 |
| BIC | 1077 | 1331.5 | 1306.8 |
| N | 990 | 990 | 990 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shittu, E.; Adewumi, F.; Ene, N.; Keluo-Udeke, S.C.; Wonodi, C. Examining Psychosocial Factors and Community Mitigation Practices to Limit the Spread of COVID-19: Evidence from Nigeria. Healthcare 2022, 10, 585. https://doi.org/10.3390/healthcare10030585
Shittu E, Adewumi F, Ene N, Keluo-Udeke SC, Wonodi C. Examining Psychosocial Factors and Community Mitigation Practices to Limit the Spread of COVID-19: Evidence from Nigeria. Healthcare. 2022; 10(3):585. https://doi.org/10.3390/healthcare10030585
Chicago/Turabian StyleShittu, Ekundayo, Funmilayo Adewumi, Nkemdilim Ene, Somto Chloe Keluo-Udeke, and Chizoba Wonodi. 2022. "Examining Psychosocial Factors and Community Mitigation Practices to Limit the Spread of COVID-19: Evidence from Nigeria" Healthcare 10, no. 3: 585. https://doi.org/10.3390/healthcare10030585
APA StyleShittu, E., Adewumi, F., Ene, N., Keluo-Udeke, S. C., & Wonodi, C. (2022). Examining Psychosocial Factors and Community Mitigation Practices to Limit the Spread of COVID-19: Evidence from Nigeria. Healthcare, 10(3), 585. https://doi.org/10.3390/healthcare10030585






