Comprehensive CAD/CAM Prosthetic Rehabilitation Management in a Young Patient with Agenesis: A Case Report
Abstract
:1. Introduction
2. Case Report
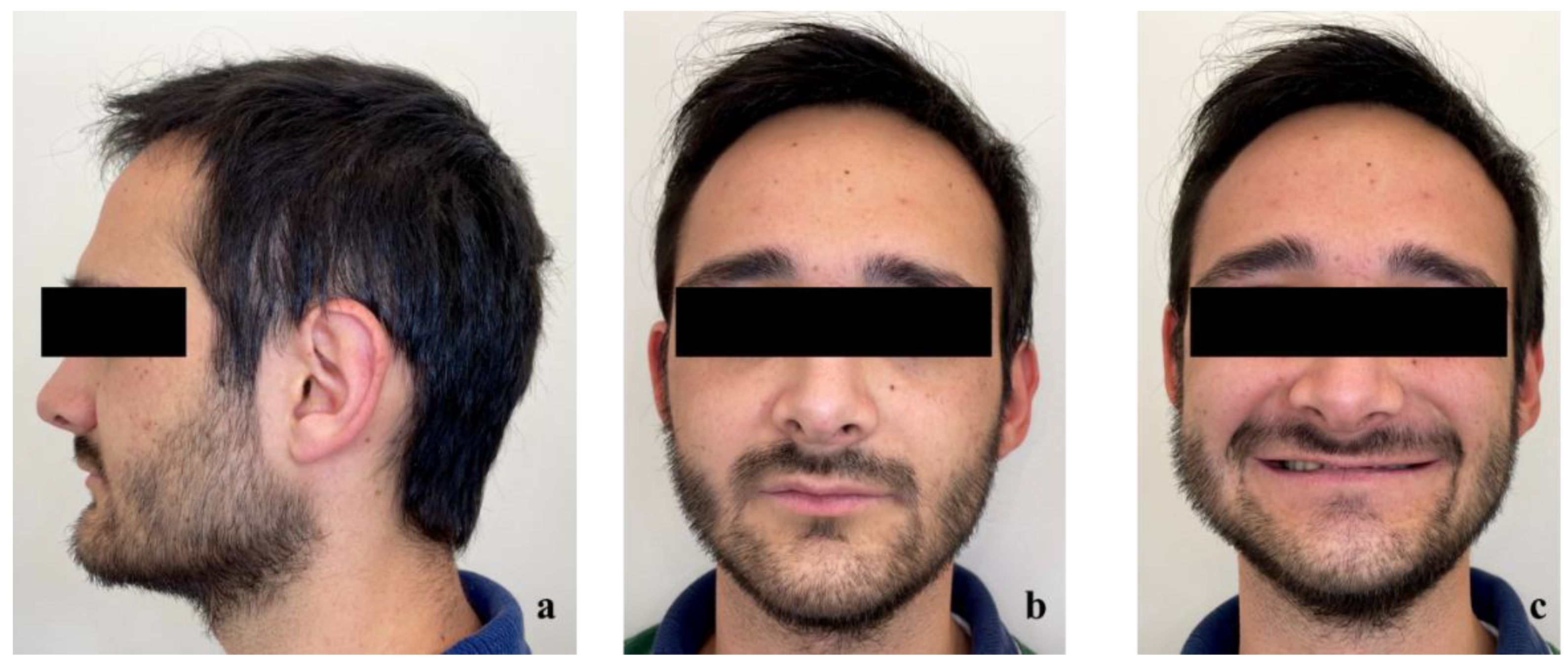
2.1. Case History
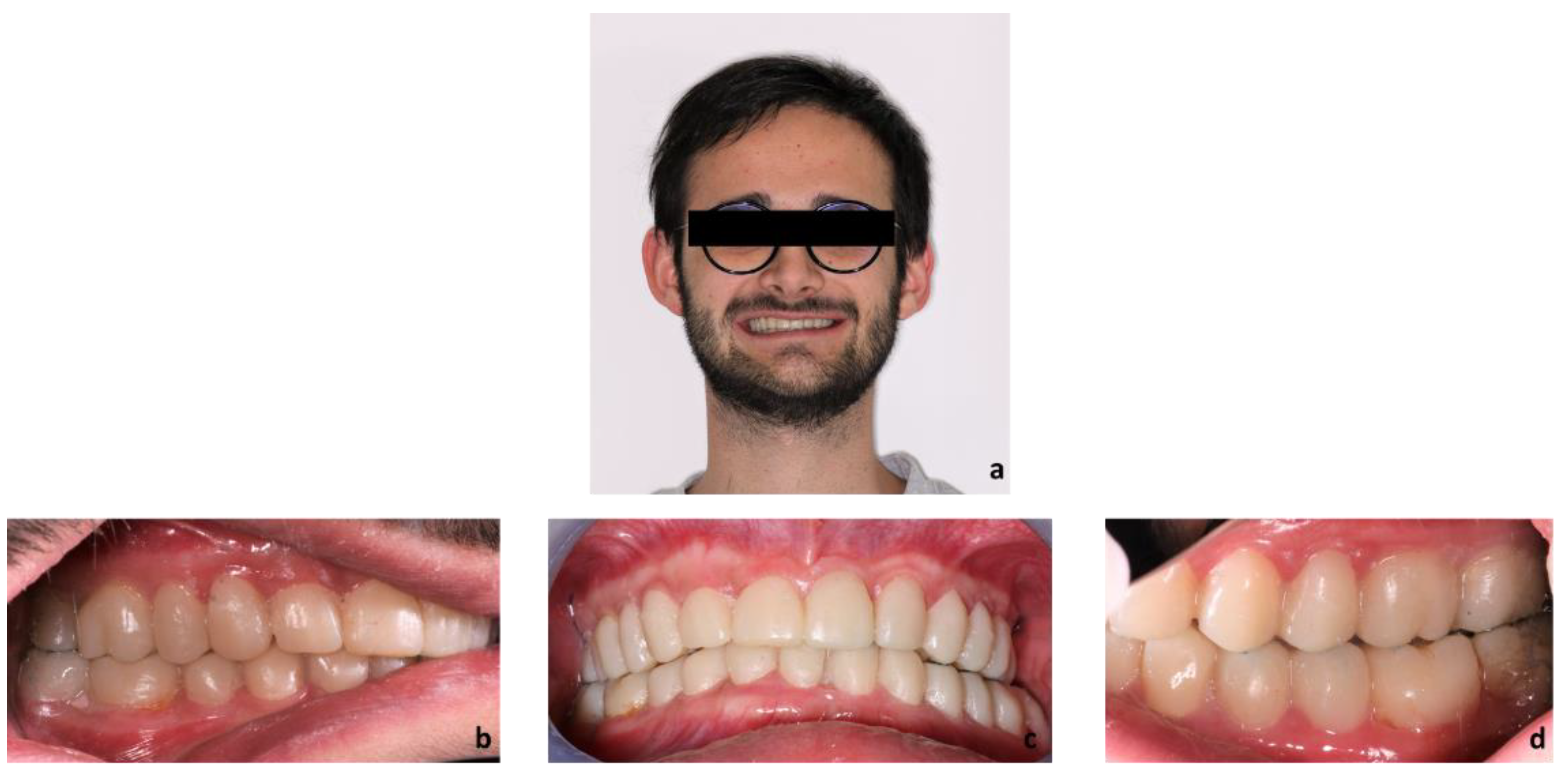
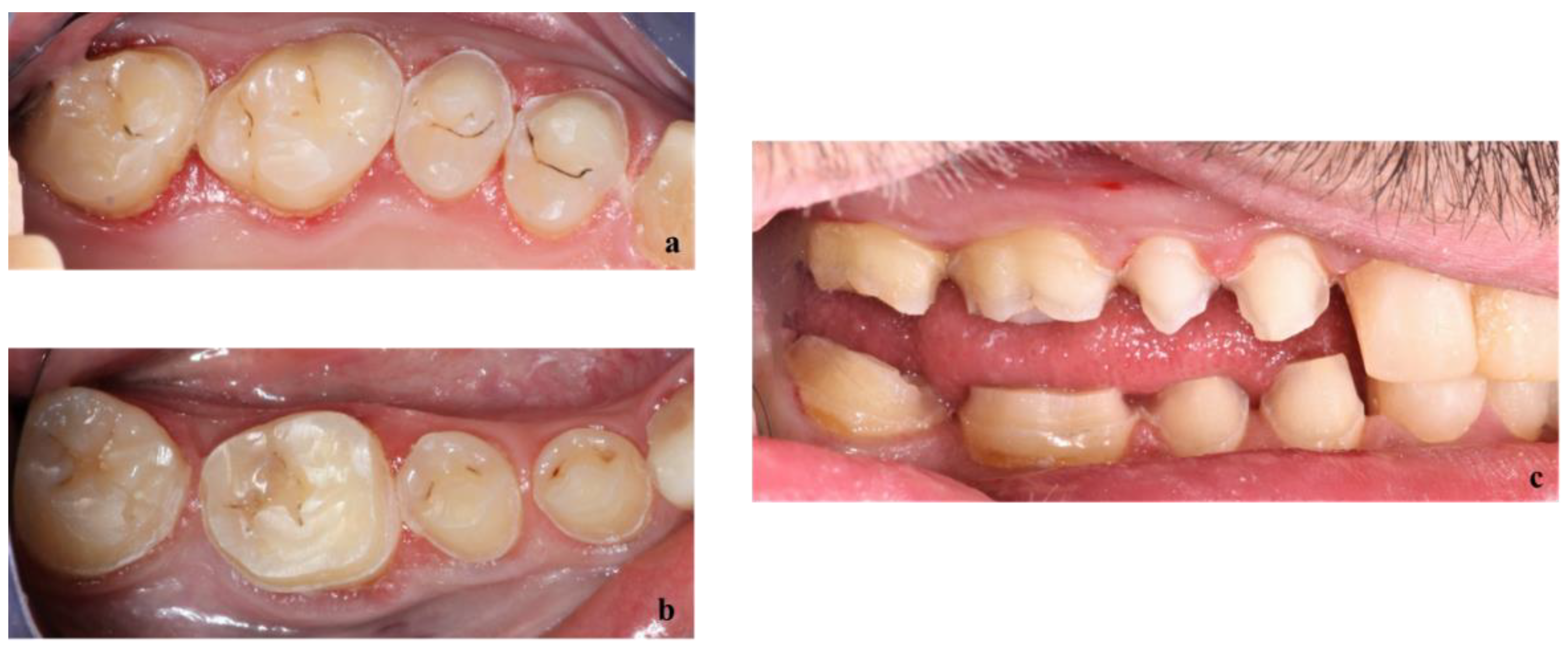
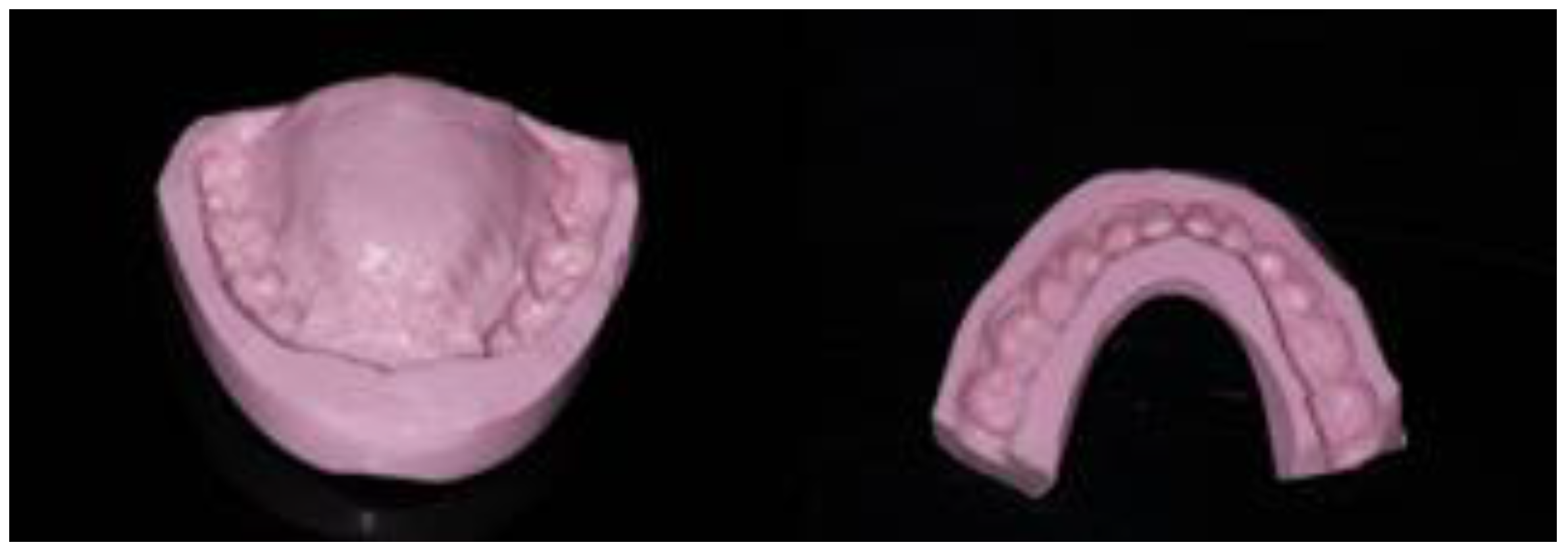
2.2. Diagnostic Assessment
2.3. Therapeutic Objectives
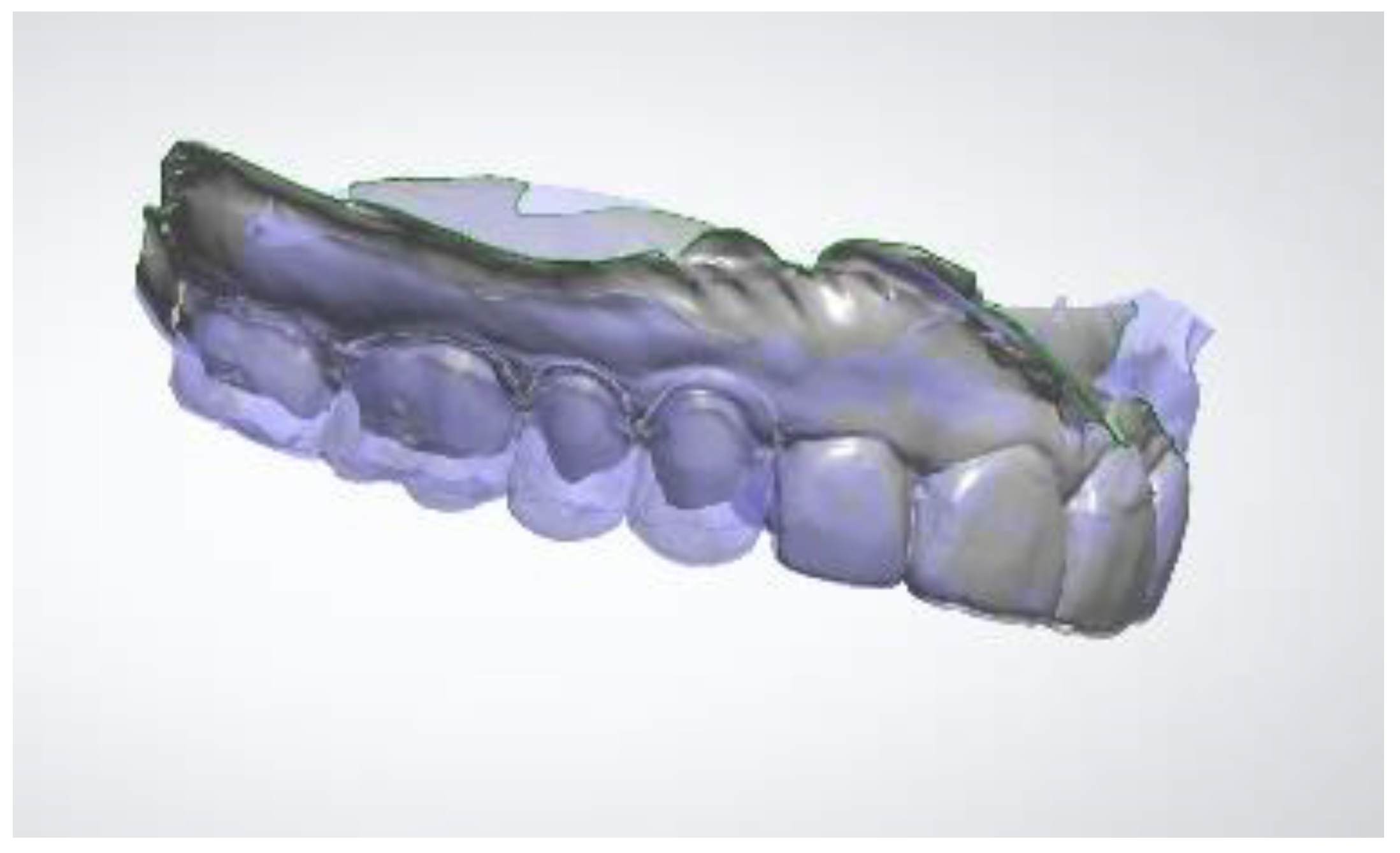
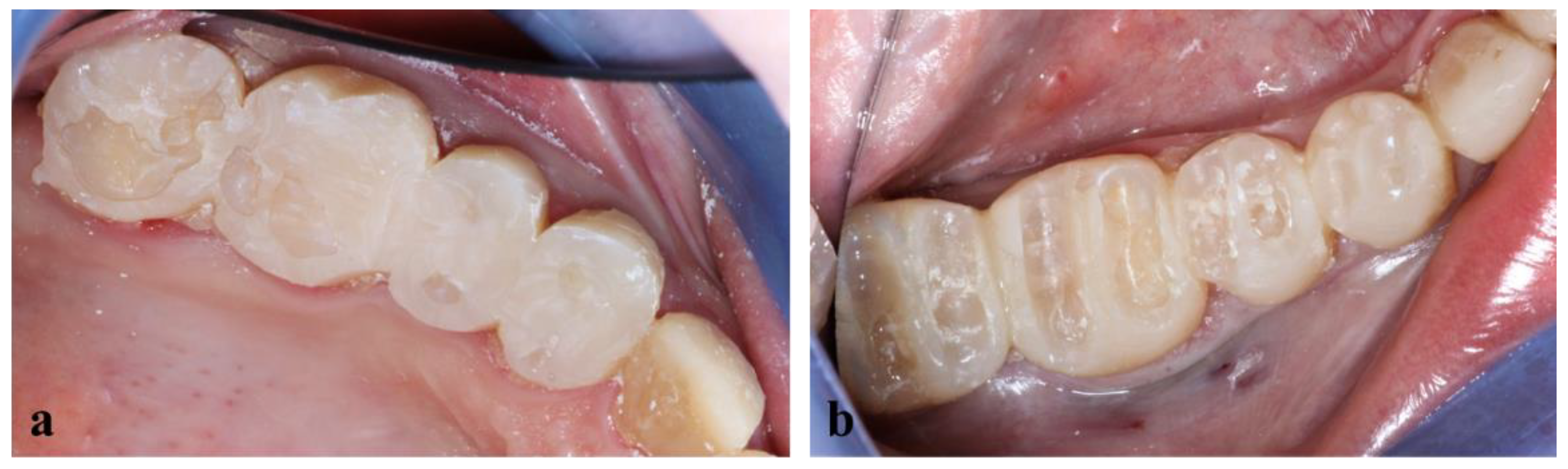
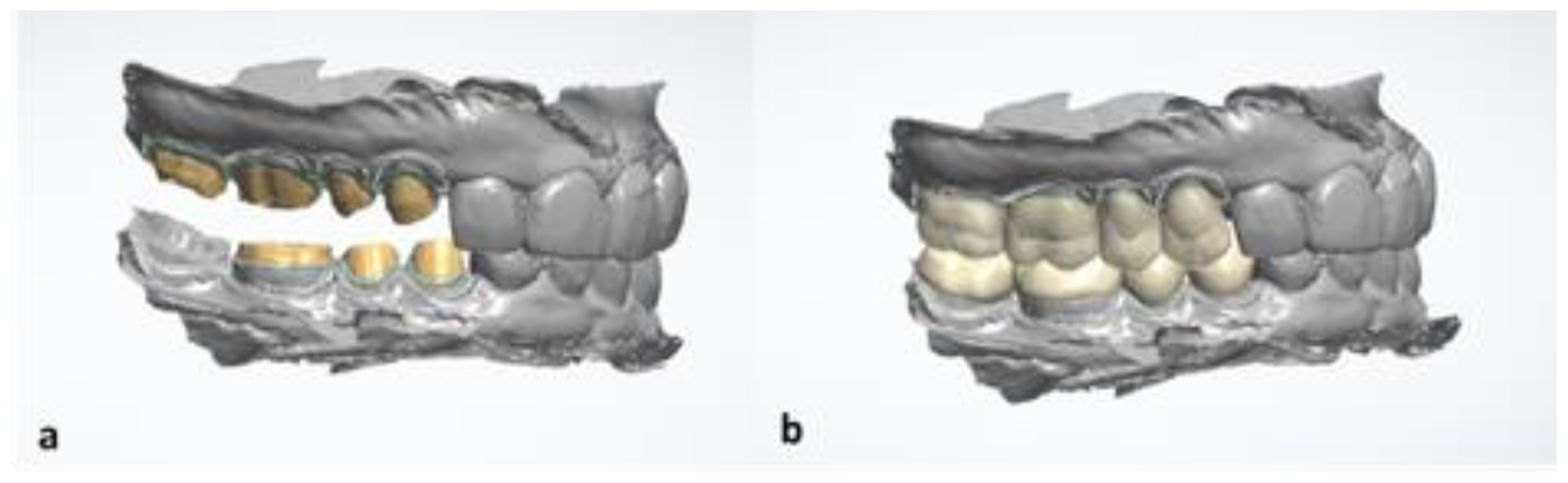
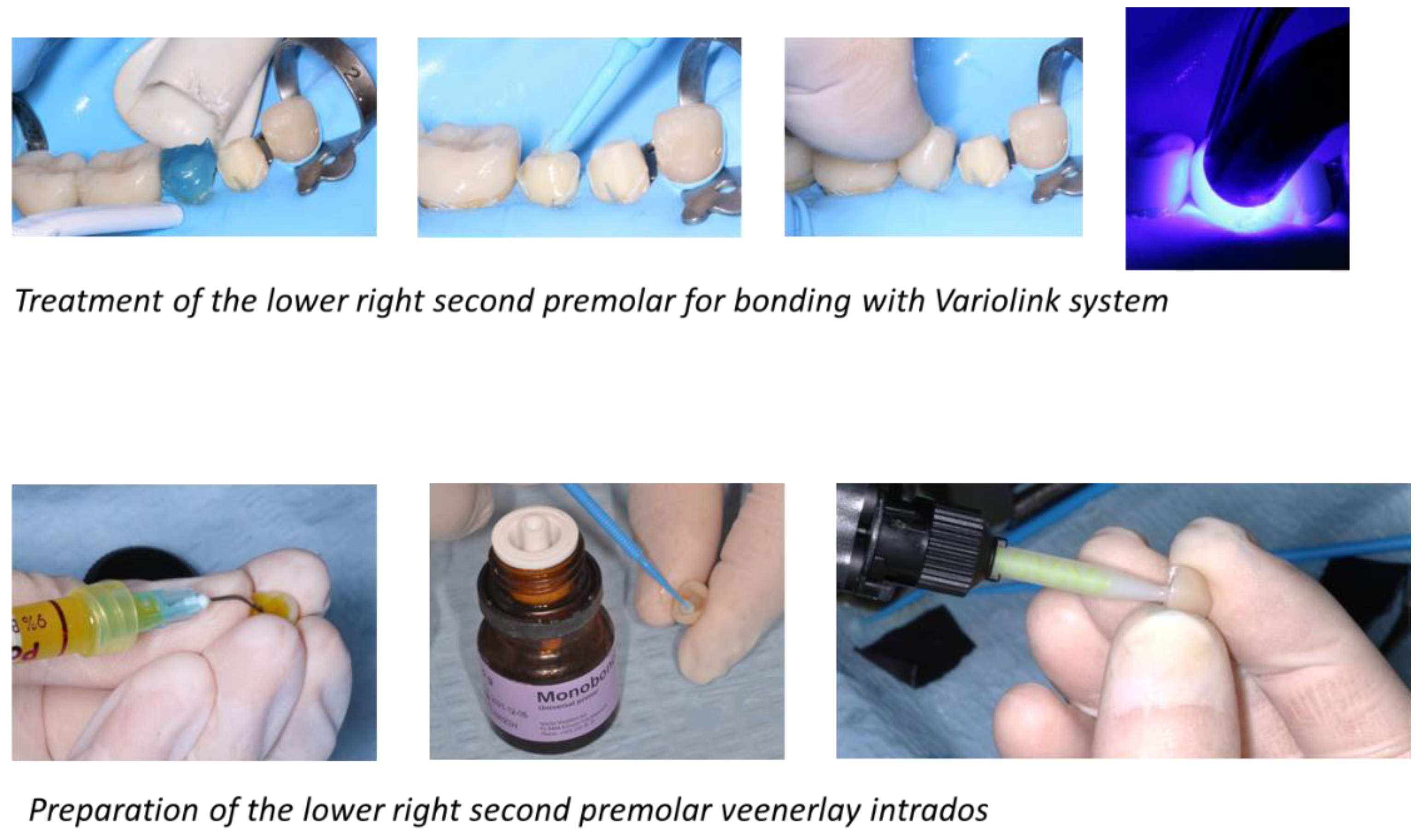
2.4. Treatment
2.5. Results of Treatment
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Bassigny, F. Root resorptions of orthodontic origin. Rev. Odontostomatol. 1982, 11, 305–311. [Google Scholar]
- Masson, E. Facteurs Affectant la Résorption Radiculaire Associée aux Traitements D’orthodontie. Available online: https://www.em-consulte.com/article/95542/facteurs-affectant-la-resorption-radiculaire-assoc (accessed on 3 January 2022).
- Frapier, L.; Massif, L.; Leplus, M.; Chouvin, M.; Canal, P. Conduite à tenir face aux résorptions radiculaires. Rev. Orthop. Dento-Faciale 2007, 41, 295–309. [Google Scholar] [CrossRef]
- Zaruba, M.; Mehl, A. Chairside Systems: A Current Review. Int. J. Comput Dent. 2017, 20, 123–149. [Google Scholar] [PubMed]
- Spitznagel, F.A.; Boldt, J.; Gierthmuehlen, P.C. CAD/CAM Ceramic Restorative Materials for Natural Teeth. J. Dent. Res. 2018, 97, 1082–1091. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Dal Piva, A.M.; Tribst, J.P.M.; Benalcázar Jalkh, E.B.; Anami, L.C.; Bonfante, E.A.; Bottino, M.A. Minimal Tooth Preparation for Posterior Monolithic Ceramic Crowns: Effect on the Mechanical Behavior, Reliability and Translucency. Dent. Mater. 2021, 37, e140–e150. [Google Scholar] [CrossRef]
- Tubert-Jeannin, S.; Riordan, P.J.; Morel-Papernot, A.; Porcheray, S.; Saby-Collet, S. Validation of an Oral Health Quality of Life Index (GOHAI) in France. Commun. Dent. Oral. Epidemiol. 2003, 31, 275–284. [Google Scholar] [CrossRef]
- Hama, Y.; Kanazawa, M.; Minakuchi, S.; Uchida, T.; Sasaki, Y. Properties of a Color-Changeable Chewing Gum Used to Evaluate Masticatory Performance. J. Prosthodont. Res. 2014, 58, 102–106. [Google Scholar] [CrossRef]
- Schimmel, M.; Christou, P.; Herrmann, F.; Müller, F. A Two-Colour Chewing Gum Test for Masticatory Efficiency: Development of Different Assessment Methods. J. Oral Rehabil. 2007, 34, 671–678. [Google Scholar] [CrossRef]
- Gonçalves, T.M.S.V.; Schimmel, M.; van der Bilt, A.; Chen, J.; van der Glas, H.W.; Kohyama, K.; Hennequin, M.; Peyron, M.-A.; Woda, A.; Leles, C.R.; et al. Consensus on the Terminologies and Methodologies for Masticatory Assessment. J. Oral Rehabil. 2021, 48, 745–761. [Google Scholar] [CrossRef]
- Taha, N.A.; Abdulkhader, S.Z. Full Pulpotomy with Biodentine in Symptomatic Young Permanent Teeth with Carious Exposure. J. Endod. 2018, 44, 932–937. [Google Scholar] [CrossRef]
- Munoz-Sanchez, M.-L.; Linas, N.; Decerle, N.; Nicolas, E.; Hennequin, M.; Cousson, P.-Y. A Combination of Full Pulpotomy and Chairside CAD/CAM Endocrown to Treat Teeth with Deep Carious Lesions and Pulpitis in a Single Session: A Preliminary Study. Int. J. Environ. Res. Public Health 2020, 17, 6340. [Google Scholar] [CrossRef] [PubMed]
- Ferraris, F. Posterior Indirect Adhesive Restorations (PIAR): Preparation Designs and Adhesthetics Clinical Protocol. Int. J. Esthet Dent. 2017, 12, 482–502. [Google Scholar]
- Monaco, C.; Arena, A.; Štelemėkaitė, J.; Evangelisti, E.; Baldissara, P. In Vitro 3D and Gravimetric Analysis of Removed Tooth Structure for Complete and Partial Preparations. J. Prosthodont Res. 2019, 63, 173–178. [Google Scholar] [CrossRef] [PubMed]
- El-Meliegy, E.; van Noort, R. Lithium Disilicate Glass Ceramics. In Glasses and Glass Ceramics for Medical Applications; El-Meliegy, E., van Noort, R., Eds.; Springer: New York, NY, USA, 2012; pp. 209–218. ISBN 978-1-4614-1228-1. [Google Scholar]
- Näpänkangas, R.; Raustia, A. Twenty-Year Follow-up of Metal-Ceramic Single Crowns: A Retrospective Study. Int. J. Prosthodont 2008, 21, 307–311. [Google Scholar]
- Sailer, I.; Makarov, N.A.; Thoma, D.S.; Zwahlen, M.; Pjetursson, B.E. All-Ceramic or Metal-Ceramic Tooth-Supported Fixed Dental Prostheses (FDPs)? A Systematic Review of the Survival and Complication Rates. Part I: Single Crowns (SCs). Dent. Mater. 2015, 31, 603–623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rauch, A.; Reich, S.; Dalchau, L.; Schierz, O. Clinical Survival of Chair-Side Generated Monolithic Lithium Disilicate Crowns:10-Year Results. Clin. Oral Investig. 2018, 22, 1763–1769. [Google Scholar] [CrossRef]
- Fradeani, M.; Barducci, G.; Bacherini, L. Esthetic Rehabilitation of a Worn Dentition with a Minimally Invasive Prosthetic Procedure (MIPP). Int. J. Esthet Dent. 2016, 11, 16–35. [Google Scholar]
- Mainjot, A.K.J. The One Step-No Prep Technique: A Straightforward and Minimally Invasive Approach for Full-Mouth Rehabilitation of Worn Dentition Using Polymer-Infiltrated Ceramic Network (PICN) CAD-CAM Prostheses. J. Esthet. Restor. Dent. 2020, 32, 141–149. [Google Scholar] [CrossRef]
- Guess Gierthmuehlen, P.C.; Steger, E. CAD/CAM Solutions for Minimally Invasive All-Ceramic Rehabilitation of Extended Erosive Lesions. Compend. Contin. Educ. Dent. 2016, 37, 340–345. [Google Scholar]
- Noirrit, E.; Chabreron, O.; Nasr, K.; Esclassan, R. A Contribution of CAD/CAM Treatment of a Dental Trauma in a Special Care Patient. Spec. Care Dent. 2018, 38, 55–57. [Google Scholar] [CrossRef]
- Davidovich, E.; Dagon, S.; Tamari, I.; Etinger, M.; Mijiritsky, E. An Innovative Treatment Approach Using Digital Workflow and CAD-CAM Part 2: The Restoration of Molar Incisor Hypomineralization in Children. Int. J. Environ. Res. Public Health 2020, 17, 1499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moreno Soriano, C.; Castañeda Vega, P.; Estrugo Devesa, A.; Jané Salas, E.; López López, J. Frequency and Type of Digital Procedures Used for the Intraoral Prosthetic Rehabilitation of Patients with Head and Neck Cancer: A Systematic Review. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef]
- Carneiro Pereira, A.L.; Bezerra de Medeiros, A.K.; de Sousa Santos, K.; Oliveira de Almeida, É.; Seabra Barbosa, G.A.; da Fonte Porto Carreiro, A. Accuracy of CAD-CAM Systems for Removable Partial Denture Framework Fabrication: A Systematic Review. J. Prosthet. Dent. 2021, 125, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Sambrook, R.J. Longevity of Ceramic Onlays: A Systematic Review. J. Esthet. Restor. Dent. 2018, 30, 193–215. [Google Scholar] [CrossRef] [PubMed]
- Aldegheishem, A.; Ioannidis, G.; Att, W.; Petridis, H. Success and Survival of Various Types of All-Ceramic Single Crowns: A Critical Review and Analysis of Studies with a Mean Follow-Up of 5 Years or Longer. Int. J. Prosthodont. 2017, 30, 168–181. [Google Scholar] [CrossRef] [Green Version]








Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drancourt, N.; Nicolas, E.; Veyrune, J.-L.; Bessadet, M. Comprehensive CAD/CAM Prosthetic Rehabilitation Management in a Young Patient with Agenesis: A Case Report. Healthcare 2022, 10, 382. https://doi.org/10.3390/healthcare10020382
Drancourt N, Nicolas E, Veyrune J-L, Bessadet M. Comprehensive CAD/CAM Prosthetic Rehabilitation Management in a Young Patient with Agenesis: A Case Report. Healthcare. 2022; 10(2):382. https://doi.org/10.3390/healthcare10020382
Chicago/Turabian StyleDrancourt, Noémie, Emmanuel Nicolas, Jean-Luc Veyrune, and Marion Bessadet. 2022. "Comprehensive CAD/CAM Prosthetic Rehabilitation Management in a Young Patient with Agenesis: A Case Report" Healthcare 10, no. 2: 382. https://doi.org/10.3390/healthcare10020382
APA StyleDrancourt, N., Nicolas, E., Veyrune, J.-L., & Bessadet, M. (2022). Comprehensive CAD/CAM Prosthetic Rehabilitation Management in a Young Patient with Agenesis: A Case Report. Healthcare, 10(2), 382. https://doi.org/10.3390/healthcare10020382





