Regression Analysis for COVID-19 Infections and Deaths Based on Food Access and Health Issues
Abstract
:1. Introduction
2. Literature Review
- Is it possible that COVID-19 cases and deaths in geospatial distribution are associated with food outlets and restaurants distribution?
- Can other variables illustrate a geospatial correlation with COVID-19 cases and deaths?
- How can machine learning discover a higher quantitative statistical correlation of COVID-19 cases and deaths against various independent variables?
- Do the machine learning results concur with the GIS regression results?
- Investigated the geospatial association of COVID-19 cases and deaths to food outlets distribution
- Examined the dependency of various socio-economic and health risk variables on COVID-19 cases and deaths
- Applied ML techniques to investigate the statistical association between COVID-19 cases and deaths to other variables
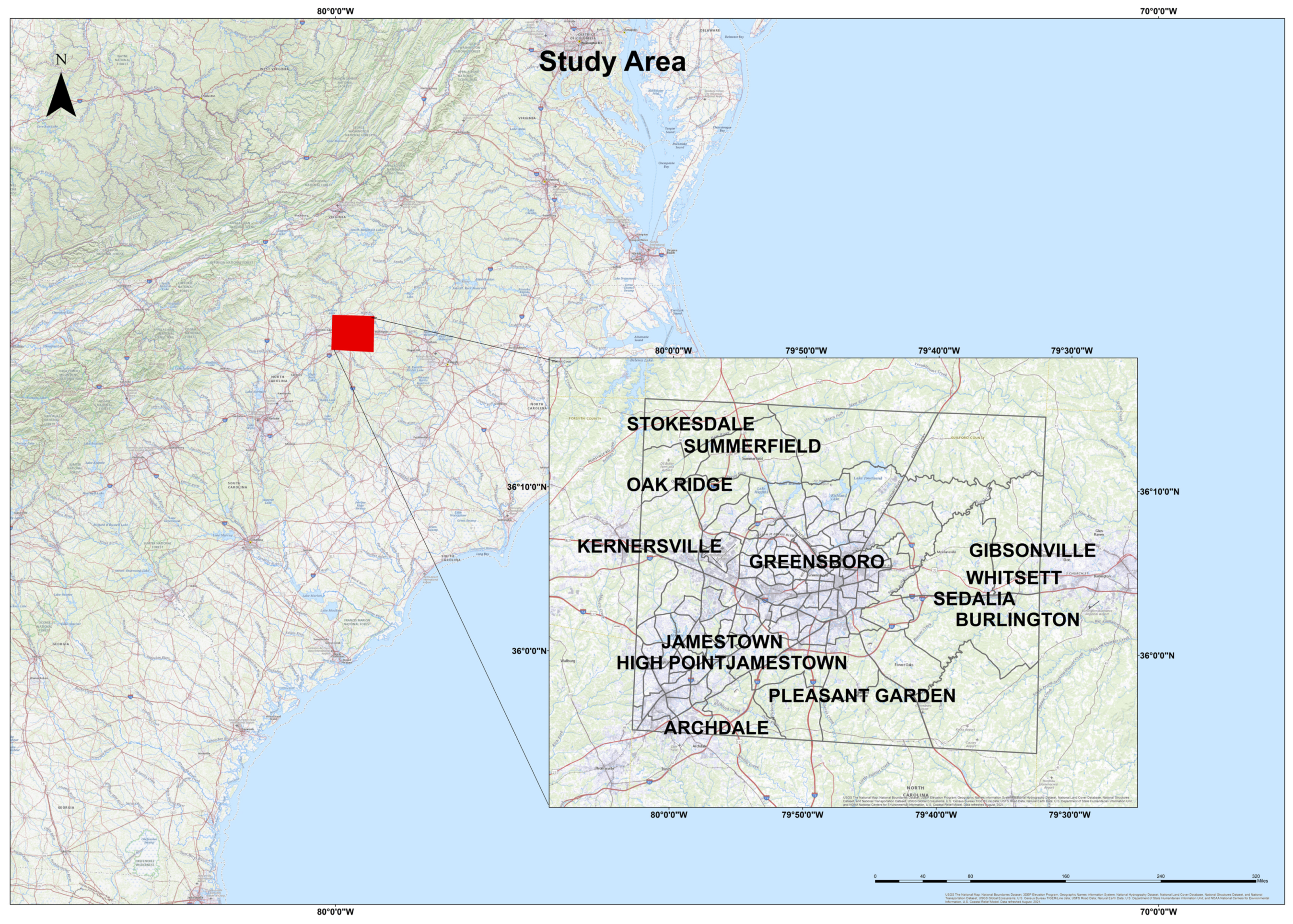
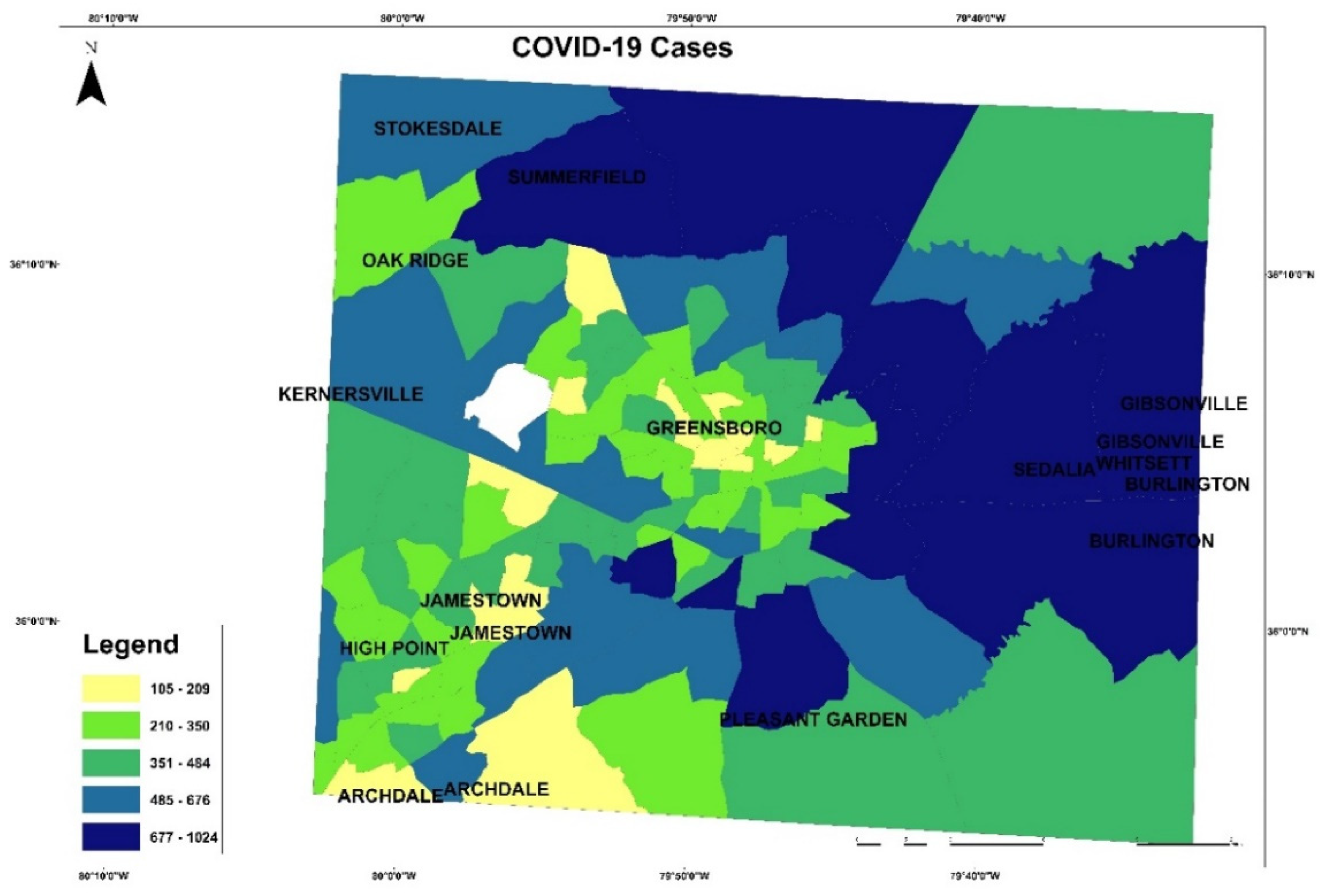
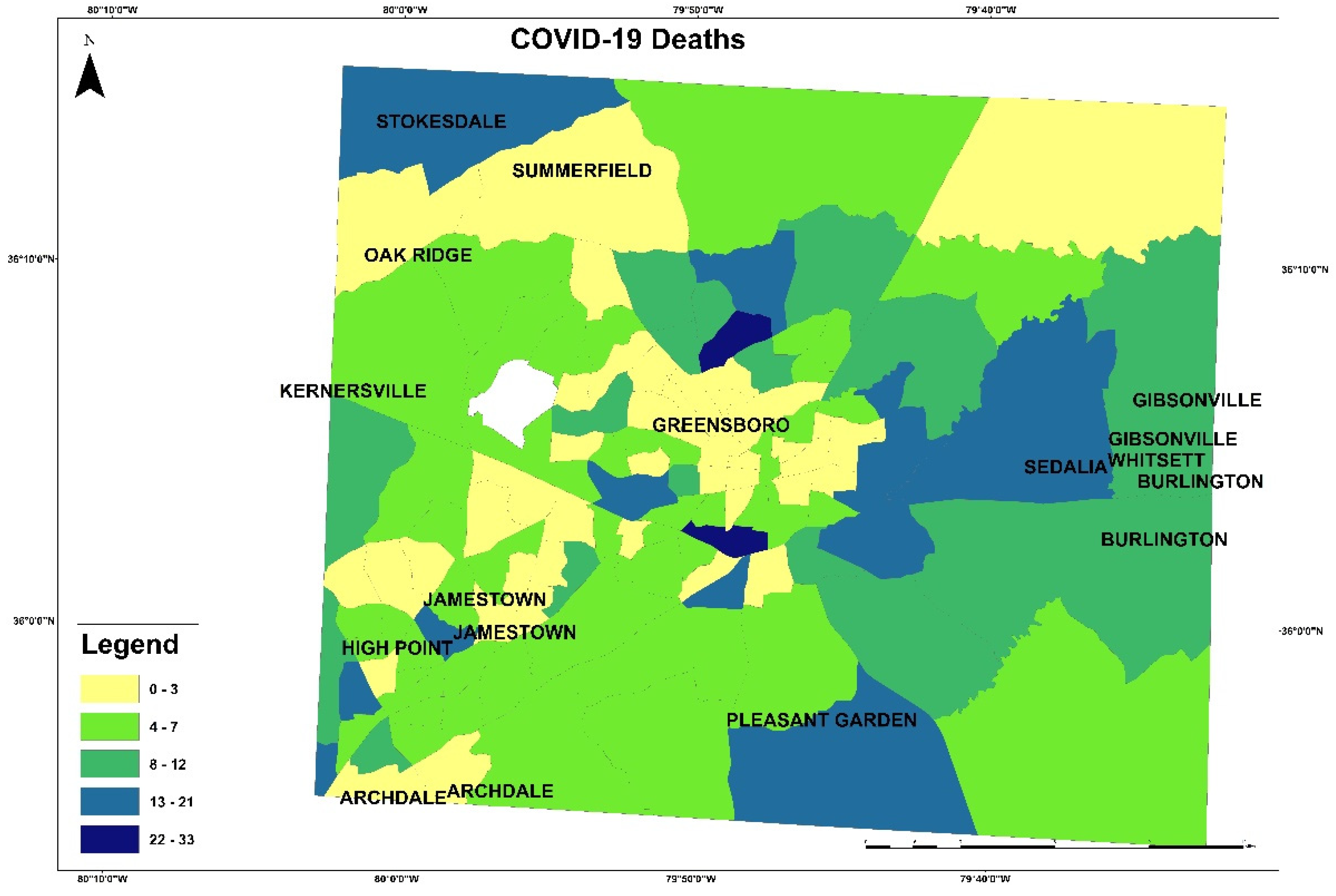
3. Study Area and Materials
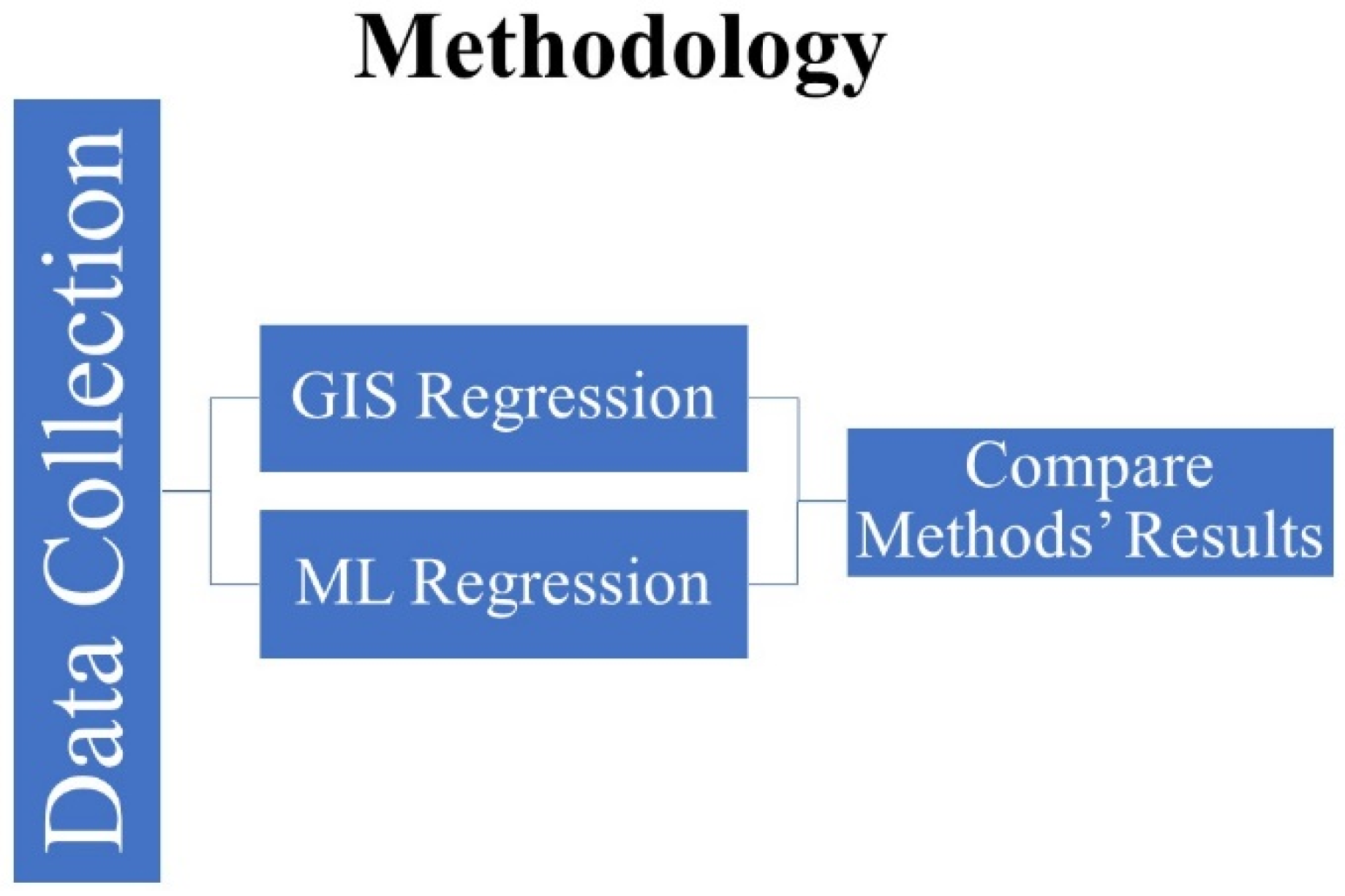
4. Methods and Results
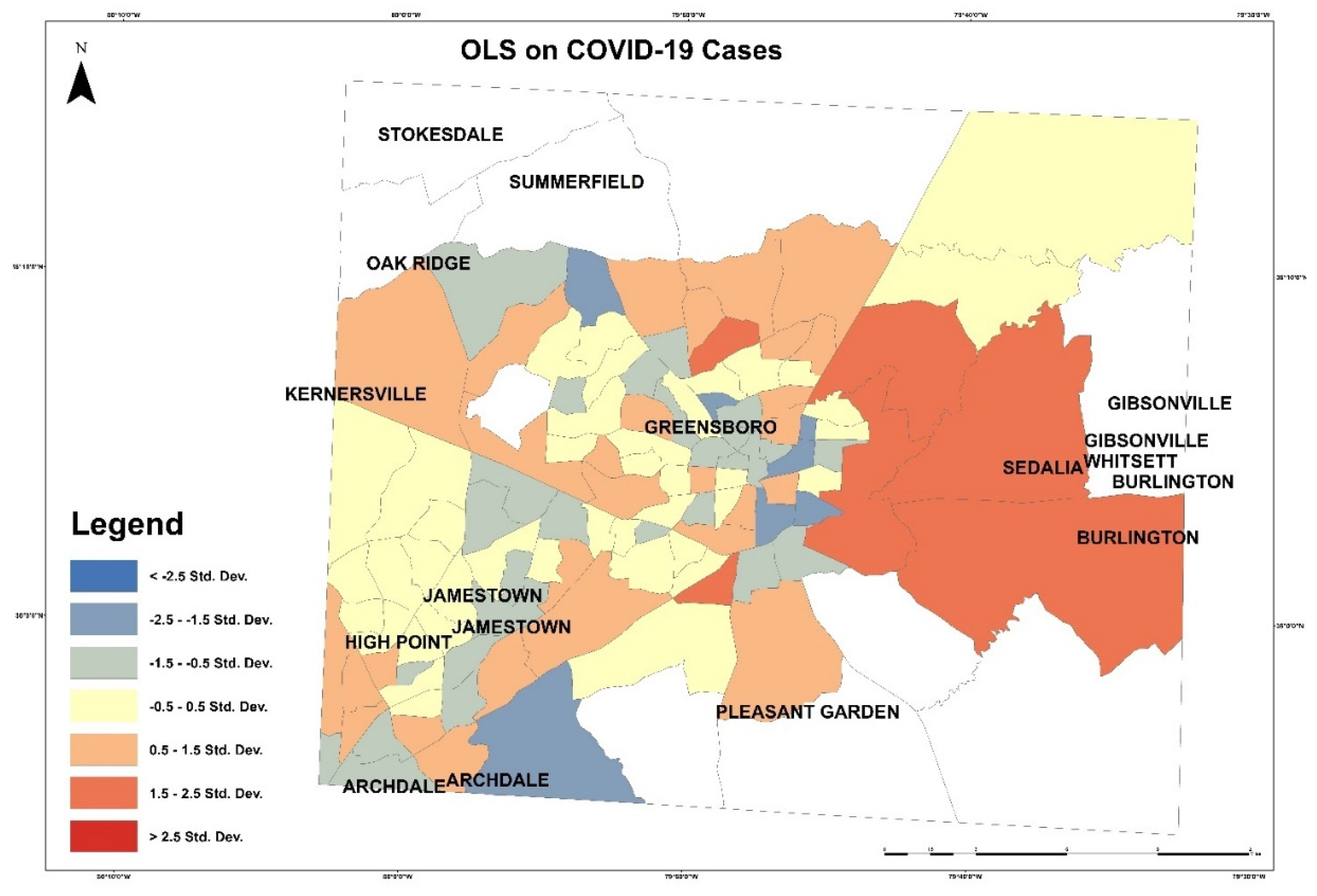
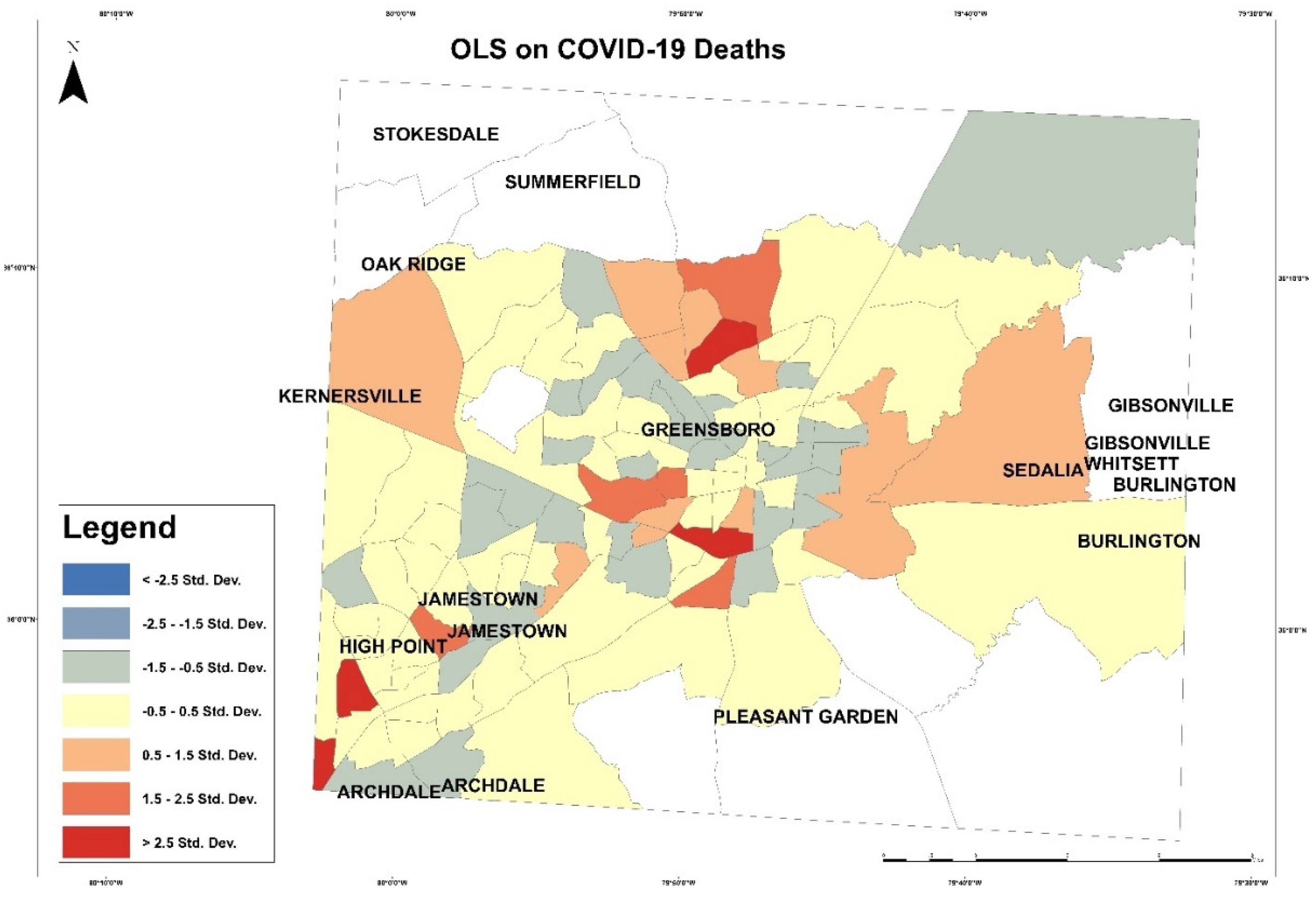
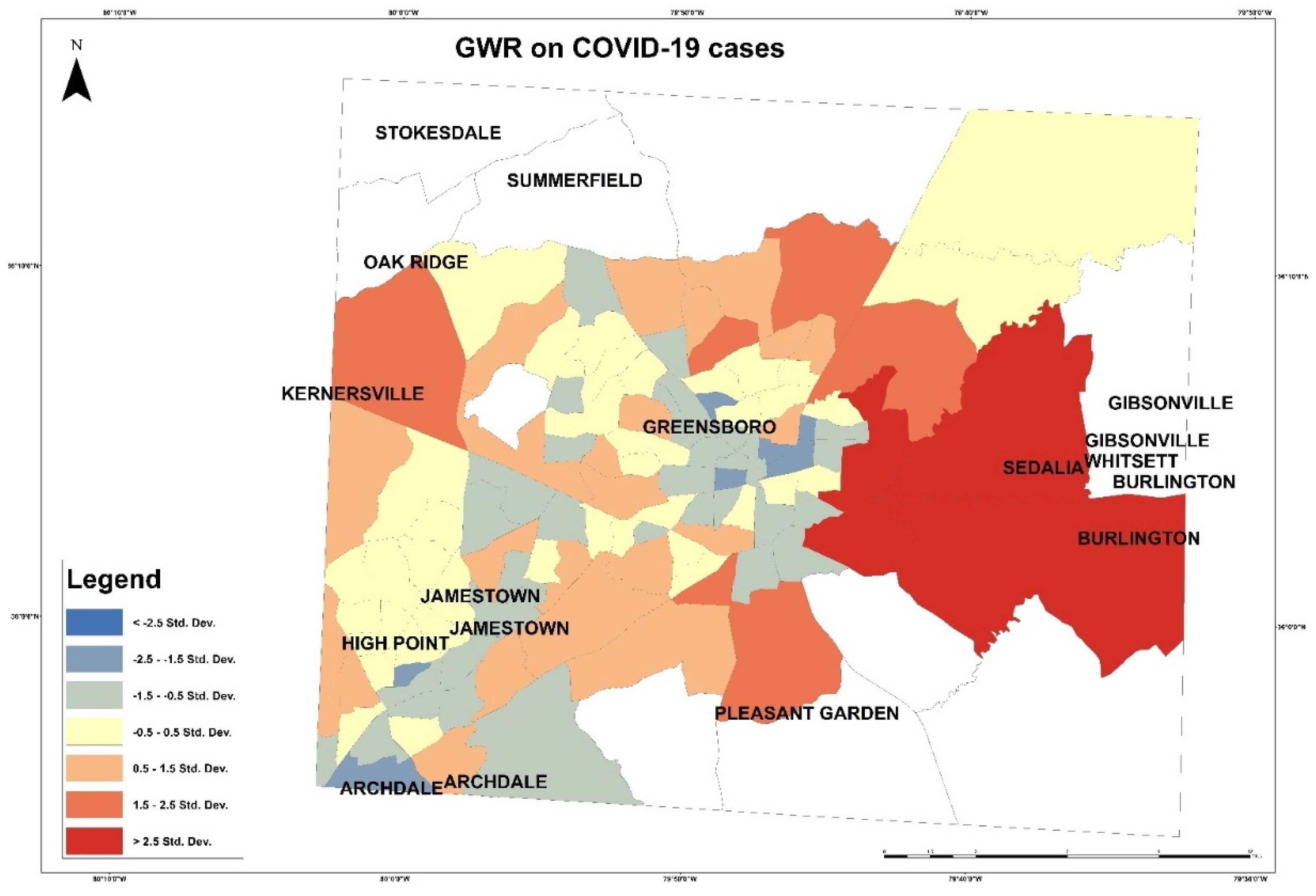
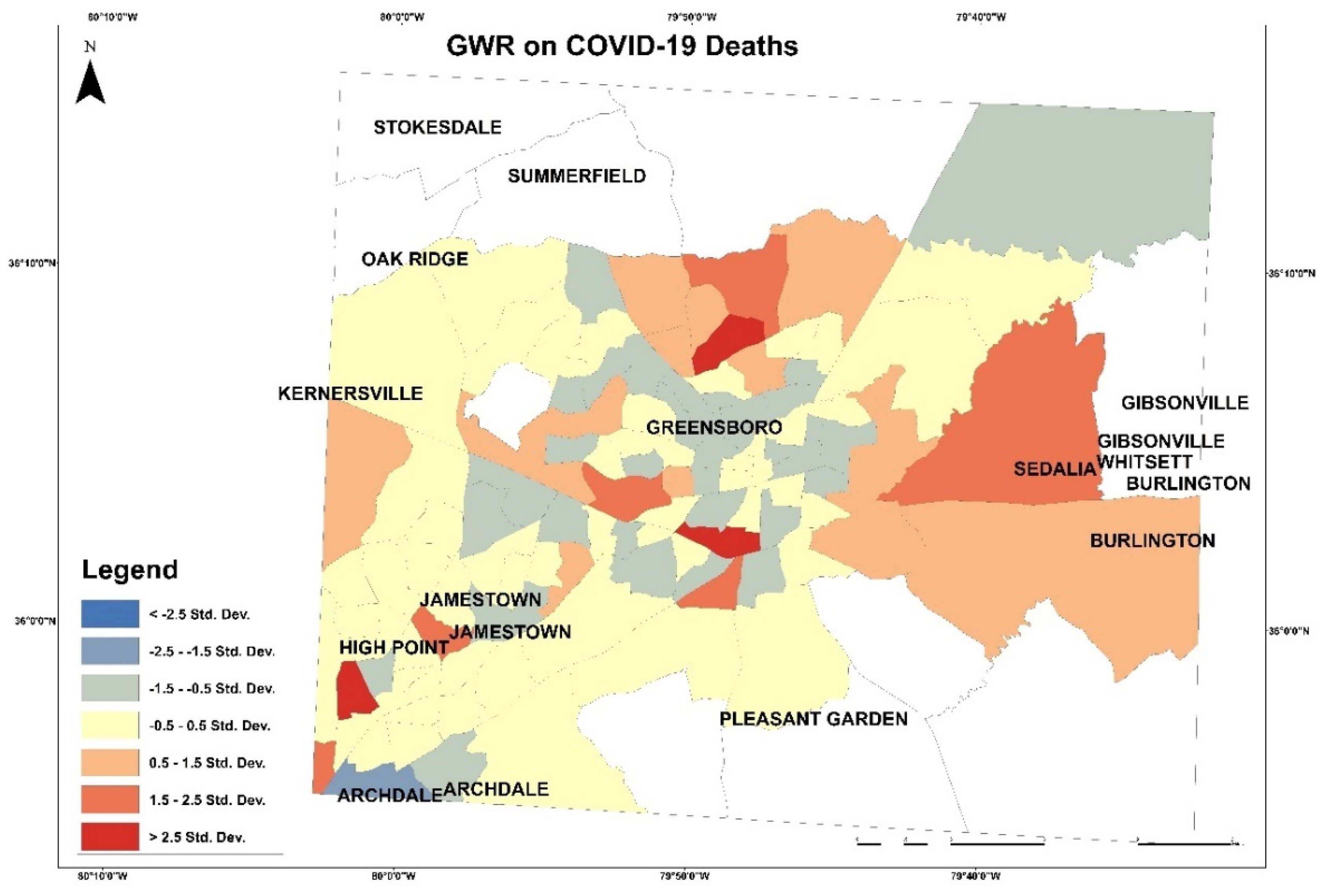
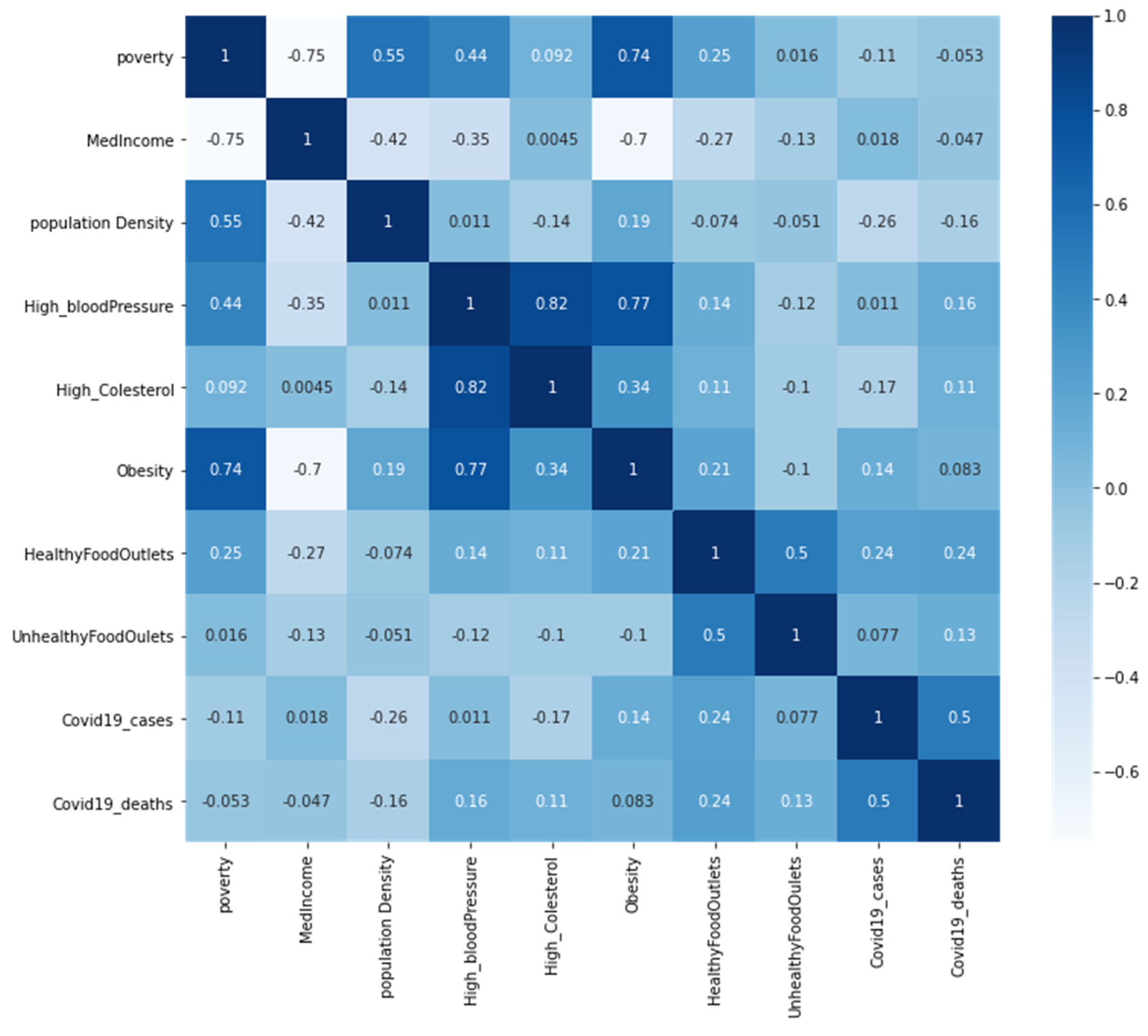
4.1. GIS Methods
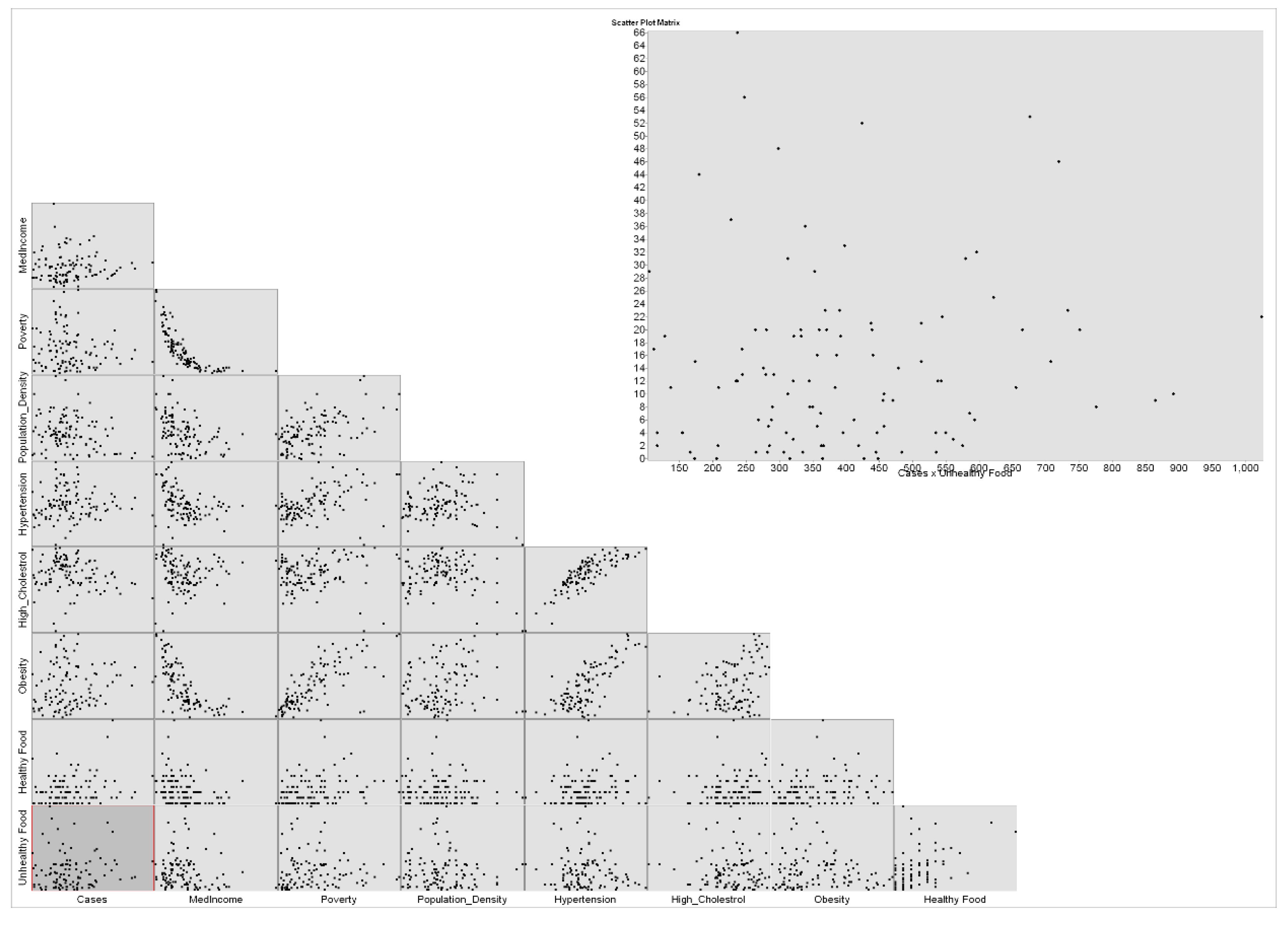
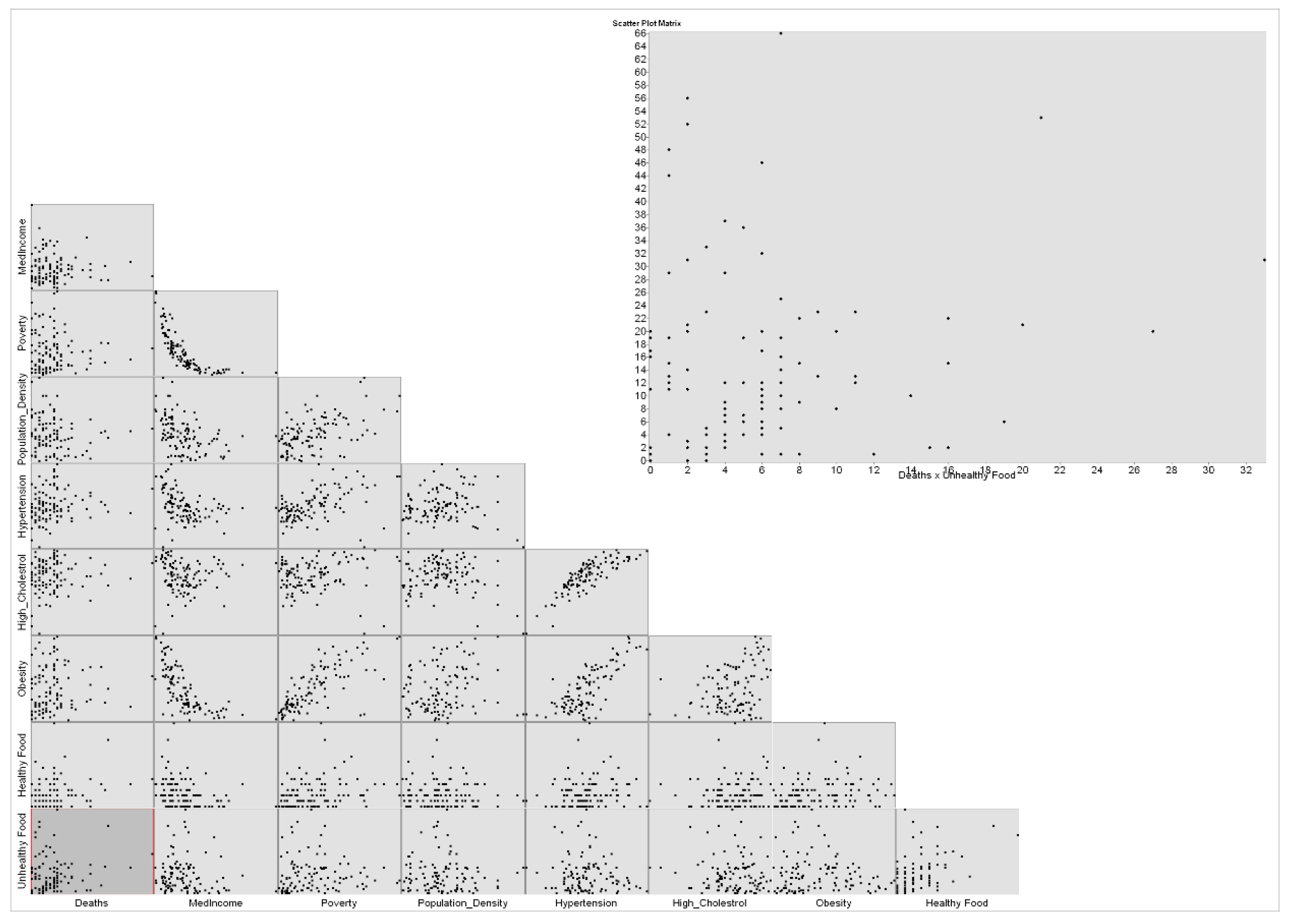
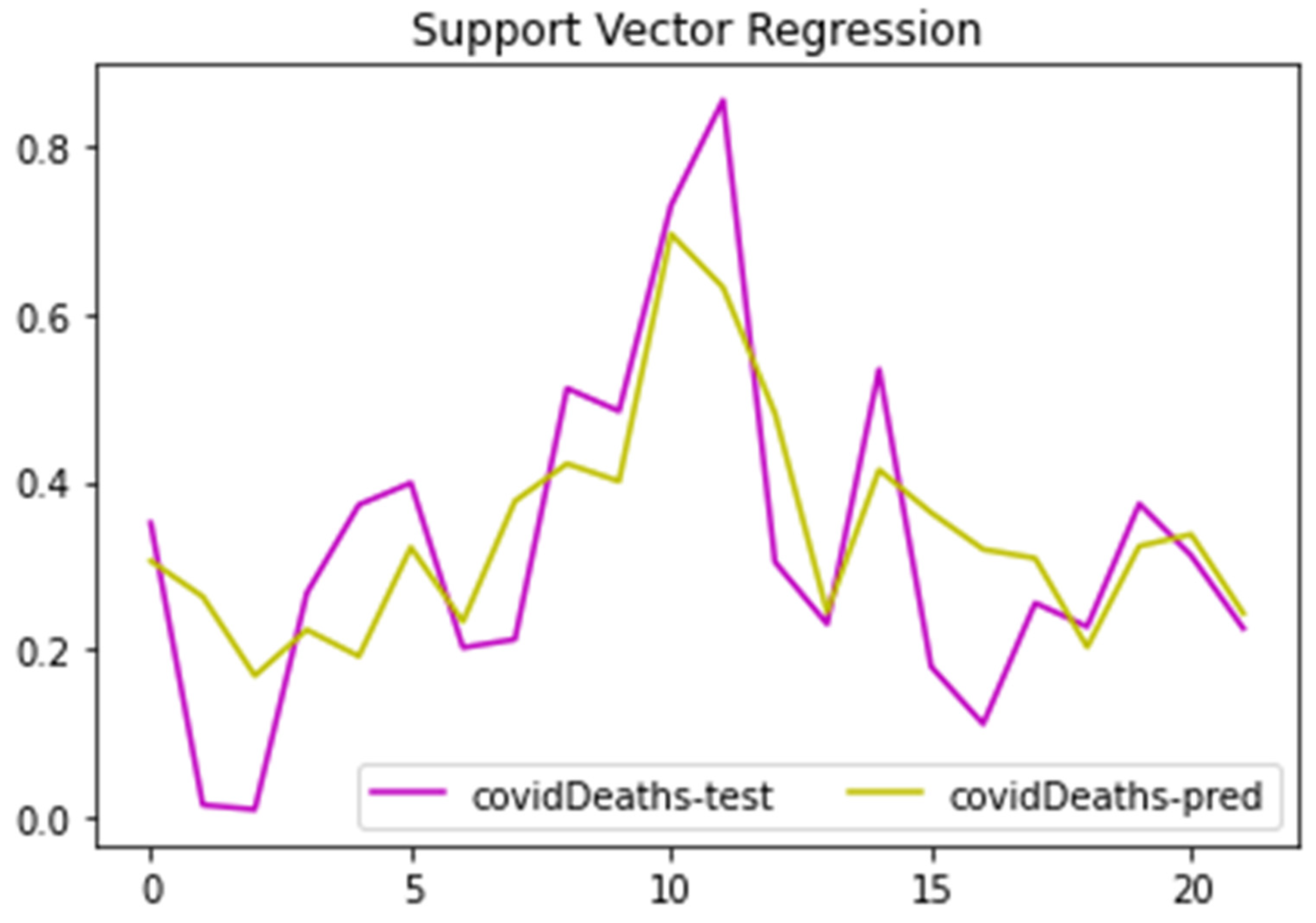
4.2. ML Regression Results and Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Potter, C.W. A history of influenza. J. Appl. Microbiol. 2001, 91, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surgery 2020, 76, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Yan, C.; Fu, Q.; Xiao, K.; Yu, Y.; Han, D.; Wang, W.; Cheng, J. Possible environmental effects on the spread of COVID-19 in China. Sci. Total Environ. 2020, 731, 139211. [Google Scholar] [CrossRef] [PubMed]
- “COVID Data Tracker”. Centers for Disease Control And Prevention, 2021. Available online: https://covid.cdc.gov/covid-data-tracker/?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fcases-updates%2Fcases-in-us.html#cases_casesper100klast7days (accessed on 1 December 2021).
- Bo, W.; Ahmad, Z.; Alanzi, A.R.; Al-Omari, A.I.; Hafez, E.; Abdelwahab, S.F. The current COVID-19 pandemic in China: An overview and corona data analysis. Alex. Eng. J. 2021, 61, 1369–1381. [Google Scholar] [CrossRef]
- Pan, L.; Wang, J.; Wang, X.; Ji, J.S.; Ye, D.; Shen, J.; Li, L.; Liu, H.; Zhang, L.; Shi, X.; et al. Prevention and control of coronavirus disease 2019 (COVID-19) in public places. Environ. Pollut. 2021, 292, 118273. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. CDC COVID-19 Global Response. 2022. Available online: https://www.cdc.gov/ (accessed on 23 January 2022).
- Donde, O.O.; Atoni, E.; Muia, A.W.; Yillia, P.T. COVID-19 pandemic: Water, sanitation and hygiene (WASH) as a critical control measure remains a major challenge in low-income countries. Water Res. 2021, 191, 116793. [Google Scholar] [CrossRef] [PubMed]
- Almalki, A.; Gokaraju, B.; Mehta, N.; Doss, D.A. Geospatial and Machine Learning Regression Techniques for Analyzing Food Access Impact on Health Issues in Sustainable Communities. ISPRS Int. J. Geo-Information 2021, 10, 745. [Google Scholar] [CrossRef]
- Gil, R.M.; Marcelin, J.R.; Zuniga-Blanco, B.; Marquez, C.; Mathew, T.; A Piggott, D. COVID-19 Pandemic: Disparate Health Impact on the Hispanic/Latinx Population in the United States. J. Infect. Dis. 2020, 222, 1592–1595. [Google Scholar] [CrossRef]
- Malik, A.; Abdalla, R. Mapping the impact of air travelers on the pandemic spread of (H1N1) influenza. Model. Earth Syst. Environ. 2016, 2, 1–15. [Google Scholar] [CrossRef]
- Lee, S.S.; Wong, N.S. The clustering and transmission dynamics of pandemic influenza A (H1N1) 2009 cases in Hong Kong. J. Infect. 2011, 63, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Maier, E.H.; Lopez, R.; Sanchez, N.; Ng, S.; Gresh, L.; Ojeda, S.; Burger-Calderon, R.; Kuan, G.; Harris, E.; Balmaseda, A.; et al. Obesity Increases the Duration of Influenza A Virus Shedding in Adults. J. Infect. Dis. 2018, 218, 1378–1382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sarmadi, M.; Ahmadi-Soleimani, S.M.; Fararouei, M.; Dianatinasab, M. COVID-19, body mass index and cholesterol: An ecological study using global data. BMC Public Heal. 2021, 21, 1–14. [Google Scholar] [CrossRef]
- Priyadarshini, I.; Mohanty, P.; Kumar, R.; Son, L.H.; Chau, H.T.M.; Nhu, V.-H.; Ngo, P.T.T.; Bui, D.T. Analysis of Outbreak and Global Impacts of the COVID-19. Health 2020, 8, 148. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, A.; Kumar, M.; Magotra, R. Role of GIS in Managing COVID-19; NISCAIR-CSIR: New Delhi, India, 2020. [Google Scholar]
- Franch-Pardo, I.; Napoletano, B.M.; Rosete-Verges, F.; Billa, L. Spatial analysis and GIS in the study of COVID-19. A review. Sci. Total Environ. 2020, 739, 140033. [Google Scholar] [CrossRef]
- Ahasan, R.; Hossain, M.M. Leveraging GIS Technologies for Informed Decision-making in COVID-19 Pandemic. SocArXiv 2020, preprint. [Google Scholar]
- Boulos, M.N.K.; Geraghty, E.M. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: How 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int. J. Health Geogr. 2020, 19, 1–12. [Google Scholar]
- Ardabili, S.; Mosavi, A.; Ghamisi, P.; Ferdinand, F.; Varkonyi-Koczy, A.; Reuter, U.; Rabczuk, T.; Atkinson, P. COVID-19 Outbreak Prediction with Machine Learning. Algorithms 2020, 13, 249. [Google Scholar] [CrossRef]
- Rezaei, M.; Nouri, A.A.; Park, G.S.; Kim, D.H. Application of Geographic Information System in Monitoring and Detecting the COVID-19 Outbreak. Iran. J. Public Heal. 2020, 49, 114–116. [Google Scholar] [CrossRef] [PubMed]
- Rosenkrantz, L.; Schuurman, N.; Bell, N.; Amram, O. The need for GIScience in mapping COVID-19. Heal. Place 2020, 67, 102389. [Google Scholar] [CrossRef] [PubMed]
- Mollalo, A.; Vahedi, B.; Rivera, K.M. GIS-based spatial modeling of COVID-19 incidence rate in the continental United States. Sci. Total Environ. 2020, 728, 138884. [Google Scholar] [CrossRef] [PubMed]
- Küchenhoff, H.; Günther, F.; Höhle, M.; Bender, A. Analysis of the early COVID-19 epidemic curve in Germany by regression models with change points. Epidemiol. Infect. 2021, 149, e68. [Google Scholar] [CrossRef] [PubMed]
- Radenkovic, D.; Chawla, S.; Pirro, M.; Sahebkar, A.; Banach, M. Cholesterol in Relation to COVID-19: Should We Care about It? J. Clin. Med. 2020, 9, 1909. [Google Scholar] [CrossRef] [PubMed]
- Vicenzi, M.; Di Cosola, R.; Ruscica, M.; Ratti, A.; Rota, I.; Rota, F.; Bollati, V.; Aliberti, S.; Blasi, F. The liaison between respiratory failure and high blood pressure: Evidence from COVID-19 patients. Eur. Respir. J. 2020, 56, 2001157. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Gale, C.R.; Kivimäki, M.; Batty, G.D. Overweight, obesity, and risk of hospitalization for COVID-19: A community-based cohort study of adults in the United Kingdom. Proc. Natl. Acad. Sci. USA 2020, 117, 21011–21013. [Google Scholar] [CrossRef]
- Caillon, A.; Zhao, K.; Klein, K.O.; Greenwood, C.M.T.; Lu, Z.; Paradis, P.; Schiffrin, E.L. High Systolic Blood Pressure at Hospital Admission Is an Important Risk Factor in Models Predicting Outcome of COVID-19 Patients. Am. J. Hypertens. 2021, 34, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.; Zhang, J.; Liu, L.; Yuan, X.; Zang, X.; Lu, F.; He, P.; Wang, Q.; Zhang, X.; Xu, Y.; et al. High-density lipoprotein cholesterol as a factor affecting virus clearance in covid-19 patients. Respir. Med. 2020, 175, 106218. [Google Scholar] [CrossRef] [PubMed]
- Bhadra, A.; Mukherjee, A.; Sarkar, K. Impact of population density on Covid-19 infected and mortality rate in India. Model. Earth Syst. Environ. 2021, 7, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.; Li, W.; Zhang, C.; Chen, X. The disguised pandemic: The importance of data normalization in COVID-19 web mapping. Public Heal. 2020, 183, 36–37. [Google Scholar] [CrossRef]
- Shakeel, S.; Hassali, M.A.A.; Naqvi, A.A. Health and Economic Impact of COVID-19: Mapping the Consequences of a Pandemic in Malaysia. Malays. J. Med Sci. 2020, 27, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Baena-Díez, J.M.; Barroso, M.; Cordeiro-Coelho, S.I.; Díaz, J.L.; Grau, M. Impact of COVID-19 outbreak by income: Hitting hardest the most deprived. J. Public Heal. 2020, 42, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Kansiime, M.K.; Tambo, J.A.; Mugambi, I.; Bundi, M.; Kara, A.; Owuor, C. COVID-19 implications on household income and food security in Kenya and Uganda: Findings from a rapid assessment. World Dev. 2021, 137, 105199. [Google Scholar] [CrossRef]
- Jay, J.; Bor, J.; Nsoesie, E.O.; Lipson, S.K.; Jones, D.K.; Galea, S.; Raifman, J. Neighbourhood income and physical distancing during the COVID-19 pandemic in the United States. Nat. Hum. Behav. 2020, 4, 1294–1302. [Google Scholar] [CrossRef]
- Gundersen, C.; Hake, M.; Dewey, A.; Engelhard, E. Food insecurity during COVID-19. Appl. Econ. Perspect. Policy 2021, 43, 153–161. [Google Scholar] [CrossRef]
- Ahn, S.; Norwood, F.B. Measuring Food Insecurity during the COVID-19 Pandemic of Spring 2020. Appl. Econ. Perspect. Policy 2021, 43, 162–168. [Google Scholar] [CrossRef]
- Nakada, L.Y.K.; Urban, R.C. COVID-19 pandemic: Environmental and social factors influencing the spread of SARS-CoV-2 in São Paulo, Brazil. Environ. Sci. Pollut. Res. 2021, 28, 40322–40328. [Google Scholar] [CrossRef] [PubMed]
- Arif, M.; Sengupta, S. Nexus between population density and novel coronavirus (COVID-19) pandemic in the south Indian states: A geo-statistical approach. Environ. Dev. Sustain. 2021, 23, 10246–10274. [Google Scholar] [CrossRef] [PubMed]
- Budhwani, K.I.; Budhwani, H.; Podbielski, B. Evaluating Population Density as a Parameter for Optimizing COVID-19 Testing: Statistical Analysis. Jmirx Med. 2021, 2, e22195. [Google Scholar] [CrossRef] [PubMed]
- Gaskin, D.J.; Zare, H.; Delarmente, B.A. Geographic disparities in COVID-19 infections and deaths: The role of transportation. Transp. Policy 2021, 102, 35–46. [Google Scholar] [CrossRef]
- Kang, D.; Choi, H.; Kim, J.-H.; Choi, J. Spatial epidemic dynamics of the COVID-19 outbreak in China. Int. J. Infect. Dis. 2020, 94, 96–102. [Google Scholar] [CrossRef]
- Kullar, R.; Marcelin, J.R.; Swartz, T.H.; Piggott, D.A.; Macias Gil, R.; Mathew, T.A.; Tan, T. Racial disparity of Coronavirus Disease 2019 in African American communities. J. Infect. Dis. 2020, 222, 890–893. [Google Scholar] [CrossRef] [PubMed]
- U.S. Census Bureau QuickFacts: Guilford County, North Carolina. 2020. Available online: http://www.census.gov/quickfacts/guilfordcountynorthcarolina (accessed on 18 August 2020).
- How will North Carolina’s Face Mask Requirement be Enforced? 2020. Available online: https://www.wcnc.com/article/news/health/coronavirus/how-will-north-carolina-mask-mandate-be-enforced/275-03964fa3-2c39-4c2c-a2e8-44d17d5a0cfa (accessed on 18 August 2020).
- Our County|Guilford County, NC. 2020. Available online: https://www.guilfordcountync.gov/our-county (accessed on 17 August 2020).
- Guilford County’s Zip Codes with Highest Number of COVID-19 Cases. 2020. Available online: https://myfox8.com/news/coronavirus/guilford-countys-zip-codes-with-highest-number-of-covid-19-cases/ (accessed on 17 August 2020).
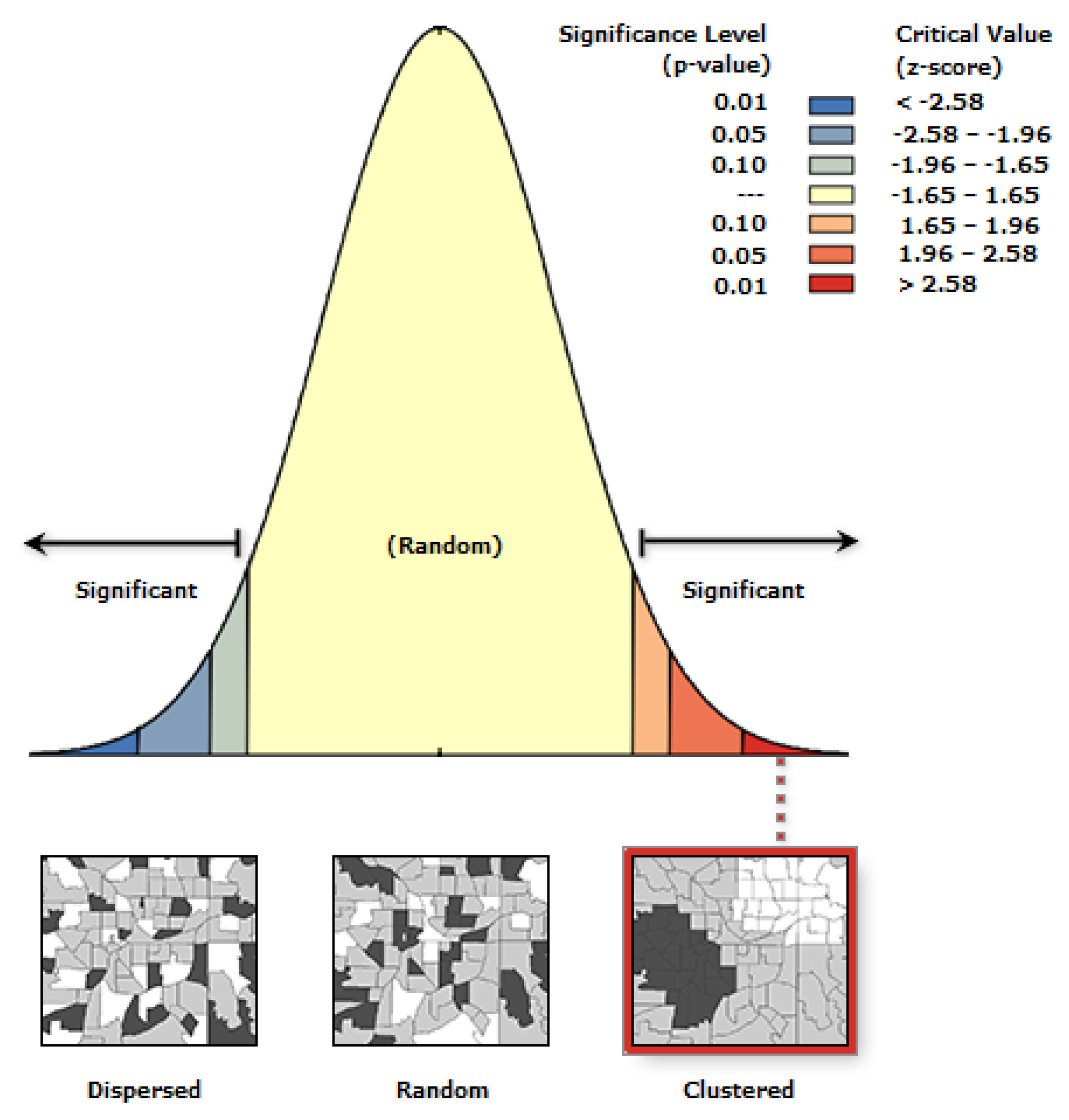
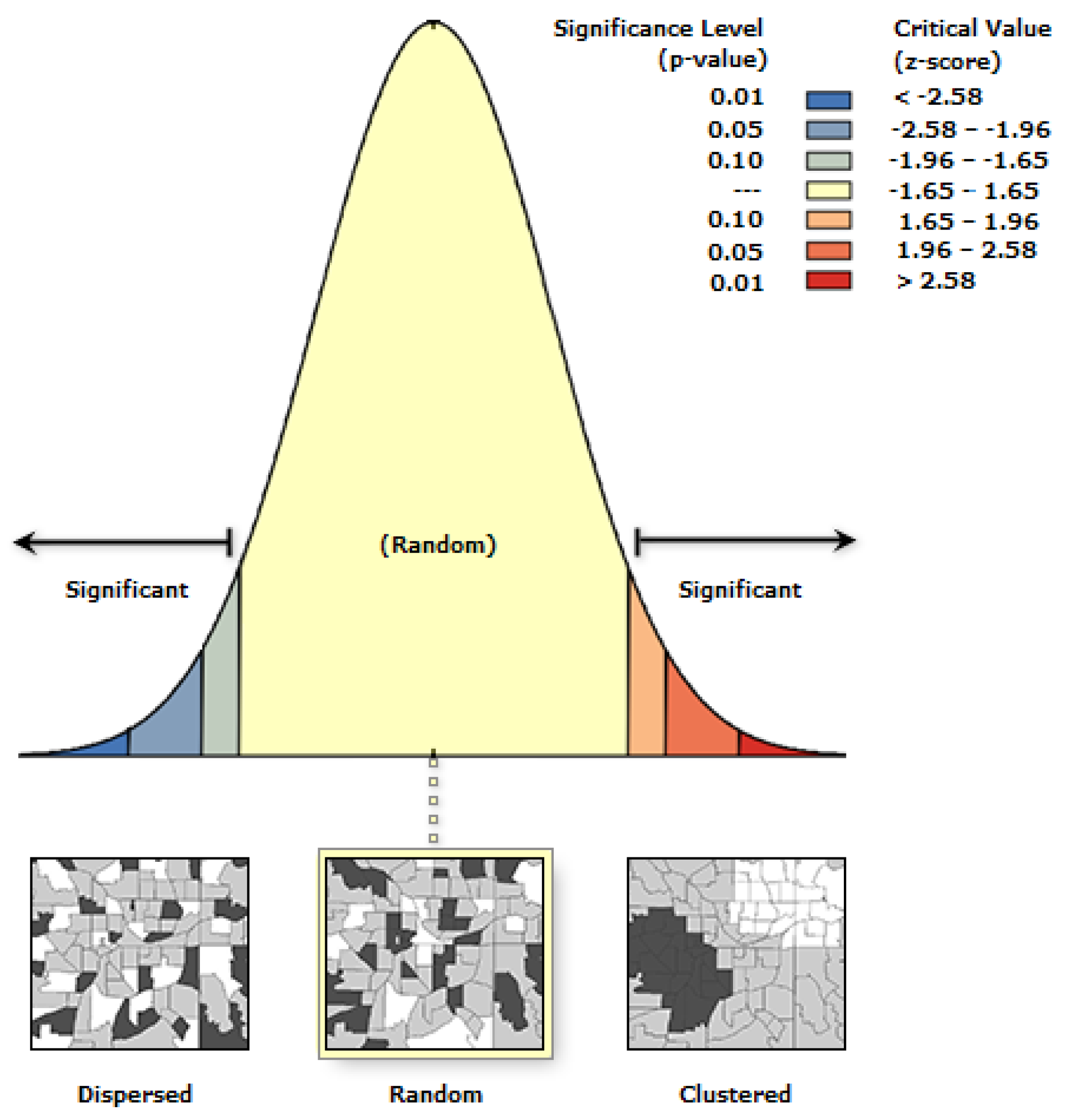
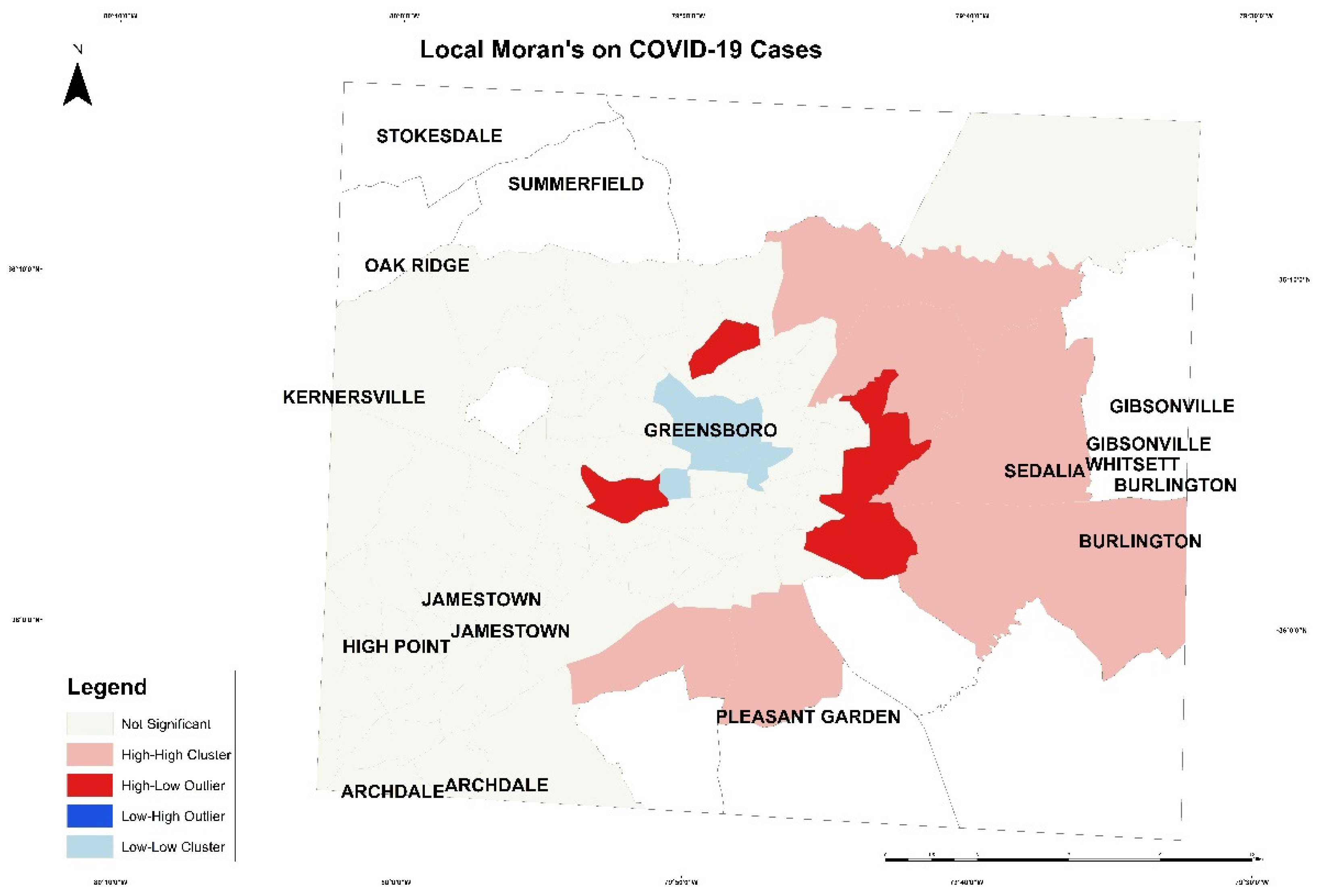
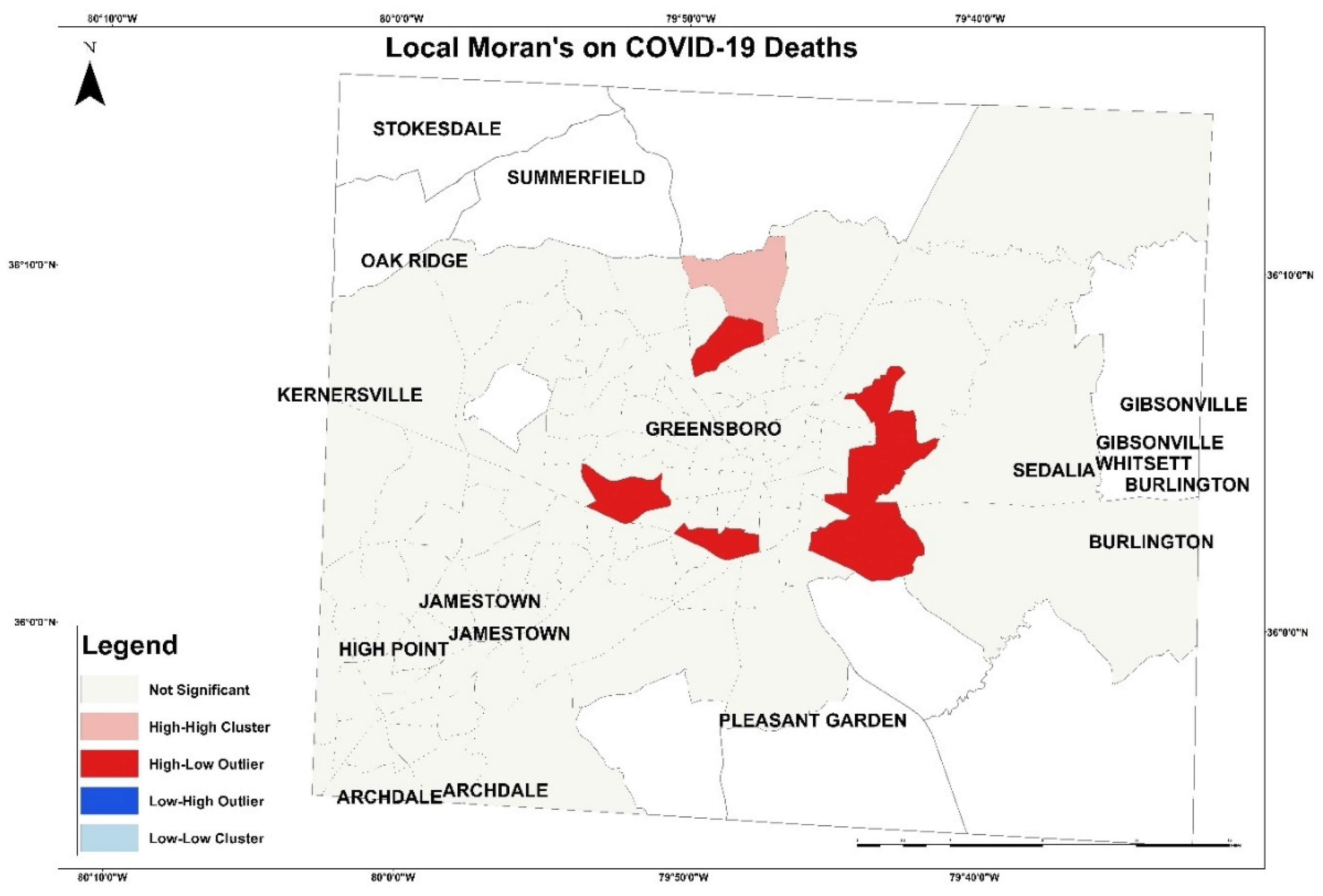
| Measures | COVID-19 Cases | COVID-19 Deaths |
|---|---|---|
| Moran’s Index | 0.118617 | 0.005965 |
| Expected Index | −0.009259 | −0.009259 |
| Variance | 0.000575 | 0.000551 |
| Z-score | 5.3314423 | 6.48788 |
| p-value | 0.000000 | 0.516475 |
| Model | Parameters |
|---|---|
| Linear Regression Model | copy_X = True,fit_intercept = True,n_jobs = None,normalize = False. |
| Random Forest Regression Model | bootstrap = True,ccp_alpha = 0.0,critrion = ‘mse’,max_depth = None,max_features = ‘ato’,max_leaf_nodes = None,max_saples = None,min_impurity_decrease = 0.0,min_imprity_split = None,min_samples_leaf = 1,min_samples_split = 2,min_weight_fraction_leaf = 0.0,n_estimtors = 100,n_jobs = None,oob_score = False,random_state = None,verbose = 0, warm_start = False) |
| K-Nearest Neighbor Regression Model | lgorithm’:’auto’,’leaf_size’:30,’metric’:’minkowski’,’metric_params’: None, ‘n_jobs’: None,’n_neighbors’: 5, ‘p’: 2, ‘weights’: ‘uniform’ |
| Root Mean Square Error | ||
|---|---|---|
| Models | CVID-19 Cases | COVID-19 Deaths |
| Linear regression for multioutput Regression | 0.146 | 0.141 |
| K-nearest neighbors for multioutput regression | 0.208 | 0.147 |
| Random forest for multioutput regression | 0.186 | 0.175 |
| Support Vector Regression | 0.168 | 0.127 |
| Correlation Coefficient | ||
|---|---|---|
| Models | CVID-19 Cases | COVID-19 Deaths |
| Linear regression for multioutput regression | 0.446 | 0.508 |
| K-nearest neighbors for multioutput regression | −0.085 | 0.466 |
| Random forest for multioutput regression | 0.137 | 0.239 |
| Support Vector Regression | 0.290 | 0.601 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almalki, A.; Gokaraju, B.; Acquaah, Y.; Turlapaty, A. Regression Analysis for COVID-19 Infections and Deaths Based on Food Access and Health Issues. Healthcare 2022, 10, 324. https://doi.org/10.3390/healthcare10020324
Almalki A, Gokaraju B, Acquaah Y, Turlapaty A. Regression Analysis for COVID-19 Infections and Deaths Based on Food Access and Health Issues. Healthcare. 2022; 10(2):324. https://doi.org/10.3390/healthcare10020324
Chicago/Turabian StyleAlmalki, Abrar, Balakrishna Gokaraju, Yaa Acquaah, and Anish Turlapaty. 2022. "Regression Analysis for COVID-19 Infections and Deaths Based on Food Access and Health Issues" Healthcare 10, no. 2: 324. https://doi.org/10.3390/healthcare10020324
APA StyleAlmalki, A., Gokaraju, B., Acquaah, Y., & Turlapaty, A. (2022). Regression Analysis for COVID-19 Infections and Deaths Based on Food Access and Health Issues. Healthcare, 10(2), 324. https://doi.org/10.3390/healthcare10020324






