Abstract
Background: The Place Model was developed in order to conceptualize the various roles and career pathways of the teaching profession. It can be used to evaluate long-term professional career trajectories and to encourage the student-teacher to visualize their future personal and professional development. Methods: In the present study, the Place Model has been applied to the Optometric profession. The four categories of the place model have been discussed in terms of Optometry and a survey of undergraduate Optometrists highlights the perception of the model amongst pre-qualified professionals. Results: The majority of participants placed qualified optometrists in the Professional area on the Place Model (87%, n = 88) with the remainder placing qualified optometrists in the De-Professional area on the Place Model (13%, n = 13). There was no statistically significant difference between responses from male and female participants (t-test, p = 0.38). There was also no statistically significant difference between responses from participants in year 1, 2 or 3 of their undergraduate program (one-way analysis of variance [ANOVA], p = 0.10). Conclusion: The Place Model may be an opportunity to discuss with Optometry students their future career pathways and to ensure that we maintain a highly skilled and caring profession that provides high quality eyecare for the public.
1. Introduction
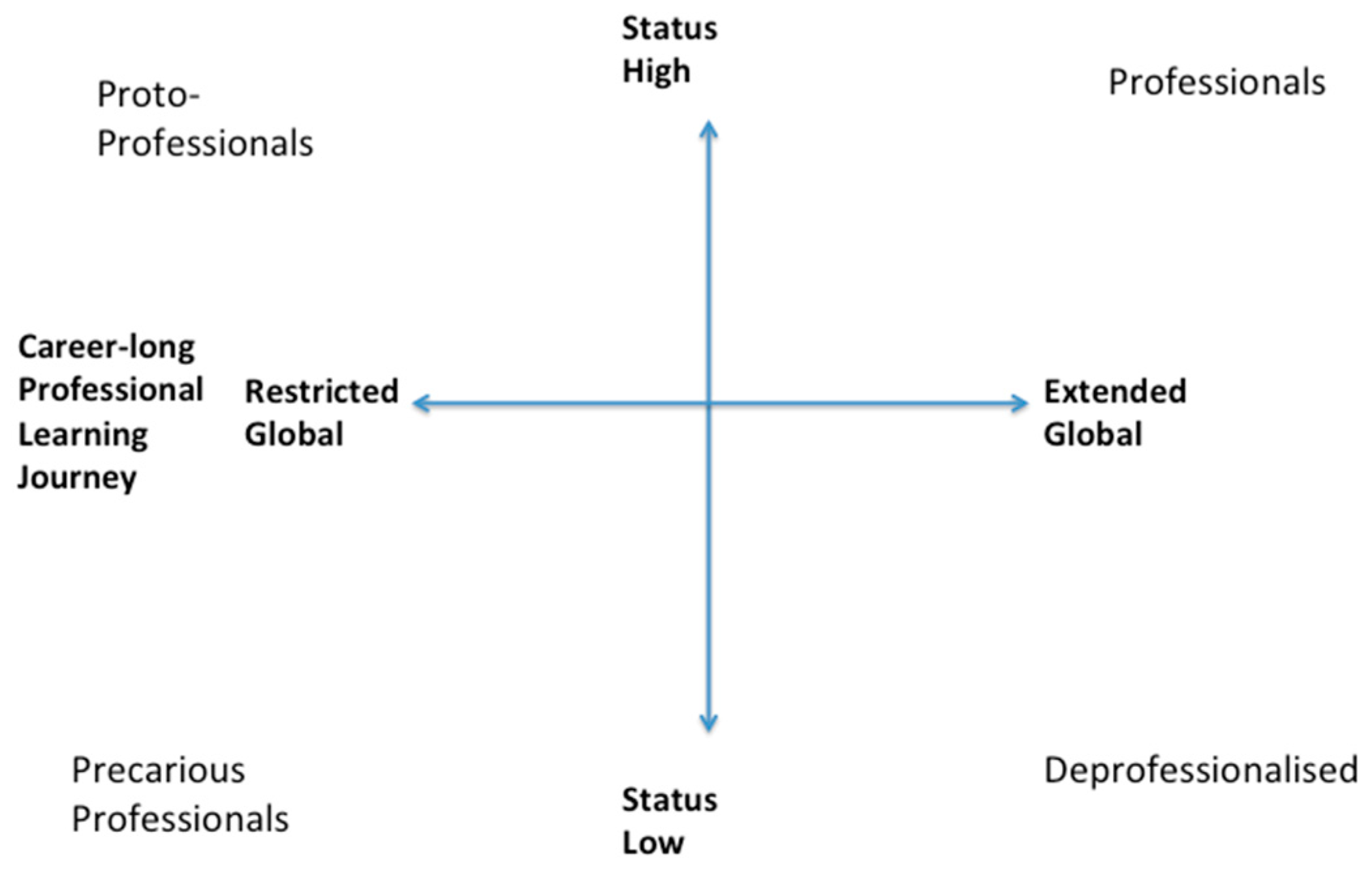
The Place Model was developed in order to conceptualize the various roles and career pathways in the teaching profession [1]. It can be used to demonstrate how the user can consider long-term professional career trajectories and to encourage the student-teacher to visualize their future personal and professional development. It classifies the place of teachers in respect of (place as) esteem and (place on a) learning journey.
In the present study, the Place Model has been applied to the Optometric profession. The five categories of the place model will be discussed in terms of Optometry and a survey of undergraduate Optometrists highlights the perception of the model amongst pre-qualified professionals.
1.1. Proto-Professional
The prefix ‘proto’ derived from the Greek word ‘protos’ meaning first, suggests that this may be applied to professionals in the early part of their career journey. Considering the application of this term to the Optometrist, it may be considered that pre-registration and newly qualified Optometrists are considered proto-professionals.
In the UK, pre-registration Optometrists are those who have completed an undergraduate Optometry qualification at the honors degree level and are working in a practice or hospital under the supervision of a qualified Optometrist during their ‘Scheme for Registration’, administered by The College of Optometrists. They are required to complete a period in practice, examining and dispensing a specified number of patients during this period. Following this time, which is typically a one-year period, they are required to undertake a series of assessments, or Objective Structured Clinical Examinations (OSCEs). These OSCEs represent Stage 2 of the qualification, with Stage 1 being the completion of the degree level qualification. In addition to the Stage 1 and 2 qualifications, Optometrists are also required to achieve clinical competency in a number of areas at both these time points and in addition, have observed assessments during the course of the pre-registration period.
Pre-registration Optometrists work full-time while studying for their final professional qualifications. There are limited data describing the perceptions of pre-registration Optometrists, however, Parkins, et al. [2] suggested that newly qualified Optometrists are more likely to generate a higher number of referrals to the Hospital Eye Service than more experienced practitioners. This study revealed that two newly qualified Optometrists generated 12.5% of the total number of referrals in the audit. The study suggested that pre-registration Optometrists referred more appropriately than newly qualified Optometrists, but this is perhaps due to the fact that pre-registration Optometrists are supervised closely and any referrals will be signed off by the supervisor.
The General Optical Council (GOC), the regulatory body for Optometrists, published a discussion paper on ‘Professional boundaries and service needs in eye health services’ and recognized that there may be specific areas of training required for newly qualified Optometrists to ensure ‘registrants are equipped to practice safely across the UK in accordance with professional standards’ [3].
Howell-Duffy, et al. [4] also agreed that experience influences management and prescribing decisions made by Optometrists. Newly qualified Optometrists were more likely to prescribe full spectacle corrections while older and more experienced optometrists more likely to ‘prescribe a partial correction’. This was three times more likely for Optometrists with a career of at least 40 years. Reasons for this included more experience with patient’s intolerance to spectacle prescriptions.
Often, Optometrist’s duties may be delegated to other optical staff including dispensing opticians and optical assistants. Dispensing opticians are a separate professional group, educated to either diploma or degree level who work with Optometrists to ensure that patients have an appropriate choice of spectacle frame and lenses. These delegated duties may include dispensing and pre-screening which involves obtaining measurements prior to the actual eye examination to inform the Optometrists’ clinical management decisions (e.g., measurements of intraocular pressure or visual field assessments). Post eye examination screening may also take place following recommendations for further tests by the Optometrist (e.g., measurements of retinal thickness during optical coherence tomography). These roles may be considered proto-professional in the context of the Optometry practice. Delegation of duties is often viewed as a minefield and leaves the Optometrist exposed to legal ramifications. Delegation is discussed in detail as part of the Professional Guidance from The College of Optometrists [5]. The guidance states that when you delegate duties you are still responsible for the overall management of the patient and the work of the person to whom you have delegated. Recently, Optometrist Honey Rose was convicted of manslaughter after a missed diagnosis of papilledema, or optic disc swelling in an eight-year-old boy who later died [6]. Although the photographs of the child’s optic discs were available at the trial there was a query regarding whether the Optometrist had actually seen these on the day the patient attended. This highlights how the delegation of roles can put both the patients and the professionals at risk of adverse outcomes. This conviction has since been overturned, however, the case has prompted Optometrists to seek additional training and advice from professional bodies regarding this medical condition.
1.2. No Optometrists
Whilst strictly outside the Place Model, millions of people across the world have limited access to eye care. Globally, 36 million people are blind with over 200 million having a moderate or severe visual impairment, however, more than 75% of all vision loss is avoidable [7]. In 2012, the World Health Organisation stated that governments could add millions of dollars to the global economy by investing in eye examinations and the provision of glasses for 700 million people worldwide [7]. The study estimated that 65,000 more Optometrists, Ophthalmologists, Optical Dispensers and other eye care professionals would be required to provide these services and that a cost of approximately 25,000 million to set up and run would be returned 10 fold by providing much needed eye care services. Investing in eye care demonstrated a 22% productivity increase amongst tea plantation workers in India during a one-month period [8]. Investing in education for eye care has vast economic and health benefits for the community.
1.3. The De-Professionalised
According to the Place Model, the de-professional includes practitioners who have significant experience in their profession but have become demotivated and disengaged with their professional values and skills over time. The members of this quadrant may previously have been highly motivated and enthusiastic professionals but have been affected by their experiences in the workplace, which have left them cynical and uninspired by their role. The role of Optometrists has changed gradually over the previous generation with newer practitioners being more likely to work in large practices with multiple Optometrists rather than smaller community practices. In addition, the increase in the use of technology has been rapid over the previous 20 years with many practices now owing optical imaging technology, automated refractive technology and computerized patient record systems. Some practitioners may be unable or unwilling to invest in the technology which they may feel is unnecessary or prohibitively expensive which may perhaps present an image of not being up-to-date with modern practice.
Fortunately, Optometrists in the UK are required to enroll on a continual scheme of education and training which ensures that they engage with peers and Optometric educators on a regular basis. The scheme, administered by the regulatory body, the General Optical Council ensures that Optometrists must gain new or updated knowledge and skills across a broad range of different clinical areas. In addition to gaining a specific number of ‘CET (continuing education and training) points’ over a three year period, registrants are required to gain a certain number of points per year, some of which must be ‘interactive’. The interactive nature of this engagement ensures that practitioners have some level of engagement with others during the course of their work, preventing those practitioners working in more remote locations or in small practices from becoming isolated from any important developments in the field.
1.4. Precarious Professionals
The Place Model describes precarious professionals as those who may have low status and have not maintained professional development beyond their initial qualification. It also may include both transients and also unprofessionals.
This status may be due to many contributing factors, such as the inability to secure a permanent position, an unsupportive or inefficient workplace or a lack of enthusiasm for the profession. The precarious professional may also represent over-confident professionals who place their own professional judgements above guidelines and regulations. The Precarious Professional is at risk of being investigated for Fitness to Practice issues.
In the UK, the General Optical Council is the professional regulator for Optometrists, Dispensing Opticians and optical businesses [3]. One of the four key functions of the GOC is ‘investigating and acting where registrants’ fitness to practice, train or carry on business is impaired’. Fitness to practice complaints about GOC registrants can be received from members of the public, patients, carers, employers, the police and other GOC registrants. Fitness to practice issues may relate to one or more of the following factors:
- Poor professional performance;
- Physical or mental health problems affecting their work;
- Inappropriate behaviour;
- Being under the influence of alcohol or drugs at work;
- Fraud or dishonesty;
- A criminal conviction or caution;
- A finding by another regulatory body.
The precarious professional may find themselves the subject of a Fitness to Practice investigation if they do not maintain an adequate level of knowledge and skills.
1.5. Professionals
This area of the model outlines the ‘Ideal Optometrist’. In June 2015, the General Optical Council prepared a report on the public’s perception of the optical profession, based on a survey of 2250 adults from across the UK. The sample was designed to reflect a cross-section of the population across various ages and socio-economic grades. Findings suggested that overall confidence in and satisfaction with opticians (both Optometrists and Dispensing Opticians) is high.
In 2018, Irving, et al. [9] suggested that patient’s knowledge of eye care had notable gaps with the potential for these gaps to increase risk of vision loss due to late detection of ocular conditions. In recent years, Optometrists have been able to access further additional professional qualifications. In 2007, the Department of Health (UK) granted permission for Optometrists to train as Independent Prescribers. This qualification allows Optometrists to manage a wider range of patients than with the entry-level qualification providing patients with more accessible eye care. In addition to independent prescribing, in the past decade, a range of Professional Certificates have been launched, allowing Optometrists to upskill in a number of areas including glaucoma management, pediatric eye care and low vision. The number of Optometrists currently undertaking these qualifications is increasing and in recent years, employment vacancies have been advertised specifically requiring these additional qualifications as part of the ‘essential criteria’.
These additional qualifications allow Optometrists to maintain and update their skills and knowledge in alignment with emerging evidence, allowing for career progression. In the past two decades, there has been a shift towards the majority of Optometrists working for large multiple franchises rather than independent practices. These additional qualifications allow Optometrists to enhance their employability and transferability.
Across the globe, the term ‘Optometrist’ does not refer to a consistent standard for the profession. In many countries, including the United States and Canada, newly qualified Optometrists hold an OD (Doctorate of Optometry) and have a wider scope of practice than in the UK, offering a greater range of therapeutic services to patients and are regarded as highly qualified professionals.
In other countries in Europe, Optometrists have a more limited role, closer aligned with Dispensing Opticians where medical eye related issues are always referred to a hospital Ophthalmologist.
It may be argued that the drive towards higher qualifications is partly motivated by the increasingly litigious nature of health care or the age of self-diagnosis via the internet. Where patients are considered as consumers, Optometrists may feel obliged to maintain their knowledge and skills to a higher level and therefore undertake courses to protect themselves.
However, whatever the motivation, there does seem to be an appetite for further qualifications in Optometry and this increased level of skills and knowledge will benefit both patients and practitioners [10].
1.6. Undergraduate Optometry Students’ Perspective of the Place Model
Due to the limited published data on professional perspectives in Optometry, we conducted a scoping exercise to determine how the Place Model may be applied to the profession.
2. Materials and Methods
The Place Model [1] Survey was originally designed to determine the views of teachers and teacher educators of the Place Model and Freidson’s three logics [11]. For the purposes of this study, the Place Model Survey has been adapted to determine the views of undergraduate Optometry students (Appendix A).
Data collection took place during the 2018–2019 academic year and the study was approved by Research Governance at Ulster University which adheres to the tenets of the Declaration of Helsinki.
Participants were undergraduate Optometry students at Ulster University and prior to participation, were provided with an information sheet outlining the study. All undergraduate Optometry students were invited to participate in the study. Consent was assumed when the subject choose to complete the survey as indicated on the survey itself (Appendix A).
Participants were provided with an oral description of the Place Model and were then asked to complete the survey. This comprised; initial demographic questions, Place Model questions where the subject was asked to locate themselves (with an X mark) and their perception of the status and professional learning journey which is typical of optometrists within their own (United Kingdom based) education system (with a 0 mark). In addition, they were asked for a written explanation of these two locations [11].
Following survey completion, statistical analyses were performed using IBM Statistical Package for the Social Sciences (SPSS) (version 25).
3. Results
From the undergraduate Optometry population at Ulster University, 33 year one students, 34 year two students and 34 year three students took part in the study (n = 101). Reflective of the current undergraduate population, the majority of participants were female (74%, n = 75).
The Place Model
All subjects placed themselves in the Proto-professional area on the Place Model. Examples of written feedback are described in Table 1.

Table 1.
Written feedback on personal Optometry undergraduate placement within the Place Model.
The majority of participants placed qualified optometrists in the Professional area on the Place Model (87%, n = 88) with the remainder placing qualified optometrists in the De-Professional area on the Place Model (13%, n = 13). There was no statistically significant difference between responses from male and female participants (t-test, p = 0.38). There was also no statistically significant difference between responses from subjects in year 1, 2 or 3 of their undergraduate program (one way ANOVA, p = 0.10). Examples of written feedback from subjects who placed qualified optometrists in the De-Professional area on the Place Model are described in Table 2. There were no comments relating to ‘precarious professionals’ or ‘no professionals’.

Table 2.
Qualitative feedback on Optometry undergraduate placement of qualified optometrists within the Place Model.
4. Discussion
Reassuringly, undergraduate optometry students unequivocally view themselves as proto-professionals. They clearly identity as professionals at the beginning of a learning career in healthcare practice.
Undergraduate Optometry students largely view qualified optometrists within the ‘Professional’ category of the Place Model which would suggest that they, as individuals, aspire to the role of the ‘Ideal Optometrist’. However, somewhat worryingly, there seems to be some evidence to suggest that there is a small number of qualified practitioners in existence who have become disillusioned with their profession. Whilst this evidence from undergraduate students is subjective and anecdotal in nature it does back up evidence from the Association of Optometrists’ Optometric Workforce survey that there is a growing shift towards de-professionalization. More work needs to be done in order to explore this further, and the Place Model may be a useful tool in order to facilitate this.
The Association of Optometrists published a report on ‘recruitment, retention and career aspirations of the optometric workforce’ in 2018 [12]. The main findings from the report suggest that the direction of the profession is changing to a more female dominated profession with a high proportion of locums with flexible work patterns. The report also suggested that Optometrists feel that, the profession is feeling devalued with other health professions and the general public not being aware of the Optometrists’ scope of practice. They reported that Optometrists feel under pressure to sell spectacles with the situation being exacerbated by the low NHS fee for sight tests. In contrast, a workforce survey by The College of Optometrists revealed that the majority of respondents (80%) rated their job satisfaction as either 5, 6, or 7 on a 1–7 scale (with 7 being the highest level of satisfaction) [13]. The findings of the survey suggested that clinical appraisals are key to maintaining and developing clinical practice [13]. This may be difficult to implement in smaller or independent practices, and particularly with part-time or locum Optometrists. This highlights the importance of continuing professional development (CPD) in order to maintain a secure professional position in terms of the Place Model. The General Optical Council (GOC), the regulatory body for the optical profession, launched the Education Strategic Review (ESR), a consultation on optometric education standards and learning outcomes in 2017. The review’s primary objectives are that the regulator is able to clearly identify the major risks within the sector; there is clarification of the role of the optometric professional and there is a clear understanding of how healthcare is delivered across all UK regions [14]. This consultation-led review received 539 responses from individual registrants (Optometrists and Dispensing Opticians), universities, professional bodies and other relevant stakeholders [14]. Following on from the consultation exercise, the GOC described five key steers all of which point towards the ‘Ideal Optometrist’ most notably the fourth steer of ‘increasing emphasis on professionalism’.
5. Conclusions
In summary, it is important that undergraduate educators ensure that Optometrists in training are fully aware of the issues relating to current practice and that they carefully consider the direction of their career progression. The Place Model may be an opportunity to discuss with Optometry students these issues and highlight the choices that are available on graduation to ensure that we maintain highly skilled and caring professionals that provides high quality eyecare for the public.
Author Contributions
Both authors J.F.M. and K.B. contributed to all aspects of the study including the design, data collection and preparation of the manuscript for publication.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
The Place Model: Survey
I would like to ascertain your views in relation to the Place Model. They will be anonymous and will be treated in confidence. Completion of this survey is voluntary and implies consent (please see Information Sheet provided).
- As an optometry student, please indicate how long you have been a student: ______years.
- Your gender__________
- On the Place Model diagram below:
(a) Please use an X to indicate where you perceive that you fit on the Place Model.
(b) Please use a 0 to indicate where you consider that optometrists are generally perceived to be placed on the Model (by the public) within the United Kingdom.
(c) Please explain briefly where you have placed yourself (X).
___________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
(d) Please explain briefly where you have placed optometrists in your UK (0).
___________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
(e) Please use the space below to describe an optometrist who you consider might clearly exemplify any of the areas of the model—please indicate which area (professional, precarious professional proto-professional or deprofessionalized.
___________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
References
- Clarke, L. Mapping teacher status and career-long professional learning: The Place Model. Discourse Stud. Cult. Politics Educ. 2018, 39, 69–83. [Google Scholar] [CrossRef]
- Parkins, D.J.; Benwell, M.J.; Edgarm, D.F.; Evansm, B.J.W. The relationship between unwarranted variation in optometric referrals and time since qualification. Ophthalmic Physiol. Opt. 2018, 38, 550–561. [Google Scholar] [CrossRef] [PubMed]
- General Optical Council. Professional Boundaries and Service Needs in Eye Health Services: The Impact on Future Education Requirements for UK Trained Optical Practitioners. Discussion Paper. 2017. Available online: https://www.optical.org/filemanager/root/site_assets/education/education_strategic_review/supplementary_reading/professional_boundaries_in_the_optical_sector_-_goc_discussion_paper_2017.pdf (accessed on 2 May 2019).
- Howell-Duffy, C.; Scally, A.J.; Elliott, D.B. Spectacle Prescribing II: Practitioner experience is linked to the likelihood of suggesting a partial prescription. Ophthalmic Physiol. Opt. 2011, 31, 155–167. [Google Scholar] [CrossRef] [PubMed]
- The College of Optometrists Professional Guidance. Available online: https://guidance.college-optometrists.org/guidance-contents/ (accessed on 6 June 2019).
- Poostchi, A.; Awad, M.; Wilde, C.; Dineen, R.A.; Gruener, A.M. Spike in neuroimaging requests following the conviction of the optometrist Honey Rose. Eye 2018, 32, 489–490. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Available online: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment (accessed on 6 June 2019).
- Reddy, P.A.; Congdon, N.; MacKenzie, G.; Gogate, P.; Wen, Q.; Jan, C.; Clarke, M.; Kassalow, J.; Gudwin, E.; O’Neill, C.; et al. Effect of providing near glasses on productivity among rural Indian tea workers with presbyopia (PROSPER): A randomised trial. Lancet Glob. Health 2018, 6, e1019–e1027. [Google Scholar] [CrossRef]
- Irving, E.L.; Sivak, A.M.; Spafford, M.M. I can see fine: Patient knowledge of eye care. Ophthalmic Physiol. Opt. 2018, 38, 422–431. [Google Scholar] [CrossRef]
- Barrett, C.; Loughman, J. Expanding the traditional role of optometry: Current practice patterns and attitudes to enhanced glaucoma services in Ireland. J. Optom. 2018, 11, 252–261. [Google Scholar] [CrossRef]
- Freidson, E. Professionalism: The Third Logic; Polity Press: Cambridge, UK, 2001. [Google Scholar]
- Robinson, D.; Edwards, M.; Cockett, J.; Hey, L. Optometrists’ Futures. A survey report of recruitment, retention and career aspirations of the optometric workforce, for the Association of Optometrists; Institute for Employment Studies: Brighton, UK, 2018; Available online: https://www.aop.org.uk/career-development/optometrists-futures (accessed on 2 May 2019).
- The College of Optometrists. The Optical Workforce Survey Full Report. Available online: https://www.college-optometrists.org/uploads/assets/uploaded/b8034532-ce20-4e5d-8792039e270a34d1.pdf (accessed on 20 May 2019).
- The General Optical Council. News from Council 15 May 2019. Education Strategic Review consultation. Available online: https://www.optical.org/en/news_publications/news_item.cfm/news-from-council-15-may-2019 (accessed on 25 May 2019).
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).