Abstract
The use of hearing technology is one of the most effective strategies for providing access to spoken language and the auditory environment for students who are deaf or hard of hearing. In recent years, rapid advancements in hearing technologies have significantly improved access to spoken languages for learners of all ages. As part of the Special Issue “Educating Deaf Students in the 21st Century: A Changed and Changing Context”, this article describes how changes in hearing technology are related to changes in where and how students who are deaf or hard of hearing are educated. This article is designed to provide a foundation of knowledge about today’s hearing technologies for families, educators, and professionals such as speech–language pathologists or early childhood educators who support families and students. It provides an overview of hearing technology options, how they are prescribed and fit, and how benefits for language and literacy development can be evaluated. Barriers to effective use and future directions for hearing technologies are also described. The section “Highlights for Educators and Families” in the article discusses the practical application of this information to the work of those supporting students who are deaf or hard of hearing at home, at school, and in the community.
1. Introduction
There is no doubt that the impact of hearing loss on a child’s spoken language development can be significant. Early identification and intervention as well as the provision of access to the speech signal through the consistent use of hearing technologies are two strategies proven effective at mitigating this impact. The role of hearing technologies is to provide individuals with hearing loss with access to sound and, most importantly, to spoken language. In the past, the limitations of technology provided children with more limited access to sound in order to acquire and use spoken language for communication. Today’s technology provides improved access to sound, resulting in improved communication outcomes for children with hearing loss. In other words, the goal in the research and development of hearing devices for children is that better hearing technology will lead to better access to spoken language and thereby to better communication outcomes. However, in order to be effective, hearing technology must be used consistently and appropriately. In essence, this means all day every day. Ensuring consistent use requires parents, professionals, and other adults in the child’s life to be knowledgeable about why a particular technology was chosen, how it needs to be used on a day-to-day basis, and any challenges or limitations that might be associated with it. If parents and educators do not have the knowledge and skills to support a child’s use of technology, the potential benefits are reduced. Parents and educators also need to be able to gather information about the child’s development and use of language, and to share this with hearing health care professionals, in order to identify when and where technology might need to be fine-tuned or even changed. Parents and educators not only need to know the mechanics of how particular devices work, but also what to look for in their child’s everyday communication development. This is true for children of all ages, but is perhaps particularly true in the case of infants and toddlers, for whom there may be more challenges in making decisions about technology. For example, if an infant is wearing hearing aids on their ears but, unknown to the parents, the hearing aids are broken, then that child has limited or no access to spoken language. The better informed parents and educators are about a child’s hearing technology, the better they can support the child in achieving their highest potential.
This article will describe hearing technologies used by deaf and hard-of-hearing children, including hearing aids, cochlear implants and bone-anchored devices, with an emphasis on implications for educators and families. The challenges of prescribing and fitting technology for children will be discussed, as well as how benefits from hearing technology can be measured in the clinic and in the real world. Barriers to effective use and future directions for hearing technology will also be discussed. Each section provides technical information. There is also a “Highlights for Educators and Families” section that presents a discussion of the application of this technical information to allow professionals and families to support children using hearing technology.
Educators may not be aware of the fact that the provision of hearing aids to children is relatively new in the history of deaf and hard-of-hearing education, and cochlear implants and bone-anchored hearing aid are even newer. In fact, prior to the early part of the 20th century, parents were not able to access hearing testing for their children to confirm the presence of hearing loss. The first modern hearing testing equipment was not developed until the early 1920s, and hearing testing for children was not widely available until the 1930s, mainly in large urban centers. Until the middle of the 20th century, the diagnosis of hearing loss in children relied primarily on observation and informal testing with noisemakers (Ciocco & Palmer, 1941; Macfarlan, 1939). The average age of diagnosis of hearing loss was reported in the 1950s to be 3 years of age; this remained true for decades until the introduction of newborn hearing screening (Durieux-Smith et al., 2008; Hyde, 2005; Schweinitz et al., 1959).
Rudimentary hearing aids were developed in the early part of the 20th century, but were often too large to be comfortably worn in everyday life because of the size of the components and their batteries. Technological advancements during and after World War II spurred the development of wearable hearing aids for the large number of veterans with acquired noise-induced hearing loss. However, hearing aids were not widely available outside of schools for the deaf for children, and procedures for fitting them were still largely based on guesswork (Berry, 1948; Myklebust, 1946; Pintner, 1942; Reiter, 1950). Without access to hearing aids, learning to talk relied very heavily (and sometimes entirely) on lipreading (Gardner, 1943). Lipreading provides important support for speech understanding. However, even under controlled situations with adult listeners, speech understanding using lipreading alone is around 20% (Bernstein et al., 2000; Fernandez-Lopez et al., 2017). The acquisition of age-appropriate spoken language in the absence of access to sound was out of reach for many children. In the 1950s and 1960s, body aids were used. These were devices, worn on the chest or back, with two cords that connected the hearing aid to receivers and custom-made earmolds (Bangs & Bangs, 1952). While ear-level hearing aids became more widely available in the 1960s and 1970s, it was not until the early 1980s that cochlear implants were approved for children with severe to profound hearing loss. First, this was only for children over the age of 5; then, this was for children under the age of 2; and now this is for children under the age of 9 months.
We can date what might be considered the modern era for children with hearing loss to the 1990s, with the intersection of 3 technological advancements in audiology. First, the addition of the otoacoustic emission test to audiological practice in the early 1990s finally provided a tool with sufficient accuracy and cost-effectiveness to serve as a foundation for universal newborn hearing screening (Kemp et al., 1990). The second advancement was the approval of cochlear implantation for children under 2 years of age in the United States in 1990. The third advancement was the introduction of digital signal processing in the early 1990s, which provided much better sound quality and more sophisticated sound processing. It has only been since the 1990s, then, that a deaf child could be identified shortly after birth, fit with effective hearing aids, have access to binaural cochlear implantation if hearing aids were not effective, and receive early intervention services for language development.
Box 1. Highlights for educators and families.
Understanding how much has changed with respect to the early diagnosis of hearing loss and the provision of hearing technology is important to understand the significant improvements in access to spoken language and in opportunities to acquire typical speech and language for children. For example, consider an individual born with severe hearing loss, who is 60 years of age or older, born in the 1960s. They are likely to have been identified late and to have been given hearing aids providing little auditory access, and may use a visual language such as American Sign Language. The grandchild of this individual, in contrast, was likely identified as an infant, had access to digital hearing technology and excellent auditory access, and may well have typical speech and language skills. The educational journey and experiences of a deaf individual born in the 1960s or 1970s were significantly different than those of a deaf child born today. In 1977, results from the annual Gallaudet Survey of Deaf and Hard of Hearing Children and Youth indicated that 51% attended schools for the deaf, and only 18% were fully mainstreamed (Holden-Pitt & Diaz, 1998). Today, in resourced countries such as the UK, almost 80% of students who are deaf or hard of hearing are mainstreamed and attending their local school, while 2% attend a school for the deaf (CRIDE, 2024).
It should be noted that a lack of access to hearing health care and hearing technology remains a challenge in under-resourced countries, sometimes also referred to as lower- and middle-income countries or LMICs, generally defined using the criteria of the World Bank (2021) (see Waterworth et al., 2022 for a review of services). The recent WHO World Report on Hearing identifies access to health care services in general, and access to hearing health care services in particular, as a significant barrier in under-resourced services (Waterworth et al., 2022; World Health Organization [WHO], 2021; Wilson & Tucci, 2021). Bisgaard et al. (2022) used sales data from the European Hearing Instrument Manufacturers Association to estimate the availability of hearing aids in European and African countries. They noted that, for under-resourced countries (which make up 85% of the world’s population), hearing aid coverage ranged from 1.5 to 2%. Of course, these data include both adults and children, and there are some potential errors in the data due to incomplete reporting; nonetheless, it is clear that the provision of hearing aids in under-resourced countries is a huge problem. Cochlear implant provision is even poorer; Bodington et al. (2021) estimate that globally, less than 1% of people who are candidates for cochlear implants have them. They note that although cochlear implant programs exist in some under-resourced countries such as China, India, Pakistan, Nigeria, Saudi Arabia, and Cuba, they are specialty services usually only available in large cities, presenting access issues for many families. Barriers to accessing audiological services can also exist in resourced countries such as Canada or Australia, which face challenges because of geography (Fitzpatrick et al., 2021; Kemper et al., 2021).
Box 2. Highlights for educators and families.
Educational philosophies and strategies need to be grounded in the local context. Students who do not have access to hearing technology will have greatly reduced opportunities to acquire spoken language and require a greater focus on visual communication. In other contexts featuring universal newborn screening and comprehensive early intervention with technology, educators may find that most students have spoken language outcomes which are commensurate with hearing peers. However, even in resourced countries with comprehensive hearing health care, it is important for educators to remember that they will still need to be prepared to support students who come to school with very limited language and literacy skills, perhaps as immigrants from under-resourced countries.
2. Challenges in Prescribing Hearing Technology for Children
The current recommendations regarding audiological management for infants call for a 1:3:6 approach, that is, hearing screening completed by 1 month of age, the identification of hearing loss by 3 months, and enrolment in early intervention programs by 6 months (Joint Committee on Infant Hearing, 2019). This is an ambitious goal and not always met (Awad et al., 2019; Gustafson & Corbin, 2021; Tang et al., 2023), but children are certainly being fit with hearing technology far earlier (Ching et al., 2018b). However, children are not simply small adults when it comes to fitting hearing technology, and there are important differences.
2.1. Reliance on Objective Measures and Incomplete Data for Infants and Toddlers
The accurate measurement of a child’s hearing is crucial for the prescription of hearing technology, but the question of how this can be achieved for children who cannot tell us what they can hear remains. The audiological assessment of very young children uses a combination of objective and behavioral tests. Objective tests do not require any behavioral response from the child (in fact, they are usually best conducted when the child is asleep). These include otoacoustic emissions, auditory brainstem response testing and acoustic reflexes. While accurate, objective tests generally do not provide a complete picture of the child’s hearing levels for all frequencies important for understanding speech, and do not provide information about the clarity of speech. Once a child is old enough to provide a behavioral response to a sound, better information about a child’s ability to comprehend auditory information can be gathered, but child cooperation and attention can still limit the information that can be obtained. While a combination of objective and behavioral tests provides sufficient information to begin the process, audiologists often have less information than would be available when treating an adult. Hearing aid prescription is therefore a process and not a single event, requiring ongoing fine-tuning as more information is obtained and as children’s communication contexts change with age.
2.2. Lack of User Feedback
In contrast to adults who can report on the benefits of amplification immediately, evaluating whether the use of hearing technology is leading to the development of spoken language takes time. It may take weeks or months of language input via hearing technology before outcomes can be measured in the form of expressive language. Hearing technology settings must be adjusted so that important sounds in the environment are amplified appropriately, while also ensuring that sound is never uncomfortable or risks damaging hearing in the absence of user feedback. When cochlear implantation is being considered, one criterion is that the child has not shown benefit from first trying hearing aids (American Academy of Audiology, 2019). However, determining benefit (or lack thereof) can be challenging when children cannot report their experience.
2.3. No Room for Error
The impact of hearing loss is significant for individuals of all ages. However, most adults have an intact spoken language system and communication strategies which can lessen the impact of hearing loss compared to children (Pittman et al., 2002). Adults who miss a word in a sentence, for example, can often fill in the missing information through context, their knowledge of language, and metacognitive strategies. Because children are acquiring language from scratch, they need full access to the speech signal. We need to ensure that the entire speech signal is made audible across the frequency range for a variety of sound inputs (soft, moderate, loud). There is no room for error; the child’s spoken language development relies on the audiologist getting it right.
2.4. Anatomical Factors (Hearing Aids)
Hearing aids need a way to direct the sound from the hearing aid into the wearer’s ear canal. This is performed via the earmold, a vinyl or silicone piece that, for children, is usually custom-made to fit the child’s ears precisely. Children’s outer ears and ear canals continue to grow and change until adolescence. Earmolds need to be remade in larger sizes on a regular basis to ensure a comfortable fit. For infants, for example, this might mean new earmolds are needed every 2 to 3 months, adding more appointments to a family’s already busy schedule, as well as additional costs. Changes in ear anatomy also change how loudly sound is perceived by the child, and this must be factored into hearing aid prescription. Hearing aid responses must be regularly evaluated to account for changes in ear anatomy until ears reach adult size.
2.5. Progressive and Fluctuating Hearing Loss
The vast majority of adults with hearing loss are those born with typical hearing who acquire hearing loss later in life through aging, noise exposure, or disease (World Health Organization [WHO], 2021). While the progression of acquired hearing loss in adults is common (for example, with age), these decreases tend to be gradual and slow. Many causes of hearing loss in children (such as cytomegalovirus and enlarged vestibular aqueduct syndrome) are more complicated and can be associated with significant progressive or fluctuating hearing loss (Barreira-Nielsen et al., 2016; Brookhouser, 2002). A common cause of fluctuating hearing loss for all children (but less common in adults) is otitis media, or middle ear infection. It is often associated with a buildup of fluid behind the eardrum, causing conductive hearing loss until the fluid resolves itself or is drained surgically. For children with hearing aids, an episode of otitis media can result in additional hearing loss for which hearing aids were not programmed to account. Children may lack the language or auditory skills necessary to identify decreases or fluctuations in hearing. Therefore, reduced access to spoken language for a child may go unaddressed unless parents and professionals are trained to be careful observers.
2.6. Verification and Validation of Hearing Technology
For children and adults, the prescription and fitting of hearing technology is a process involving several stages, including hearing assessment, the determination of hearing aid targets and features, the prescription and fitting of the hearing aid, and the evaluation of benefit (Seewald et al., 2005). The evaluation of benefit consists of two processes, namely, verification and validation. Verification uses technological measurements to confirm whether the technology is meeting software targets and operating according to technical standards. In contrast, validation aims to ensure that hearing technologies provide benefit in real-world situations in a variety of listening environments. Hearing technology can then be fine-tuned based on this feedback. For adults, this typically involves user feedback, but for children validation relies heavily on observations and feedback from parents and other individuals in the child’s environment.
Box 3. Highlights for educators and families.
It is important for families and preschool educators to understand that prescribing and fitting hearing technology is a process which typically requires ongoing fine-tuning; the relationship with the child’s audiologist that begins when their child is an infant will last for years. Fitting hearing technology on very young children is challenging, and yet getting this right is crucial because the communication stakes are so high. It may take several appointments for the initial hearing technology fitting, as well as regular appointments afterwards to fine-tune hearing technology as students become older and/or hearing levels change through the process of verification. The validation of hearing technology relies on a partnership between families, educators, and audiologists. Audiologists rely on observations and feedback from families and educators because they only interact with the child for a limited time in their clinics. However, audiologists need to understand how children are reacting to the use of hearing technology in their everyday life, and to recognize situations where hearing levels may have changed. An important role of preschool educators for deaf and hard-of-hearing students is to help parents become effective observers of their child’s development so that their feedback can inform the best possible provision of hearing technology.
3. Types of Hearing Technologies and Candidacy
There are three types of hearing technologies available—hearing aids, cochlear implants and bone-anchored hearing devices. Candidacy for hearing technology in children is essentially based on the presence of any degree of hearing loss. Types of hearing loss (conductive, sensorineural, mixed or auditory neuropathy), the degree of hearing loss and, to a lesser extent, the cause of hearing loss are important factors in choosing the most appropriate device for a child. Table 1 provides an overview of each device.

Table 1.
Overview of types of hearing technologies.
Hearing Aids
There are generally two types of hearing aid style: behind-the-ear hearing aids and custom hearing aids. Behind-the-ear hearing aids require an earmold to couple the aid to the user’s ear, while custom hearing aids consist of one piece, which is made to fit the user’s ear exactly based on an ear impression. Custom aids come as one piece, with different sizes ranging from larger in-the-ear (ITE) aids and in-the-canal (ITC) aids to the smallest completely-in-the-canal (CIC) aids. Figure 1 illustrates some examples of hearing aids; from left to right, the first 5 aids are custom-made and the 3 aids on the right are behind-the-ear aids.

Figure 1.
Behind-the-ear hearing aids with charger. Courtesy of Oticon.
Behind-the-ear hearing aids are preferred for children as they have better circuit flexibility, durability, battery life, and connectivity to assistive devices. In addition, because the earmold can be detached from the hearing aid, it can be easily remade when a child’s ear grows, in contrast to ITE, ITC, or CIC hearing aids, where the entire hearing aid shell needs to be replaced at greater cost. Figure 2 shows a BTE hearing aid with a custom-made earmold on a child’s ear. Since the first discussion of binaural hearing aids in the 1960s (Fisher, 1964), the research is very clear that two hearing aids are better than one for a wide variety of auditory tasks, and binaural hearing aid fitting is always recommended as the default approach (see Ching et al., 2006 for a review).

Figure 2.
Behind-the-ear hearing aid with a custom earmold on a child’s ear.
All hearing aids consist of several parts: one or more microphones that pick up sound in the environment, and an amplifier/processor that amplifies the signal picked up by the microphone according to the degree and configuration of the individual’s hearing loss. These amplified signals are processed by a small computer chip, which provides further tailoring of the signal. The third component is the receiver, which converts the modified electrical signal back into sound waves, which are then delivered into the wearer’s ear canal.
Behind-the-ear hearing aids also require earmolds, custom-made pieces typically made of silicone or acrylic. Earmolds help keep the hearing aid securely in place, ensuring proper functionality and comfortable wear. They direct sound from the hearing aid down the ear canal, while preventing sound from escaping out of the ear and causing feedback. Audiologists use silicone material to take an exact impression of the child’s outer ear and ear canal, which is then made into the earmold. One of the most challenging aspects of making earmolds for children is obtaining a proper fit, particularly for infants with very small outer ears and children with outer ear malformations (Wolfe & Scholl, 2009). Infants in particular require frequent remakes of the earmold as their ears grow, which is sometimes every 2 to 3 months.
Box 4. Highlights for educators and families.
Educators and families do not prescribe or fit hearing technology. However, they still need to have sufficient knowledge to support children in using it to ensure that it is working well and to identify when there may be a problem. For example, the first sign that a child is outgrowing their earmolds is that the hearing aid produces a whistling sound known as feedback. Families or educators who notice this need to know that a visit to the audiologist is in order to take impressions for new earmolds. Until children are old enough to manage their own technology, it is up to the adults in their life to keep the technology working and used consistently. Even older children with good communication skills may not always be able to detect subtle problems such as blocked earmold tubing or low batteries. Educators and families need to ensure that attention is paid to ensuring that children develop the skills to monitor and manage their own hearing technology, and to have the advocacy skills to speak up when something is not working. For example, for a preschool child, families and educators need to be able to detect changes in behavior that indicate a dead battery or malfunctioning technology. For older students, educators need to be aware that this can happen at any time, and so, for example, advocating for having extra batteries at school or allowing students to excuse themselves to change batteries is important.
4. Hearing Technology Features and Options
The explosion in hearing technology circuitry began with the introduction of digital signal processing in the 1990s and continues with the development of sophisticated adaptive circuits and incorporation of other technologies such as Bluetooth. It should be noted that much of the research on the benefits of these features involves adults, and so care should be taken to consider these features on a case-by-case basis for individual children (Seewald et al., 2005).
Receiver-in-the-canal (RIC) hearing aids: Receiver-in-the-canal (RIC) hearing aids are newer types of hearing aids that are more commonly prescribed for adults than children. Unlike conventional behind-the-ear hearing aids, which have all of their electronic components housed inside the hearing aid, RIC hearing aids have some components located inside the ear canal. RIC hearing aids do not use custom-made earmolds. Instead, there is a thin plastic tube protruding from the hearing aid that contains wiring. Tt the end of the plastic tube is the receiver for the hearing aid, with a soft rubber “dome” to hold the hearing aid in place. While RIC hearing aids are popular for adults due to their small size, they may not be appropriate for children for several reasons (McCreery & Walker, 2017). Because they do not use custom-made earmolds, there can be issues with fit, retention, and loss of the hearing aid. The electronic components located in the ear canal can be damaged by wax or moisture, leading to expensive repairs and downtime for the child. While most enable Bluetooth connectivity, their small size limits options for assistive technology in the classroom (Millett, 2023).
Directional microphones: Directional microphones work by focusing on sounds in front of the user while reducing the amplification of sounds from the sides or back to enhance the user’s ability to hear speech in noisy environments while minimizing background noise. Some hearing technologies can adaptively switch between omnidirectional (capturing sound from all directions) and directional modes (prioritizing sounds from the front) based on the environment. However, there is discussion in the literature around the suitability of directional microphones for children (Ricketts et al., 2017). The benefits of directional microphones are based on the principle that the sound source of interest is always in front of the child, i.e., that the wearer is looking at the speaker. This is not always a valid assumption for children, who may be looking in another direction. Directional microphones may also reduce the audibility of other important sounds in the environment. There is a small amount of research suggesting that directional microphones can provide improved speech understanding under controlled conditions for children, but this research has not been conducted in real-world, dynamic listening environments where incidental learning and access to classroom discussion may be impacted (McCreery et al., 2012).
Noise reduction circuits: Signal processing algorithms are employed to reduce the effects of background noise by analyzing the sound data captured by the microphones, classifying them as noise or speech, and reducing or amplifying the signal accordingly. Some technologies employ adaptive strategies that continuously adjust their noise reduction settings based on the changing sound environment. They achieve this, for instance, by automatically switching to a different mode windy conditions. Noise reduction circuits are becoming increasingly sophisticated and can provide benefit for children, although, again, not to the extent that assistive listening devices are not required in education (Browning et al., 2019; McCreery et al., 2012; Millett, 2023).
Automatic volume controls: Many hearing aids no longer have manual volume controls. Instead, automatic gain control circuits continually monitor incoming sounds and adjust the volume in real time so that soft and moderate level sounds are amplified to ensure audibility, but loud sounds are reduced for comfort and hearing protection. As discussed previously, careful assessment and prescription through evidence-based practice are crucial to ensure that settings are appropriate, as the wearer or parent has no control over the volume.
Multiple programs: Today’s hearing technologies generally contain multiple listening programs, which allow the audiologist to provide different hearing aid characteristics for different situations (e.g., Program 1 for general use and Program 2 for the subway, providing a lower volume). This provides more precise amplification for common listening scenarios than simply turning the volume up and down. Multiple listening programs are generally not used in the same way for children as for adults, as most children would be expected to have difficulty identifying which program would be most appropriate for a particular situation and then moving in and out of that program. However, multiple programs can be extremely useful for children with fluctuating hearing loss. A parent with access to an “ear infection program”, such as one that would provide the correct hearing aid response for the decreased hearing levels created by an ear infection, or a “feedback reduction program” to reduce whistling when earmolds start to become too small, would be able to deal with a temporary problem more appropriately.
Wireless connectivity: Today, wearers can stream audio directly to their hearing technologies, enhancing their listening experience and providing greater convenience and accessibility. For example, Bluetooth connectivity to a cellphone allows wearers to take calls, listen to music, or watch videos. Other technologies include telecoils (T-coils), electromagnetic coils that pick up signals from compatible audio systems. In venues equipped with hearing loop systems (induction loop systems), wearers can switch to the T-coil mode to receive amplified sound directly from the microphone or sound system without background noise. Remote controls and apps are also available, allowing wearers to adjust settings, volume, and programs, and even access additional features provided by the manufacturer.
CROS aids: CROS (contralateral routing of signal) hearing aids are used to help individuals with unilateral hearing loss or single-sided deafness, (i.e., one ear with little to no useable hearing and the other ear with typical hearing). The CROS system consists of two parts: a microphone/transmitter in a hearing aid case worn on the ear with hearing loss, and a receiver in a hearing aid case worn on the typically hearing ear. The microphone/transmitter picks up sound from that side of the head, and transmits it to the hearing ear, allowing the individual to hear from both sides of the head. However, the CROS system does not improve localization or speech discrimination in noise. CROS systems are more commonly used with adults than children; the research literature for children is very small, with some studies showing some benefit in difficult listening situations (Kwak et al., 2021), but others showing much variation in outcomes and compliance (Appachi et al., 2017).
Box 5. Highlights for educators and families.
As noted, families and educators do not prescribe hearing aids. However, they can and should be active participants in the hearing aid prescription process in terms of discussing their own challenges and objectives for their child. For example, if an RIC hearing aid is proposed for a child, parents should understand why the audiologist’s rationale for choosing this technology, as well as the potential limitations and disadvantages for children. If the hearing technology has directional microphones, families and educators need to ensure that the child is facing them when interacting, as the child will not hear sounds from the side or the back as well. If multiple programs are prescribed, families need to clearly understand how to identify when a different program is needed, and how to physically change the program. Some parents of infants and toddlers appreciate remote control as they allow one to easily make adjustments without having to take the hearing technology off; other parents may not want a remote control because it is just one more thing to manage. Educators are very familiar with the listening requirements at school, and may have valuable feedback or opinions on compatibility with assistive listening devices such as FM systems, tablets, or laptop computers for a particular make and model of hearing device. Educators can support families by explaining the particular listening challenges that a student faces at school so that families can provide a comprehensive picture to their audiologist for the consideration of different options, features, or characteristics.
4.1. Prescription and Fitting of Hearing Aids
The provision of any hearing technology is an ongoing process involving a number of steps (and therefore a number of appointments with the audiologist for the family). How do audiologists determine what is needed in a hearing aid in the absence of feedback from the child, often working with limited hearing test results? Audiologists rely on either of two research-based software programs developed for children, the Desired Sensation Level (DSL 5.0) approach from Western University in London, Canada, and the National Acoustics Lab-2 (NAL-NL2) approach from the National Acoustics Lab in Australia. While there are some differences, both aim to provide targets for hearing aid characteristics that provide the best audibility for soft and medium sounds while ensuring that loud sounds are not uncomfortably loud (Ching et al., 2013, 2018a).
Both methods use hearing thresholds to calculate appropriate acoustic targets. Once these are calculated, audiologists use Real-Ear Measurement (REM) to measure the sound level in a person’s ear canal with and without hearing aids. During REM, a tiny microphone probe is placed in the ear canal near the eardrum. Because children’s ears are still developing, and as they come in various shapes and sizes, it is important to use REM to incorporate the size and resonance characteristics of each child’s ear into the fitting. This measurement can then be used to evaluate different hearing aids and hearing aid settings to ensure that they match the specific needs of the child’s hearing loss. Once hearing aids have been provided to the child, REM is again used to verify that targets have been matched and adjusted as necessary over time as the child grows and as more audiological information is obtained.
4.2. Use of the Speech Intelligibility Index
In the past, the degree of hearing loss is a commonly used variable in research on outcomes for deaf and hard-of-hearing children. The degree of hearing loss has typically been indicated by a descriptor (mild, moderate, etc.) or by the calculation of the pure tone average. However, the degree of hearing loss does not indicate how much access a child has to spoken language with or without hearing technology. A better indicator of access to spoken language available is the Speech Intelligibility Index (SII) (ANSI, 1997). The SSI is a measure that estimates how speech is understood by a child with hearing loss by calculating the audibility of speech sounds under various conditions (e.g., with and without hearing aids) (Scollie, 2008). The SSI can be calculated to determine which hearing aid/ hearing aid settings provide the best SII and therefore the best audibility of the speech signal. This is valuable information for the clinical audiologist and can also serve as a useful counselling tool for families and school staff. The SII has been found to be a better predictor of children’s language development than pure tone average (McCreery et al., 2015; Stiles et al., 2012; Wiseman et al., 2023). It can also be a valuable tool when evaluating hearing aid candidacy for children with very mild hearing losses, where it is not always clear whether hearing aids are needed (McCreery et al., 2020).
There are two large longitudinal studies investigating the benefits of early identification and early amplification for children with hearing loss, the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study in Australia, and the Outcomes of Children with Hearing Loss (OCHL) study, from the Boys Town National Research Hospital in the USA. Both are large-scale longitudinal research projects that tracked the developmental progress of children with hearing loss from 2010 to the present. Key findings from both studies suggest that early intervention and access to appropriate hearing technology significantly impact the developmental outcomes of children with hearing loss. Children who received timely and effective interventions demonstrated notable progress in language acquisition, communication skills, and overall cognitive development (Ching & Leigh, 2020; Ching et al., 2018b; Moeller & Tomblin, 2015; Tomblin et al., 2015).
Box 6. Highlights for educators and families.
As hearing aids have become more sophisticated, the technology which audiologists use to evaluate benefit has become more sophisticated. Before the development of digital hearing aids, audiologists often conducted a standard hearing test while the child was wearing hearing aids, plotting the hearing aid thresholds on the child’s audiogram. There are many reasons why this approach to evaluating hearing aid benefit is no longer used by audiologists; however, it leaves families and educators without a tool to understand what they should expect a child to be able to hear with hearing aids. It is important for audiologists to take the time to explore this with families so that they have realistic expectations of what their child should be able to hear with hearing aids, as well as situations where the child would be expected to have difficulty hearing. Strategies for addressing this problem are discussed later in the section on functional hearing assessment. Functional hearing assessment is an excellent tool for understanding how clearly a child hears in dynamic listening environments (such as with distance or background noise). Parents and educators are not expected to understand all of the details of their child’s hearing technology, but they should understand what to expect for a student, how to monitor the impact of the technology, and how to identify when something is not quite right.
4.3. Cochlear Implants
Cochlear implants can provide access to sound for individuals who do not receive benefit from conventional hearing aids (generally, although not exclusively, those with bilateral severe to profound hearing loss). While traditional hearing aids amplify sound, cochlear implants bypass damaged portions of the ear and directly stimulate the auditory nerve, allowing individuals with severe hearing loss to send signals to the brain.
Cochlear implants consist of two components, the internal implant (with an electrode array that receives the sound from the external processor) and the external sound processor. A microphone on the external part of the implant picks up sound from the environment. Sound is then processed into digital signals by the external speech processor, worn externally. Processed signals are sent wirelessly across the skin to a transmitter and receiver/stimulator implanted under the skin behind the ear and then to the electrode array. These electrodes directly stimulate the auditory nerve fibers. The auditory nerve carries these electrical impulses to the brain, where they are interpreted as sound. This provides the sensation of sound to the wearer. Figure 3 indicates the internal and external components of a cochlear implant.
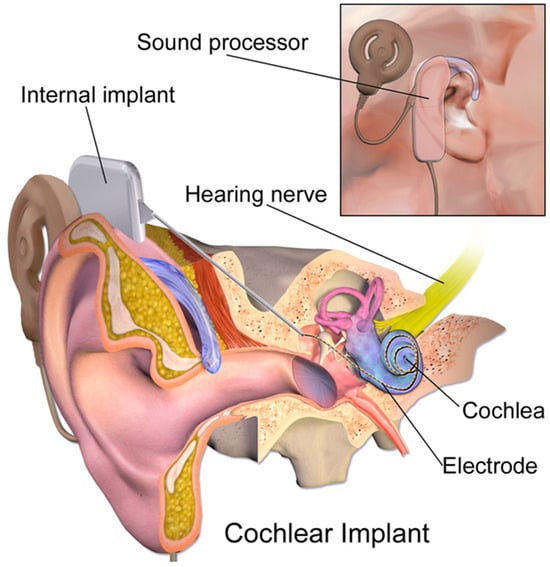
Figure 3.
Hearing with a cochlear implant. Blausen.com staff (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1(2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. Creative Commons Attribution 3.0. accessed on 23 February 2025.
As with hearing aids, technology is advancing very rapidly, and so it is important to note that information which might have been accurate even 5 or 10 years ago may no longer be true. For example, it was once true that cochlear implant surgery destroyed any residual hearing through the process of inserting the electrode. However today, advancements in both the electronic component and in surgical techniques mean that residual hearing is generally conserved (Schaefer et al., 2021).
4.4. Candidacy
While candidacy criteria vary to a certain extent across programs, cochlear implants are generally considered for two populations of children. The first is infants and toddlers (9 months of age or older) with severe to profound hearing loss who are not predicted to be able to acquire typical spoken language without intervention. Typically, this would be children born with hearing loss, but can also include preverbal children with a sudden loss of hearing (for example, from meningitis). In fact, children of any age (as well as adults) with deafness resulting from meningitis are always considered priority candidates for implantation. This is due to both the degree of hearing loss and the fact that a process of bone growth inside the cochlea known as ossification begins within days or weeks of meningitis, potentially preventing insertion of the electrode array into the cochlea if surgery is not performed quickly.
The second population is children with sensorineural hearing loss who demonstrate insufficient benefit from hearing aids for spoken language and literacy development because of poor access to the speech signal. This could include children with progressive hearing loss (where hearing loss becomes too severe for effective hearing aid use), children with sudden hearing loss from meningitis, trauma, or infection, children with hearing loss and poor speech discrimination, andr children with auditory neuropathy spectrum disorder. Warner-Czyz et al. (2022) recommend a 50/70+ criteria for children; that is, clinicians should consider referring a child for assessment with (i) a pure tone average of greater than 70 dB, and/or (ii) speech recognition scores of less than 50%, and/or (iii) poor functional performance, limited progress in language or auditory development, or a poor quality of life.
Research clear shows that earlier implantation (prior to the age of 12 months) results in better speech, language, and literacy outcomes than later implantation (see S. D. Sharma et al., 2020, for a review). There is a critical period for the development of the auditory pathways and auditory cortex, a period during which sound stimulation is required for development (Fliegelman, 2020; Harrison et al., 2005; Kral & Sharma, 2012; A. Sharma & Campbell, 2011). It is possible for implants to reduce or even prevent the adverse effects of auditory deprivation on the brain. Because of this, it is important to note that candidacy continues to evolve, specifically expanding to younger infants, children with lesser degrees of hearing loss, and those with unilateral hearing loss (American Academy of Audiology, 2019; Carlson et al., 2015; Patro et al., 2023; Purcell et al., 2021; Naik et al., 2021; Varadarajan et al., 2021).
Candidacy for an individual child requires the consideration of more than just age and the degree of hearing loss, however. Cochlear implant centers have dedicated teams of professionals, including specialist ear, nose, and throat (ENT) surgeons, audiologists, speech and language therapists, social workers, psychologists, and teachers of the deaf, all of whom play a role in determining whether cochlear implantation is appropriate. During the assessment phase, many factors are considered. This not only includes audiological information and medical test results (e.g., MRI results), but also speech, language, and developmental assessment results, as well as psychosocial and family factors. Even if the cochlear implant team recommends implantation, the final decision always rests with the family (and the child, depending on age).
4.5. Process
Surgery is performed for children under general anesthesia, typically lasts 1.5 to 2 h per ear and, in many programs, is performed as day surgery where children go home on the same day. The regular assessment of wound healing is performed, but for most children, external processor fitting can occur 3–4 weeks after surgery. This initial appointment involves the process of programming the speech processor and electrode array, known as MAPping. MAPping is the term used to describe the process of programming the cochlear implant to provide the best possible access to sound (Wolfe & Schafer, 2010). Cochlear implant audiologists determine the minimum amount of stimulation that is needed to make sounds audible (called threshold, or T levels), as well as the maximum amount of stimulation that can be allowed (called C level). The initial MAP of the cochlear implant is always conservative in terms of loudness; the cochlear implant is initially programmed to be softer than what is ultimately needed.
There is also a need for the validation of the cochlear implant fitting (as with hearing aids), and the tools used for this (observation, checklists, questionnaires) are similar or often the same as those used to validate hearing aid fittings. Initially, regular appointments with the audiologist are required to track progress; once the MAP is finalized, annual or biannual checkups are scheduled for follow-up.
4.6. Sequential vs. Simultaneous Cochlear Implantation
As discussed previously, binaural hearing provides significant benefits over hearing in only one ear. However, when cochlear implantation for children was first introduced, the approach was more conservative, and funding was not as readily available; therefore, many young people only received only one cochlear implant. Subsequent research has clearly demonstrated that children have better outcomes with binaural cochlear implants, including more natural hearing, reduced listening effort, an improved quality of life, better speech understanding in noise, and improved localization (see S. D. Sharma et al., 2020 for a review). Therefore, many individuals received a second cochlear implant at a later date; this is known as sequential cochlear implantation. As cochlear implant candidacy criteria have expanded based on recommendations from the research, simultaneous cochlear implantation (i.e., both ears implanted at the same time, during the same surgery) has become the standard recommendation (Messersmith et al., 2019; National Institute for Health and Clinical Excellence [NICE], 2019; Warner-Czyz et al., 2022).
4.7. Bimodal Use
It is not uncommon for children to have bilateral hearing loss, where hearing loss in one ear meets the criteria for cochlear implantation but the other has a less severe degree of hearing loss. In these cases, the standard recommendation is to implant in the ear with more hearing loss, but continue the use of a hearing aid on the other, in a technique known as bimodal stimulation. In the early days of cochlear implantation, it was thought that the user would have difficulty understanding input from two different devices, and that it was preferable to use the cochlear implant alone. However, there are significant benefits to continuing to use a hearing aid with a cochlear implant on the other side and current guidelines indicate that bimodal fittings should be considered (Belsare et al., 2020; Holder et al., 2022; Mok et al., 2009). Gifford (2020) noted that bimodal stimulation is most appropriate when the hearing loss in the better ear is less than approximately 70 dB. If the better ear shows hearing loss which is greater than approximately 70 dB, implanting in that ear is the better choice.
4.8. Unilateral Hearing Loss/Single-Sided Deafness
There is a large body of research documenting the listening difficulties that children experience when they only have typical hearing in one ear, and no useable hearing in the other (see van Wieringen et al., 2019 for a review). In the past, technology for this kind of hearing loss was limited to the CROS aid described previously. However, within the last few years, the provision of a cochlear implant to the deaf ear has been investigated for children (see Park et al., 2022 for clinical guidelines). Candidacy criteria are generally more conservative for this use than for children with bilateral hearing loss (Park et al., 2022). It should be noted that a common finding in children with single-sided deafness is that the auditory nerve is small (hypoplastic) and therefore expectations for cochlear implant success are often lower (Park et al., 2022). Results have been mixed, as some studies report improvements in speech understanding in noise (Brown et al., 2022; H. V. Ganek et al., 2020; Patro et al., 2023; Zeitler et al., 2023), while others have reported that some children use the cochlear implant inconsistently or discontinue its use over time (Thomas et al., 2017). A third option in addition to CROS aids and cochlear implantation is the use of the bone-anchored hearing device described in the next section. As with the CROS aid, sound is not heard in the ear with hearing loss. The device simply picks up sound from that sound of the head and sends it to the cochlea with normal hearing via bone conduction. As with CROS aids, the use of BAHA for single-sided deafness provides better access to sound, but does not significantly improve localization or speech understanding in noise (Kubina et al., 2023).
Box 7. Highlights for educators and families.
The process of evaluating candidacy for cochlear implants is the responsibility of health care professionals, but families are involved every step of the way and have the final say in whether their child receives an implant or not. Families and educators play a crucial role in the candidacy evaluation process, gathering observational data on the child’s current functioning in terms of responses to sound and spoken language development. While educators may not be professionals who refer a child for a cochlear implant evaluation, they are sometimes the first to recognize how much a child is struggling with auditory access and spoken language development, even with hearing aids, and to make parents aware of cochlear implants as a possible option. It is crucial for families to understand the potential advantages and disadvantages of cochlear implantation for their child, information which is best provided by the professionals in the cochlear implant program. After the cochlear implant has been programmed, audiologists again rely on families and educators to provide functional data on how the child is responding to sound and progressing with spoken language. As with hearing aid fitting, cochlear implant programming involves a process of fine-tuning based on the observations of the people who spend the most time with the child. As with hearing aids, the adults in the child’s environment are initially responsible for ensuring that cochlear implants are being worn consistently, and for identifying when there is a problem or a need for a change in the cochlear implant’s programming.
5. Bone-Anchored Hearing Devices
Bone-anchored hearing aids (BAHAs), sometimes known as bone-conducted hearing aids (BCHAs), are used when the provision of sound through a conventional hearing aid is not possible. Most commonly, this is for children who are born without ear canals (a condition known as atresia), resulting in significant conductive hearing loss. The use of a conventional hearing aid is not possible because there is no outer or middle ear, and using a cochlear implant is not an option because the hearing loss is conductive, not sensorineural. Bone-anchored devices use a vibrator on the skull to send sound directly to the cochlea via vibration, effectively bypassing the outer and middle ear. Bone-anchored hearing devices are also used for older children and adults with very chronic ear infections, such that drainage from the ear canal makes it inadvisable to wear an earmold.
For the bone-anchored device to work, the vibrator/sound processor simply needs to be held against the skull. The most effective way to convey sound is to implant an internal component under the skin coupled to an external processor so that the sound processor is secure and does not slide around. This requires the implantation of a titanium piece which ultimately fuses with the bone of the skull through a process known as osseointegration. However, the bones of the skull must be thick enough to hold the titanium implant and, therefore, surgery is generally not performed until children are 4 to 5 years of age (see Kruyt et al., 2020 for a discussion of surgical issues). Infants and toddlers who are candidates for bone-anchored devices therefore wear the sound processor on a headband until they grow old enough for surgery (Bagatto et al., 2022; Roman et al., 2011). Both surgical and non-surgical options are described here.
5.1. Non-Surgical Options
Bone conduction hearing aids are not new technology; the original versions used a conventional hearing aid worn on one side of a headband which powered a bone conduction vibrator worn on the other side of the headband (Mudry & Tjellström, 2011). While these devices worked well for sound transmission, their use can be uncomfortable at times and cause headaches and they can slide out of place. However, they can still be a viable option where more current devices are not available.
These days, the bone-anchored device can be worn on a headband (see Figure 4).

Figure 4.
Bone-anchored device processor worn on a headband. https://www.cochlear.com/us/en/home/products-and-accessories/cochlear-baha-start, accessed 23 February 2025.
As noted, this wearing option is required for children under the age of 4 to 5 years of age until they are eligible for the required surgery. While older children can certainly continue to wear the bone-anchored device processor, it is less secure, tends to slide around, and is less cosmetically appealing; therefore, most eligible children receive surgery for the bone-anchored device.
5.2. Surgical Options
Bone-anchored devices that incorporate a surgically implanted component are based on the principle that the best sound transmission occurs when the device is coupled securely to the skull. The surgically implanted options can be divided into two categories—those using percutaneous transmission (meaning that there is an abutment that sits through the skin) and those using transcutaneous transmission (meaning that the internal component is covered by skin). Today’s bone-anchored devices uniformly use transcutaneous transmission. It should be noted that the different devices described here represent different stages in development, not clinician choices. Because the internal component becomes fused with the bones of the skull, it cannot be removed or replaced with a different bone-anchored device; therefore, educators and professionals may still work with older children and young adults who have percutaneous bone-anchored devices.
Percutaneous transmission, older bone-anchored devices used an implanted abutment to couple the processor to the skull. This type of implanted bone conduction device consists of three components. The first component is a titanium implant, which is surgically fitted into the skull around the mastoid area. This implant fuses with the bone over time, creating a stable anchor point.
The second component is a metal abutment that attaches to the titanium implant through the skin. The third component is the processor, which snaps onto the abutment. Once the processor is attached to the abutment, sound travels through the skull by vibrations and directly stimulates the inner ear. While sound quality is excellent when using a device with an abutment, skin infections sometimes occur, particularly if strict hygiene measures are not used, because the abutment sits through the skin (Shapiro et al., 2018).
Transcutaneous transmission, newer technology also uses an implanted component, but it sits under the skin, not through it. This type of device consists of an internal implanted magnet, a magnetic spacer, and a sound processor (see Figure 5). This option is more cosmetically appealing and does not present the same ongoing risks of infection as percutaneous implants.
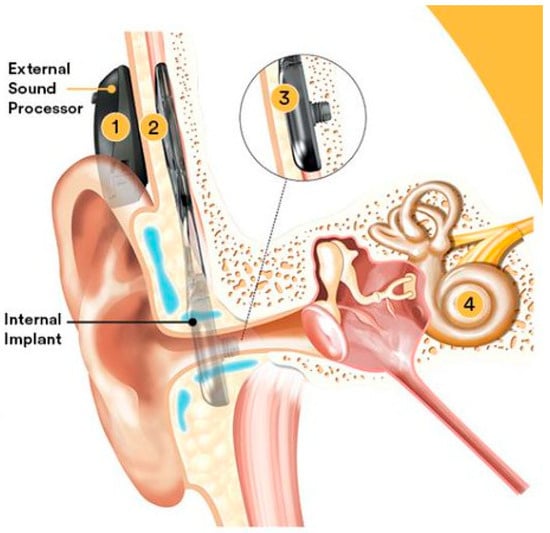
Figure 5.
Transcutaneous bone-anchored hearing device components. Component 1 is the external sound processor; components 2 and 3 are two parts of the internal implant, 4 indicates the location of the cochlea. Photo courtesy of Cochlear Inc.
Audiologists program bone-anchored devices via a computer in the way they would program hearing aids or cochlear implant processors, just using different measurements and based on different practice guidelines (Bagatto et al., 2022; Roman et al., 2011).
Box 8. Highlights for families and educators.
The majority of children using bone-anchored hearing devices have ear anomalies, which are readily identifiable at birth, meaning families know about the child’s hearing loss from birth. Bone-anchored hearing devices can be fitted very early and provide good access to spoken language, but close attention is required by parents to ensure that the device is always in place so that consistent access to sound is provided. Until children are old enough for the surgical option, the bone-anchored speech processor is usually worn on a headband, and processors can become prone to slipping or moving out of place. Preschool and kindergarten educators will likely have no experience with this type of device and will need support in understanding what the device is and to feel comfortable adjusting it throughout the school day so that children have consistent access to sound.
6. Less Common Implantable Devices
6.1. Auditory Brainstem Implants
Auditory brain stem implants (ABIs) have similar components to cochlear implants, but differ in that they directly stimulate the brainstem, bypassing the cochlea and auditory nerve.
Auditory brainstem implants are only considered for individuals who are not candidates for cochlear implants, and are typically used when the auditory nerve or cochlea are absent. Currently, there are very few recipients of ABIs worldwide because there are only a very small number of candidates, there can be significant complications associated with the surgery, and reported benefits associated with use are limited (Colletti et al., 2010). While ABIs can provide some auditory sensation, the quality of sound perception is reduced, as the brainstem processes auditory information differently from the inner ear. Success for children varies among individuals, and intensive rehabilitation is required to adapt to the new way of hearing (Behr et al., 2022; Colletti et al., 2010; Eisenberg et al., 2018; Fernandes et al., 2020; Martins et al., 2023; Teagle et al., 2018).
6.2. Hybrid Cochlear Implants Using Electro-Acoustic Stimulation
In the past, individuals with relatively good low-frequency hearing levels but severe hearing loss in the high-frequency range were not considered to be appropriate cochlear implant candidates because of fears that residual low-frequency hearing would be damaged. More recently, the use of both a hearing aid and a cochlear implant together in the same device has become an option, termed a hybrid cochlear implant. The electrode array is only inserted partially into cochlea, providing mid- to high-frequency sound while the hearing aid component amplifies low frequencies. The inner ear then processes the acoustic and electric stimuli simultaneously (Woodson et al., 2010). Results have shown good outcomes for adults, with a smaller research corpus for children reporting better speech recognition in quiet and in noise, better localization, improvements in sound quality, better music appreciation and aptitude, and better pitch recognition (Wolfe et al., 2017; Woodson et al., 2010).
7. Evaluating Benefit from Hearing Technology
As discussed previously, fitting hearing technology to children presents unique challenges, but can have profound detrimental effects on a child’s development if performed incorrectly or carelessly. In the face of sometimes incomplete audiological information and limited or no user feedback to guide them, audiologists must determine the best hearing technology device for a child and assess continuous benefit. This is the “validation” stage of the fitting process, and requires us to gather information from the child’s life outside of the audiology clinic, both at home and school and in the community. How can this information be gathered?
7.1. Datalogging
Many of today’s hearing technologies contain a feature called datalogging, which automatically records information from the device, including hours per day of usage time, the characteristics of the listening environment (e.g., noise levels), volume adjustments made by the user or by the hearing aid itself, and battery usage. H. Ganek et al. (2021) found that datalogging accurately describes and represents the listening environments that children are engaged in over the course of a day. Datalogging can help identify factors that may be contributing to poor outcomes for a child (such as the inconsistent use of devices, or only wearing devices at school and not at home) (Easwar et al., 2016, 2018; Gustafson et al., 2017).
7.2. Functional Hearing Assessment
Erber (1982) described a framework for evaluating how a child with hearing loss uses the residual hearing available to them, dubbed the auditory skills hierarchy; using the auditory skills hierarchy can help us determine how clearly a child hears with technology, as well as whether a child is progressing to a higher level of auditory skill and spoken language over time. The auditory skills hierarchy consists of four levels, based on the premise that children can perform increasingly difficult listening tasks through focused practice and attention. As such, it can be used by parents and professionals to help evaluate whether a child is using their residual hearing effectively. The four levels are as follows: (i) detection, meaning the ability to recognize when a sound is present but not implying recognition or understanding of the sound; (ii) discrimination, differentiating between two sounds by identifying if the sounds are the same or different; (iii) identification, recognizing and identifying specific sounds or words (for example, by pointing to a picture of a word); and (iv) comprehension, understanding the meaning of spoken sounds, words, sentences, and conversation. Children who are able to use their hearing technology to access and understand auditory information should be able to progress through these stages quickly.
The issue of functional hearing assessment for infants, toddlers, and preschoolers persists. How do we know if children are learning to use their hearing to acquire language if we fit amplification before they can talk? Audiologists and other professionals will need to rely on parent observation and reports to assess what is happening when families leave the audiology clinic. This requires good early intervention and communication development support services, not only to learn how to use the devices and identify problems, but also to be careful observers of auditory behavior and language development. A number of instruments have been developed to help parents accomplish this. These include standardized parent interview tools and questionnaires such as the Infant-Toddler Meaningful Auditory Integration Scale (IT-MAIS) (Zimmerman-Phillips et al., 1997), the LittlEars Auditory Questionnaire (Tsiakpini et al., 2004), and the Parent Evaluation of Auditory/Oral Performance of Children (PEACH) (Ching & Hill, 2007). These questionnaires are available in many different languages. They sometimes have apps associated with them for ease of use, as well as parent diaries to help parents track their child’s progress.
Functional hearing assessment for school-aged children is pertinent. There is a great deal of valuable information to be gained by observing a child in his/her classroom, and from asking classroom teachers for their observations in evaluating benefit from hearing technology. Checklists can help a classroom teacher focus on the specific auditory behaviors of interest. Functional speech perception testing, where the student is asked to perform a variety of listening tasks (e.g., repeating back a list of words in the presence of background noise), can identify situations that present difficulty for the student. Asking a student through conversation or using a published questionnaire to assess their perspective is also valuable. Published checklists and observational tools are readily accessible online through websites such as Success for Kids with Hearing Loss (successforkidswithhearingloss.com) and The Online Itinerant (theonlineitinerant.com).
The topic of listening fatigue is an emerging research focus for children (Bess et al., 2014, 2020; Davis et al., 2021; Hornsby et al., 2021; Sindhar et al., 2021). Listening fatigue can occur in any situation, but tends to be more common in difficult listening situations (such as in a noisy classroom or daycare setting). While hearing technology improves access to the speech signal, that access can still be reduced by distance, noise, and reverberation, and consideration should be given to the addition of access technologies such as remote microphones (Millett, 2023).
Box 9. Highlights for educators and families.
Since families and educators often do not have quantitative test results that indicate how well a child hears while using hearing technology, the best way to gather this information is through functional hearing assessment. As noted, there are a wide variety of questionnaires and tools available to help gather this information. The websites provided above also describe a variety of listening activities that one could perform with a child to develop an understanding of how well the child hears (e.g., repeating a list of words at a close distance versus from several feet away). For all individuals with hearing loss, speech understanding deteriorates under adverse listening conditions (such as with distance, noise, or reverberation). Functional hearing assessment allows educators and families to explore the child’s auditory functioning under a variety of listening conditions. It is more informal and less standardized than audiological assessment, but has the advantage of being conducted under a variety of natural listening conditions that occur for that child.
8. Barriers to Use of Hearing Technologies
8.1. Cost
As noted previously, access to hearing health care services for the diagnosis of hearing loss and prescription of hearing aids is a huge problem in under-resourced countries (World Health Organization [WHO], 2021). Even where services exist, cost can represent a significant barrier. Cost varies widely between hearing aids, cochlear implants, and bone-anchored devices, but none of these are inexpensive (Valente & Amlani, 2017). While there can be financial support for these devices, this is very jurisdiction-specific and often tied into service delivery models of payment for health care services in general. Even where financial support for the initial purchase of hearing technology is available, it often does not extend to ongoing costs related to daily use, maintenance, and repairs (e.g., replacing earmolds when a child’s ears grow). Financial assistance for hearing technology is very much related to the structure of health care funding, and therefore varies widely, even among resourced countries.
Cochlear implantation and bone-anchored device implantation add an additional cost, that of the surgery, to the cost of the device. Bodington et al. (2021) note that, in under-resourced countries, the cost of the device (first time and ongoing costs) is the larger barrier. In some countries, cochlear implant surgery is relatively accessible, but the crucial programming and intensive rehabilitative services that are required after surgery are not. Some countries provide cochlear implantation for children on a fee-for-service basis, so that families can travel to another country to have the surgery performed and the device programmed, after which families return to their own country, which may be under-resourced in terms of rehabilitation services.
8.2. Issues for Immigrant Families
Challenges for deaf children in under-resourced countries in terms of access to technology are immense. Indeed, access to technology can be limited or non-existent. It is not uncommon for families to immigrate to countries with more resources, hoping to find better services for their deaf child (Akamatsu & Cole, 2004). Pape et al. (2014) note that in the United States, accurate data regarding the number of immigrant children with hearing loss are not available and that any data that do exist likely significantly underestimate this number.
It is important to acknowledge that significant challenges continue to exist upon arrival in the new country (Jaradeh et al., 2023). Children may arrive with hearing loss that is either undiagnosed, or diagnosed but without access to hearing technology, presenting challenges to both the hearing health care and educational systems (Ligny et al., 2018). Parents may have unrealistic expectations about their deaf child’s potential to use hearing technology; parents may be disappointed to learn that their deaf teenager who has never used hearing technology is not, in fact, a cochlear implant candidate. Or they may have very different perspectives, attitudes, and experiences with deafness, leading to challenging relationships with health care or education professionals in their new context (Akamatsu & Cole, 2004; Krasniqi et al., 2022).
8.3. Stigma, Self-Esteem and Self-Advocacy
The issue of stigma related to hearing technologies has been widely discussed in the adult literature (see Ritter et al., 2020, for a review). The term “hearing aid effect” was coined by G. W. Blood et al. (1977) to describe a phenomenon where people assign negative attributes to individuals with hearing aids. In their study, adults rating young children with and without hearing aids assigned negative attributes to children pictured with hearing aids. This topic has been revisited in recent years, with studies finding less evidence of this phenomenon (I. M. Blood, 1997; Cienkowski & Pimentel, 2001; Johnson et al., 2005; Rauterkus & Palmer, 2014). However, just because others do not have negative reactions to the use of hearing aid technology by others, does not mean that users themselves do not struggle with the fact that hearing technology is a visible indicator of their hearing loss. The literature on stigma and hearing technology for children is extremely small, but a small body is emerging for teens. This suggests that the problem of stigma still exists and can contribute to the discontinuation of hearing technology use (Kent & Smith, 2006; Rauterkus & Palmer, 2014; Ryan et al., 2006; Strange et al., 2008).
However, wearing hearing technology is not always seen as a negative by users; Profita et al. (2018) analyzed discussions by young adults in online forums around customizing hearing technology (i.e., using colors, adding decorations, etc.). They found that participants listed many reasons for customizing their devices to make them more noticeable, including demonstrating agency, expressing oneself in a creative way, expressing pride and confidence, promoting disability advocacy, raising awareness of hearing loss, and finding community.
8.4. Support for Management and Troubleshooting of Hearing Technology
Luterman and Kurtzer-White (1999) noted that, prior to universal newborn hearing screening, the diagnosis of hearing loss was driven by parents (i.e., parents were the first to suspect hearing loss, not health care professionals), and now, diagnosis is driven by the technology and the health care system. With universal newborn screening, parents are faced with a diagnosis of hearing loss when their baby is only weeks old. This is not an argument against newborn hearing screening, but is simply to emphasize the need for hearing health care professionals to keep in mind the amount of stress that families face in navigating the complex array of health care and intervention services (Wiseman et al., 2021). Luterman (2007) goes on to note that as the technology increases in complexity, the amount of information that parents need to understand is enlarged and the decisions that parents need to make (e.g., making choices about cochlear implantation) also increase in complexity.
Parents will be the primary managers of hearing technology until the child is at least of school age. This not only means that parents need to know how to use the device (turning it on and off, inserting earmolds or putting on cochlear implant coils, charging batteries, etc.), but that they are also responsible for implementing and maintaining consistent daily device use. Responsibility for keeping devices on the head of a fussy baby or active toddler falls to parents and family members. At the same time, parents are learning how to facilitate language development for their child and are asked to be responsible for observing and reporting on benefits and challenges to health care and education professionals. They need to ensure that the devices are working properly, identify when they are not, and know what to do to have them looked at. As noted previously, children may or may not have the auditory or language skills to identify malfunctioning technology and report it to an adult for help; therefore, responsibility for ensuring access to spoken language falls on families. Parents’ abilities to manage all of these tasks, in addition to job, family, and daily living activities, will vary considerably. Professionals need to be sensitive to the demands placed on the families of children with hearing loss (K. Munoz et al., 2014; K. F. Munoz et al., 2019; Preston et al., 2017).
Once children reach school age, teachers and school staff also become involved in supporting the consistent use of hearing technology and will have questions and concerns that need to be addressed by teachers of the deaf and hard of hearing and by educational audiologists (Davenport & Alber-Morgan, 2016). While hearing technology generally owned by families and not directly the responsibility of the classroom teacher, learning is likely to be at least compromised and at worst impossible if a child is unable to access classroom instruction because their hearing technology is not working. Assistive technology may be used in the classroom to support auditory access such as FM systems, passaround microphones, or remote microphones, and it is important for parents to have at least a working knowledge of this technology to ensure that the student’s own personal hearing aids, cochlear implants, or bone-anchored devices can interface appropriately with classroom technology (see Millett, 2023 for a discussion of assistive listening technology for students with hearing loss).
Box 10. Highlights for educators and families.
Families face many unexpected challenges when children use hearing technology. These not only include paying for and learning about technology that is completely new to them, but also having the primary responsibility of ensuring that children are using it as many hours a day as possible. For families who are new immigrants, these responsibilities are added to the already significant challenges of settling in a new country, navigating health care and educational obstacles for their child, learning a new language, and finding housing, employment, and community. Schools are often uniquely equipped to support new immigrant families; many school districts employ settlement workers and can connect families to services and support, both at school and in the community. This can include connecting them with other families of deaf or hard-of-hearing children in the school district, which provides for social and emotional support through peers. School staff can also be important support for student adjustment, socialization, and mental health struggles.
9. The Future of Hearing Technologies
9.1. Artificial Intelligence (AI)
Research and development by hearing device manufacturers is focused on maximizing access to sound, and particularly on ensuring effective communication in a wide variety of listening conditions for a wide variety of users. However, to a certain extent, it is a “one-size-fits-all” strategy. Artificial intelligence allows for the potential individualization of acoustical characteristics, in essence providing a “trainable” hearing aid (Umashankar et al., 2021). Developers can also make use of large data sets compiled from shared user data to evaluate and improve features (Balling et al., 2021; Fabry & Bhowmik, 2021).
9.2. Teleaudiology
Teleaudiology, which provides families with access to audiologists for hearing testing and hearing technology fitting and follow-up services through videoconferencing, offers various benefits that enhance the accessibility, convenience, and quality of audiological care. With advancements largely driven by the COVID-19 pandemic, it is now possible to assess hearing and program hearing technologies remotely, improving accessibility and convenience for families (Eikelboom et al., 2022; Ramos et al., 2009; Slager et al., 2019). Continuity of care is improved when families can access services and information, resources, and educational materials more easily and consistently. Interest in, and access to, teleaudiology has increased due to the COVID-19 pandemic. Teleaudiology may not be suitable for all cases, especially those requiring physical examinations or specific diagnostic procedures that necessitate in-person assessment. Additionally, reliable Internet connectivity and technology access are critical for successful teleaudiology implementation.
9.3. Over the Counter Hearing Aids
Over-the-counter (OTC) hearing aids are a relatively recent offering of the market. They are intended to allow adults to purchase inexpensive hearing devices over the Internet without an audiological assessment and without a prescription from an audiologist or physician. They have been approved for sale by some jurisdictions (e.g., the United States), but not others (e.g., Canada), and so access to these devices depends on the patient’s geographical location. Once purchased, these devices are adjusted by the user using manual controls or an app to determine appropriate settings. Research into potential advantages, disadvantages, and risk of harm is just beginning to emerge, and audiologists’ views on this new practice for adult patients are mixed (Manchaiah et al., 2023). Government agencies regulating OTC hearing aids have been clear that these devices are only intended for adults over the age of 18. However, as they are purchased over the Internet, it is possible for a parent to purchase such a device for a child. There is clear consensus among hearing health care professionals that OTC hearing aids should not be purchased for, or fit on, a child due to significant risk of harm (American Academy of Audiology, 2018; American Academy of Otolaryngology, Head and Neck Surgery, 2021; Canadian Academy of Audiology, 2022).
A variation in this technology is the inclusion of hearing aid features into an existing consumer audio device, such as the hearing aid option in Apple AirPods Pro 2TM devices. This feature allows consumers to use their AirPodsTM to perform a hearing self-test on an app and allows the device to program appropriate hearing aid settings. While there are hearing health care professional reviews on this product on the Internet, as of yet there are not any published research studies or clinical practice guidelines. However, the same cautions should apply around the use of technology, such as AirPodsTM, as replacements for hearing aids for children as exist for OTC hearing aids.
Hearing technologies will continue to evolve in effectiveness, but also in complexity.
10. Conclusions
Hearing technology has come a long way since the development of the first hearing aids in the post-World War 2 era, and outcomes for deaf children in language, literacy and communication continue to improve as more children have better access to spoken language through its use. Ensuring success for children using hearing technology requires a partnership between health care professionals such as audiologists, educators in schools, and families, and attention needs to be paid to ensure that everyone has the necessary knowledge and skills to ensure consistent auditory access. Hearing technology provides children with access to the auditory world not only at home and in the classroom, but also in the gym, on the playground, on field trips, on the football field, and even in the pool—anywhere they are in communication with others. The remarkable access to sound that modern hearing technology can provide across a wide range of daily activities and communication situations is only possible, however, when parents and educators have a good understanding of why, when, and how the technology is used and are able to support children in its use.
Author Contributions
Conceptualization, I.M. and P.M.; writing—original draft preparation, I.M.; writing—P.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Akamatsu, C. T., & Cole, E. (2004). Deaf immigrant and refugee children: Institutional and cultural clash. In Literacy and deaf people: Cultural and contextual perspectives (pp. 110–138). Gallaudet University Press. [Google Scholar]
- American Academy of Audiology. (2018). Children and over the counter hearing aids. Available online: https://www.audiology.org/consumers-and-patients/children-and-hearing-loss/children-and-over-the-counter-hearing-aids/#:~:text=Both%20FDA%20regulations%20as%20well,children%20younger%20than%20age%2018 (accessed on 23 February 2025).
- American Academy of Audiology. (2019). Clinical practice guideline: Cochlear implants. Available online: https://www.audiology.org/news-and-publications/audiology-today/articles/academy-news-clinical-practice-guidelines-for-cochlear-implants-now-available/ (accessed on 23 February 2025).
- American Academy of Otolaryngology, Head and Neck Surgery. (2021). AAO-HNS summary: FDA over-the-counter hearing aids final rule. Available online: https://www.entnet.org/advocacy/regulatory-advocacy/over-the-counter-sale-of-hearing-aids/aao-hns-summary-fda-over-the-counter-hearing-aids-final-rule/ (accessed on 23 February 2025).
- ANSI. (1997). Methods for calculation of the speech intelligibility index. ANSI S3.5-1997. American National Standards Institute. [Google Scholar]
- Appachi, S., Specht, J. L., Raol, N., Lieu, J. E., Cohen, M. S., Dedhia, K., & Anne, S. (2017). Auditory outcomes with hearing rehabilitation in children with unilateral hearing loss: A systematic review. Otolaryngology–Head and Neck Surgery, 157(4), 565–571. [Google Scholar] [CrossRef]
- Awad, R., Oropeza, J., & Uhler, K. M. (2019). Meeting the Joint Committee on Infant Hearing Standards in a large metropolitan children’s hospital: Barriers and next steps. American Journal of Audiology, 28(2), 251–259. [Google Scholar] [CrossRef] [PubMed]
- Bagatto, M., Gordey, D., Brewster, L., Brown, C., Comeau, M., Douglas, C., & Wollet, A. (2022). Clinical consensus document for fitting non-surgical transcutaneous bone conduction hearing devices to children. International Journal of Audiology, 61(7), 531–538. [Google Scholar] [CrossRef] [PubMed]
- Balling, L. W., Mølgaard, L. L., Townend, O., & Nielsen, J. B. B. (2021). The collaboration between hearing aid users and artificial intelligence to optimize sound. Seminars in Hearing, 42(3), 282–294. [Google Scholar] [CrossRef]
- Bangs, J. L., & Bangs, T. E. (1952). Hearing aids for young children. AMA Archives of Otolaryngology, 55(5), 528–535. [Google Scholar] [CrossRef]
- Barreira-Nielsen, C., Fitzpatrick, E., Hashem, S., Whittingham, J., Barrowman, N., & Aglipay, M. (2016). Progressive hearing loss in early childhood. Ear and Hearing, 37(5), e311–e321. [Google Scholar] [CrossRef]
- Behr, R., Schwager, K., & Hofmann, E. (2022). Auditory brainstem implants—Hearing restoration in congenitally deaf children. Deutsches Ärzteblatt International, 119(9), 135. [Google Scholar] [CrossRef] [PubMed]
- Belsare, G., Sarda, S., Bhardwaj, P., & Belsare, S. (2020). Comparison of speech perception abilities of children using bimodal hearing with children using cochlear implant alone. Annals of Otology and Neurotology, 3(2), 72–76. [Google Scholar] [CrossRef]
- Bernstein, L. E., Demorest, M. E., & Tucker, P. E. (2000). Speech perception without hearing. Perception and Psychophysics, 62, 233–252. [Google Scholar] [CrossRef]
- Berry, G. (1948). Hearing aids: The evaluation and practicability of hearing aids, with review of recent literature. Annals of Otology, Rhinology & Laryngology, 57(2), 500–508. [Google Scholar]
- Bess, F. H., Davis, H., Camarata, S., & Hornsby, B. W. (2020). Listening-related fatigue in children with unilateral hearing loss. Language, Speech, and Hearing Services in Schools, 51(1), 84–97. [Google Scholar] [CrossRef] [PubMed]
- Bess, F. H., Gustafson, S. J., & Hornsby, B. W. (2014). How hard can it be to listen? Fatigue in school-age children with hearing loss. Grantee Submission, 20, 1–14. [Google Scholar]
- Bisgaard, N., Zimmer, S., Laureyns, M., & Groth, J. (2022). A model for estimating hearing aid coverage world-wide using historical data on hearing aid sales. International Journal of Audiology, 61(10), 841–849. [Google Scholar] [CrossRef]
- Blood, G. W., Blood, I. M., & Danhauer, J. L. (1977). The hearing aid effect. Hearing Instruments, 28(6), 12. [Google Scholar]
- Blood, I. M. (1997). The hearing aid effect: Challenges for counseling. The Journal of Rehabilitation, 63(4), 59–63. [Google Scholar]
- Bodington, E., Saeed, S. R., Smith, M. C., Stocks, N. G., & Morse, R. P. (2021). A narrative review of the logistic and economic feasibility of cochlear implants in lower-income countries. Cochlear Implants International, 22(1), 7–16. [Google Scholar] [CrossRef]
- Brookhouser, P. E. (2002). Fluctuating sensorineural hearing loss in children. Otolaryngologic Clinics of North America, 35(4), 909–923. [Google Scholar] [CrossRef]
- Brown, K. D., Dillon, M. T., & Park, L. R. (2022). Benefits of cochlear implantation in childhood unilateral hearing loss (CUHL trial). The Laryngoscope, 132, S1–S18. [Google Scholar] [CrossRef] [PubMed]
- Browning, J. M., Buss, E., Flaherty, M., Vallier, T., & Leibold, L. J. (2019). Effects of adaptive hearing aid directionality and noise reduction on masked speech recognition for children who are hard of hearing. American Journal of Audiology, 28(1), 101–113. [Google Scholar] [CrossRef]
- Canadian Academy of Audiology. (2022). Canadian academy of audiology position statement on over-the-counter hearing aids. Available online: https://canadianaudiology.ca/wp-content/uploads/2025/04/Canadian-Academy-of-Audiology-Position-Statement-on-Over-The-Counter-devices-and-Sound-Amplifying-Products.pdf (accessed on 14 October 2024).
- Carlson, M. L., Sladen, D. P., Haynes, D. S., Driscoll, C. L., DeJong, M. D., Erickson, H. C., Sunderhaus, L. W., Hedley-Williams, A., Rosenzweig, E. A., Davis, T. J., & Gifford, R. H. (2015). Evidence for the expansion of pediatric cochlear implant candidacy. Otology & Neurotology, 36, 43–50. [Google Scholar]
- Ching, T. Y. C., Dillon, H., Hou, S., Zhang, V., Day, J., Crowe, K., & Thomson, J. (2013). A randomized controlled comparison of NAL and DSL prescriptions for young children: Hearing-aid characteristics and performance outcomes at three years of age. International Journal of Audiology, 52(Suppl. 2), S17–S28. [Google Scholar] [CrossRef]
- Ching, T. Y. C., Dillon, H., Leigh, G., & Cupples, L. (2018a). Learning from the longitudinal outcomes of children with hearing impairment (LOCHI) study: Summary of 5-year findings and implications. International Journal of Audiology, 57(Suppl. 2), S105–S111. [Google Scholar] [CrossRef] [PubMed]
- Ching, T. Y. C., & Hill, M. (2007). The parent’s evaluation of aural/oral performance of children (PEACH) scale: Normative data. Journal of the American Academy of Audiology, 18(3), 220–235. [Google Scholar] [CrossRef]
- Ching, T. Y. C., Incerti, P., Hill, M., & Van Wanrooy, E. (2006). An overview of binaural advantages for children and adults who use binaural/bimodal hearing devices. Audiology and Neurotology, 11(Suppl. 1), 6–11. [Google Scholar] [CrossRef]
- Ching, T. Y. C., & Leigh, G. (2020). Considering the impact of universal newborn hearing screening and early intervention on language outcomes for children with congenital hearing loss. Hearing, Balance and Communication, 18(4), 215–224. [Google Scholar] [CrossRef]
- Ching, T. Y. C., Zhang, V. W., Johnson, E. E., Van Buynder, P., Hou, S., Burns, L., & McGhie, K. (2018b). Hearing aid fitting and developmental outcomes of children fit according to either the NAL or DSL prescription: Fit-to-target, audibility, speech and language abilities. International Journal of Audiology, 57(Suppl. 2), S41–S54. [Google Scholar] [CrossRef] [PubMed]
- Cienkowski, K. M., & Pimentel, V. (2001). The hearing aid ‘effect’ revisited in young adults. British Journal of Audiology, 35(5), 289–295. [Google Scholar] [CrossRef]
- Ciocco, A., & Palmer, C. E. (1941). The hearing of school children. A statistical study of audiometric and clinical records. Monographs of the Society for Research in Child Development, 6(3), i-77. [Google Scholar] [CrossRef]
- Colletti, V., Shannon, R., Carner, M., Veronese, S., & Colletti, L. (2010). Complications in auditory brainstem implant surgery in adults and children. Otology and Neurotology, 31(4), 558–564. [Google Scholar] [CrossRef]
- CRIDE. (2024). 2024 UK-wide summary: Education provision for deaf children in 2023/24. Retrieved from 2024 UK-wide summary education provision for deaf children in 2023/24. Available online: https://www.ndcs.org.uk/media/9606/cride-2024-uk-summary-final.pdf (accessed on 25 February 2025).
- Davenport, C. A., & Alber-Morgan, S. R. (2016). I have a child with a cochlear implant in my preschool classroom. Now What? Teaching Exceptional Children, 49(1), 41–48. [Google Scholar] [CrossRef]
- Davis, H., Schlundt, D., Bonnet, K., Camarata, S., Hornsby, B., & Bess, F. H. (2021). Listening-related fatigue in children with hearing loss: Perspectives of children, parents, and school professionals. American Journal of Audiology, 30(4), 929–940. [Google Scholar] [CrossRef]
- Durieux-Smith, A., Fitzpatrick, E., & Whittingham, J. (2008). Universal newborn hearing screening: A question of evidence. International Journal of Audiology, 47(1), 1–10. [Google Scholar] [CrossRef]
- Easwar, V., Sanfilippo, J., Papsin, B., & Gordon, K. (2016). Factors affecting daily cochlear implant use in children: Datalogging evidence. Journal of the American Academy of Audiology, 27(10), 824–838. [Google Scholar] [CrossRef] [PubMed]
- Easwar, V., Sanfilippo, J., Papsin, B., & Gordon, K. (2018). Impact of consistency in daily device use on speech perception abilities in children with cochlear implants: Datalogging evidence. Journal of the American Academy of Audiology, 29(9), 835–846. [Google Scholar] [CrossRef]
- Eikelboom, R. H., Bennett, R. J., Manchaiah, V., Parmar, B., Beukes, E., Rajasingam, S. L., & Swanepoel, D. W. (2022). International survey of audiologists during the COVID-19 pandemic: Use of and attitudes to telehealth. International Journal of Audiology, 61(4), 283–292. [Google Scholar] [CrossRef]
- Eisenberg, L. S., Hammes Ganguly, D., Martinez, A. S., Fisher, L. M., Winter, M. E., Glater, J. L., & Los Angeles Pediatric ABI Team. (2018). Early communication development of children with auditory brainstem implants. The Journal of Deaf Studies and Deaf Education, 23(3), 249–260. [Google Scholar] [CrossRef] [PubMed]
- Erber, N. (1982). Auditory training. Alexander Graham Bell Association for the Deaf. [Google Scholar]
- Fabry, D. A., & Bhowmik, A. K. (2021). Improving speech understanding and monitoring health with hearing aids using artificial intelligence and embedded sensors. Seminars in Hearing, 42(3), 295–308. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, N. F., Gomes, M. D. Q. T., Tsuji, R. K., Bento, R. F., & Goffi-Gomez, M. V. S. (2020). Auditory and language skills in children with auditory brainstem implants. International Journal of Pediatric Otorhinolaryngology, 132, 110010. [Google Scholar] [CrossRef]
- Fernandez-Lopez, A., Martinez, O., & Sukno, F. M. (2017, May 30–June 3). Towards estimating the upper bound of visual-speech recognition: The visual lip-reading feasibility database. 2017 12th IEEE International Conference on Automatic Face & Gesture Recognition (FG 2017) (pp. 208–215), Washington, DC, USA. [Google Scholar]
- Fisher, B. (1964). An investigation of binaural hearing aids. The Journal of Laryngology & Otology, 78(7), 658–668. [Google Scholar]
- Fitzpatrick, E. M., McCurdy, L., Whittingham, J., Rourke, R., Nassrallah, F., Grandpierre, V., & Bijelic, V. (2021). Hearing loss prevalence and hearing health among school-aged children in the Canadian Arctic. International Journal of Audiology, 60(7), 521–531. [Google Scholar] [CrossRef]
- Fliegelman, J. (2020). What role does age-associated neuroplasticity play in the efficacy of cochlear implantation? The Science Journal of the Lander College of Arts and Sciences, 14(1), 14–21. [Google Scholar]
- Ganek, H., Forde-Dixon, D., Cushing, S. L., Papsin, B. C., & Gordon, K. A. (2021). Cochlear implant datalogging accurately characterizes children’s ‘auditory scenes’. Cochlear Implants International, 22(2), 85–95. [Google Scholar] [CrossRef] [PubMed]
- Ganek, H. V., Cushing, S. L., Papsin, B. C., & Gordon, K. A. (2020). Cochlear implant use remains consistent over time in children with single-sided deafness. Ear and Hearing, 41(3), 678–685. [Google Scholar] [CrossRef]
- Gardner, W. H. (1943). History and present status of the education of the hard of hearing. Journal of Speech Disorders, 8(3), 227–236. [Google Scholar] [CrossRef]
- Gifford, R. H. (2020). Bilateral cochlear implants or bimodal hearing for children with bilateral sensorineural hearing loss. Current Otorhinolaryngology Reports, 8, 385–394. [Google Scholar] [CrossRef]
- Gustafson, S. J., & Corbin, N. E. (2021). Pediatric hearing loss guidelines and consensus statements—Where do we stand? Otolaryngologic Clinics of North America, 54(6), 1129–1142. [Google Scholar] [CrossRef]
- Gustafson, S. J., Ricketts, T. A., & Tharpe, A. M. (2017). Hearing technology use and management in school-age children: Reports from data logs, parents, and teachers. Journal of the American Academy of Audiology, 28(10), 883–892. [Google Scholar] [CrossRef] [PubMed]
- Harrison, R., Gordon, K., & Mount, R. (2005). Is there a critical period for cochlear implantation in congenitally deaf children? Analyses of hearing and speech perception performance after implantation. Developmental Psychobiology, 46(3), 252–261. [Google Scholar] [CrossRef]
- Holden-Pitt, L., & Diaz, J. A. (1998). Thirty years of the Annual Survey of Deaf and Hard-of-Hearing Children & Youth: A glance over the decades. American Annals of the Deaf, 143(2), 71–76. [Google Scholar]
- Holder, J. T., Holcomb, M. A., Snapp, H., Labadie, R. F., Vroegop, J., Rocca, C., & Gifford, R. H. (2022). Guidelines for best practice in the audiological management of adults using bimodal hearing configurations. Otology & Neurotology Open, 2(2), e011. [Google Scholar]
- Hornsby, B. W., Davis, H., & Bess, F. H. (2021). The impact and management of listening-related fatigue in children with hearing loss. Otolaryngologic Clinics of North America, 54(6), 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Hyde, M. L. (2005). Newborn hearing screening programs: Overview. Journal of Otolaryngology, 34(2), S70. [Google Scholar] [PubMed]
- Jaradeh, K., Liao, E. N., Chehab, L. Z., Tebb, K. P., Florentine, M. M., Bellfort-Salinas, S., & Chan, D. K. (2023). Understanding barriers to timely diagnosis and intervention among immigrant children with hearing loss. Otolaryngology–Head and Neck Surgery, 169(3), 701–709. [Google Scholar] [CrossRef]
- Johnson, C. E., Danhauer, J. L., Gavin, R. B., Karns, S. R., Reith, A. C., & Lopez, I. P. (2005). The “hearing aid effect” 2005: A rigorous test of the visibility of new hearing aid styles. American Journal of Audiology, 14(2), 169–175. [Google Scholar] [CrossRef] [PubMed]
- Joint Committee on Infant Hearing. (2019). Year 2019 position statement: Principles and guidelines for early hearing detection and intervention programs. Journal of Early Hearing Detection and Intervention, 4, 1–44. [Google Scholar]
- Kemp, D. T., Ryan, S., & Bray, P. (1990). A guide to the effective use of otoacoustic emissions. Ear and Hearing, 11(2), 93–105. [Google Scholar] [CrossRef]
- Kemper, E., Willis, K., & Simpson, A. (2021). ‘When you are on your own, everything is your responsibility’: Experiences of audiologists and audiometrists working in rural Australia. Australian Journal of Rural Health, 29(3), 382–390. [Google Scholar] [CrossRef]
- Kent, B., & Smith, S. (2006). They only see it when the sun shines in my ears: Exploring perceptions of adolescent hearing aid users. Journal of Deaf Studies and Deaf Education, 11(4), 461–476. [Google Scholar] [CrossRef]
- Kral, A., & Sharma, A. (2012). Developmental neuroplasticity after cochlear implantation. Trends in Neurosciences, 35(2), 111–122. [Google Scholar] [CrossRef]
- Krasniqi, R., Musyoka, M. M., Msengi, C., & Appanah, T. (2022). Untold stories of US immigrant mothers of D/HH children. International Research and Review, 12(1), 3–17. [Google Scholar]
- Kruyt, I. J., Bakkum, K. H. E., Caspers, C. J. I., & Hol, M. K. S. (2020). The efficacy of bone-anchored hearing implant surgery in children: A systematic review. International Journal of Pediatric Otorhinolaryngology, 132, 109906. [Google Scholar] [CrossRef] [PubMed]
- Kubina, M., Fornwalt, B., Patel, S., Sharma, B., & Jeyakumar, A. (2023). Comparison of treatment modalities for single-sided deafness in paediatric patients. The Journal of Laryngology & Otology, 137(7), 725–731. [Google Scholar]
- Kwak, S. H., Kim, D., Bae, S. H., Moon, I. S., Kim, S. H., Choi, J. Y., & Jung, J. (2021). Effects of contralateral routing of signal hearing aids on audiological and academic performance in school-age children with unilateral hearing loss. Clinical and Experimental Otorhinolaryngology, 14(3), 355–358. [Google Scholar] [CrossRef]
- Ligny, C., Ciardelli, R., Simon, P., Van Vlierberghe, C., Vandevoorde, A., Marquet, T., & Mansbach, A. L. (2018). How to manage immigrant children with cochlear implants? Our experience in Brussels, a multicultural city. Journal of Hearing Science, 8(2), 84. [Google Scholar]
- Luterman, D. (2007). Technology and early childhood deafness. The ASHA Leader, 12(6), 43. [Google Scholar] [CrossRef]
- Luterman, D., & Kurtzer-White, E. (1999). Identifying hearing loss. ASHA Leader, 8(1), 13–18. [Google Scholar] [CrossRef]
- Macfarlan, D. (1939). History of audiometry. Archives of Otolaryngology, 29(3), 514–519. [Google Scholar] [CrossRef]
- Manchaiah, V., Sharma, A., Rodrigo, H., Bailey, A., De Sousa, K. C., & Swanepoel, D. W. (2023). Hearing healthcare professionals’ views about over-the-counter (OTC) hearing aids: Analysis of retrospective survey data. Audiology Research, 13(2), 185–195. [Google Scholar] [CrossRef] [PubMed]
- Martins, Q. P., Gindri, B. D. F. S., Valim, C. D., Ferreira, L., & Patatt, F. S. A. (2023). Hearing and language development in children with brainstem implants: A systematic review. Brazilian Journal of Otorhinolaryngology, 88, 225–234. [Google Scholar] [CrossRef]
- McCreery, R. W., Venediktov, R. A., Coleman, J. J., & Leech, H. M. (2012). An evidence-based systematic review of directional microphones and digital noise reduction hearing aids in school-age children with hearing loss. American Journal of Audiology, 21(2), 295–312. [Google Scholar] [CrossRef]
- McCreery, R. W., & Walker, E. A. (2017). Hearing aid candidacy and feature selection for children. In Pediatric amplification: Enhancing auditory access (pp. 51–76). Plural Publishing. [Google Scholar]
- McCreery, R. W., Walker, E. A., Spratford, M., Bentler, R., Holte, L., Roush, P., & Moeller, M. P. (2015). Longitudinal predictors of aided speech audibility in infants and children. Ear and Hearing, 36, 24S. [Google Scholar] [CrossRef] [PubMed]
- McCreery, R. W., Walker, E. A., Stiles, D. J., Spratford, M., Oleson, J. J., & Lewis, D. E. (2020). Audibility-based hearing aid fitting criteria for children with mild bilateral hearing loss. Language, Speech, and Hearing Services in Schools, 51(1), 55–67. [Google Scholar] [CrossRef]
- Messersmith, J. J., Entwisle, L., Warren, S., & Scott, M. (2019). Clinical practice guidelines: Cochlear implants. Journal of the American Academy of Audiology, 30(10), 827–844. [Google Scholar] [CrossRef] [PubMed]
- Millett, P. (2023). The Connected Life: Using access technology at home, at school and in the community. Education Sciences, 13(8), 761. [Google Scholar] [CrossRef]
- Moeller, M. P., & Tomblin, J. B. (2015). An introduction to the outcomes of children with hearing loss study. Ear and Hearing, 36, 4S–13S. [Google Scholar] [CrossRef] [PubMed]
- Mok, M., Galvin, K. L., Dowell, R. C., & McKay, C. M. (2009). Speech perception benefit for children with a cochlear implant and a hearing aid in opposite ears and children with bilateral cochlear implants. Audiology and Neurotology, 15(1), 44–56. [Google Scholar] [CrossRef]
- Mudry, A., & Tjellström, A. (2011). Historical background of bone conduction hearing devices and bone conduction hearing aids. Advances in Oto-Rhino-Laryngology, 71, 1–9. [Google Scholar]
- Munoz, K., Preston, E., & Hicken, S. (2014). Pediatric hearing aid use: How can audiologists support parents to increase consistency? Journal of the American Academy of Audiology, 25(4), 380–387. [Google Scholar] [CrossRef]
- Munoz, K. F., Larsen, M., Nelson, L., Yoho, S. E., & Twohig, M. P. (2019). Pediatric amplification management: Parent experiences monitoring children’s aided hearing. Journal of Early Hearing Detection and Intervention, 4(1), 73–82. [Google Scholar]
- Myklebust, H. R. (1946). The use of individual hearing aids in a residential school for the deaf with implications for acoustic training. American Annals of the Deaf, 91, 255–261. [Google Scholar]
- Naik, A. N., Varadarajan, V. V., & Malhotra, P. S. (2021). Early pediatric cochlear implantation: An update. Laryngoscope Investigative Otolaryngology, 6(3), 512–521. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Clinical Excellence (NICE). (2019). Cochlear implants for children and adults with severe to profound deafness. National Institute for Health and Clinical Excellence (NICE). [Google Scholar]
- Pape, L., Kennedy, K., Kaf, W., & Zahirsha, Z. (2014). Immigration within the United States: Prevalence of childhood hearing loss revisited. American Journal of Audiology, 23(2), 238–241. [Google Scholar] [CrossRef] [PubMed]
- Park, L. R., Griffin, A. M., Sladen, D. P., Neumann, S., & Young, N. M. (2022). American Cochlear Implant Alliance Task Force Guidelines for clinical assessment and management of cochlear implantation in children with single-sided deafness. Ear and Hearing, 43(2), 255–267. [Google Scholar] [CrossRef]
- Patro, A., Holder, J. T., Brown, C. L., DeFreese, A., Virgin, F., & Perkins, E. L. (2023). Cochlear implantation in very young children with single-sided deafness. Otolaryngology–Head and Neck Surgery, 169(6), 1615–1623. [Google Scholar] [CrossRef]
- Pintner, R. (1942). Interim Report of the Sub-Committee on the Value of Individual Hearing Aids for Hard-of-Hearing Children. American Annals of the Deaf, 87(4), 306–310. [Google Scholar]
- Pittman, A. L., Stelmachowicz, P. G., Lewis, D. E., & Hoover, B. M. (2002). Influence of hearing loss on the perceptual strategies of children and adults. Journal of Speech, Language, and Hearing Research, 45, 1276–1284. [Google Scholar] [CrossRef] [PubMed]
- Preston, E., Twohig, M., & Muñoz, K. (2017). Parent-professional partnerships: Managing behavior to increase hearing aid use. Perspectives of the ASHA Special Interest Groups, 2(9), 66–71. [Google Scholar] [CrossRef]
- Profita, H. P., Stangl, A., Matuszewska, L., Sky, S., Kushalnagar, R., & Kane, S. K. (2018). “Wear it loud” how and why hearing aid and cochlear implant users customize their devices. ACM Transactions on Accessible Computing (TACCESS), 11(3), 1–32. [Google Scholar]
- Purcell, P. L., Deep, N. L., Waltzman, S. B., Roland, J. T., Jr., Cushing, S. L., Papsin, B. C., & Gordon, K. A. (2021). Cochlear implantation in infants: Why and how. Trends in Hearing, 25, 23312165211031751. [Google Scholar] [CrossRef]
- Ramos, A., Rodríguez, C., Martinez-Beneyto, P., Perez, D., Gault, A., Falcon, J. C., & Boyle, P. (2009). Use of telemedicine in the remote programming of cochlear implants. Acta Oto-Laryngologica, 129(5), 533–540. [Google Scholar] [CrossRef]
- Rauterkus, E. P., & Palmer, C. V. (2014). The hearing aid effect in 2013. Journal of the American Academy of Audiology, 25(9), 893–903. [Google Scholar] [CrossRef]
- Reiter, F. H. (1950). Hearing aids not a substitute for lack of hearing. American Annals of the Deaf, 95(2), 249–253. [Google Scholar]
- Ricketts, T. A., Picou, E. M., & Galster, J. (2017). Directional microphone hearing aids in school environments: Working toward optimization. Journal of Speech, Language, and Hearing Research, 60(1), 263–275. [Google Scholar] [CrossRef]
- Ritter, C. R., Barker, B. A., & Scharp, K. M. (2020). Using attribution theory to explore the reasons adults with hearing loss do not use their hearing aids. PLoS ONE, 15(9), e0238468. [Google Scholar] [CrossRef] [PubMed]
- Roman, S., Nicollas, R., & Triglia, J. M. (2011). Practice guidelines for bone-anchored hearing aids in children. European Annals of Otorhinolaryngology, Head and Neck Diseases, 128(5), 253–258. [Google Scholar] [CrossRef] [PubMed]
- Ryan, B. J., Jhonson, A., Strange, A., & Yonovitz, A. (2006). The “Hearing Aid Effect” in Northern Territory Indigenous Australian children as perceived by their peers. Australian and New Zealand Journal of Audiology, 28(2), 55–74. [Google Scholar] [CrossRef]
- Schaefer, S., Sahwan, M., Metryka, A., Kluk, K., & Bruce, I. A. (2021). The benefits of preserving residual hearing following cochlear implantation: A systematic review. International Journal of Audiology, 60(8), 561–577. [Google Scholar] [CrossRef]
- Schweinitz, L. D., Miller, C. A., & Miller, J. B. (1959). Delays in the diagnosis of deafness among preschool children. Pediatrics, 24(3), 462–468. [Google Scholar] [CrossRef] [PubMed]
- Scollie, S. D. (2008). Children’s speech recognition scores: The Speech Intelligibility Index and proficiency factors for age and hearing level. Ear and Hearing, 29(4), 543–556. [Google Scholar] [CrossRef]
- Seewald, R., Moodie, S., Scollie, S., & Bagatto, M. (2005). The DSL method for pediatric hearing instrument fitting: Historical perspective and current issues. Trends in Amplification, 9(4), 145–157. [Google Scholar] [CrossRef]
- Shapiro, S., Ramadan, J., & Cassis, A. (2018). BAHA skin complications in the pediatric population: Systematic review with meta-analysis. Otology & Neurotology, 39(7), 865–873. [Google Scholar]
- Sharma, A., & Campbell, J. (2011). A sensitive period for cochlear implantation in deaf children. The Journal of Maternal-Fetal & Neonatal Medicine, 24(Suppl. 1), 151–153. [Google Scholar]
- Sharma, S. D., Cushing, S. L., Papsin, B. C., & Gordon, K. A. (2020). Hearing and speech benefits of cochlear implantation in children: A review of the literature. International Journal of Pediatric Otorhinolaryngology, 133, 109984. [Google Scholar] [CrossRef] [PubMed]
- Sindhar, S., Friesen, T. L., Carpenter, D., Kesser, B., & Lieu, J. E. (2021). Fatigue in children with unilateral and bilateral hearing loss. Otology & Neurotology, 42(9), e1301–e1307. [Google Scholar]
- Slager, H. K., Jensen, J., Kozlowski, K., Teagle, H., Park, L. R., Biever, A., & Mears, M. (2019). Remote programming of cochlear implants. Otology & Neurotology, 40(3), e260. [Google Scholar]
- Stiles, D. J., Bentler, R. A., & McGregor, K. K. (2012). The speech intelligibility index and the pure-tone average as predictors of lexical ability in children fit with hearing aids. Journal of Speech, Language and Hearing Research, 55(3), 764–778. [Google Scholar] [CrossRef] [PubMed]
- Strange, A., Johnson, A., Ryan, B. J., & Yonovitz, A. (2008). The stigma of wearing hearing aids in an adolescent aboriginal population. Australian and New Zealand Journal of Audiology, 30(1), 19–37. [Google Scholar] [CrossRef]
- Tang, J. Z., Ng, P. G., & Loo, J. H. (2023). Do all infants with congenital hearing loss meet the 1-3-6 criteria? A study of a 10-year cohort from a universal newborn hearing screening programme in Singapore. International Journal of Audiology, 62(8), 795–804. [Google Scholar] [CrossRef]
- Teagle, H. F., Henderson, L., He, S., Ewend, M. G., & Buchman, C. A. (2018). Pediatric auditory brainstem implantation: Surgical, electrophysiological and behavioral outcomes. Ear and Hearing, 39(2), 326. [Google Scholar] [CrossRef]
- Thomas, J. P., Neumann, K., Dazert, S., & Voelter, C. (2017). Cochlear implantation in children with congenital single-sided deafness. Otology & Neurotology, 38, 496–503. [Google Scholar]
- Tomblin, J. B., Harrison, M., Ambrose, S. E., Walker, E. A., Oleson, J. J., & Moeller, M. P. (2015). Language outcomes in young children with mild to severe hearing loss. Ear and Hearing, 36, 76S–91S. [Google Scholar] [CrossRef]
- Tsiakpini, L., Weichbold, V., Kuehn-Inacker, H., Coninx, F., D’Haese, P., & Almadin, S. (2004). LittlEARS auditory questionnaire. MED-EL. [Google Scholar]
- Umashankar, A., Umashankar, A. A., Anusha, M. N., Pachaiappan, C., & Pachaiappan, C. (2021). Application of artificial intelligence in hearing aids and auditory implants: A short review. Journal of Hearing Science, 11(3), 20. [Google Scholar] [CrossRef]
- Valente, M., & Amlani, A. M. (2017). Cost as a barrier for hearing aid adoption. JAMA Otolaryngology–Head & Neck Surgery, 143(7), 647–648. [Google Scholar]
- van Wieringen, A., Boudewyns, A., Sangen, A., Wouters, J., & Desloovere, C. (2019). Unilateral congenital hearing loss in children: Challenges and potentials. Hearing Research, 372, 29–41. [Google Scholar] [CrossRef]
- Varadarajan, V. V., Sydlowski, S. A., Li, M. M., Anne, S., & Adunka, O. F. (2021). Evolving criteria for adult and pediatric cochlear implantation. Ear, Nose & Throat Journal, 100(1), 31–37. [Google Scholar]
- Warner-Czyz, A. D., Roland, J. T., Jr., Thomas, D., Uhler, K., & Zombek, L. (2022). American Cochlear Implant Alliance Task Force guidelines for determining cochlear implant candidacy in children. Ear and Hearing, 43(2), 268. [Google Scholar] [CrossRef] [PubMed]
- Waterworth, C. J., Marella, M., O’Donovan, J., Bright, T., Dowell, R., & Bhutta, M. F. (2022). Barriers to access to ear and hearing care services in low- and middle-income countries: A scoping review. Glob Public Health, 17(12), 3869–3893. [Google Scholar] [CrossRef]
- Wilson, B. S., & Tucci, D. L. (2021). Addressing the global burden of hearing loss. The Lancet, 397(10278), 945–947. [Google Scholar] [CrossRef]
- Wiseman, K. B., McCreery, R. W., & Walker, E. A. (2023). Hearing thresholds, speech recognition, and audibility as indicators for modifying intervention in children with hearing aids. Ear and Hearing, 44(4), 787–802. [Google Scholar] [CrossRef]
- Wiseman, K. B., Warner-Czyz, A. D., & Nelson, J. A. (2021). Stress in parents of school-age children and adolescents with cochlear implants. The Journal of Deaf Studies and Deaf Education, 26(2), 209–222. [Google Scholar] [CrossRef]
- Wolfe, J., Neumann, S., Schafer, E., Marsh, M., Wood, M., & Baker, R. S. (2017). Potential benefits of an integrated electric-acoustic sound processor with children: A preliminary report. Journal of the American Academy of Audiology, 28(2), 127–140. [Google Scholar] [CrossRef]
- Wolfe, J., & Schafer, E. (2010). Programming cochlear implants: Core clinical concepts in audiology. Plural Publishing. [Google Scholar]
- Wolfe, J., & Scholl, J. R. (2009). Ensuring well-fitted earmolds for infants and toddlers. The Hearing Journal, 62(10), 56. [Google Scholar] [CrossRef]
- Woodson, E. A., Reiss, L. A., Turner, C. W., Gfeller, K., & Gantz, B. J. (2010). The Hybrid cochlear implant: A review. Cochlear Implants and Hearing Preservation, 67, 125–134. [Google Scholar]
- World Bank. (2021). World bank country and lending groups. World bank data help desk. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lendinggroups (accessed on 14 October 2024).
- World Health Organization (WHO). (2021). World report on hearing. World Health Organization. [Google Scholar]
- Zeitler, D. M., Dunn, C., Schwartz, S. R., McCoy, J. L., Jamis, C., Chi, D. H., & Anne, S. (2023). Health-Related quality of life in children with unilateral sensorineural hearing loss following cochlear implantation. Otolaryngology–Head and Neck Surgery, 168(6), 1511–1520. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman-Phillips, S., Osberger, M. J., & Robbins, A. M. (1997). Infant-toddler: Meaningful auditory integration scale (IT-MAIS). Advanced Bionics Corporation. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).