Health and Mental Well-Being of Academic Staff and Students in Thailand: Validation and Model Development
Abstract
1. Introduction
2. Materials and Methods
2.1. Data and Sample
2.2. Theoretical Scale Construction and Development
2.3. Measures
2.4. Instruments
2.5. Proposed Model Modification
2.6. Analyses
3. Results
3.1. Sample Characteristics
3.2. Initial Model Development
3.3. Measurement Model
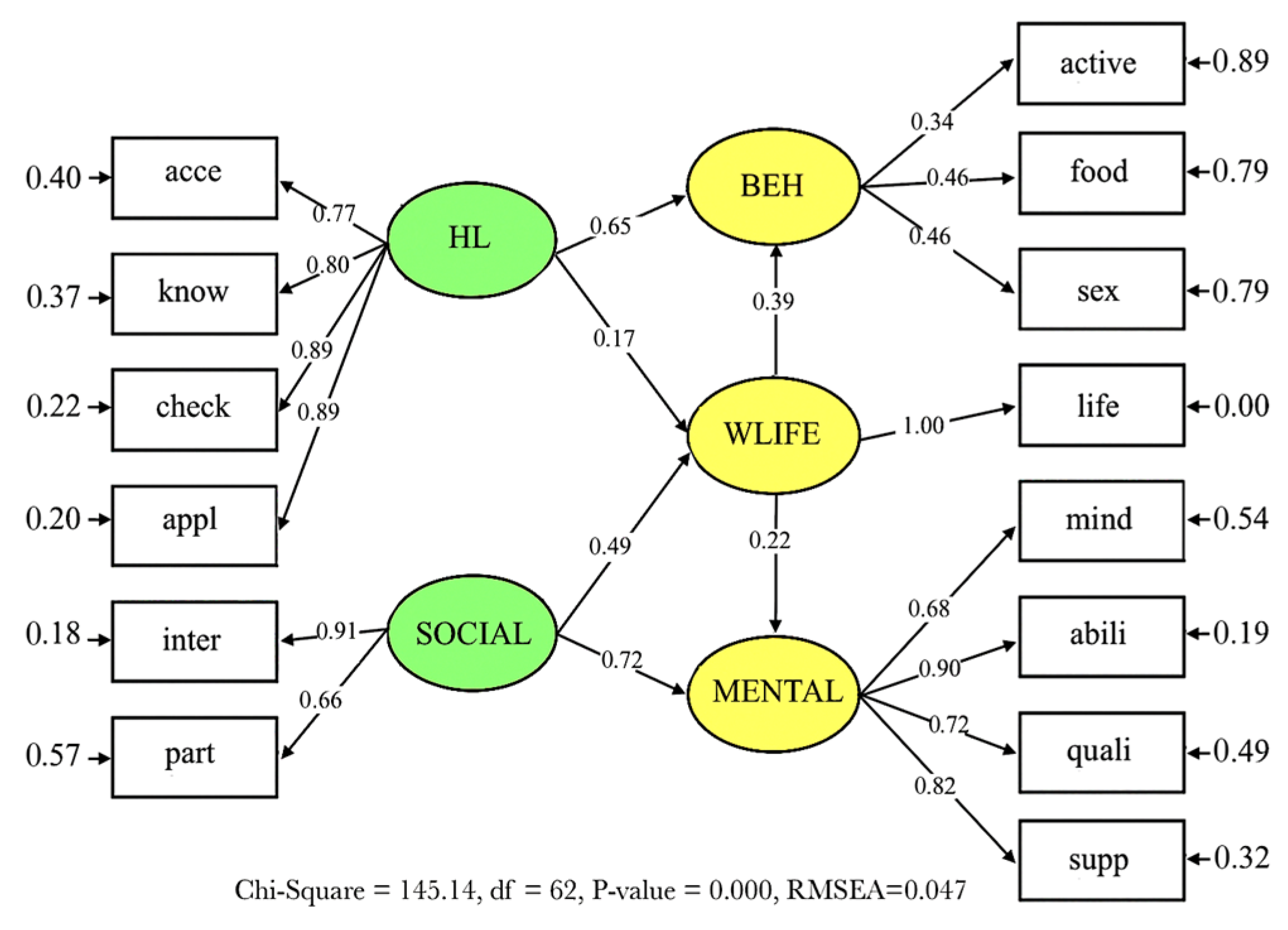
3.4. CFA Structural Model
3.5. Hypothesis Testing
4. Discussion
4.1. Practical Implications
4.2. Theoretical Contributions
4.3. Future Implications and Policy Initiatives
4.4. Potential Limitations and Directions for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aba Shaar, M. Y. M., Waluyo, B., Rofiah, N. L., Singhasuwan, P., & Tongumpa, K. (2025). The antecedents of online teaching anxiety among university lecturers in Thailand: A mixed-methods investigation. Asian Association of Open Universities Journal, 20(1), 27–39. [Google Scholar] [CrossRef]
- Agudelo-Hernández, F., & Rojas-Andrade, R. (2024). Design and validation of a scale of core components of community interventions in mental health. The International Journal of Health Planning and Management, 39(1), 36–47. [Google Scholar] [CrossRef]
- Alzadjali, B., & Ahmad, S. Z. (2024). The impacts of a high commitment work system on well-being: The mediating role of organization support and employee work-life balance. Industrial and Commercial Training, 56(1), 53–77. [Google Scholar] [CrossRef]
- Amoah, P. A., Leung, A. Y., Okyere, J., Lau, S. S., Dadaczynski, K., & Okan, O. (2025). Health literacy and mental well-being of school staff in times of crisis: A path analysis of sense of coherence, work-related stress, and health-protective behaviours. Public Health, 245, 105749. [Google Scholar] [CrossRef]
- Asparouhov, T., & Muthén, B. (2009). Exploratory structural equation modeling. Structural Equation Modeling: A Multidisciplinary Journal, 16(3), 397–438. [Google Scholar]
- Brown, A. D., Ross, N., Sangraula, M., Laing, A., & Kohrt, B. A. (2023). Transforming mental healthcare in higher education through scalable mental health interventions. Cambridge Prisms: Global Mental Health, 10, e33. [Google Scholar]
- Browne, M., Rockloff, M., & Rawat, V. (2018). An SEM algorithm for scale reduction incorporating evaluation of multiple psychometric criteria. Sociological Methods & Research, 47(4), 812–836. [Google Scholar]
- Brunner, L. R. (2023). Higher education institutions as eyes of the state: Canada’s international student compliance regime. Globalisation, Societies and Education, 21(2), 236–251. [Google Scholar] [CrossRef]
- Byrne, B. M. (2013). Structural equation modeling with LISREL, PRELIS, and SIMPLIS: Basic concepts, applications, and programming. Psychology Press. [Google Scholar]
- Chen, S. F., Wang, S., & Chen, C. Y. (2012). A simulation study using EFA and CFA programs based the impact of missing data on test dimensionality. Expert Systems with Applications, 39(4), 4026–4031. [Google Scholar] [CrossRef]
- Clark, S. C. (2000). Work/family border theory: A new theory of work/family balance. Human Relations, 53(6), 747–770. [Google Scholar] [CrossRef]
- Cook, D., & Davíðsdóttir, B. (2021). An appraisal of interlinkages between macro-economic indicators of economic well-being and the sustainable development goals. Ecological Economics, 184, 106996. [Google Scholar] [CrossRef]
- De, G., Joshi, H., & Sondhi, N. (2025). Understanding primordial preventive healthcare behaviour: The role of individual and social factors. Global Business Review. [Google Scholar] [CrossRef]
- Duffy, A. (2023). University student mental health: An important window of opportunity for prevention and early intervention. The Canadian Journal of Psychiatry, 68(7), 495–498. [Google Scholar] [CrossRef]
- Garg, M., Punia, B. K., Bansal, G., & Singh, M. (2025). Psychological empowerment and prosocial service behaviour in Indian universities: The mediating role of non-violent behaviour. Asia-Pacific Journal of Management Research and Innovation. [Google Scholar] [CrossRef]
- Goodwin, L. D. (1999). The role of factor analysis in the estimation of construct validity. Measurement in Physical Education and Exercise Science, 3(2), 85–100. [Google Scholar] [CrossRef]
- Haybron, D. M., & Tiberius, V. (2015). Well-being policy: What standard of well-being? Journal of the American Philosophical Association, 1(4), 712–733. [Google Scholar] [CrossRef]
- Henderson, K., & Loreau, M. (2023). A model of sustainable development goals: Challenges and opportunities in promoting human well-being and environmental sustainability. Ecological Modelling, 475, 110164. [Google Scholar] [CrossRef]
- Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Jansem, A., Intarakamhang, U., Suwanwong, C., Chuenphitthayavut, K., Tuntivivat, S., Le, K., Lien, L. T. M., & Prasittichok, P. (2025). Multi-group causal model of mental health literacy and helping behavior toward people at risk of depression among Thai and Vietnamese health science students. Journal of Preventive Medicine and Public Health, 58(3), 241. [Google Scholar] [CrossRef]
- Kantamaturapoj, K., Chanchitpricha, C., Hongsuwan, P., Suebsing, P., Thaweesuk, S., & Wibulpolprasert, S. (2023). Contextual attributes associated with public participation in environmental impact assessments in Thailand: Perspectives obtained from authorities and academics. Heliyon, 9(11), e21786. [Google Scholar] [CrossRef]
- Keyes, C. L. (2002). The mental health continuum: From languishing to flourishing in life. Journal of Health and Social Behavior, 43(2), 207–222. [Google Scholar] [CrossRef]
- Khan, A., Zeb, I., Zhang, Y., Fazal, S., & Ding, J. (2024). Relationship between psychological capital and mental health at higher education: Role of perceived social support as a mediator. Heliyon, 10(8), e29472. [Google Scholar] [CrossRef]
- Lavrijsen, J., Dockx, J., Struyf, E., & Verschueren, K. (2022). Class composition, student achievement, and the role of the learning environment. Journal of Educational Psychology, 114(3), 498–512. [Google Scholar] [CrossRef]
- Liangruenrom, N., Joshanloo, M., Hutaphat, W., & Kittisuksathit, S. (2025). Prevalence and correlates of depression among Thai university students: Nationwide study. BJPsych Open, 11(2), e59. [Google Scholar] [CrossRef]
- Manochaiwuthikul, T., Chaichutchouwakul, A., Yunan, N., Winothai, N., Kanta, P., & Sapbamrer, R. (2025). Health literacy disparities in Thai university students: Exploring differences between health science and non-health science disciplines. BMC Public Health, 25(1), 557. [Google Scholar] [CrossRef]
- McDonald, I., & Nanni, A. (2023). Measuring the impact of a positive psychology course at a Thai university: Addressing student well-being in challenging times. Psychology in the Schools, 60(9), 3403–3418. [Google Scholar] [CrossRef]
- Meeks, K., Peak, A. S., & Dreihaus, A. (2023). Depression, anxiety, and stress among students, faculty, and staff. Journal of American College Health, 71(2), 348–354. [Google Scholar] [CrossRef]
- Mueller, R. M., Lambert, M. J., & Burlingame, G. M. (1998). Construct validity of the outcome questionnaire: A confirmatory factor analysis. Journal of Personality Assessment, 70(2), 248–262. [Google Scholar] [CrossRef]
- Nitzsche, A., Jung, J., Kowalski, C., & Pfaff, H. (2014). Validation of the work-life balance culture scale (WLBCS). Work, 49(1), 133–142. [Google Scholar] [CrossRef]
- Nutbeam, D. (2000). Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15(3), 259–267. [Google Scholar] [CrossRef]
- Papavasileiou, E. F., & Dimou, I. (2025). Evidence of construct validity for work values using triangulation analysis. EuroMed Journal of Business, 20(5), 98–115. [Google Scholar] [CrossRef]
- Patel, V., Saxena, S., Lund, C., Kohrt, B., Kieling, C., Sunkel, C., Kola, L., Chang, O., Charlson, F., O’Neill, K., & Herrman, H. (2023). Transforming mental health systems globally: Principles and policy recommendations. The Lancet, 402(10402), 656–666. [Google Scholar] [CrossRef]
- Petrič, G., & Atanasova, S. (2024). Validation of the extended e-health literacy scale: Structural validity, construct validity and measurement invariance. BMC Public Health, 24(1), 1991. [Google Scholar] [CrossRef]
- Phetphum, C., Keeratisiroj, O., & Prajongjeep, A. (2023). The association between mobile game addiction and mental health problems and learning outcomes among Thai youths classified by gender and education levels. Asian Journal of Social Health and Behavior, 6(4), 196–202. [Google Scholar] [CrossRef]
- Putnam, R., Light, I., de Souza Briggs, X., Rohe, W. M., Vidal, A. C., Hutchinson, J., Gress, J., & Woolcock, M. (2004). Using social capital to help integrate planning theory, research, and practice: Preface. Journal of the American Planning Association, 70(2), 142–192. [Google Scholar] [CrossRef]
- Ratanasiripong, P., Siri, S., Hanklang, S., Chumchai, P., & Galvan, F. (2024). Factors related to mental health and quality of life among college and university teaching professionals in Thailand. Thai Journal of Public Health, 54(1), 828–845. [Google Scholar]
- Rosenstock, I. M. (1974). Historical origins of the health belief model. Health Education Monographs, 2(4), 328–335. [Google Scholar] [CrossRef]
- Schartner, A., Young, T. J., & Snodin, N. (2023). Intercultural adjustment of internationally mobile academics working in Thailand. Higher Education, 85(3), 483–502. [Google Scholar] [CrossRef]
- Shang, Y., Xie, Y., & Chen, W. (2024). Addressing resource scarcity and fostering sustainability through environmental education in Asia. Resources Policy, 90, 104823. [Google Scholar] [CrossRef]
- Stubin, C. A., Ruth-Sahd, L., & Dahan, T. A. (2024). Promoting nursing student mental health wellness: The impact of resilience-building and faculty support. Nurse Educator, 49(3), 119–124. [Google Scholar] [CrossRef]
- Suwathanpornkul, I., Sarnkhaowkhom, C., Tulmethakaan, M., Sakuntanak, P., & Charoensuk, O. U. (2023). Learning loss and psychosocial issues among Thai students amidst the COVID-19 pandemic: The perspectives of teachers in the online classroom. BMC Psychology, 11(1), 232. [Google Scholar] [CrossRef]
- Thanapop, C., Jit-akson, S., Suwankhong, D., Rasdi, I., Chankong, W., & Thanapop, S. (2023). Work ability, work-related health, and effort–reward imbalance: A cross-sectional study among university staff during the COVID-19 pandemic in Thailand. Social Sciences, 12(4), 252. [Google Scholar] [CrossRef]
- Thanoi, W., Vongsirimas, N., Sitthimongkol, Y., & Klainin-Yobas, P. (2023). Examining predictors of psychological well-being among university students: A descriptive comparative study across Thailand and Singapore. International Journal of Environmental Research and Public Health, 20(3), 1875. [Google Scholar] [CrossRef]
- Turner, R. C., & Carlson, L. (2003). Indexes of item-objective congruence for multidimensional items. International Journal of Testing, 3(2), 163–171. [Google Scholar] [CrossRef]
- Vasli, P., Shekarian-Asl, Z., Zarmehrparirouy, M., & Hosseini, M. (2024). The predictors of COVID-19 preventive health behaviors among adolescents: The role of health belief model and health literacy. Journal of Public Health, 32(1), 157–166. [Google Scholar] [CrossRef]
- Vien, H., & Galik, C. S. (2024). Individual and interlinked SDGs: Higher education institutions and metro area sustainability performance. International Journal of Sustainability in Higher Education, 25(5), 962–987. [Google Scholar] [CrossRef]
- Waleewong, O., & Yueayai, K. (2022). Patterns of socioeconomic inequities in SDGs relating to children’s well-being in Thailand and policy implications. International Journal of Environmental Research and Public Health, 19(20), 13626. [Google Scholar] [CrossRef]
- Wampler, B., & Touchton, M. (2019). Designing institutions to improve well-being: Participation, deliberation and institutionalisation. European Journal of Political Research, 58(3), 915–937. [Google Scholar] [CrossRef]
- Yadav, A., Pandita, D., & Singh, S. (2022). Work-life integration, job contentment, employee engagement and its impact on organizational effectiveness: A systematic literature review. Industrial and Commercial Training, 54(3), 509–527. [Google Scholar] [CrossRef]
- Zarei, A., Taheri, G., & Ghazvini, H. (2024). Conceptualization and validation of brand social capital construct by analyzing the role of social media capital. VINE Journal of Information and Knowledge Management Systems, 54(5), 1011–1038. [Google Scholar] [CrossRef]
- Zhang, X., Abbas, J., Shahzad, M. F., Shankar, A., Ercisli, S., & Dobhal, D. C. (2024). Association between social media use and students’ academic performance through family bonding and collective learning: The moderating role of mental well-being. Education and Information Technologies, 29(11), 14059–14089. [Google Scholar] [CrossRef]
| Stage | Recommended Procedure | Technique Implemented |
|---|---|---|
| 1. Construct identification | Theoretical constructs were identified through an extensive review of relevant literature and the development of a coherent theoretical framework. | Foundational models, including the Health Belief Model, Social Capital Theory, and established frameworks of health literacy, were systematically reviewed. |
| 2. Item generation | Items were developed to reflect and operationalise the dimensions of each construct. | Initial items were generated based on operational definitions, with between 10 and 15 items developed for each construct. |
| 3. Content validity | Content relevance and clarity were assessed through expert evaluation. | The Index of Item–Objective Congruence (IOC) was applied, drawing on the evaluations of five subject-matter experts. |
| 4. Item revision | Items identified as weak, based on expert feedback and IOC scores, were revised or eliminated. | Items receiving IOC scores below 0.50 were revised or removed. |
| 5. Pilot testing | The instrument was pre-tested to evaluate clarity and reliability and to obtain user feedback. | A pilot study was conducted with 50 participants, comprising both staff and students, and qualitative feedback was obtained. |
| 6. Questionnaire distribution | The full-scale survey was administered to the target population. | Online questionnaires were distributed to 300 staff members and 300 students across universities. |
| 7. Construct validation | The factor structure and the interrelationships between constructs were assessed. | EFA and CFA were conducted. |
| 8. Reliability testing | Internal consistency and measurement stability were evaluated. | Cronbach’s alpha, Composite Reliability (CR), and test–retest reliability were calculated. |
| 9. Model development | The theoretical model was developed based on validated constructs. | A CFA structural model was constructed to estimate predictive pathways among the constructs. |
| 10. Final refinement | The scale was refined to optimise its practical use and interpretability. | The item pool and scale instructions were finalised, and a user-friendly digital format was ensured. |
| General Information | Student | Staff | Total | χ2 | p-Value | |||
|---|---|---|---|---|---|---|---|---|
| 1. Sample characteristics | ||||||||
| Academic staff | – | – | 85 | 28.33 | 85 | 14.17 | – | – |
| Support staff | – | – | 215 | 71.67 | 215 | 35.83 | ||
| Undergraduate student | 272 | 90.67 | – | – | 272 | 45.33 | ||
| Graduate student | 14 | 4.67 | – | – | 14 | 2.33 | ||
| PhD student | 14 | 4.67 | – | – | 14 | 2.33 | ||
| 2. Which field does your current faculty or field of study belong to? | ||||||||
| Humanities and Social Sciences | 149 | 49.67 | 130 | 43.33 | 279 | 46.50 | 6.829 | 0.033 * |
| Health Science | 100 | 33.33 | 93 | 31.00 | 193 | 32.17 | ||
| Science and Technology | 51 | 17.00 | 77 | 25.67 | 128 | 21.33 | ||
| 3. Gender | ||||||||
| Male | 65 | 21.67 | 66 | 22.00 | 131 | 21.83 | 4.584 | 0.205 |
| Female | 198 | 66.00 | 209 | 69.67 | 407 | 67.83 | ||
| LGBTQ+ | 27 | 9.00 | 22 | 7.33 | 49 | 8.17 | ||
| Not Specified | 10 | 3.33 | 3 | 1.00 | 13 | 2.17 | ||
| 4. Level of Age | ||||||||
| Under 25 years old | 268 | 89.33 | 6 | 2.00 | 274 | 45.67 | – | – |
| 25–34 years old | 16 | 5.33 | 74 | 24.67 | 90 | 15.00 | ||
| 35–44 years old | 10 | 3.33 | 115 | 38.33 | 125 | 20.83 | ||
| 45–54 years old | 6 | 2.00 | 88 | 29.33 | 94 | 15.67 | ||
| 55 years old and over | – | – | 17 | 5.67 | 17 | 2.83 | ||
| 4. Current overall income and expenditure | ||||||||
| Sufficient/with savings | 154 | 51.33 | 102 | 34.00 | 256 | 42.67 | 59.000 | 0.000 * |
| Sufficient/no savings | 111 | 37.00 | 96 | 32.00 | 207 | 34.50 | ||
| Not sufficient/without debt | 23 | 7.67 | 25 | 8.33 | 48 | 8.00 | ||
| Insufficient/in debt | 12 | 4.00 | 77 | 25.67 | 89 | 14.83 | ||
| 5. With whom do you reside for most of the time? | ||||||||
| Family | 185 | 61.67 | 234 | 78.00 | 419 | 69.83 | 39.637 | 0.000 * |
| Friend | 44 | 14.67 | 4 | 1.33 | 48 | 8.00 | ||
| Live alone | 71 | 23.67 | 62 | 20.67 | 133 | 22.17 | ||
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mental state | 1.000 | |||||||||||||
| 2. Mental capacity | 0.613 * | 1.000 | ||||||||||||
| 3. Mental quality | 0.472 * | 0.657 * | 1.000 | |||||||||||
| 4. Supporting factors | 0.550 * | 0.631 * | 0.568 * | 1.000 | ||||||||||
| 5. Social interaction | 0.529 * | 0.700 * | 0.549 * | 0.633 * | 1.000 | |||||||||
| 6. Participation in health activities | 0.454 * | 0.506 * | 0.325 * | 0.538 * | 0.585 * | 1.000 | ||||||||
| 7. Work–life balance | 0.514 * | 0.495 * | 0.447 * | 0.558 * | 0.530 * | 0.448 * | 1.000 | |||||||
| 8. Access to health information and services | 0.338 * | 0.438 * | 0.388 * | 0.477 * | 0.562 * | 0.356 * | 0.399 * | 1.000 | ||||||
| 9. Understanding of health information and services | 0.361 * | 0.513 * | 0.446 * | 0.480 * | 0.610 * | 0.333 * | 0.416 * | 0.717 * | 1.000 | |||||
| 10. Assessment of health information and services | 0.346 * | 0.522 * | 0.448 * | 0.473 * | 0.605 * | 0.327 * | 0.436 * | 0.681 * | 0.754 * | 1.000 | ||||
| 11. Application of health information and services | 0.440 * | 0.518 * | 0.443 * | 0.513 * | 0.641 * | 0.414 * | 0.512 * | 0.674 * | 0.694 * | 0.792 * | 1.000 | |||
| 12. Exercise and physical activity | 0.294 * | 0.259 * | 0.201 * | 0.254 * | 0.285 * | 0.332 * | 0.264 * | 0.221 * | 0.191 * | 0.254 * | 0.291 * | 1.000 | ||
| 13. Healthy eating | 0.309 * | 0.304 * | 0.308 * | 0.350 * | 0.365 * | 0.290 * | 0.361 * | 0.298 * | 0.287 * | 0.338 * | 0.374 * | 0.505 * | 1.000 | |
| 14. Safe sexual behaviour | 0.173 * | 0.230 * | 0.255 * | 0.261 * | 0.298 * | 0.172 * | 0.346 * | 0.269 * | 0.298 * | 0.339 * | 0.316 * | 0.039 | 0.229 * | 1.000 |
| 3.70 | 4.05 | 4.40 | 4.11 | 4.13 | 3.44 | 3.93 | 4.14 | 4.20 | 4.24 | 4.11 | 2.33 | 3.04 | 4.43 | |
| SD | 0.69 | 0.61 | 0.58 | 0.67 | 0.63 | 0.99 | 0.71 | 0.63 | 0.60 | 0.62 | 0.62 | 0.75 | 0.74 | 0.60 |
| Variable | Student Groups | Staff Groups | Total Groups | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Skewness | Kurtosis | p-Value | Skewness | Kurtosis | p-Value | Skewness | Kurtosis | p-Value | |
| 1. Mental state | −0.463 | −0.755 | 0.676 | −0.394 | −0.714 | 0.717 | −0.640 | −1.041 | 0.474 |
| 2. Mental capacity | −1.118 | −1.727 | 0.121 | −0.752 | −1.210 | 0.362 | −1.337 | −2.084 | 0.052 |
| 3. Mental quality | −2.743 | −2.940 | 0.000 | −2.728 | −2.986 | 0.000 | −2.893 | −2.995 | 0.000 |
| 4. Supporting factors | −1.230 | −1.866 | 0.080 | −1.136 | −1.645 | 0.136 | −1.677 | −2.534 | 0.030 |
| 5. Social interaction | −1.549 | −2.101 | 0.053 | −1.110 | −1.697 | 0.128 | −1.881 | −2.738 | 0.050 |
| 6. Participation in health activities | −0.905 | −1.709 | 0.154 | −0.650 | −1.244 | 0.374 | −1.089 | −2.203 | 0.056 |
| 7. Work–life balance | −0.760 | −1.231 | 0.351 | −0.626 | −1.046 | 0.476 | −0.983 | −1.685 | 0.149 |
| 8. Access to health information and services | −1.473 | −2.185 | 0.051 | −1.165 | −1.730 | 0.114 | −1.859 | −2.816 | 0.008 |
| 9. Understanding of health information and services | −1.547 | −2.202 | 0.027 | −1.364 | −2.070 | 0.050 | −2.056 | −2.602 | 0.018 |
| 10. Assessment of health information and services | −1.560 | −2.417 | 0.016 | −1.662 | −2.302 | 0.018 | −2.282 | −2.763 | 0.006 |
| 11. Application of health information and services | −1.631 | −2.305 | 0.029 | −1.092 | −1.523 | 0.173 | −1.914 | −2.795 | 0.032 |
| 12. Exercise and physical activity | 0.091 | −0.203 | 0.976 | 0.150 | −0.494 | 0.875 | 0.172 | −0.620 | 0.813 |
| 13. Healthy eating | −0.016 | −0.054 | 0.998 | −0.040 | −0.019 | 0.999 | −0.061 | −0.120 | 0.991 |
| 14. Safe sexual behaviour | −1.615 | −2.280 | 0.020 | −1.685 | −2.301 | 0.017 | −2.327 | −2.864 | 0.002 |
| Variable | Work–Life Balance = 0.40) | Health Behaviour = 0.84) | Mental Health = 0.76) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| DE | IE | TE | DE | IE | TE | DE | IE | TE | |
| Social participation | 0.49 * | – | 0.49 * | – | 0.19 * | 0.19 * | 0.72 * | 0.11 * | 0.83 * |
| Health literacy | 0.17 * | – | 0.17 * | 0.65 * | 0.07 * | 0.72 * | – | 0.04 * | 0.04 * |
| Work–life balance | – | – | – | 0.39 * | – | 0.39 * | 0.22 * | – | 0.22 * |
| Hypothesised Relationship Model | Fit Index | Invariance Condition | |||||||
|---|---|---|---|---|---|---|---|---|---|
| χ2 | df | p-Value | RMSEA | χ2/df | GFI | Δχ2 | Δdf | p-Value | |
| Step 1: Configural invariance | 315.09 | 151 | 0.00 | 0.060 | 2.073 | 0.93 | – | – | – |
| Step 2: Metric invariance | 332.82 | 161 | 0.00 | 0.060 | 2.067 | 0.93 | 17.73 (2→1) | 10 (2→1) | 0.059 |
| Step 3: Structural invariance | 344.08 | 167 | 0.00 | 0.060 | 2.060 | 0.93 | 11.26 (3→2) | 6 (3→2) | 0.081 |
| Latent Variable | Mean Difference | t-Value | p-Value | |
|---|---|---|---|---|
| Social participation | 0.158 | 0.059 | 2.694 | 0.007 * |
| Health literacy | 0.003 | 0.045 | 0.074 | 0.941 |
| Work–life balance | 0.074 | 0.059 | 1.276 | 0.203 |
| Health behaviour | 0.062 | 0.041 | 1.516 | 0.130 |
| Mental health | 0.025 | 0.044 | 0.572 | 0.567 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Intarakamhang, U.; Jearajit, C.; Daovisan, H.; Wanitchanon, P.; Panyachit, S.; Pattrawiwat, K. Health and Mental Well-Being of Academic Staff and Students in Thailand: Validation and Model Development. Educ. Sci. 2025, 15, 1310. https://doi.org/10.3390/educsci15101310
Intarakamhang U, Jearajit C, Daovisan H, Wanitchanon P, Panyachit S, Pattrawiwat K. Health and Mental Well-Being of Academic Staff and Students in Thailand: Validation and Model Development. Education Sciences. 2025; 15(10):1310. https://doi.org/10.3390/educsci15101310
Chicago/Turabian StyleIntarakamhang, Ungsinun, Cholvit Jearajit, Hanvedes Daovisan, Phoobade Wanitchanon, Saichol Panyachit, and Kanchana Pattrawiwat. 2025. "Health and Mental Well-Being of Academic Staff and Students in Thailand: Validation and Model Development" Education Sciences 15, no. 10: 1310. https://doi.org/10.3390/educsci15101310
APA StyleIntarakamhang, U., Jearajit, C., Daovisan, H., Wanitchanon, P., Panyachit, S., & Pattrawiwat, K. (2025). Health and Mental Well-Being of Academic Staff and Students in Thailand: Validation and Model Development. Education Sciences, 15(10), 1310. https://doi.org/10.3390/educsci15101310






