Abstract
Digital learning plays an increasing role in medical education. Virtual Reality (VR) has a high potential for acquiring clinical competencies in a safe and immersive environment. With this survey, we assessed the level of acceptance and potential for VR in medical education among students. From January to April 2022, we provided an anonymous online survey at Saarland University. Besides demographic data, items covered previous VR experience, expectations of including VR in medical curricula, and estimated advantages and disadvantages. Additionally, ideas for VR scenarios could be submitted. Two hundred fifty-two medical students completed the survey. Of these, 54.4% were 21–25 years old, with 34.5% males, 50.4% being preclinical students, and 67.5% never had contact with VR. Males and preclinical students were more likely to be VR experienced. While almost all students approved the integration of VR into their curriculum, most use cases have been allocated to anatomy and surgery. Technical requirements and competencies were the main selected disadvantages. Most medical students can imagine VR being integrated into medical curricula. The implementation of immersive VR technology into medical curricula will allow students to train in practical, procedural, and soft skills repeatedly to acquire highly relevant clinical decision-making competencies with great benefit to public health.
1. Introduction
Nowadays, medical education is undergoing continuous changes through the increasing availability and development of digital teaching and learning technologies [1,2,3]. The motivation underneath is evident: extending the path of passive theoretical knowledge acquisition with active knowledge application to offer more diverse options to train, strengthen, and test hard and soft skills as core competencies, such as clinical reasoning [4] and communication skills [5]. Without risks to patients, digital teaching can set up safe, repeatable, and simulated training scenarios and allow medical students to train needed skills for their professional life [6,7].
In addition, digital technologies yield challenges in considering appropriate evaluation methods and integration strategies to embed them into medical curricula. This holds for Virtual Reality (VR) as well [8], which is one of the progressing high-potential candidates for education [9] fueled by technological advances, combining levels of interaction, immersion, and imagination, and achieving highly realistic 3D environments to experience and interact with [10]. Although VR in the context of medical education has been the subject of scientific research and studies considering various medical disciplines and specific procedures [11,12,13,14,15,16,17,18], there is still a lack of standardized guidelines for its evaluation and integration into medical curricula [8].
The perception and appreciation of medical students to benefit from novel digital teaching and learning technologies are essential for the success and efficiency of these methods. A previous survey investigating a similar topic was performed by Walter et al., 2021 [19]. In their study, medical students watched videos about VR technology and rated them based on acceptance indicators. The authors found that VR was accepted in teaching rather than in an objective structured clinical examination (OSCE). The same was true for ready-to-use technologies compared to visionary future functionalities. They concluded that missing acceptance of VR is based on limited experience, a problem that should be tackled by integrating VR into the medical study curriculum.
The main subject of the presented study is a survey that was conducted among medical students at Saarland University, Germany, to assess their experience, perception, and expectation towards VR in the context of medical education. We wanted to explore the level of acceptance and potential of this technology and to find those medical specialties that will benefit most from VR according to the student’s opinions. The knowledge gained will be crucial for the identification of future directions considering the development of VR applications for medical education.
In addition, it can be expected that the resulting enrichment in teaching and learning practices by VR will positively impact provided public health care services by improving the practical skills and decision-making of prospective physicians.
2. Materials and Methods
2.1. Survey and Participants
In January 2022, we launched an online survey (see Supplementary S1) at the Saarland University Faculty of Medicine to be completed by April 2022. The form was created using Microsoft Forms under the Microsoft Office University License. Voluntary participants remained anonymous but needed to sign in with their Microsoft Login to ensure the inclusion of only medical students and only one completion per person. The survey link was spread by the Dean’s office, the students’ council, and the Coordination Center Homburg for Education and Learning in Medicine (CHELM). Besides demographic data (age, gender, study progress), the developed questionnaire covered items on students’ previous experience with VR and their expectations of the potential of VR integration into medical curricula. This also included the assessment of assumed advantages and disadvantages. Additional free-text answers could be submitted to suggest ideas on VR training scenarios. For the analysis of free-text answers, we grouped them according to disciplines and provided reasons for the participant’s decision, and reported the most given answers. Ethical approval was obtained by the Ethical Committee of the Ärztekammer des Saarlandes (Reference: 244/21 from 8 November 2021), allowing research related to virtual reality in medical education, explicitly including the completion of questionnaires with regard to, e.g., usability, attitude towards and satisfaction with VR training scenarios.
2.2. Statistical Analysis
IBM® SPSS Statistics Version 28.0.1.1, Armonk, NY, USA, was used for statistical analysis. Besides descriptive statistics, the integrated Chi-Square Test of Independence was performed to assess for significant associations between categorical variables. In case the test’s requirements were not fulfilled [20], the Fisher Exact test (for 2 × 2 cross table) or Fisher–Freeman–Halton Exact Test (for cross tables larger than 2 × 2) was applied to determine any significant relationship. p < 0.05 was defined as the threshold for statistically significant test results. The same software, as well as Microsoft PowerPoint, was used for data visualizations.
3. Results
In this section, when referring to a survey question, we use the abbreviation “SQx”, with “x” referring to the number of the corresponding survey question in the Supplementary S1.
3.1. Demographics and VR Experience
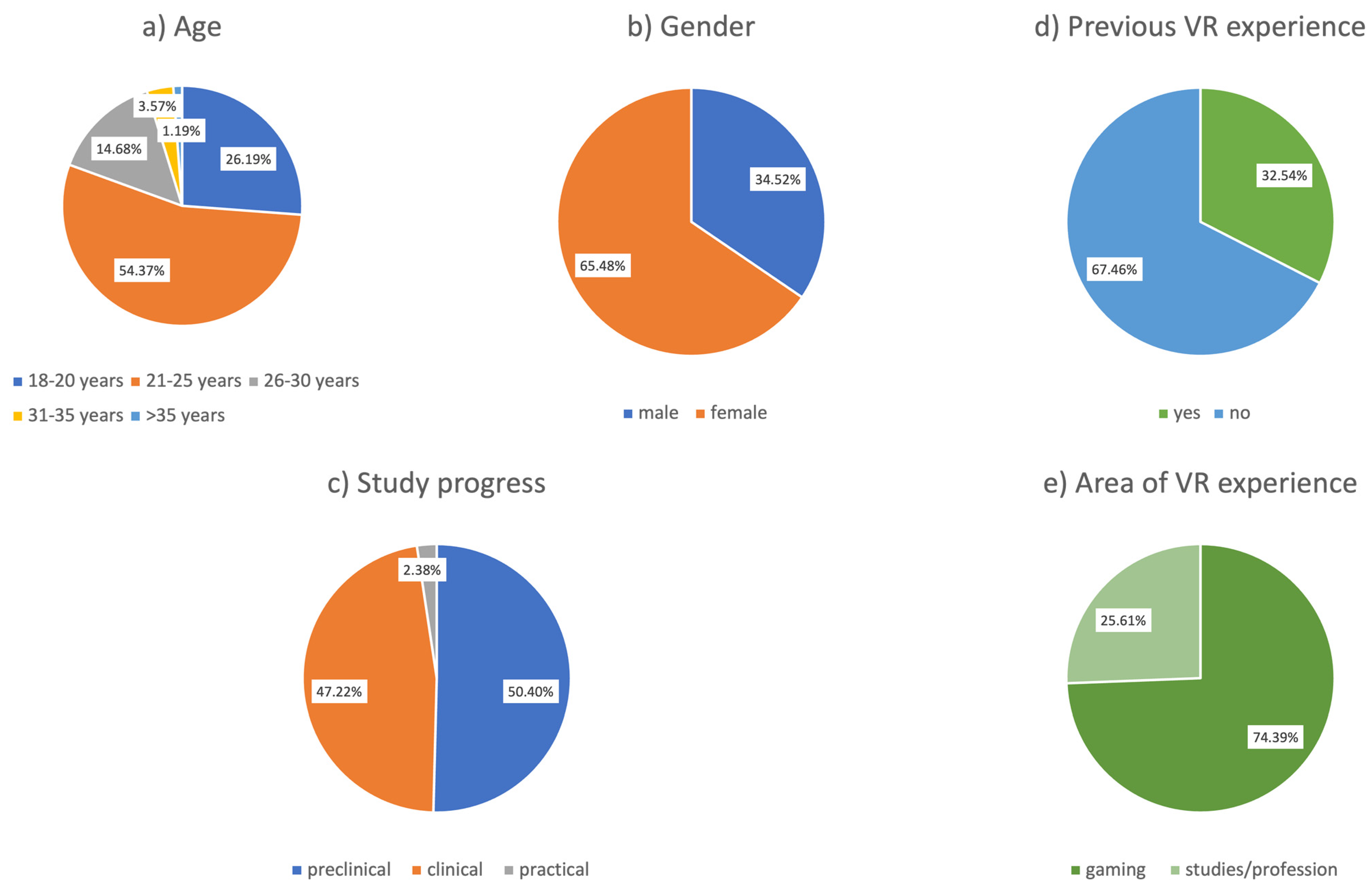
A total of 252 medical students have completed the survey (14.5% of all medical students at Saarland University). Figure 1a–c and Table 1 show the cohort’s age, gender, and study progress distribution being representative of medical students according to current demographics in Germany [21] and at our faculty [SQ1,2]. Approximately one-half (50.4%) of the students were in the preclinical phase, and 2.9% were in the final practical year [SQ3]. In addition, 67.5% of the respondents had no first-hand experience with VR (Figure 1d) [SQ4], and in those with previous VR experiences (n = 82), 74.4% played VR games (Figure 1e) [SQ5] with a significant relationship between gender [SQ2] and area of VR experience [SQ5] (p = 0.03); males rather voted for gaming (60.7% male votes, 39.3% female votes) while females rather voted for studies/profession (33.3% male votes, 66.7% female votes). No significant association could be detected between age [SQ1] and VR experience [SQ4] (p = 0.147) but between gender [SQ2] and VR experience [SQ4] (p < 0.001); only 23.0% of all females had VR experience compared to 50.6% of all males. The most noticeable difference regarding the ratio of male-to-female students with VR experience could be found among the group of 26–30-year-olds (m:f = 9:1). In addition, a significant relationship exists between study progress [SQ3] and VR experience [SQ4] (p = 0.02); 43 preclinical students made up for more than half (52.4%) of all students with VR experience (n = 82) compared to 47.6% in clinical phase or practical year.
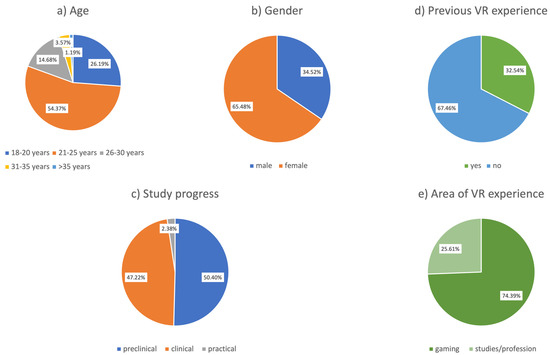
Figure 1.
Characteristics and VR experience of survey participants (a–d): n = 252; (e): n = 82.

Table 1.
Demographics of the Study Cohort (n = 252).
3.2. Integration of VR into Medical Curricula
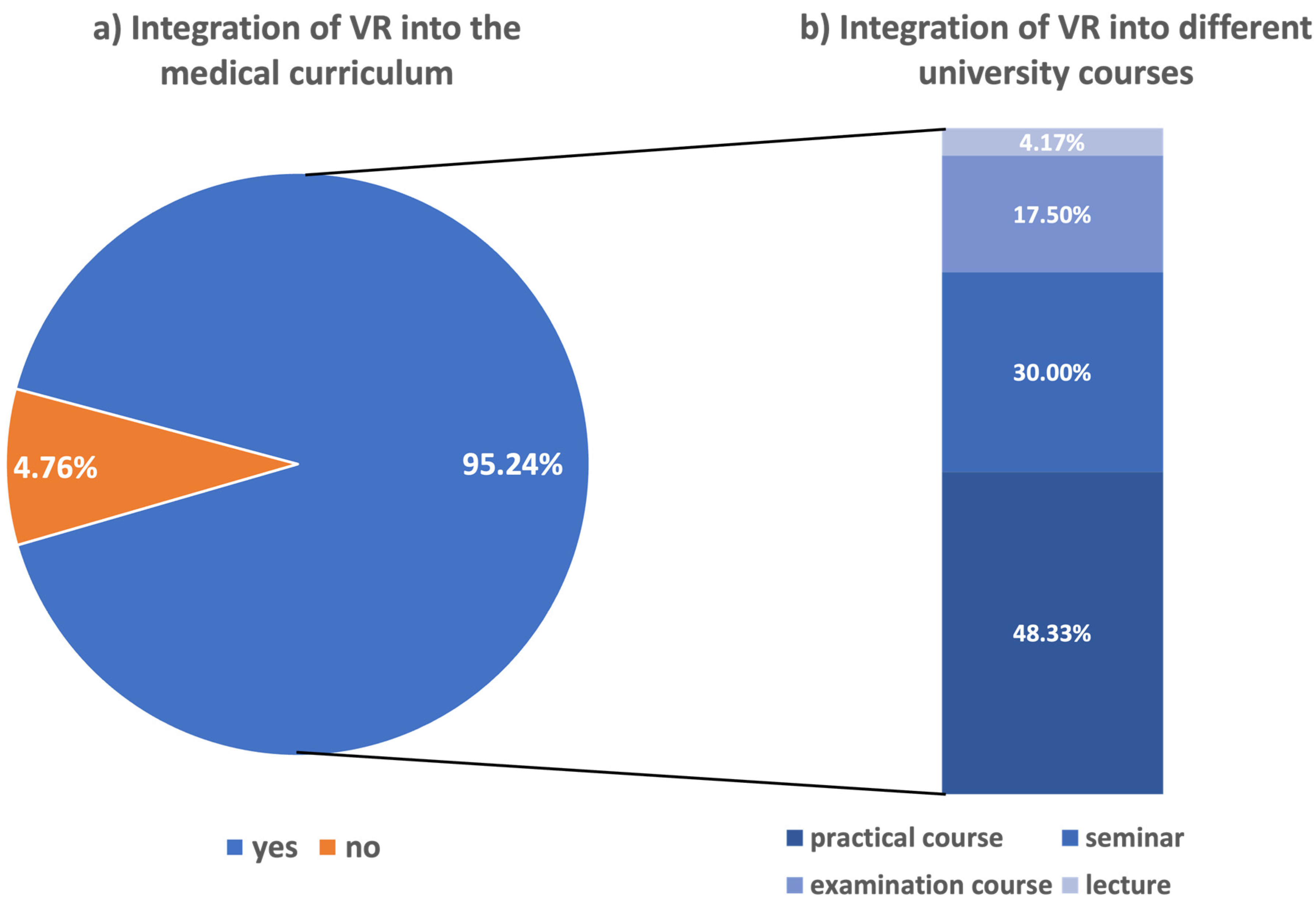
Overall, 95.2% of participants supported the potential integration of VR technologies into medical education (Figure 2a) [SQ6]. There was neither a significant difference between those with (93.9%) and those without previous VR experience (95.9%) nor between male (96.6%) and female students (94.5%) (p = 0.552). Nevertheless, out of all twelve votes against the integration of VR, nine came from female participants. According to age groups, approval rates in favor of VR integration were not significantly different (p = 0.677) and ranged between 88.9% (31–35 years) and 100% (>35 years, n = 3). In addition, no statistical relationship could be assessed between study progress [SQ3] and the question of whether VR should be integrated into medical curricula [SQ6] (p = 0.674). Among the students who voted in favor of VR integration (n = 240), 48.3% preferred practical courses, followed by seminars (30.0%) and clinical examination courses (17.5%). Only 10 participants (4.2%) assumed lectures to be the best format (Figure 2b) [SQ9].
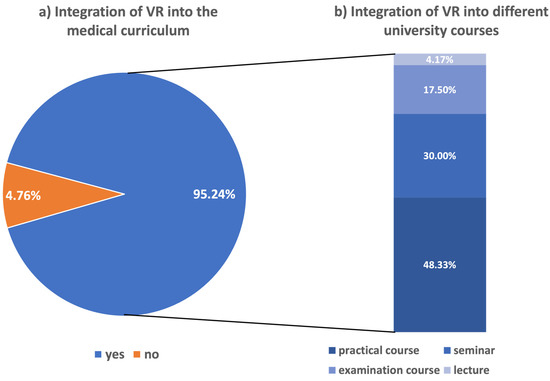
Figure 2.
Results: Integration of VR into the medical curriculum (a): n = 252; (b): n = 240, thus representing only participants answering yes (blue) to [SQ6] shown in Figure 2a.
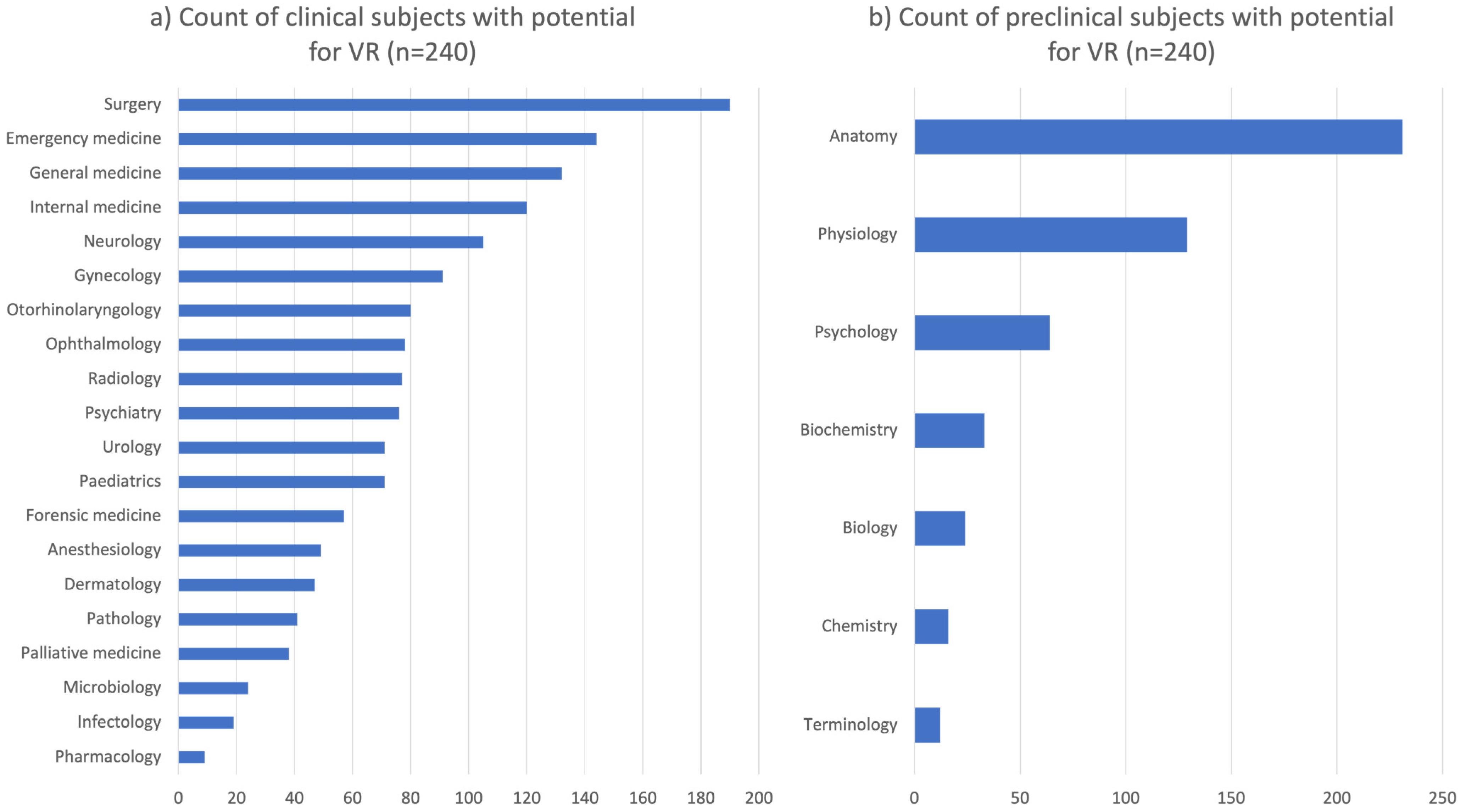
3.3. VR Integration in Clinical Specialties [SQ7]
The cohort voting in favor of VR integration (n = 240) selected independently of age groups, on average, six items from the list of 20 clinical specialties (SD = 3.56). In this cohort, a significant relationship was assessed between gender [SQ2] and the following clinical specialties [SQ7]: dermatology (p = 0.04), neurology (p = 0.02), pediatrics (p = 0.011), palliative medicine (0.025), psychiatry (p < 0.001), and forensic medicine (p = 0.027). For all these clinical specialties, females were more likely to vote in favor than their male counterparts, except for forensic medicine, in which the opposite was the case. Surgery received the most votes (n = 190; 79.2%), followed by emergency medicine (n = 144; 60.0%) and general medicine (n = 132; 55.0%) (Figure 3a) without a significant difference between preclinical and clinical students. Final-year students saw the highest potential in surgery, followed by pathology and emergency medicine.
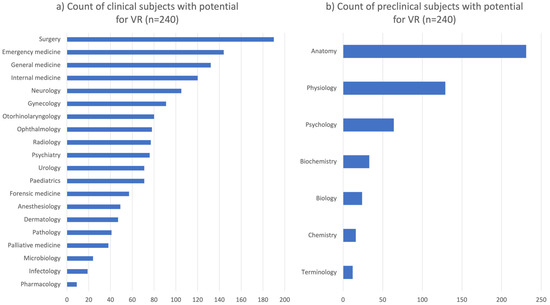
Figure 3.
Results: Subjects with potential for VR.
3.4. VR Integration in Preclinical Specialties [SQ8]
On average, students voting in favor of VR integration (n = 240) chose two of eight available preclinical academic subjects (SD = 1.118). No significant association could be detected regarding age or gender. Anatomy received the most votes of all students (91.7%), followed by physiology and psychology (Figure 3b). The same order was observed among students in their preclinical or clinical phase. Only final-year students assessed the potential of psychology to be higher than physiology.
3.5. Advantages of VR [SQ10, SQ12]
Two-thirds of the students (n = 169) consider VR to have enormous advantages [SQ12c], and 148 (58.7%) desire this technology to be integrated into medical curricula [SQ12d]. In addition, 86.1% (n = 217) of our cohort stated that VR could improve teaching in medical studies [SQ12a]. Offering a VR elective, 218 (86.5%) showed interest, and more than half of the participants would ‘definitely’ join such a course [SQ12b].
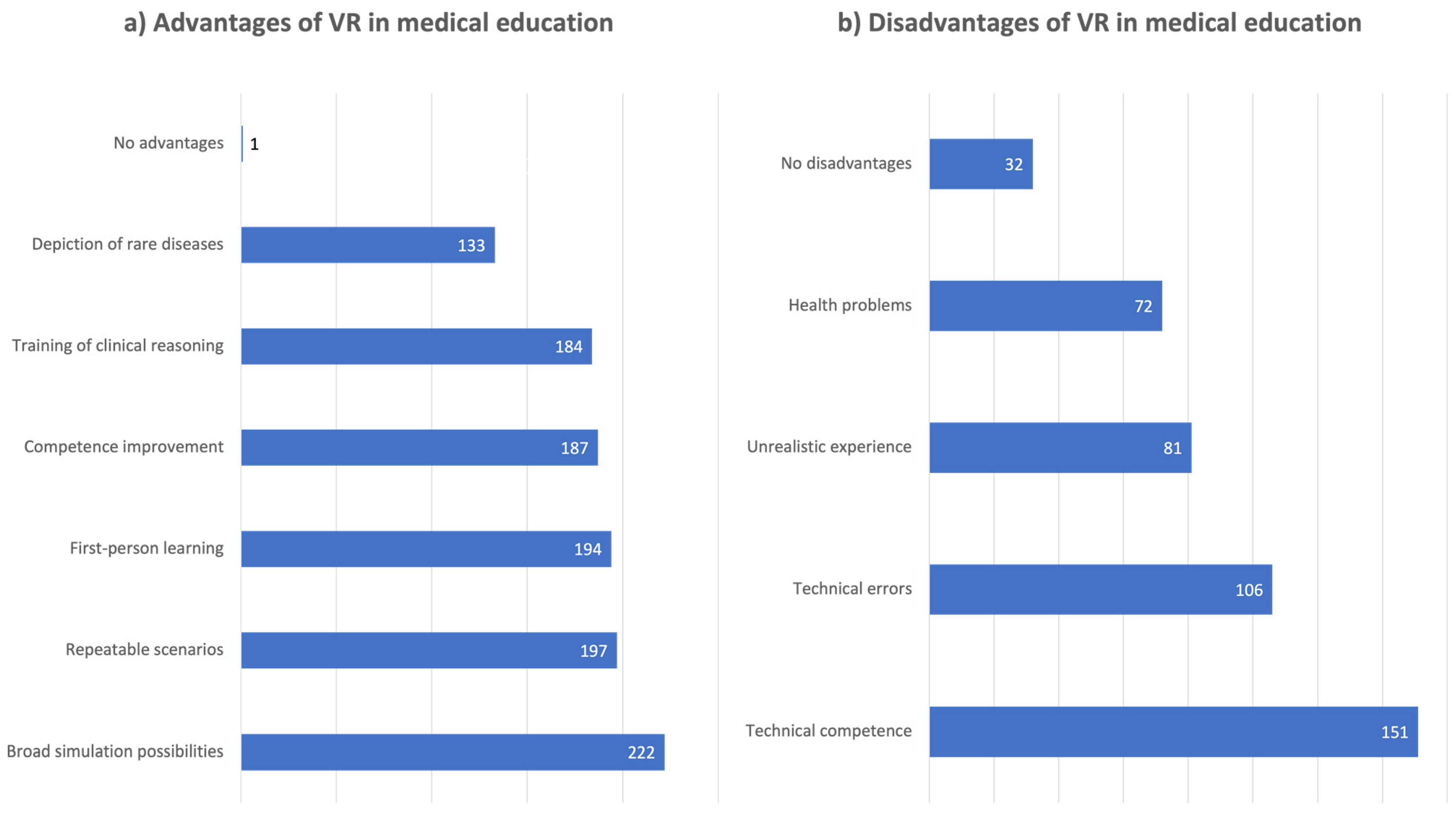
The majority of our cohort favored the broad simulation possibilities (n = 222; 88.1%), followed by the possibility of repeatable usage of VR (n = 197; 78.2%), interactive learning from a first-person perspective (n = 194; 77.0%), improvement of medical competencies (n = 187; 74.2%), training of clinical reasoning (n = 184; 73.0%), and depiction of rare diseases (n = 133; 52.8%). Only one student, who had never used VR before, assumed no advantage at all (Figure 4a). A higher percentage of the different listed advantages of VR was seen by VR-naive participants (74–78%) compared to those with previous VR experience (31–35%).
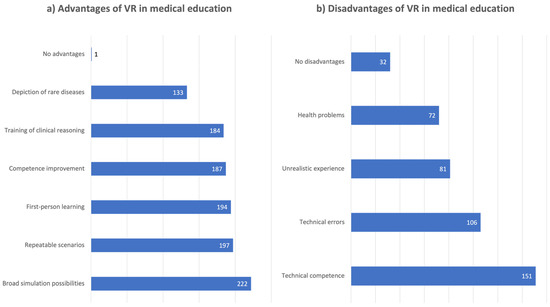
Figure 4.
Results: Estimated advantages and disadvantages of VR in medical education (n = 252).
Our findings referring to the advantages of VR in medical education according to the participants’ opinions are summarized in Table 2.

Table 2.
Advantages of VR in medical education (SQ10). The first four items belong to SQ12 (a–d), which were answered using Likert-type items. The numbers of the responses “Definitely yes” and “Rather yes” were summed up for this table.
3.6. Disadvantages of VR [SQ11]
The most voted disadvantages of VR in medical education were technical requirements or competencies (n = 151; 59.9%), followed by technical susceptibility to errors (n = 106; 42.1%) (Figure 4b). This aspect was chosen by almost half of the 18–20-year-olds (n = 31/66; 47.0%) but far less by older groups (31–35 years: n = 2/9, 22.2%; >35 years: n = 0, 0%). Unrealistic scenarios were expected by 81 (32.1%) medical students (35.6% male and 30.3% female) and 72 students (28.6%; male: n = 28, 32.2%; female: n = 44, 26.7%) mentioned health problems, such as dizziness or nausea also known as ‘cybersickness’. Comparing VR-naive with VR-experienced users, a significant difference could be observed. While 40.2% of VR-experienced participants expected health problems, this was only the case among 22.9% of VR-naive students (p = 0.004). Thirty-two participants (12.7%) did not select any disadvantages. Our findings referring to the disadvantages of VR in medical education, according to our cohort’s opinion, are summarized in Table 3.

Table 3.
Disadvantages of VR in Medical Education (SQ11).
3.7. Patient Interactions in VR [SQ12]
About one quarter (n = 62; 24.6%) of all participating medical students were fully convinced that VR could provide holistic and realistic virtual patient simulations, and 120 (47.6%) answered with ‘rather yes’ to the associated question [SQ12h]. Only nine participants (3.6%) did not assess feasibility. Two-thirds of the cohort could imagine communicating with virtual agents, 21.0% were not sure, and 12.7% were skeptical [SQ12g]. Realistic care of patients is teamwork. Our results showed that 62.3% could imagine co-work with other medical staff within a VR environment, while 22.6% were unsure and 15.1% were not convinced [SQ12i]. The examination of virtual patients in an immersive VR environment with a focus on visual findings was considered feasible by 220 students (87.3%) [SQ12e] and clinical examination by 188 (74.6%) [SQ12f]. Table 4 presents detailed results of all Likert-type items.

Table 4.
Detailed Results of Likert-type items [SQ12].
3.8. Ideas for VR-Scenarios [SQ14]
Free-text answers to the survey provided by 104 students (41.3%) supported already mentioned possibilities of VR. Among them, most students (n = 45; 43.3%) suggested using VR in surgical disciplines for training surgical skills. This was followed by emergency scenarios, especially to train faster decision-making in difficult or dangerous situations. Soft skills and psychological competencies were also suggested by students frequently. Considering this field, students expressed their desire to practice delivering bad news and handling emotionally difficult situations. Further potential was seen in internal medicine as well as general and special clinical examinations, mainly to acquire routine. Fewer responses were addressing biology, neurology, anesthesiology, radiology, dermatology, pediatrics, forensic medicine, otorhinolaryngology, and gynecology.
4. Discussion
Over the last decades, digitalization, alongside the increasing use of new technologies, has been forming health professionals’ education [22]. VR is one of the emerging technologies with the potential to shape medical education substantially [11].
Our survey reveals that most of the participating medical students have never had contact with VR before. Those claiming previous VR experience were mainly male, which is consistent with the generally observed tendency of men to have a higher affinity to video games and technology [22,23,24]. Even without previous VR experience, the attitude toward integrating this technology into medical curricula was very positive among the students surveyed. Votes against such integration were rather gender specific. Female students seem to be slightly more skeptical than male students, which is in agreement with the findings of Walter et al. (2021) [19].
Looking at clinical specialties, students believe that they would benefit from the application of VR technologies, i.e., in surgery and emergency medicine, which rely on manual skills and immediate decision-making. VR enables aspiring surgeons and emergency doctors to repeatedly train in clinical scenarios and medical procedures while not risking real patients’ safety. This way, they can get used to procedures and their steps to be prepared for real-world situations as better-trained prospective physicians, which is of great benefit to public health services. Literature matches this perception describing most use cases in training surgical specialties and psychomotor skills while, in contrast, emergency scenarios have rather been underrepresented so far [11]. Likewise, when participants were asked to come up with their own use cases for VR applications, a clear focus on procedural skill training and 3D visualization was observed in the survey. This involved mainly surgery, emergency medicine, as well as anatomy.
Considering preclinical medical subjects, anatomy had by far the highest VR potential, according to our survey. Various research projects have already examined applying VR in anatomy education [25]. One of the main advantages is that body structures and details can be viewed from different perspectives to the point of immersion into organs themselves, e.g., cardiac anatomy [26]. Kolla et al. (2020) developed a VR anatomy training module for first-year medical students. Participants evaluated the educational value of VR in comparison to traditional methods, such as lectures and cadaveric dissection [27]. Approximately 80% of their cohort reported that the module helped to study anatomy, and 90% claimed improvement in learning the names and locations of different structures. This perceived usefulness is in line with the findings of a previous survey by Huang et al., 2013 [18]. Most users (97%) found VR more helpful than an anatomy lecture and better for understanding anatomical relationships in 3D compared to cadaveric dissection. Nevertheless, the authors emphasize that some experiences, such as physical contact with human organs, feeling their consistency and texture, as well as the potential platform for discussions about mortality, will not allow to replace cadaveric dissection by VR in medical education [27].
An interesting approach to VR was suggested in our study by final-year medical students who assume high potential in psychology. This goes along with the current shift to emphasize the development of social skills and non-technical skills [28], an often-neglected area in current medical curricula [29] and, so far, targeted less by VR simulation than technical skills training [15].
VR training is one form of simulation-based medical education. Practicing clinical decision-making in a simulated context offers various benefits, such as a safe environment in which students can repeatedly practice scenarios and skills from an active first-person perspective [30]. This advantage has also been pointed out by the majority of our cohort. In addition, compared to other traditional simulation-based methods, e.g., manikins and acting patients, immersive virtual training with head-mounted displays can be a cost-effective alternative or addition to established methods [8]. Nonetheless, based on our experience after starting the first VR courses at our medical faculty, the students still need feedback from an external observer or directly by the application to improve their skills during VR training. In this context, didactic and digital training of teachers using VR technology is advisable, given the fact that health sciences professors still report a low self-concept of digital skills while seeing high potential in VR for their educational approaches [31].
We observed a more positive attitude towards VR technology among VR-naive participants. They were twice as likely to vote for its advantages than the VR-experienced participants. This indicates a general openness to this new technology while also showing that medical students who have already used VR are more likely to think of its limitations. One of these limitations is given by Bui et al. (2021), pointing out the complexity of human facial expression and language that cannot be processed adequately yet, e.g., in scenarios in which bad news is delivered [32]. Nevertheless, recent advances in AI technologies enable IT specialists to improve realistic communication and representation of emotions in simulations to practice essential non-technical skills. Considering a holistic case scenario including customizable, interactive virtual patients with realistic pathologies, almost 75% of our students supported such feasibilities. In the long-term perspective, this potential could culminate in creating a virtual hospital, in which medical students can enter various rooms to train in scenarios from different specialties.
Disadvantages are mainly associated with technical aspects. Baniasadi et al. (2020) stated that the successful implementation of this technology depends on appropriate educational training [12]. This means that a certain level of technical competence is essential for successfully using VR as a training tool [8]. When users are generally less familiar with IT, using VR will be more challenging. Furthermore, using VR software and hardware requires close technical support to rule out and react to errors in a timely manner. Interestingly, these technical problems are considered mainly among the youngest age group in our survey compared to older participants. This may reflect that such technical pitfalls are expected more often by students who have grown up in an already very technological environment in contrast to older generations [32]. Another major flaw of immersive VR is called ‘cybersickness’, which is ‘a constellation of symptoms of discomfort and malaise produced by VR exposure’ [33] that is, for example, caused by mismatches between observed and expected sensory signals, self-motion, and gameplay experience [34]. In this survey, these concerns were primarily raised by VR-experienced users who had probably already faced these problems themselves in the past.
Considering the limitations of our study, we cannot exclude a potential selection bias by only students interested in VR answering our questionnaire. However, answers of uninterested participants could be criticized as being less relevant on the one hand or representing a more unbiased expectation on the other hand. In contrast to our strategy, Walter et al. (2021) primarily presented ten videos about VR technology to participants prior to a survey, also finding acceptance of VR in medical teaching [19].
One strength of our study cohort is that it resembles the demographics of German medical students in terms of gender, age, and study progress. Expectation bias was prevented by anonymization of the students’ results. Therefore, our predominantly positive results towards the integration of VR in medical curricula can serve as a baseline for implementing VR in medical curricula. However, the inclusion of VR in medical courses requires the advice and perspective of didactic medical experts. It needs to be mentioned that this study did not aim to demonstrate the effectiveness of VR technology in medical education in contrast to other published prospective studies measuring specific VR training outcomes [16,17]. However, our results support the increasing importance of VR technology in medical education and advocate its integration into medical curricula, which is strongly encouraged by medical students.
5. Conclusions
Our survey about experience, perceptions, and expectations considering the application of VR in medical education reveals that most students are open to the integration of this technology into their curricula. While technical and procedural skills training scenarios received the most votes, practicing soft skills with virtual patients plays an increasing role that can be supported by advancing AI technology. While being in favor of the various advantages that VR might offer, students are also aware of its limitations. The general openness towards the integration of VR, as demonstrated in this survey, can serve as a backbone for conducting further projects in this area, also including surveys with medical professionals and didactics experts to purposely incorporate new learning and training methods into medical education. Eventually, this will benefit public health care by enhancing competences of prospective physicians especially in practical skills and decision-making.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/educsci13050477/s1, Document S1: Student-Survey: Virtual Reality in Medical School.
Author Contributions
Conceptualization, M.M. (Marvin Mergen) and N.G.; formal analysis, M.M. (Marvin Mergen), M.M. (Marcel Meyerheim) and N.G.; writing—original draft preparation, M.M. (Marvin Mergen) and M.M. (Marcel Meyerheim); writing—review and editing, M.M. (Marvin Mergen), M.M. (Marcel Meyerheim) and N.G.; visualization, M.M. (Marvin Mergen); supervision, N.G. All authors have read and agreed to the published version of the manuscript.
Funding
This study received funding from the German Federal Ministry of Education and Research under the BMBF project number 16DHBKI080 within the project “medical tr.AI.ning”. Furthermore, we acknowledge support by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) and Saarland University within the ‘Open Access Publication Funding’ program.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Ethics Committee of Ärztekammer des Saarlandes (Reference: 244/21 from 8 November 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, Dr. Marvin Mergen, upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Han, E.R.; Yeo, S.; Kim, M.J.; Lee, Y.H.; Park, K.H.; Roh, H. Medical Education Trends for Future Physicians in the Era of Advanced Technology and Artificial Intelligence: An Integrative Review. BMC Med. Educ. 2019, 19, 460. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, S.; Frankenhauser, S.; Tolks, D. Digitale Lehr- Und Lernangebote in Der Medizinischen Ausbildung: Schon Am Ziel Oder Noch Am Anfang? Bundesgesundheitsbl 2018, 61, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Pasquier, P.; Gaudry, S.; Tesniere, A.; Mignon, A. New Insights into Virtual Medical Education and Assessment, Serious Games, and Digital Platforms. Bull. Acad. Natl. Med. 2015, 199, 1153–1164. [Google Scholar] [CrossRef]
- Norman, G. Research in Clinical Reasoning: Past History and Current Trends. Med. Educ. 2005, 39, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Kyaw, B.M.; Posadzki, P.; Paddock, S.; Car, J.; Campbell, J.; Tudor Car, L. Effectiveness of Digital Education on Communication Skills Among Medical Students: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12967. [Google Scholar] [CrossRef]
- Phillips, D.C. The Good, the Bad, and the Ugly: The Many Faces of Constructivism. Educ. Res. 1995, 24, 5–12. [Google Scholar] [CrossRef]
- Isaza-Restrepo, A.; Gómez, M.T.; Cifuentes, G.; Argüello, A. The Virtual Patient as a Learning Tool: A Mixed Quantitative Qualitative Study. BMC Med. Educ. 2018, 18, 297. [Google Scholar] [CrossRef]
- Barteit, S.; Lanfermann, L.; Bärnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, Mixed, and Virtual Reality-Based Head-Mounted Devices for Medical Education: Systematic Review. JMIR Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef]
- Kamińska, D.; Sapiński, T.; Wiak, S.; Tikk, T.; Haamer, R.E.; Avots, E.; Helmi, A.; Ozcinar, C.; Anbarjafari, G. Virtual Reality and Its Applications in Education: Survey. Information 2019, 10, 318. [Google Scholar] [CrossRef]
- Burdea, G.C.; Coiffet, P. Virtual Reality Technology, 2nd ed.; Wiley-IEEE Press: Hoboken, NJ, USA, 2003; ISBN 978-0-471-36089-6. [Google Scholar]
- Jiang, H.; Vimalesvaran, S.; Wang, J.K.; Lim, K.B.; Mogali, S.R.; Car, L.T. Virtual Reality in Medical Students’ Education: Scoping Review. JMIR Med. Educ. 2022, 8, e34860. [Google Scholar] [CrossRef]
- Baniasadi, T.; Ayyoubzadeh, S.M.; Mohammadzadeh, N. Challenges and Practical Considerations in Applying Virtual Reality in Medical Education and Treatment. Oman Med. J. 2020, 35, e125. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.; McKechnie, J.; Edgerton, E.; Wilson, C. Immersive Virtual Reality as a Pedagogical Tool in Education: A Systematic Literature Review of Quantitative Learning Outcomes and Experimental Design. J. Comput. Educ. 2021, 8, 1–32. [Google Scholar] [CrossRef]
- Kyaw, B.M.; Saxena, N.; Posadzki, P.; Vseteckova, J.; Nikolaou, C.K.; George, P.P.; Divakar, U.; Masiello, I.; Kononowicz, A.A.; Zary, N.; et al. Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21. [Google Scholar] [CrossRef]
- Bracq, M.S.; Michinov, E.; Jannin, P. Virtual Reality Simulation in Nontechnical Skills Training for Healthcare Professionals: A Systematic Review. Simul. Healthc. 2019, 14, 188–194. [Google Scholar] [CrossRef]
- Birrenbach, T.; Zbinden, J.; Papagiannaki, G.; Exadaktylos, A.K.; Müller, M.; Hautz, W.E.; Sauter, T.C. Effectiveness and Utility of Virtual Reality Simulation as an Educational Tool for Safe Performance of COVID-19 Diagnostics: Prospective, Randomized Pilot Trial. JMIR Serious Games 2021, 9, e29586. [Google Scholar] [CrossRef] [PubMed]
- Lerner, D.; Mohr, S.; Schild, J.; Göring, M.; Luiz, T. An Immersive Multi-User Virtual Reality for Emergency Simulation Training: Usability Study. JMIR Serious Games 2020, 8, e18822. [Google Scholar] [CrossRef]
- Huang, H.M.; Liaw, S.S.; Lai, C.M. Exploring Learner Acceptance of the Use of Virtual Reality in Medical Education: A Case Study of Desktop and Projection-Based Display Systems. Interact. Learn. Environ. 2013, 24, 3–19. [Google Scholar] [CrossRef]
- Walter, S.; Speidel, R.; Hann, A.; Leitner, J.; Jerg-Bretzke, L.; Kropp, P.; Garbe, J.; Ebner, F. Skepticism towards Advancing VR Technology—Student Acceptance of VR as a Teaching and Assessment Tool in Medicine. GMS J. Med. Educ. 2021, 38, Doc100. [Google Scholar] [CrossRef]
- Yates, D.; Moore, D.; McGabe, G. The Practice of Statistics; W.H. Freeman: New York, NY, USA, 1999. [Google Scholar]
- Rudnicka, J. Studierende der Medizin Nach Geschlecht bis 2021/2022, Statista. Available online: https://de.statista.com/statistik/daten/studie/200758/umfrage/entwicklung-der-anzahl-der-medizinstudenten/ (accessed on 3 March 2023).
- O’Doherty, D.; Dromey, M.; Lougheed, J.; Hannigan, A.; Last, J.; McGrath, D. Barriers and Solutions to Online Learning in Medical Education—An Integrative Review. BMC Med. Educ. 2018, 18, 130. [Google Scholar] [CrossRef]
- Koinig, I.; Diehl, S.; Karmasin, M. Gender and Technology. In The International Encyclopedia of Gender, Media, and Communication; Ross, K., Bachmann, I., Cardo, V., Moorti, S., Scarcelli, M., Eds.; John Wiley & Sons, Ltd.: New York, NY, USA, 2020; pp. 1–8. [Google Scholar]
- Goswami, A.; Dutta, S.; Goswami, A.; Dutta, S. Gender Differences in Technology Usage—A Literature Review. Open J. Bus. Manag. 2015, 4, 51–59. [Google Scholar] [CrossRef]
- Karbasi, Z.; Kalhori, S.R.N. Application and Evaluation of Virtual Technologies for Anatomy Education to Medical Students: A Review. Med. J. Islam. Repub. Iran 2020, 34, 163. [Google Scholar] [CrossRef] [PubMed]
- Maresky, H.S.; Oikonomou, A.; Ali, I.; Ditkofsky, N.; Pakkal, M.; Ballyk, B. Virtual Reality and Cardiac Anatomy: Exploring Immersive Three-Dimensional Cardiac Imaging, a Pilot Study in Undergraduate Medical Anatomy Education. Clin. Anat. 2019, 32, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Kolla, S.; Elgawly, M.; Gaughan, J.P.; Goldman, E. Medical Student Perception of a Virtual Reality Training Module for Anatomy Education. Med. Sci. Educ. 2020, 30, 1201–1210. [Google Scholar] [CrossRef] [PubMed]
- Prineas, S.; Mosier, K.; Mirko, C.; Guicciardi, S. Non-Technical Skills in Healthcare. In Textbook of Patient Safety and Clinical Risk Management; Donaldson, L., Ricciardi, W., Sheridan, S., Tartaglia, R., Eds.; Springer International Publishing: New York, NY, USA, 2021; pp. 413–434. [Google Scholar]
- Dolev, N.; Naamati-Schneider, L.; Meirovich, A. Making Soft Skills a Part of the Curriculum of Healthcare Studies. In Medical Education for the 21st Century; Firstenberg, M., Stawicki, S., Eds.; IntechOpen: London, UK, 2021; ISBN 978-1-83969-732-6. [Google Scholar]
- Akaike, M.; Fukutomi, M.; Nagamune, M.; Fujimoto, A.; Tsuji, A.; Ishida, K.; Iwata, T. Simulation-Based Medical Education in Clinical Skills Laboratory. J. Med. Invest. 2012, 59, 28–35. [Google Scholar] [CrossRef]
- Antón-Sancho, Á.; Fernández-Arias, P.; Vergara, D. Virtual Reality in Health Science Education: Professors’ Perceptions. Multimodal Technol. Interact. 2022, 6, 110. [Google Scholar] [CrossRef]
- Bui, I.; Bhattacharya, A.; Wong, S.H.; Singh, H.R.; Agarwal, A. Role of Three-Dimensional Visualization Modalities in Medical Education. Front. Pediatr. 2021, 9, 760363. [Google Scholar] [CrossRef]
- Stanney, K.M.; Kennedy, R.S.; Drexler, J.M. Cybersickness Is Not Simulator Sickness. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2016, 2, 1138–1141. [Google Scholar] [CrossRef]
- Weech, S.; Kenny, S.; Barnett-Cowan, M. Presence and Cybersickness in Virtual Reality Are Negatively Related: A Review. Front. Psychol. 2019, 10, 158. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).