Model and Validation Study for Optimizing Students’ Positions in Classrooms to Limit the Spread of Infectious Diseases Such as COVID
Abstract
:1. Introduction
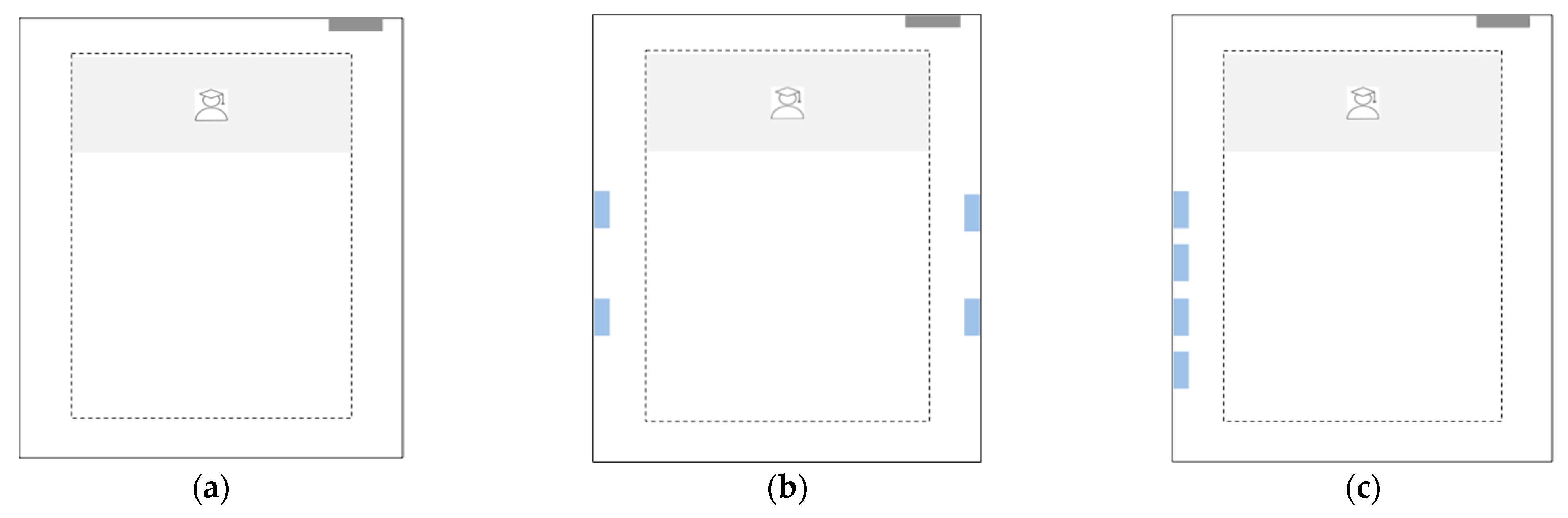
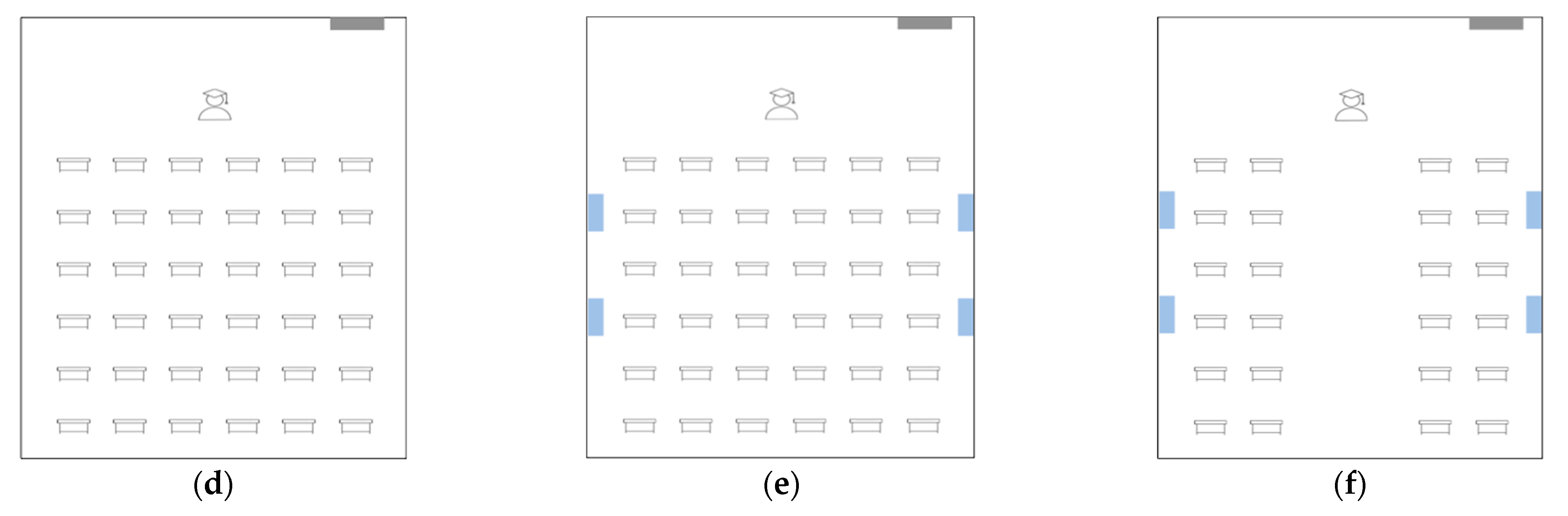
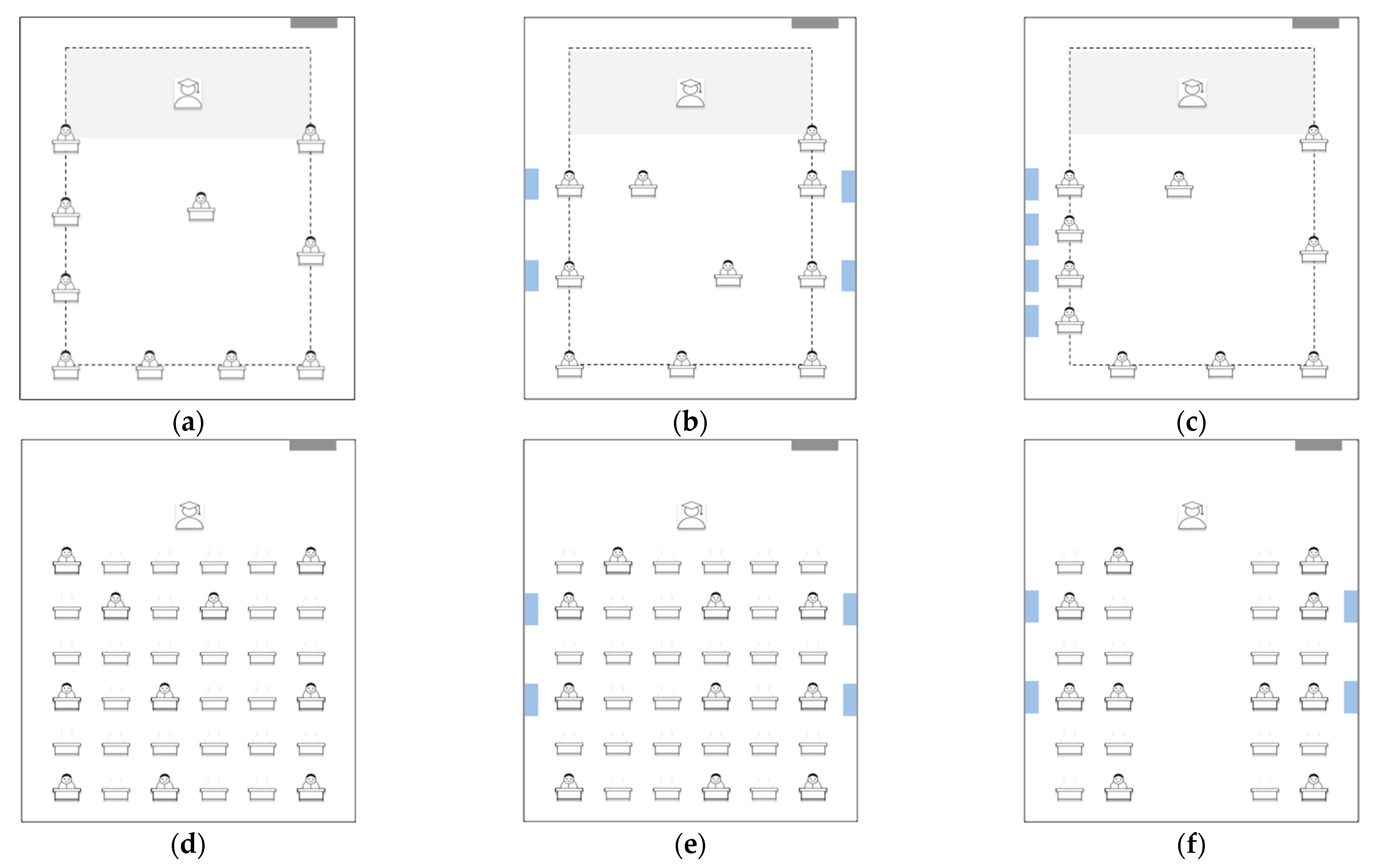
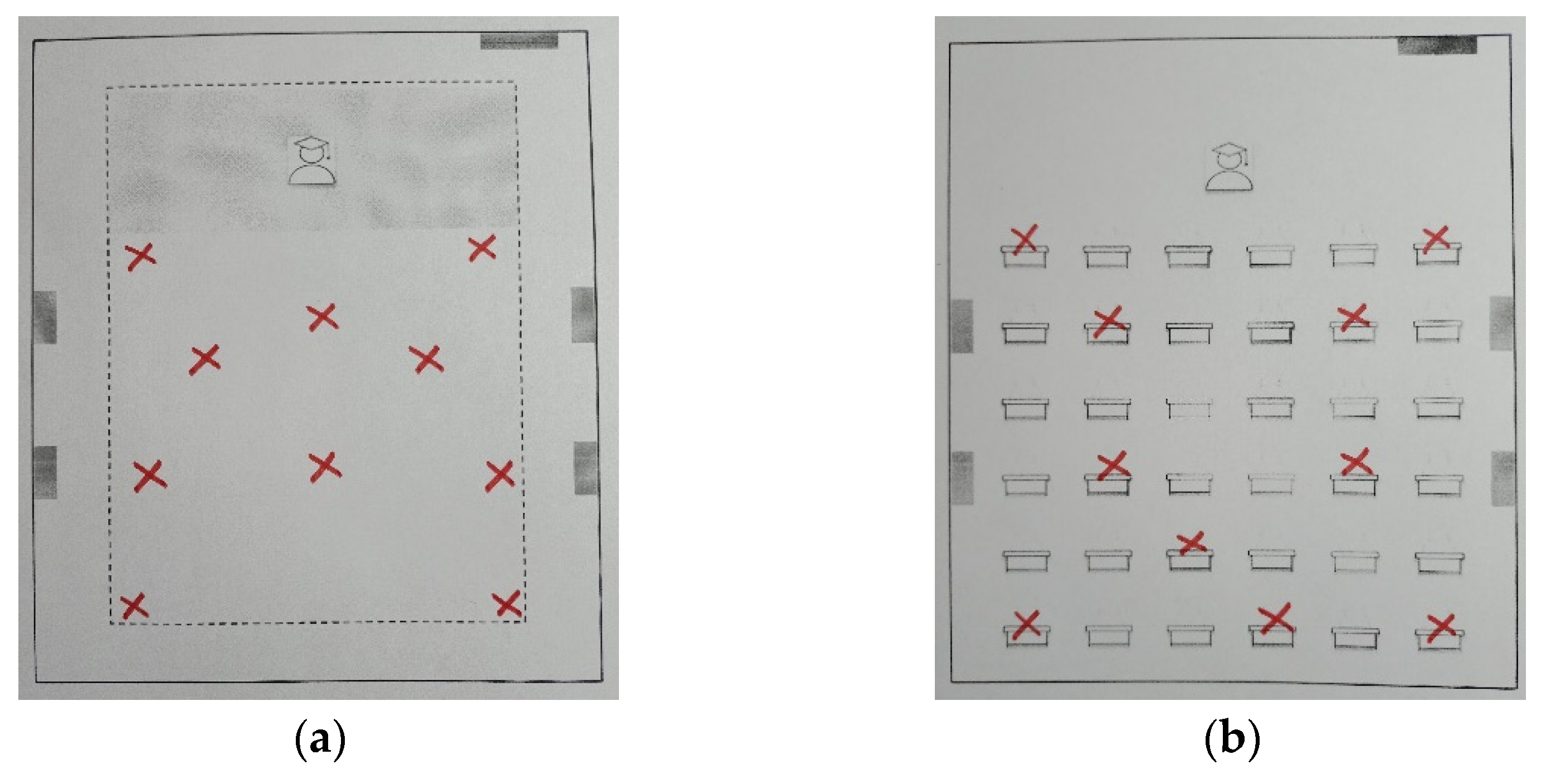
2. Methodology
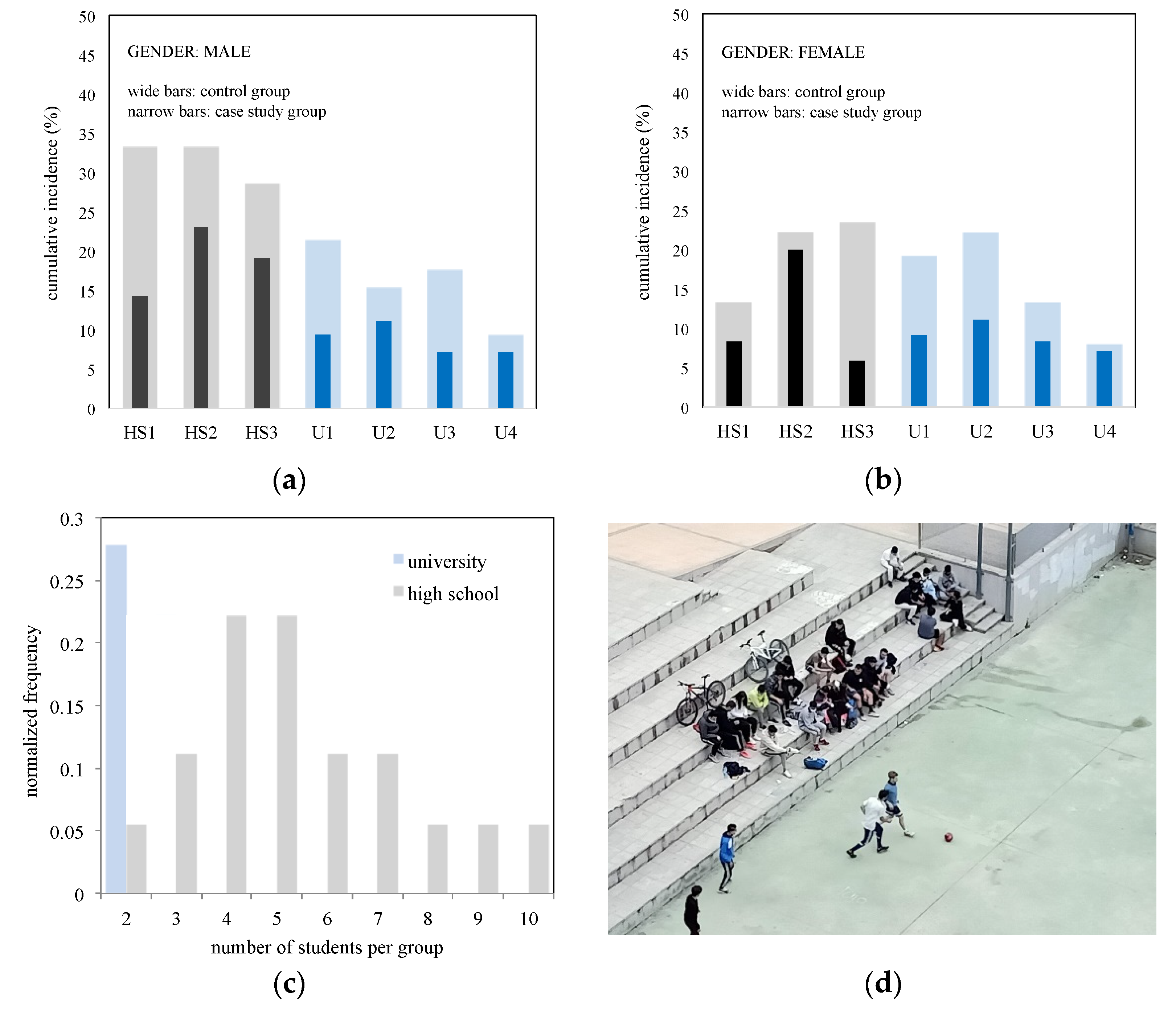
2.1. Description of the Context and Participants
2.2. Method
2.2.1. Data Collection
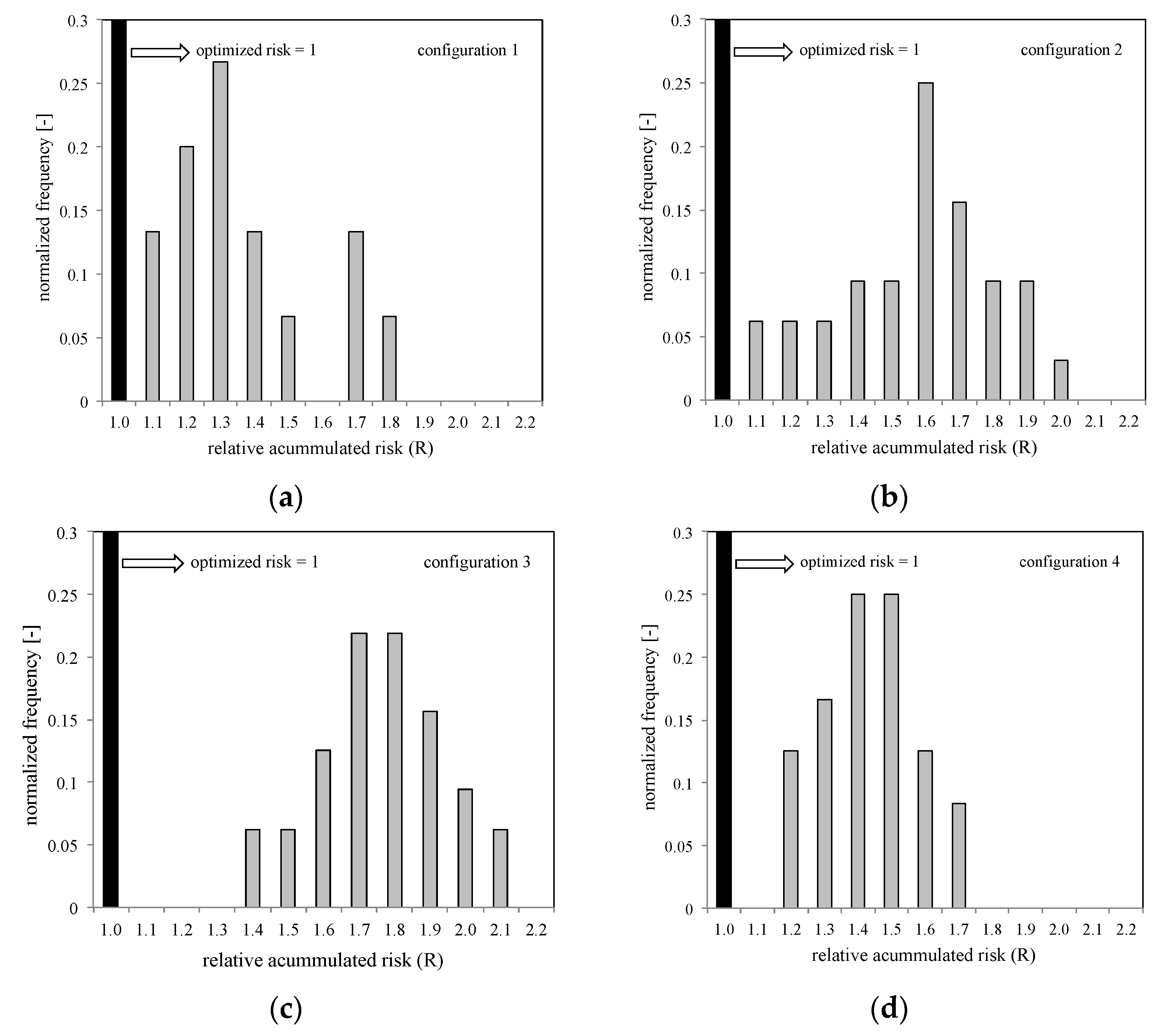
2.2.2. Proposed Model for Calculating Cumulative Risk
2.2.3. Implementation of the Proposed Model in a Calculation Tool
2.2.4. Quantification of Risk Using Data Gathered in Handwritten Templates
3. Results and Discussion
- -
- Both the control and study groups adhered to the general protocols established by each centre, which are consistent with the general guidelines of the Spanish Ministry of Health. These guidelines include the use of face masks inside and outside the classroom, as well as dispensers of hydroalcoholic gel in each classroom.
- -
- The study group adhered to a strict protocol for entering and exiting the classrooms, as suggested by some authors [3], who emphasize the importance of maintaining interpersonal distance throughout the classroom corridors until reaching the study tables.
4. Comments on the Limitations of This Study
5. Conclusions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Koopman, O.; Koopman, K.J. The Rise of the University without Classrooms after COVID-19. In Re-Thinking the Humanities Curriculum in the Time of COVID-19; CSSALL Publishers (Pty) Ltd.: Durban, South Africa, 2021; pp. 153–168. ISBN 9780986993619. [Google Scholar]
- Said, A.N. University without Walls: A Novel Approach to HigherEducation. New Dir. 1973, 1, 6. [Google Scholar]
- Lelieveld, J.; Helleis, F.; Borrmann, S.; Cheng, Y.; Drewnick, F.; Haug, G.; Klimach, T.; Sciare, J.; Su, H.; Pöschl, U. Model calculations of aerosol transmission and infection risk of COVID-19 in indoor environments. medRxiv 2020, 17, 8114. [Google Scholar] [CrossRef] [PubMed]
- Romero, V.; Stone, W.D.; Ford, J.D. COVID-19 indoor exposure levels: An analysis of foot traffic scenarios within an academic building. Transp. Res. Interdiscip. Perspect. 2020, 7, 100185. [Google Scholar] [CrossRef] [PubMed]
- Rezaei, M.; Azarmi, M. Deepsocial: Social distancing monitoring and infection risk assessment in COVID-19 pandemic. Appl. Sci. 2020, 10, 7514. [Google Scholar] [CrossRef]
- Lipinski, T.; Ahmad, D.; Serey, N.; Jouhara, H. Review of ventilation strategies to reduce the risk of disease transmission in high occupancy buildings. Int. J. Thermofluids 2020, 7–8, 100045. [Google Scholar] [CrossRef]
- Sun, C.; Zhai, Z. The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain. Cities Soc. 2020, 62, 102390. [Google Scholar] [CrossRef]
- van Hooff, T.; Blocken, B. Low-Reynolds number mixing ventilation flows: Impact of physical and numerical diffusion on flow and dispersion. Build. Simul. 2017, 10, 589–606. [Google Scholar] [CrossRef] [Green Version]
- Riley, C.E.; Murphy, G.; Riley, R.L. Airbone spread of measles in a suburban elementary school. Am. J. Epidemiol. 1978, 107, 421–432. [Google Scholar] [CrossRef]
- Duan, X.; Beijing, T.; Cao, S.; Beijing, T. Highlights of the Chinese Exposure Factors Handbook; Elsevier Inc.: Amsterdam, The Netherlands, 2015. [Google Scholar] [CrossRef]
- Buonanno, G.; Stabile, L.; Morawska, L. Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ. Int. 2020, 141, 105794. [Google Scholar] [CrossRef]
- Escombe, A.R.; Oeser, C.C.; Gilman, R.H.; Navincopa, M.; Ticona, E.; Pan, W.; Martínez, C.; Chacaltana, J.; Rodríguez, R.; Moore, D.A.J.; et al. Natural ventilation for the prevention of airborne contagion. PLoS Med. 2007, 4, 0309–0317. [Google Scholar] [CrossRef] [Green Version]
- Gao, N.P.; Niu, J.L.; Perino, M.; Heiselberg, P. The airborne transmission of infection between flats in high-rise residential buildings: Particle simulation. Build. Environ. 2009, 44, 402–410. [Google Scholar] [CrossRef]
- Gupta, J.K.; Lin, C.H.; Chen, Q. Risk assessment of airborne infectious diseases in aircraft cabins. Indoor Air 2012, 22, 388–395. [Google Scholar] [CrossRef]
- Noakes, C.J.; Beggs, C.B.; Sleigh, P.A.; Kerr, K.G. Modelling the transmission of airborne infections in enclosed spaces. Epidemiol. Infect. 2006, 134, 1082–1091. [Google Scholar] [CrossRef]
- Qian, H.; Li, Y.; Nielsen, P.V.; Huang, X. Spatial distribution of infection risk of SARS transmission in a hospital ward. Build. Environ. 2009, 44, 1651–1658. [Google Scholar] [CrossRef]
- Guo, Y.; Qian, H.; Sun, Z.; Cao, J.; Liu, F.; Luo, X.; Ling, R.; Weschler, L.B.; Mo, J.; Zhang, Y. Assessing and controlling infection risk with Wells-Riley model and spatial flow impact factor (SFIF). Sustain. Cities Soc. 2021, 67, 102719. [Google Scholar] [CrossRef]
- Rudnick, S.N.; Milton, D.K. Risk of indoor airborne infection transmission estimated from carbon dioxide concentration. Indoor Air 2003, 13, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Stabile, L.; Pacitto, A.; Mikszewski, A.; Morawska, L.; Buonanno, G. Ventilation procedures to minimize the airborne transmission of viruses in classrooms. Build. Environ. 2021, 202, 108042. [Google Scholar] [CrossRef]
- Melikov, A.K. COVID-19: Reduction of airborne transmission needs paradigm shift in ventilation. Build. Environ. 2020, 186, 19–21. [Google Scholar] [CrossRef]
- Gil-Baez, M.; Lizana, J.; Becerra Villanueva, J.A.; Molina-Huelva, M.; Serrano-Jimenez, A.; Chacartegui, R. Natural ventilation in classrooms for healthy schools in the COVID era in Mediterranean climate. Build. Environ. 2021, 206, 108345. [Google Scholar] [CrossRef]
- ECLAC-UNESCO, Education in the Time of COVID-19. 2020. Available online: https://www.cepal.org/en/publications/45905-education-time-covid-19 (accessed on 15 April 2022).
- Kogevinas, M.; Castaño Vinyals, G.; Karachaliou, M.; Espinosa, A.; De Cid, R.; Garcia Aymerich, J.; O’callaghan Gordo, C.; Moncunill, G.; Dobaño, C.; Tonne, C. Ambient air pollution and risk of SARS-CoV-2 infection and of COVID-19 disease in a cohort study in Catalonia (COVICAT Cohort). ISEE Conf. Abstr. 2021, 2021, 1–10. [Google Scholar] [CrossRef]
- Heiselberg, P.; Dam, H.; Sorensen, L.C.; Nielsen, P.V.; Svidt, K. Characteristics of Air Flow through Windows. Indoor Environ. Eng. 1999, R9940, 1–9. [Google Scholar]
- Masood, O.A.; Guirguis, N.M.; Al-hady, M.I.A.; Fahmi, A.A. Windows Factors Impact on Air Speed and Quality Inside Architectural Spaces. Int. J. Appl. Eng. Res. 2018, 13, 12146–12156. [Google Scholar]
- American Society of Heating Refrigerating and Air-Conditioning Engineers (ASHRAE). Ventilation for Acceptable Indoor Air Quality; ASHRAE: Atlanta, GA, USA, 2019; Available online: https://www.ashrae.org/technical-resources/bookstore/standards-62-1-62-2 (accessed on 20 February 2022).
- Rock, B.A.; Anderson, R. Simplified Air Modeling Effectiveness National Renewable Energy Laboratory University of Colorado at Boulder Brandemuehl, 1992, June. pp. 1–37. Available online: file:///C:/Users/MDPI/Downloads/4737.pdf (accessed on 15 April 2022).
- Gungor, K.; Airah, M. Guide to air change effectiveness. Ecolibrium 2013, 33–39. [Google Scholar]
- Memarzadeh, F.; Xu, W. Role of air changes per hour (ACH) in possible transmission of airborne infections. Build. Simul. 2012, 5, 15–28. [Google Scholar] [CrossRef] [PubMed]
- CIRES—Cooperative Institute for Research in Environmental Sciences at the University of Colorado COVID-19 Airborne Transmission Tool Available. 2020. Available online: https://cires.colorado.edu/news/covid-19-airborne-transmission-tool-available (accessed on 15 April 2022).
- American Society of Heating Refrigerating and Air-Conditioning Engineers (ASHRAE). Ventilation and Acceptable Indoor Air Quality in Residential Buildings; ASHRAE: Atlanta, GA, USA, 2016; Available online: www.ashrae.org (accessed on 15 April 2022).
- Kopel, J.; Perisetti, A.; Roghani, A.; Aziz, M.; Gajendran, M.; Goyal, H. Racial and Gender-Based Differences in COVID-19. Front. Public Health 2020, 8, 418. [Google Scholar] [CrossRef]
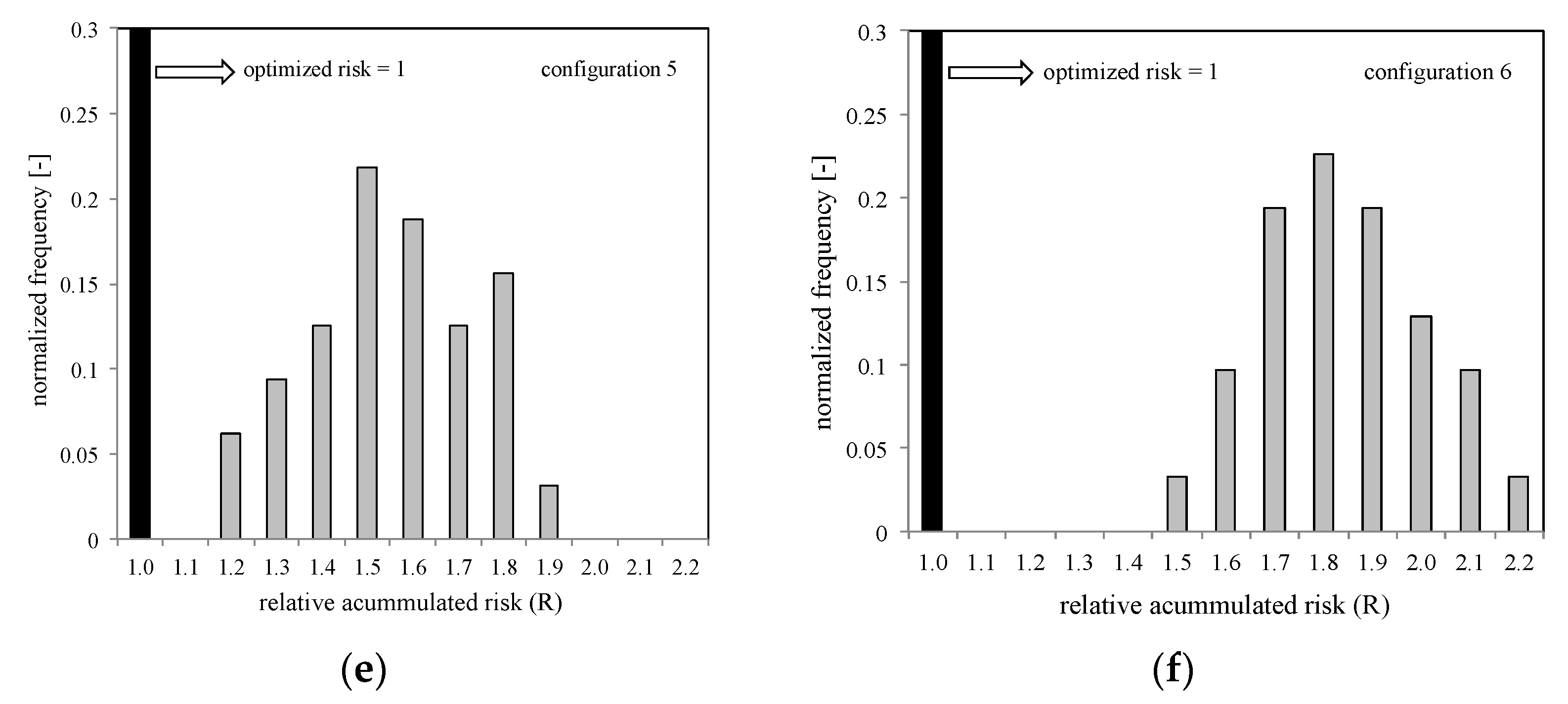
| Centre | Code | CC | Control Group: Classroom with Non-Optimized Student Arrangement | Case Study Group: Classroom with Optimized Student Arrangement | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of Students | Accumulated Incidence | Number of Students | Accumulated Incidence | |||||||
| M | F | M | F | M | F | M | F | |||
| High-School | HS1 | C | 12 | 15 | 3 | 2 | 14 | 12 | 2 | 1 |
| HS2 | A | 15 | 9 | 2 | 2 | 13 | 10 | 3 | 2 | |
| HS3 | C | 14 | 17 | 4 | 3 | 21 | 17 | 2 | 1 | |
| University | U1 | E | 28 | 26 | 6 | 5 | 32 | 22 | 3 | 2 |
| U2 | C | 13 | 18 | 4 | 4 | 18 | 18 | 2 | 2 | |
| U3 | F | 17 | 15 | 8 | 2 | 14 | 12 | 1 | 1 | |
| U4 | F | 32 | 25 | 9 | 7 | 28 | 28 | 4 | 3 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miguel Molina-Jordá, J. Model and Validation Study for Optimizing Students’ Positions in Classrooms to Limit the Spread of Infectious Diseases Such as COVID. Educ. Sci. 2022, 12, 390. https://doi.org/10.3390/educsci12060390
Miguel Molina-Jordá J. Model and Validation Study for Optimizing Students’ Positions in Classrooms to Limit the Spread of Infectious Diseases Such as COVID. Education Sciences. 2022; 12(6):390. https://doi.org/10.3390/educsci12060390
Chicago/Turabian StyleMiguel Molina-Jordá, José. 2022. "Model and Validation Study for Optimizing Students’ Positions in Classrooms to Limit the Spread of Infectious Diseases Such as COVID" Education Sciences 12, no. 6: 390. https://doi.org/10.3390/educsci12060390
APA StyleMiguel Molina-Jordá, J. (2022). Model and Validation Study for Optimizing Students’ Positions in Classrooms to Limit the Spread of Infectious Diseases Such as COVID. Education Sciences, 12(6), 390. https://doi.org/10.3390/educsci12060390






