Pre-Clerkship Medical Students’ Experiences and Perspectives of System 1 and System 2 Thinking: A Qualitative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Approach
2.2. Study Context
2.3. Recruitment
2.4. Data Collection
2.5. Reflexivity
2.6. Data Analysis
3. Results
I don’t think I would know about the names of these different thinking systems if it wasn’t for your research project. I don’t think we’ve specifically talked about dual process theory. I know we’ve talked about heuristics. Is that the right word? About problems with reasoning. I don’t remember if that was in CAS or SRCC. But I know we’ve talked a lot about how doctors do a lot of this. We didn’t say System 1. But a lot of this pattern recognition, quick judgment in diagnoses. And that the best physicians are the ones that can recognize that there’s bias and there’s problems with that thinking, and can use the more analytical, complete thought process. But we didn’t really talk about how that’s System 1 and System 2. (S12)
3.1. Cognitive Processes
I read the student guide which… it’s a bit more effortful because it takes time to read… but then I visualize what the guide is actually saying: how I would maneuver, or how I would perform this maneuver, how I would put it all together so it makes sense in a chronological order, when actually seeing a patient. Then I practice that on the standardized patient. Generating mental imagery helps me transition over time to a System 1 approach: where I’m moving the patient intuitively, I’m manipulating the abdomen, or performing independently what the student guide was stipulating. (S08)
I need to know definitive facts about a subject. This is related to this, and this is always going to be related to this. That helps me make the connections clear in my mind to get that baseline of whatever kind of topic I’m thinking about. (S02)
Okay, this person’s going into septic shock. Okay, let me open up my brain file cabinet on septic shock and go through my normal processing of this. And then it’s just having that ability and awareness… again, which comes through time I think… that if there’s a red flag that goes off, and it says, “Okay, this is abnormal. This is not what it is,” that’s when you need to be able to stop, slow down, switch over, and think logically, analytically. (S10)
3.2. Deliberate Practice
Only through repetition can you really establish System 1…You could read about how to apply EKG [electrocardiogram] leads, and you could know it off the top of your head. How to apply it to the exact locations and which leads go where. But you have to do it at some point. You’re not going to get that muscle memory—that’s what I kind of attribute to System 1—automatic, muscle memory. Because you’re not going to get that until you actually physically do it and you repeat it a few times. (S02)
I use ANKI for [learning retrieval] repetition. I test myself. I ask myself questions with my ANKI cards and continue to do that. If I learn something new on Monday, by Friday I’ve seen that content tons of times. So when I go to weekly case review and faculty ask something—boom—I’ve seen this a hundred times, I’ve seen this so often that it clicks in my head. (S05)
3.3. Learning Environment: Being Alone or Being Together
Sketchy videos [informative, sketch-based learning videos; SketchyMedical, Sketch Group LLC] have helped me go from effortful, slow thinking about pharmacology and microbiology to very fast, intuitive thinking. But I don’t like distractions. I can’t watch the videos with anybody around. (S08)
I tend to be more of a solitary learner, so I learn better when I just can focus and sit by myself and have my time with the material. Although I prefer learning on my own in a solitary way, it’s sometimes hard to gauge whether I really understand the material or not. So then, when somebody mentions something that we learned that I don’t have a clear grasp on, it becomes very apparent. (S09)
I think [collaborative classroom events] might be too fast paced for me. And I think it’s the group setting. I’m not always comfortable raising my hand and asking questions or stopping. And also, our CCs often have a lot of material to get through, like a big long worksheet to get through in one hour. So we always end up splitting it up amongst our group like, I’ll do whatever…question four…and I’ll then I can learn how to answer question four, but I have no idea how to do any of the other questions on the paper. (S06)
“It’s because I have not had enough time to consolidate the material and I’m trying to go directly to System 1, but I haven’t had enough time to really develop it in my head. So I’m still on System 2 when we get to CC, and even then I can’t perform that well on System 2 and that’s where I’m at when I’m in CC. I’m still trying to figure things out, and we’re moving so quickly trying to answer all the questions and explain it to people and I’m just like, “I haven’t learned this yet.” So I’m still in System 2 when we get to CC.” (S05)
3.4. Stickiness Factor
I get pimped quite often in MeSH. Sometimes I just don’t know the answer, so I try to reason through possible answers. What type of therapy should we give this patient? Or what are underlying causes of presenting symptoms? My nervous system is going crazy because I don’t know the answer immediately and its awkward silence, where I’m almost embarrassed. But afterwards I don’t forget it. Once we talk it out together and it does make sense, I can make that connection again easily. (S08)
I feel like you remember things a lot more when you get them wrong and you were embarrassed in that moment. Whenever you see a case like it again, you’re like, “Oh, my god I remember that one time I was super embarrassed because I got this wrong.” Then you just spew out the answer when you are presenting because you remember automatically. (S07)
3.5. Biases and Heuristics
I can give you a great example where I was wrong. My pattern recognition in our pulmonary embolism [problem-based learning] case. Looking through the EKG data, my mind immediately recognized what I thought was a pattern. I believed it was an inferior myocardial infarction. I didn’t do a more detailed analysis of the EKG and really compare it well with the patient’s presentation. I just kind of saw what I wanted to see to make it work with what I had quickly jumped to, the diagnosis in my head. (S12)
When I first see a patient… mostly I think what’s their chief concern? What’s the thing that they want to prioritize in that visit? And then from there I create a list of differential diagnoses. Like…there is always an issue or there is always the dilemma of…okay…how do I get out of my natural heuristic of immediately going to my familiar top diagnoses versus generating a long list of different things that I should consider? (S01)
3.6. Prior Experience of Attaining Competence
I’m trying to use more of System 2 but I think that my default is System 1… I think my previous experience [as a paramedic] has given me some kind of a background of patterns to recognize… I had to quickly treat a patient and I didn’t necessarily have all of the time that I would like to reason through it. Our [paramedic] program emphasized reflexive, pattern recognition of presentation or vitals rather than understanding the pathology or why the patient looks like this or why I’m treating with this medicine or intervening through these actions. (S12)
Before medical school I worked in basic and translational research. That arena is very conducive for System 2 thinking. You’re trying to answer a research question. You come up with a hypothesis and then you come up with how you’re going to test out that hypothesis… And the data analysis… you have a lot of time to look at the data and sit with the data, consult with related literature, and think about what is this actually telling me?... So there’s just a lot more room to do the System 2 kind of thinking. And it tends to be very…you have to be very methodical. You have a protocol. If you’re being very methodical and effortful and logical, then you tend to do a better job than if you do things too quickly in that setting. (S09)
4. Discussion
4.1. Intersection with Self-Regulated Learning and Cognitive Load Theory
4.2. Heuristics
4.3. Implications for Medical Education
4.4. Limitations
4.5. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Pre-Interview Guide
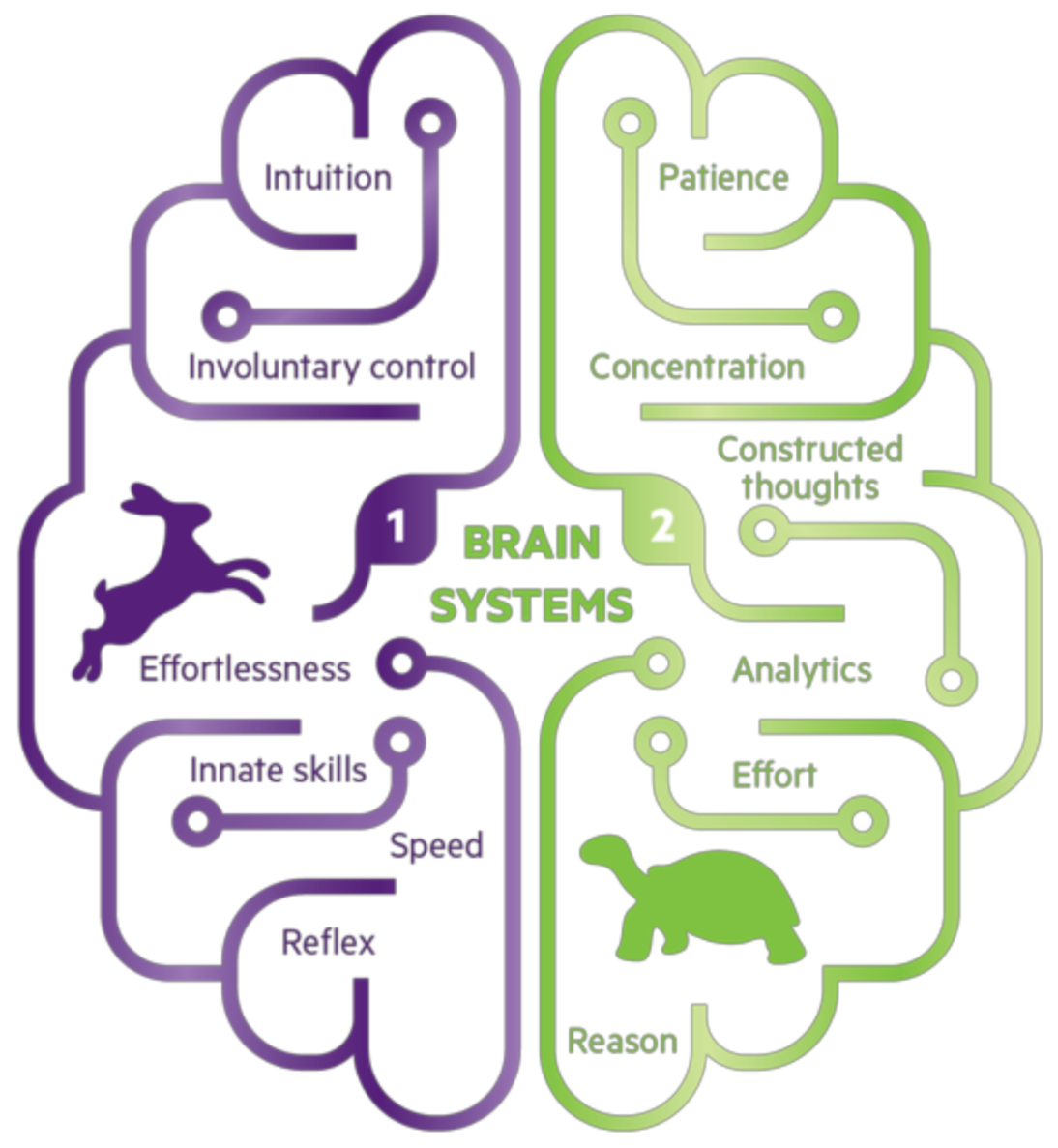
- “System 1 is the fast, automatic, emotional, subconscious process that drives intuitive decisions.” (Aragón 2017) [54];
- “System 2 is the slow, reflective, rational, conscious process that enables deliberative decisions.” (Aragón 2017) [54].
Appendix B
Interview Questions
- -
- how would you explain them to someone who hadn’t heard of them before?
- -
- can you talk me through examples of when you have had to use these skills already?
- -
- what were the outcomes?
- -
- what other pre-clerkship opportunities exist to use these different types of thinking processes at the Frank H. Netter MD School of Medicine?
- -
- can you talk me through an example?
- -
- what about when learning situations or responding to questions?
- -
- how often do trust your first instinct or intuition?
- -
- how often do you revise these decisions? why or why not?
- -
- same question, but how and when do you make decisions slowly?
- -
- can you talk me through an example?
- -
- what have been the outcomes when implementing System 2 thinking?
References
- Cutrer, W.B.; Sullivan, W.M.; Fleming, A.E. Educational strategies for improving clinical reasoning. Curr. Probl. Pediatric Adolesc. Health Care 2013, 43, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Rencic, J.; Durning, S.; Holmboe, E.; Gruppen, L.D. Assessing competence in professional performance across disciplines and professions. In Innovation and Change in Professional Education; Wimmers, P.F., Mentkowski, M., Eds.; Springer International Publishing: Cham, Switzerland, 2016. [Google Scholar]
- Kelman, M. The Heuristics Debate; Oxford University Press: New York, NY, USA, 2011. [Google Scholar]
- Croskerry, P. Clinical cognition and diagnostic error: Applications of a dual process model of reasoning. Adv. Health Sci. Educ. 2009, 14, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Stanovich, K.E. Who is Rational? Studies of Individual Differences in Reasoning; Lawrence Elrbaum Associates: Mahwah, NJ, USA, 1999. [Google Scholar]
- Stanovich, K.E.; West, R.F. Individual differences in reasoning: Implications for the rationality debate? Heuristics Biases 2002, 39, 421–440. [Google Scholar] [CrossRef]
- Evans, J.S.B.T. In two minds: Dual-process accounts of reasoning. Trends Cogn. Sci. 2003, 7, 454–459. [Google Scholar] [CrossRef]
- Hogarth, R.M. Educating Intuition; University of Chicago Press: Chicago, IL, USA, 2001. [Google Scholar]
- Hogarth, R.M. Deciding analytically or trusting your intuition? The advantages and disadvantages of analytic and intuitive thought. In Routines of Decision Making; Betsch, T., Haberstroh, S., Eds.; Lawrence Elrbaum Associates: Mahwah, NJ, USA, 2005; pp. 67–82. [Google Scholar]
- Croskerry, P. Context is everything or how could I have been that stupid? Health Q. 2009, 12, e171–e176. [Google Scholar] [CrossRef] [PubMed]
- Croskerry, P. A universal model of diagnostic reasoning. Acad. Med. 2009, 84, 1022–1028. [Google Scholar] [CrossRef]
- Rotgans, J.I.; Schmidt, H.G.; Rosby, L.V.; Tan, G.J.S.; Mamede, S.; Zwaan, L.; Low-Beer, N. Evidence supporting dual-process theory of medical diagnosis: A functional near-infrared spectroscopy study. Med. Educ. 2019, 53, 143–152. [Google Scholar] [CrossRef]
- Moulton, C.-A.; Regehr, G.; Mylopoulos, M.; Macrae, H.M. Slowing down when you should: A new model of expert judgment. Acad. Med. 2007, 82, S109–S116. [Google Scholar] [CrossRef]
- Croskerry, P. Critical thinking and reasoning in emergency medicine. In Patient Safety in Emergency Medicine; Croskerry, P., Cosby, K.S., Schenkel, S.M., Wears, R.L., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008; pp. 213–218. [Google Scholar]
- Ericsson, K.A. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad. Med. 2004, 79, S70–S81. [Google Scholar] [CrossRef]
- Choudhry, N.K.; Fletcher, R.H.; Soumerai, S.B. Systematic review: The relationship between clinical experience and quality of health care. Ann. Intern. Med. 2005, 142, 260–273. [Google Scholar] [CrossRef]
- Tay, S.W.; Ryan, P.; Ryan, A. Systems 1 and 2 thinking processes and cognitive reflection testing in medical students. Can. Med. Educ. J. 2016, 7, e97–e103. [Google Scholar] [CrossRef] [PubMed]
- Quirk, M. Intuition and metacognition in medical education: Keys to developing expertise. In Springer Series on Medical Education; Springer Publishing Company: New York, NY, USA, 2006. [Google Scholar]
- Blumenthal-Barby, J.S.; Krieger, H. Cognitive biases and heuristics in medical decision making: A critical review using a systematic search strategy. Med. Decis. Mak. 2015, 35, 539–557. [Google Scholar] [CrossRef] [PubMed]
- Sinkovics, R.R.; Alfoldi, E.A. Progressive focusing and trustworthiness in qualitative research: The enabling role of computer-assisted qualitative data analysis software (CAQDAS). Manag. Int. Rev. 2012, 52, 817–845. [Google Scholar] [CrossRef]
- Parlett, M.; Hamilton, D. Evaluation as illumination: A new approach to the study of innovative programmes. In Evaluation Studies Review Annual; Glass, G., Ed.; Sage: Beverley Hills, CA, USA, 1976; pp. 140–157. [Google Scholar]
- Bringer, J.D.; Johnston, L.H.; Brackenridge, C.H. Maximizing transparency in a doctoral thesis: The complexities of writing about the use of QSR*NVIVO within a grounded theory study. Qual. Res. 2004, 4, 247–265. [Google Scholar] [CrossRef]
- Locke, K.; Golden-Biddle, K.; Feldman, M.S. Perspective—Making doubt generative: Rethinking the role of doubt in the research process. Organ. Sci. 2008, 19, 907–918. [Google Scholar] [CrossRef]
- King, N. Doing template analysis. In Qualitative Methods and Analysis in Organizational Research; Symon, G., Cassell, C., Eds.; Sage: London, UK, 2012; pp. 426–450. [Google Scholar]
- Lincoln, Y.; Guba, E. Naturalistic Inquiry; SAGE Publications Ltd.: London, UK, 1985. [Google Scholar]
- Langdridge, D. Phenomenological Psychology: Theory, Research and Method; Pearson Education: London, UK, 2007. [Google Scholar]
- Onwuegbuzie, A.J.; Combs, J.P. Emergent data analysis techniques in mixed methods research—A synthesis. In SAGE Handbook of Mixed Methods in Social & Behavioural Research; Tashakkori, A., Teddlie, C., Eds.; SAGE Publications: Thousand Oaks, CA, USA, 2010; pp. 397–430. [Google Scholar]
- Butler-Kisber, L. Constant comparison inquiry. In Qualitative Inquiry; Butler-Kisber, L., Ed.; SAGE Publications Ltd.: London, UK, 2018; pp. 41–59. [Google Scholar]
- Browncoat, J. Pimping. Urban Dictionary. 2006. Available online: https://www.urbandictionary.com/define.php?term=pimping (accessed on 15 August 2020).
- Van Merriënboer, J.J.G.; Kester, L.; Paas, F. Teaching complex rather than simple tasks: Balancing intrinsic and germane load to enhance transfer of learning. Appl. Cogn. Psychol. 2006, 20, 343–352. [Google Scholar] [CrossRef]
- Mizuno, K.; Tanaka, M.; Yamaguti, K.; Kajimoto, O.; Kuratsune, H.; Watanabe, Y. Mental fatigue caused by prolonged cognitive load associated with sympathetic hyperactivity. Behav. Brain Funct. 2011, 7, 17. [Google Scholar] [CrossRef]
- Van Merriënboer, J.; Sweller, J. Cognitive load theory in health professional education: Design principles and strategies. Med. Educ. 2010, 44, 85–93. [Google Scholar] [CrossRef]
- Cleary, T.J.; Durning, S.J.; Gruppen, L.D.; Hemmer, P.; Artino, A.R. Self-regulated learning in medical education. In Oxford Textbook of Medical Education; Walsh, K., Ed.; Oxford University Press: Oxford, UK, 2013. [Google Scholar]
- Young, J.Q.; Van Merrienboer, J.; Durning, S.; Cate, O.T. Cognitive Load Theory: Implications for medical education: AMEE Guide No. 86. Med. Teach. 2014, 36, 371–384. [Google Scholar] [CrossRef]
- Gandomkar, R.; Mirzazadeh, A.; Jalili, M.; Yazdani, K.; Fata, L.; Sandars, J. Self-regulated learning processes of medical students during an academic learning task. Med. Educ. 2016, 50, 1065–1074. [Google Scholar] [CrossRef]
- Leppink, J.; Duvivier, R. Twelve tips for medical curriculum design from a cognitive load theory perspective. Med. Teach. 2016, 38, 669–674. [Google Scholar] [CrossRef] [PubMed]
- Sewell, J.L.; Maggio, L.A.; Cate, O.T.; Van Gog, T.; Young, J.Q.; O’Sullivan, P.S. Cognitive load theory for training health professionals in the workplace: A BEME review of studies among diverse professions: BEME Guide No. 53. Med. Teach. 2019, 41, 256–270. [Google Scholar] [CrossRef] [PubMed]
- Zheng, B.; Ward, A.; Stanulis, R. Self-regulated learning in a competency-based and flipped learning environment: Learning strategies across achievement levels and years. Med. Educ. Online 2020, 25, 1686949. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, B.J. Investigating self-regulation and motivation: Historical background, methodological developments, and future prospects. Am. Educ. Res. J. 2008, 45, 166–183. [Google Scholar] [CrossRef]
- Sweller, J. Cognitive load during problem solving: Effects on learning. Cogn. Sci. 1988, 12, 257–285. [Google Scholar] [CrossRef]
- Mayer, R.E.; Moreno, R. Nine ways to reduce cognitive load in multimedia learning. Educ. Psychol. 2003, 38, 43–52. [Google Scholar] [CrossRef]
- Shunk, D. Goal and self-evaluative influences during children’s cognitive skill learning. Am. Educ. Res. J. 1996, 33, 359–382. [Google Scholar] [CrossRef]
- Harris, K.R.; Graham, S. Programmatic intervention research: Illustrations from the evolution of self-regulated strategy development. Learn. Disabil. Q. 1999, 22, 251–262. [Google Scholar] [CrossRef]
- Schraw, G.; Crippen, K.J.; Hartley, K. Promoting self-regulation in science education: Metacognition as part of a broader perspective on learning. Res. Sci. Educ. 2006, 36, 111–139. [Google Scholar] [CrossRef]
- Kirschner, F.; Paas, F.; Kirschner, P.A. A cognitive load approach to collaborative learning: United brains for complex tasks. Educ. Psychol. Rev. 2009, 21, 31–42. [Google Scholar] [CrossRef]
- Zimmerman, B.J. Development and adaptation of expertise: The role of self-regulatory processes and beliefs. In The Cambridge Handbook of Expertise and Expert Performance; Ericsson, K.A., Charness, N., Feltovich, P.J., Hoffman, R.R., Eds.; Cambridge University Press: New York, NY, USA, 2006; pp. 705–723. [Google Scholar]
- Issenberg, S.B.; McGaghie, W.C.; Petrusa, E.R.; Lee, G.D.; Scalese, R.J. Features and uses of high-fidelity medical simulations that lead to effective learning: A BEME systematic review. Med. Teach. 2005, 27, 10–28. [Google Scholar] [CrossRef] [PubMed]
- Karpicke, J.D.; Blunt, J.R. Retrieval practice produces more learning than elaborative studying with concept mapping. Science 2011, 331, 772–775. [Google Scholar] [CrossRef] [PubMed]
- McDaniel, M.A.; Wildman, K.M.; Anderson, J.L. Using quizzes to enhance summative-assessment performance in a web-based class: An experimental study. J. Appl. Res. Mem. Cogn. 2012, 1, 18–26. [Google Scholar] [CrossRef]
- Rosby, L.V.; Rotgans, J.I.; Tan, G.; Low-Beer, N.; Mamede, S.; Zwaan, L.; Schmidt, H. Inducing System-1-type diagnostic reasoning in second-year medical students within 15 min. Med. Teach. 2018, 40, 1030–1035. [Google Scholar] [CrossRef]
- Simpson, D.; Hamilton-Shield, A.; Giza, M.; Baker, J. Comment on: Inducing system-1-type diagnostic reasoning in second-year medical students within 15 min. Med. Teach. 2019, 41, 483. [Google Scholar] [CrossRef]
- Lee, C.S.; Nagy, P.G.; Weaver, S.J.; Newman-Toker, D.E. Cognitive and system factors contributing to diagnostic errors in radiology. Am. J. Roentgenol. 2013, 201, 611–617. [Google Scholar] [CrossRef]
- Furnham, A.; Boo, H.C. A literature review of the anchoring effect. J. Socio-Econ. 2011, 40, 35–42. [Google Scholar] [CrossRef]
- Aragón, T.J. How You Actually Make Decisions Will Surprise You. 2017. Available online: https://taragonmd.github.io/2017/12/08/how-you-actually-make-decisions-will-surprise-you/ (accessed on 15 August 2020).
- Kahneman, D.; Tversky, A. Subjective probability: A judgment of representativeness. Cogn. Psychol. 1972, 3, 430–454. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Availability: A heuristic for judging frequency and probability. Cogn. Psychol. 1973, 5, 207–232. [Google Scholar] [CrossRef]
- Taylor, S.E. The interface of cognitive and social psychology. In Cognition, Social Behavior, and the Environment; Harvey, J.H., Ed.; Lawrence Erlbaum Associates Inc.: Hillsdale, NJ, USA, 1981; pp. 189–211. [Google Scholar]
- Lefroy, J.; Watling, C.; Teunissen, P.W.; Brand, P. Guidelines: The do’s, don’ts and don’t knows of feedback for clinical education. Perspect. Med. Educ. 2015, 4, 284–299. [Google Scholar] [CrossRef]
- Association of American Medical Colleges. Recommendations for Preclerkship Clinical Skills Education for Under-graduate Medical Education. Task Force on the Clinical Skills Education of Medical Students. 2008. Available online: https://paeaonline.org/wp-content/uploads/2016/07/7a-Clinical-Skills-Education.pdf (accessed on 16 July 2020).
- Panadero, E. A Review of Self-regulated Learning: Six Models and Four Directions for Research. Front. Psychol. 2017, 8, 422. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5408091/ (accessed on 18 July 2020).
- Cutrer, W.B.; Miller, B.; Pusic, M.V.; Mejicano, G.; Mangrulkar, R.S.; Gruppen, L.D.; Hawkins, R.E.; Skochelak, S.E.; Moore, D.E., Jr. Fostering the development of master adaptive learners: A conceptual model to guide skill acquisition in medical education. Acad. Med. 2017, 92, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Land, S. Illustration of the Characteristics Ascribed to System 1 and System 2 Thinking. 2018. Available online: https://siimland.com/thinking-fast-and-slow-explained/ (accessed on 15 December 2020).

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanders, W.; McHugh, D. Pre-Clerkship Medical Students’ Experiences and Perspectives of System 1 and System 2 Thinking: A Qualitative Study. Educ. Sci. 2021, 11, 34. https://doi.org/10.3390/educsci11020034
Sanders W, McHugh D. Pre-Clerkship Medical Students’ Experiences and Perspectives of System 1 and System 2 Thinking: A Qualitative Study. Education Sciences. 2021; 11(2):34. https://doi.org/10.3390/educsci11020034
Chicago/Turabian StyleSanders, William, and Douglas McHugh. 2021. "Pre-Clerkship Medical Students’ Experiences and Perspectives of System 1 and System 2 Thinking: A Qualitative Study" Education Sciences 11, no. 2: 34. https://doi.org/10.3390/educsci11020034
APA StyleSanders, W., & McHugh, D. (2021). Pre-Clerkship Medical Students’ Experiences and Perspectives of System 1 and System 2 Thinking: A Qualitative Study. Education Sciences, 11(2), 34. https://doi.org/10.3390/educsci11020034





