Abstract
The aims of this study were to investigate the feasibility of an experiential learning initiative led by minority exercise science undergraduates and to observe the adaptations after a 10-week high-intensity functional training (HIFT) program in 34 underrepresented, hypertensive, and overweight/obese professional firefighters (PFF; age: 36.8 ± 11.0 years, body weight: 97.3 ± 21.5 kg, height: 181.7 ± 6.6 cm; BMI: 29.2 ± 4.9 kg/m2). Data were analyzed for muscular strength and endurance, cardiorespiratory endurance, body composition, agility, flexibility, and readiness for change. The PFFs trained two to three times weekly during their work shifts at vigorous intensity for 40 min. Their resting diastolic blood pressure and resting heart rate significantly decreased. Improvements in agility, muscular strength, and readiness for change were observed. This HIFT experiential learning initiative was feasible and beneficial and improved the PFFs’ health and physical fitness with limited resources. Accredited programs in exercise science participating in low-cost initiatives may aid in mitigating public service workers’ compensation and injury rates to better respond to occupational demands.
1. Introduction
Experiential learning, such as services or experiences, has long been used as a principal constituent to foster the application of concepts and skills learned in the classroom to real-world public situations [1,2]. According to Rogers [3], experiential learning refers to an active learning approach that allows trainees to use and critically process knowledge, skills, abilities (KSAs), and experience gain via the educational process. Previous studies examining learning in a wide array of disciplines found that experiential learning effectively leads to better learning results [4,5,6,7]. Service learning (SL), a form of experiential learning [8], is designed to foster a collaboration between students and community or health organization(s) to provide an opportunity to eventually apply learned KSAs to meet the needs of a specific community [9]. Researchers from several studies examining SL programs in kinesiology have documented the benefits of students’ participation, including enhanced levels of self-efficacy [10], moral development [11], deeper understanding of course contents [7], and greater interaction with culturally different individuals [12]. Accordingly, SL within the discipline of kinesiology could deliver an exercise intervention to community firefighters who are hypertensive and overweight.
Firefighting is commonly recognized as one of the most physically demanding and dangerous occupations in the public sector. While performing their duties, firefighters must wear personal protective equipment (PPE), adding an external load of approximately 90 lbs and further increasing the physiological burden of the occupation [13]. It has been demonstrated that PPE increases energy expenditure during a firefighting task by 33% and decreases the maximal oxygen capacity by 20% [14]. Given the working conditions and physiological demands of firefighting, a firefighter’s physical condition is critical for optimal performance. Interestingly, many states in the USA do not mandate annual fitness assessments of their firefighters. As such, overweight (75%) and obesity (35%) in US firefighters are extremely common [15], resulting in many firefighters not meeting the proposed levels of cardiorespiratory fitness or metabolic equivalents for aerobic capacity [16,17]. Although the National Fire Protection Association (NFPA) has standards for the health risk of firefighters [18], there are currently no nationwide enforceable physical activity requirements to sustain firefighters’ physical fitness to safeguard them from obesity, injury, musculoskeletal disorder, and cardiovascular-related events post-academy.
Given the importance of fitness for firefighters, innovative techniques for improving their overall fitness relative to their unique job demands are needed. One promising approach is high-intensity functional training (HIFT), which is an approach to exercise that conveys both aerobic and muscle-strengthening exercises, emphasizing functional multi-joint movements at vigorous intensity. Most HIFT methodologies use increased work capacity overtime, combining mono-structural exercise (e.g., running) with weight movements (e.g., squats, push-ups) and weightlifting derivatives (e.g., snatch, shoulder press, deadlift) [19]. These exercise modalities may be a better way for firefighters to prepare for their physiological demands, given the similar movement patterns that mimic actual firefighting tasks. A recent investigation evaluated a HIFT program used for fire academy recruits and found that a 10-week online-based training program resulted in significant improvements in maximal oxygen consumption (VO2max), body composition, and grip strength relative to a control group subjected to habitual exercise pattern [20].
While fire departments and city managers are working to improve fitness and health among its workers, key research data are lacking for the firefighter population, especially where it pertains to practical conditioning modalities such as HIFT. In this paper, we describe a service-learning initiative in kinesiology to administer a HIFT exercise program addressing the fitness and wellness of city firefighters. The initiative allowed underrepresented undergraduate students enrolled in an exercise testing and prescription course, an internship culminating experience of 225 h/semester, and a capstone course preparing students for in-field professional certifications, to administer the ten-week long vigorous intensity exercise intervention to deconditioned firefighters. Anatomy and Physiology I and II with laboratories were prerequisites for the aforementioned kinesiology courses as part of the CoAES Accreditation for Exercise Science Programs [21,22]. The purpose of this study was to (1) test the feasibility of a large-scale SL in kinesiology to address the needs of a community partner, and (2) to administer a ten-week HIFT program to deconditioned firefighters to improve their health and wellness.
2. Materials and Methods
2.1. Participants
The study was conducted in accordance with the Declaration of Helsinki and the protocol #20190205001 was approved by the Institutional Review Board at the university following the US Federal Policy for the Protection of Human Subjects. The participants provided consent prior to the start of the study. Forty-seven career firefighters from a city fire department (CRFD) in the southeast of the United States volunteered to determine their eligibility and were asked to complete the Physical Activity Readiness Questionnaire [23], a medical/health history form adapted from Box 3.1 [24] (p. 47), a pre-COVID waiver of liability reviewed and approved by the university legal affairs department (all student trainers were covered by an umbrella liability coverage from the university as part of their course fees approved by the university system), and the medical clearance form provided by the City Management Human Resources as part of their occupational medical forms. The inclusion criteria for participation were subjects who were (1) a career firefighter at the CRFD and (2) at least 18 years old. Exclusion criteria were (1) any contraindications (e.g., cardiovascular or orthopedic conditions) to resistance or endurance exercise as identified by the medical history and clearance forms, (2) pregnancy, (3) active work compensation for physical injury, and (4) currently taking prescription medications for cardiovascular diseases. Of the forty-seven participants initially recruited (Figure 1), 34 firefighters (mean ± SD: age: 36.8 ± 11.0 years, body weight: 97.3 ± 21.5 kg, height: 181.7 ± 6.6 cm) volunteered for the study.
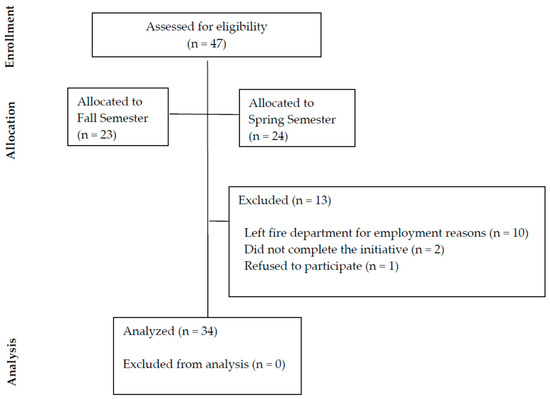
Figure 1.
Participant selection and screening.
The sample size was calculated with an assumed type I error of 0.05 and a type II error rate of 0.10 (90% statistical power); it was suggested that 19 participants would be sufficient to observe moderate effect sizes in the difference between two dependent means [25]. In total, 23 students participated in this initiative by delivering forty-minute exercise sessions two to three times a week, including a warm-up and cool down of five minutes each, under the supervision of graduating undergraduate interns supervised by certified university faculty.
2.2. Procedures
This study followed a convenience single-group longitudinal research design. Measurement outcomes were collected the week before and the week after a 10-week exercise training intervention. Participating volunteers obtained blank forms delivered at the firefighting station by students during the second week of the 16-week long university semester. Eligibility screening (week 2), primary pre/post outcome measures (weeks 3–4 and week 16), and the training intervention described below (weeks 5–15) happened at the City Recreation Center (CRC) located a mile away from the station. The firefighters dropped in for their screening depending on their work shift during the third week of the semester. Once cleared, they completed the exercise testing sessions during their day-time work shift at their convenience during weeks 3 and 4. For exercise testing and prescription, the participants were asked to refrain from strenuous physical activity and alcohol and caffeine consumption 24 h preceding testing. The participants were also instructed to avoid heavy meals three hours preceding tests. The testing procedures were rehearsed between students at the laboratory on campus with faculty prior to being administered by pairing one student under the supervision of an intern at the CRC. Interns were also coached and supervised remotely by both full- and part-time faculty. The faculty tracked the proposed exercise prescriptions by the student-trainers weekly using a secured cloud storage space to store, organize, share, and access information for exercise safety review and feedback. For each exercise testing and prescription session and on a needed basis, students were in direct contact with the faculty using a chat-based collaboration platform for some non-Health Insurance Portability and Accountability Act (HIPAA) document sharing and online approved communication. For confidentiality and privacy purposes, each firefighter was assigned a unique code and only that code was posted on all forms during data collection and used for all online communication. Equipment for exercise testing was purchased ahead of week 3 by the CRFD Chief of Fire from a list of online vendors selected by the interns based on cost effectiveness. To maintain consistency in measurements among participants, the same intern assisted by faculty, supervised the students during the measurements and data collection.
2.3. Measures
2.3.1. Cardiovascular Assessments
Student trainers recorded the firefighters’ resting heart rate (HR) and blood pressure (BP) before each session following procedures published by the American College of Sports Medicine (ACSM) [24] (p. 53). Mid-exercise session HR and BP were checked to regulate the exercise intensity within the desired vigorous limit set by ACSM [24] (p. 150). Recovery HR and BP were recorded at the end of each session. HR was measured with a chest-worn monitor (Polar Electro T31, Lake Success, NY, USA), and BP was measured with a sphygmomanometer and stethoscope after five minutes of sitting quietly in a chair. Two BP measurements were taken one minute apart, and the average of the two was recorded.
The Forestry Step Test was used to calculate the firefighters’ cardiovascular capacity (VO2max) using the methods described by Sharkey et al. [26,27]. Participants stepped up on to and down off of a 15 ¾ inch step to the beat of a metronome set to 90 beats per minute for five minutes. After completing the five minutes of stepping, participants immediately sat on their respective steps and recovery HRs were recorded at 15s post-test. Participants’ HR were reported in beats per minute (bpm) and participants’ recovery HR data were used to obtain gender-specific, age-adjusted, estimated measures of maximal oxygen uptake (estimated VO2max) from a published table [26,27]. The participants’ estimated VO2max values were reported in relative terms or milliliters of oxygen consumed per kilogram of body weight per minute (mL/kg/min).
2.3.2. Body Composition
This included three separate assessments: (1) percent body fat (%BF), (2) waist to hip ratio, and (3) body mass index (BMI). To assess %BF, skinfolds were measured with a cost-effective skinfold caliper (Sequoia Fitness TrimCal 4000) at seven different anatomical sites: midaxillary, pectoral, triceps, subscapular, abdominal, supra-iliac and thigh skinfold using methods described in Jackson et al. studies [28,29]. Waist and hip circumferences were measured with a flexible tape and used to compute the waist-to-hip ratio according to the standardized procedures published by the World Health Organization [30]. BMI was calculated (body weight in kg/height in m2), with height assessed using a portable stadiometer and body weight assessed using a calibrated scale [31,32].
2.3.3. Agility Test
Agility was assessed with a timed agility T-test. This assessment required the participants to move in a T-shaped pattern requiring lateral and front-to-back movements. The agility test was administered using the protocol outlined in Semenick [33]. The subjects began with both feet behind the starting point A. At their own discretion, each subject sprinted forward 9.14 m (10 yd) to point B touching the cone with the right hand. Then, they shuffled to the left 4.57 m (5 yd) and touched the cone with the left hand. Subjects then shuffled to the right 9.14 m and touched the cone with their right hand. They then shuffled to the left 4.57 m back to the middle (point B) and touched the cone with their left hand. Subjects then ran backward, passing the finish line at point A. Three trials were performed, and times were recorded to the nearest one-hundredth of a second using a low-cost stopwatch. The fastest trial was used for statistical analyses.
2.3.4. Flexibility Test
The Young Men’s Christian Association (YMCA) sit-and-reach test was administered to assess low back and hamstring flexibility using the protocol outlined in Adams and Beam [34]. Participants performed the test after warming up with the agility test. A measuring tape was placed on the floor and a line placed perpendicular to the tape at 38 cm, establishing a consistent reference for all participants. The participants removed their shoes and sat on the floor and aligned their heels to this line 15 cm apart. Placing one hand on top of the other, instructions were given to keep hands on the measuring tape and slowly bend forward, keeping the back straight. The furthest displacement over three repetitions of the test was retained for analysis. During the execution of this test, shoulder motion was visually assessed to minimize scapular protraction.
2.3.5. Muscular Strength Test
A Jamar hand dynamometer was used to measure the firefighters’ dominant hand grip strength (HGS) as a measure of strength, mimicking the handgrip needed for the job requirements. The procedure was explained and the technique was demonstrated to each participant based on the standard procedure recommended by the American Society of Hand Therapists. Subjects were positioned in a straight back chair with both feet flat on the floor. For the arm to be tested, the elbow was flexed to 90°, the forearm in neutral position, wrist in 0–15° of extension, and 0–15° of ulnar deviation. The fingers were flexed as needed for a maximal contraction. A verbal command of “Squeeze! Harder! Harder! Relax!” was given by the examiner. Three trials were conducted to measure the average (mean) HGS, with 1 min rest between each trial [35]. The cut-off value for evaluating the scores for handgrip test was adopted from Wang et al. [36].
For the one-repetition maximum (1-RM) leg press estimation, a prediction equation has been developed using 10 repetitions [37]. This method of 1-RM estimation is based on the relationship between the number of repetitions performed and the actual 1-RM. The student-trainer found the estimation of 1-RM method a more practical and safer alternate to maximal testing. Testing procedures for a 10 RM are similar to that of the 1 RM test [24] (p.101). The participants warmed up with 50% of the estimated 10-RM. They rested for three minutes between sets and proceeded to complete the 10 RM lift at 60 to 80% of the estimated maximum. The estimated leg press was reported in pounds.
2.3.6. Muscular Endurance Tests
A push-up test until physical or mental exhaustion was used to test upper body muscular endurance, as described by ACSM [24] (p. 102). The participants performed controlled push-ups keeping their back straight, with their hands shoulder width apart and feet together and were instructed to lower their body toward the floor until their chin touched the floor. The researchers terminated the test when (1) the participant volitionally terminated the test due to fatigue, (2) the participant could not maintain the appropriate technique within two repetitions, or (3) the participant completed 37 push-ups. The total number of push-ups completed during the test was then recorded by the researchers and the participants were ranked using Table 4.11 from ACSM [24] (p. 106).
2.3.7. Physical Activity Readiness for Change
The transtheoretical model (TTM), aimed at understanding individuals’ behavioral changes based on their dynamic movement through five different stages of behavioral change, was used to check for health behavioral changes [38]. The TTM categorized the respondents into the five behavioral stages [39]: precontemplation, contemplation, preparation, action, and maintenance. These stages are typically operationalized around intent or actual behavior change that has occurred during the first six months. For example, people in the Precontemplation stage of change do not intend to make any health behavior changes within the next six months. On the other hand, people in the Contemplation stage of change are thinking about making changes, typically within the next six months. People in the Preparation stage of change are typically ready to make changes in the next 30 days and have begun to take small steps toward engaging in these new behaviors. People in the Action stage of change have been engaging in the new behaviors for one to six months, and people in the Maintenance stage of change have been engaging in these behaviors for longer than six months. Based on these stages, the students recorded the firefighters’ readiness for change stage and asked three questions: (1) Do you intend to find ways to improve your physical activity level (PA)? (2) In the past three months, how often did you do things to help you be physically active? (3) How long have you been doing things to help you become more physically active? Firefighters who indicated that they were not making behavior changes, not intending to make changes within the next six months, or who were making sporadic changes less than once a month were categorized into the Precontemplation or Contemplation stage of change. Those who indicated that they were already making some behavior changes or intending to in the next month but were only making changes one to three times per month or had only been making more frequent behavior changes for 1 month or less, were categorized into the Preparation stage of change. Lastly, firefighters who indicated that they were already trying to be more physically active, implementing these changes more than once a week, and engaging in these behaviors for more than 1 month, were categorized into the Action stage of change. We did not ask for these for longer than six months, and therefore we did not include the Maintenance stage.
2.3.8. Intervention
Every one-on-one exercise training session started with the recording of resting HR and BP, which were used to determine the vigorous target HR (using the HR Reserve (HRR) method [24]) (p. 150). Each firefighter initiated each session with a 5 min warm-up and ended it with a 5 min cool-down. The initiative started at moderate intensity (HRR < 85%) during the program initiation phase (weeks 3–4). Eight to 10 exercises in a circuit alternating upper and lower body parts for safety, were performed to exhaustion, repeated twice, a full minute rest in between sets, two to three times weekly. All movements were based on the participant’s own body weight and utilized low-cost equipment such as a rope, steps, and sliders. During weeks 5 to 15, the intensity of the functional exercises was increased to vigorous (a minimum of 85% of HRR with a goal of 90%). This was done for all firefighters since they all reacted positively to the moderate intensity and modality during the program initiation phase. During the vigorous intensity functional exercises, the students demonstrated and instructed on the type of exercises to be executed safely under their supervision. To confirm that the firefighter was responding and maintaining a high intensity exercise in a safe manner, midway through each workout, target heart rate, ratings of perceived exertion, and blood pressure were verified for any needed adjustment in intensity but not recorded for analysis, and the workout continued for at least 30 min, not exceeding 40 min. Each exercise prescription was prepared by students under the supervision of their professors. Fitness training sessions were, Monday to Friday 9 a.m. to 5 p.m., and dependent on set schedule shared with the fire department. Firefighters’ schedules were flexible and varied depending on their emergency calls. Only one session was interrupted by an emergency call and the firefighter returned and started the workout from the beginning.
2.4. Statistical Analysis
The statistical package software (IBM SPSS v.24) was used for data analysis. Linear interpolation occurred to replace missing data (<2%) without altering power. First, normality of data was assessed using the Shapiro-Wilk test. Variables of resting HR, diastolic BP, VO2max, BMI, %BF, fat free mass, HGS, agility, flexibility, and push-up performance were found to be parametric (p > 0.05). The variables of resting SBP, WHR, fat mass, leg-press performance. and readiness for change were found to be non-parametric (p < 0.05). Log base 10 transformation of the non-parametric variables resulted in normality (p > 0.05) of all variables except resting SBP, leg-press performance, and readiness for change. Differences between pre- and post-measurements for parametric variables were firstly compared with dependent t-tests. The analysis of covariance (ANCOVA) was employed to control for any effect of frequency of participation: low consisted of an average of one weekly session, moderate consisted of a range of one to two weekly sessions, high consisted of a range of two to three weekly sessions and semester participated (fall or spring or both of the same academic year) on pre-post change. This was done by including participation and semester participated as fixed factors with pre-assessment as a covariate, and post-assessment as the dependent variable. For variables that did not achieve normality, the Wilcoxon signed-rank test was used to analyze pre- and post-change differences. Statistical significance was set at 0.05. For all ANCOVAs, the homogeneity of variance was met. The effect sizes were analyzed using partial eta squared (ηp2) to describe small (ηp2 = 0.01), medium (ηp2 = 0.06), and large (ηp2 = 0.14) effects.
3. Results
3.1. Participants’ Characteristics
The characteristics of the 34 participants can be found in Table 1. A total of 69% were overweight (BMI ≥ 25) or obese (BMI ≥ 30), and only one participant had a normal BP (BP < 120/80).

Table 1.
Baseline descriptive characteristics of the participants.
3.2. Intervention Results
3.2.1. Cardiorespiratory Endurance
Table 2, Table 3 and Table 4 contain data describing the results of the 10-week HIFT intervention. Using dependent t tests, significant changes were observed for the adjusted VO2max (t(33) = 2.075, p = 0.046, d = 0.36). Using ANCOVAs after controlling for frequency of participation and semester participated, there was a significant improvement in resting DBP (F(1, 25) = 6.163, p =.02, ηp2 = 0.20) and resting HR (F(1, 25) = 14.427, p = 0.001, ηp2 = 0.37) with large effects. Bonferroni’s post-hoc comparisons did not reveal any significant changes between groups; however, the new recruits at the station in the spring had a significantly lower resting HR compared to the fall cohort while accounting for the 10 returning firefighters from fall to spring. The age-adjusted VO2max was significantly different even after controlling for the pre-assessment measures of resting HR, SBP and SDP, the semester they participated in, the frequency of participation, and their interaction (F(1, 22) = 13.017, p = 0.002, ηp2 = 0.37). Bonferroni’s post-hoc comparisons did not reveal any significant changes between groups. A Wilcoxon signed-ranked test did not indicate a significant change in resting SBP (pre-Mdn = 128 ± 14 mmHg and post-Mdn = 126 ± 10 mmHg; Z = 1.77, p = 0.076, r = 0.30).

Table 2.
Cardiorespiratory measurements (mean ± SD) for the HIFT experiential learning initiative (HIFT-ELI).

Table 3.
Raw mean ± SD values for body composition parameters for the HIFT-ELI.

Table 4.
Raw mean ± SD values for muscular strength and endurance, agility, and flexibility measurement for the HIFT-ELI.
3.2.2. Body Composition
Dependent t-tests showed no significant changes in the body composition parameters. After controlling for participation, the semester participated in, and their interaction, there were statistically significant improvements in BMI (F(1, 25) = 2079.873, p < 0.001, ηp2 = 0.99), %BF (F(1, 25) = 145.286, p < 0.001, ηp2 = 0.85), Fat Mass (F(1, 25) = 377.764, p < 0.001, ηp2 = 0.94), and Fat-Free Mass (F(1, 25) = 750.246, p < 0.001, ηp2 = 0.97). Fat Mass was significantly greater in the frequency groups that met at least twice a week compared to the one meeting only once a week even after controlling for pre-assessment measures of %BF, WHR, BMI, Fat Mass, and Fat-Free Mass. BMI was significantly lower in the low frequency group compared to the two other frequency groups (F(1, 25) = 5.737. p = 0.009, ηp2 = 0.32) even after controlling for pre-assessment measures of %BF, WHR, BMI, Fat Mass, and Fat Free Mass. Bonferroni post-hoc comparisons did not show any other significant changes. In total, 23 out of 34 participants demonstrated increases in their BMI; 26 out of 34 participants increased their Fat-Free Mass, and 23 out of 34 participants experienced a decrease in Fat Mass.
3.2.3. Agility, Flexibility and Muscular Strength and Endurance
Using dependent t-tests, improvements were observed in measures of agility (t(33) = 4.062, p < 0.001, d = 0.70) and the push-up test (t(33) = −2.822, p = 0.008, d = 0.48). Using ANCOVA, after controlling for participation, the semester participated in, and interaction, there were significant improvements in hand strength (F(1, 25) = 42.755, p < 0.001, ηp2 = 0.63), agility (F(1, 25) = 30.248, p < 0.001, ηp2 = 0.55), flexibility (F(1, 25) = 187.409, p < 0.001, ηp2 = 0.88), and push-up performance (F(1, 25) = 168.138, p < 0.001, ηp2 = 0.87). However, Bonferroni’s post-hoc comparisons did not reveal any differences. Log 10 transformation did not yield normality for the estimated 1RM leg press; hence, the Wilcoxon signed-rank sum test was used. The weight lifted increased significantly post-training for the leg press (pre-Mdn = 227 ± 48 lbs., post-Mdn = 244 ± 43 lbs.; Z = 2.5, p = 0.012, r = 0.43). Out of the cohort of participants, 85% increased their leg strength.
3.3. Semi-Quantitative Report of Intervention
No injury was reported and the feasibility was excellent. At the end of the study, the chief of fire concluded that his workforce had taken less sick leave and his workers’ compensation during the time of the initiative had been significantly lowered, positively impacting the city budget. Additionally, the Wilcoxon signed-rank sum test was used to estimate the readiness for change (pre-Mdn = 3.00 ± 0.79 and post-Mdn = 4.00 ± 0.73; Z = 3.8, p < 0.001, r = 0.65). There was a significant change from preparation to action with the initiative.
4. Discussion
The purpose of the current study was to examine the feasibility of the experiential learning initiative and the changes in health and fitness parameters of a sample of professional firefighters subjected to a 10-week HIFT program. The training program was administered by kinesiology students who used KSAs gained from three undergraduate courses from an accredited program in exercise sciences [21,22]. We hypothesized that the integration of service learning to administer HIFT to hypertensive and overweight firefighters would improve cardiorespiratory fitness, body composition, and muscular strength and endurance post-intervention relative to a baseline (pre-training). This study examined the benefits of HIFT by improving on the limitations seen in several studies [20,40]—in particular, where the authors stated that they were working with high-intensity training but did not report consistently checking that the participants were actually at high intensity during the vigorous exercise.
It is important to note that, prior to participation in the HIFT, the current group of professional firefighters demonstrated health and fitness levels significantly below that deemed essential for firefighting tasks [41]. Firefighting requires optimal balance between workloads and physical and cognitive capabilities. The National Fire Protection Association [18] documents that physical and cognitive capabilities are related to job performance, including performance related to firefighting tasks (e.g., lifting, carrying, and pulling objects, working with heavy objects in front of them, climbing and hoisting tasks). The physical and cognitive capabilities of firefighting can be determined by factors such as age, anthropometric parameters (stature, %BF, fat-free mass, and BMI), and muscle capacity (total strength, total hand-grip strength, push-up scores, sit-up scores, and endurance) [42]. For example, research has reported strong positive associations between high levels of muscle and endurance strengths, particularly of the trunk and lower limbs with specific firefighting tasks [43,44,45]. These studies also demonstrated a correlation between an increase in fat mass and BMI with time to complete a simulated firefighting task. Overweight and obesity are limiting factors that not only affect firefighting tasks but also the health of firefighters. These are risk factors for cardiovascular health, the leading cause of death among North American firefighters, accounting for 45–47% of firefighter deaths from 1994 to 2012 [46,47]. A recent meta-analysis on exercise interventions in firefighters found significant improvements in %BF, aerobic capacity, endurance, strength, and power [48]. Specifically, resistance exercise training (RET) in the selected studies for this meta-analysis improved the %BF, aerobic capacity, endurance, strength, and power, while aerobic exercise training (AET) improved aerobic capacity only, and AET + RET improved aerobic capacity and endurance. These positive outcomes for firefighters’ health and fitness were associated with superior job performance and a reduced risk of injury and cardiovascular disease. At baseline, 71% of the firefighters were overweight or obese and 97% experienced elevated blood pressure or were hypertensive. Additionally, the majority of the participants (80%) were below the VO2max standard of 45 mL/kg/min recommended for carrying out demanding firefighting operations. These findings are not surprising, as several previous investigations found that the prevalence rates of overweight/obesity are very high in firefighters [49]. In addition, cardiac events, for which hypertension is a risk factor, have been shown to be the leading cause deaths among US firefighters [46,47]. These findings are, however, unprecedented, as it is mandatory for all firefighter recruits to complete initial training focusing on health (e.g., body composition) and fitness (e.g., cardiorespiratory fitness) improvement in line with the demands of firefighting [50]. Therefore, this study demonstrated that once this sample of firefighters left the firefighting academy, their health and fitness declined. It is important to note that this cohort of firefighters were professionals hired by a city management in a state where there are no mandatory annual fitness testing requirements.
As such in this study, SL with underrepresented kinesiology students was based on a HIFT intervention aimed at improving health and fitness for professional deconditioned firefighters. Regarding the effect of HIFT on aerobic fitness, there is little agreement in previous research. For example, in Brisebois, Rigby, and Nichols [40], an 8-week HIFT program resulted in a 5.5% improvement in VO2max and 6.8% improvement in resting HR in physically inactive adults. Gnacinski et al. [50] similarly reported an overall 16.5% and 12.8% gain in VO2max and resting HR in firefighter recruits. Our intervention did not significantly improve the resting SBP and VO2max. However, there were significant improvements in the resting DBP and resting HR in line with the ones observed by Brisebois, Rigby, and Nichols [40} and Menz et al. [51]. The participants in this study also did not experience improvements in VO2max and resting SBP, in line with the Crawford et al. study in inactive adults [52]. The disagreements between these studies could be due to differences in the implementation of the HIFT program, considering that VO2max can be activity-specific. For instance, the HIFT program used in Brisebois, Rigby, and Nichols [40] seems to be more intense and had the participants perform more running protocols relative to the Crawford et al. study [52]. One study by Menz et al. [51] found that functional and running high-intensity training affected VO2max to a similar extent despite the lower improvement in HR in the functional program. Regarding BP, we found a 3.5% decrease in DBP. This finding is in agreement with several studies (e.g., Brisebois, Rigby, and Nichols [40]) that found that the HIFT program significantly decreased DBP but not SBP. In this study, the current baseline resting SBPs (mean = 131.2 mmHg) and DBPs (mean = 82.6 mmHg) were significantly higher than that the ones reported in Brisebois, Rigby, and Nichols [40] study (mean SBP = 112.0 mean resting DBP = 71.7 mmHg). As the majority of our participants were hypertensive, our study confirmed findings from a previous study by Mahjoub et al. [53] in hypertensive men. Such vigorous exercise programs can help to reduce blood pressure.
The results of the study indicated that there were improvements in the body composition parameters of %BF (−1.5%), fat mass (−0.5%), and fat free mass (+0.9%) but not in the parameters of WHR (+1%) and BMI, which increased (+0.7%). This increase in BMI may be due to the significant increase in fat-free mass concurrent to the significant decrease in fat mass after the training program. Using a study of inactive adults, Brisebois, Rigby, and Nichols [40] found similar improvements in %BF (−2.4%), primarily due to increases in free-fat mass (2.2%) in a sample of inactive adults. Heinrich et al. [54], in a clinical population, also found improvements in the body composition parameters of %BF (−15.3%), fat mass (−15.0%), and fat-free mass (+7.5%). These magnitudes of improvements in raw mean were higher than those seen in the current study. This may be due to the frequency of participation, which is explained in changes between pre- and post-measurement. Some studies also found no significant changes in body composition variables after HIFT training [55]. These differences may be due to differences in body composition assessment methods, such as the use of the low-cost caliper method in the current study. This is a clear limitation compared to the more expensive method of the dual-energy X-ray absorptiometry scan used in the Heinrich et al. [54] and Brisebois, Rigby, and Nichols [40] studies. However, the purpose of our study was to limit the cost to the fire department, and as such all measurements were conducted in the field instead of inside a laboratory.
In line with the desired training change, our study found significant improvements in the health and fitness parameters in professional hypertensive deconditioned firefighters. Specifically, significant improvements in lower body muscular strength (mean percent change: estimated 1 RM leg press (5.7%) but not HGS (mean percent change: −0.3%) were observed. There were also significant improvements in muscle endurance (mean percent change: push-up 8%) and agility (mean percent change −7.1%), but not flexibility. The literature is equivocal regarding the effect of the HIFT program on muscle strength and endurance. The Brisebois study [40] found similar increases in leg press, but to a greater extent (+18%). The same author found improvements in flexibility which we could not replicate. However, the push-up improvement is different to the result reported in Menz et al. [51], where no changes were observed with the HIFT training; however, their training was over a four-week period instead of eight weeks.
Fire service proponents advocating the benefits of improved health and physical fitness can reduce firefighter disability, which in turn saves money while improving community safety and fire protection. Firefighting is one of the most physically demanding occupations, given the wide range of hazards. Acute and chronic exposures to hazardous situations can induce life-threating injuries, illnesses, and fatalities. Cardiovascular disease is the foremost cause of death for firefighters while on-duty (45% of on-duty fatalities) and a major cause of morbidity [56]. As body mass index increases from normal weight, the yearly costs to fire departments increase per firefighter at a rate of $74 (overweight), $254 (Class I obese), and $1683 (Class II and II obese). Further, overweight to obese firefighters missed 2.7–5.0 times the number of days missed due to injury compared to normal-weight firefighters [49]. Previous estimates for overweight and obesity (BMI ≥ 25.0 kg/m2) rates have ranged from 73% to 88% in career firefighters [15]. Following an introduction of a wellness initiative at many fire departments in Oregon, the average annual increase in incurred medical costs was just 1% compared to a 5% increase for nonparticipating fire departments [57].
Investigations in the future will have to explore the concept of remote testing technology utilizing (live) video training sessions and Bluetooth®-linked devices (for example, EKO® stethoscope and KardiaMobile clinical grade personal electrocardiogram monitor). Online telemedicine systems have demonstrated their efficient ability to diagnose patients remotely. These systems are based on advanced wireless and wearable sensor technologies that have thoroughly enhanced the capacity of remote health monitoring systems to the point of remote cardiovascular fitness testing becoming a viable option [58]. During the current COVID-19 health pandemic, this concept should be further explored with student-centered learning interventions to permit students to be trained on new technologies that will continue to be utilized in the field.
This HIFT experiential learning initiative was feasible, beneficial, and improved the PFFs’ health and physical fitness with limited resources. Specifically, improvements in agility, muscular strength, and readiness for change were observed. Accredited programs in exercise science participating in low-cost initiatives may aid in mitigating public service workers’ compensation and injury rates to better respond to occupational demands.
Author Contributions
Conceptualization, M.P. and T.A.; Data curation, C.D.; Formal analysis, M.P.; Funding acquisition, M.P. and T.A.; Investigation, M.P.; Methodology, M.P.; Project administration, M.P. and C.D.; Supervision, M.P., C.D., D.M. and R.P.; Validation, M.P.; Visualization, X.Z.; Writing —Original draft, M.P., E.C. and T.A.; Writing—Review & editing, C.D., D.M., R.P. and X.Z. All authors have read and agreed to the published version of the manuscript.
Funding
Research was funded by the (confidential city name) City Management, Clayton County, GA, USA.
Institutional Review Board Statement
The study was conducted according to the guidelines of the World Medical Association’s Declaration of Helsinki, and approved by the Institutional Review Board of Clayton State University (protocol #20190205001, approved 02/18/2019, approved continuation 01/31/2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available at the participants’ requests.
Acknowledgments
The authors would like to thank the students and the subjects for their time and participation; the Chief of Fire for his leadership, Antoinette Miller for the PACE training, and the City Management in Clayton County, GA. for their sponsorship.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analysis, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Bennett, G.; Henson, R.K.; Drane, D. Student experiences with service-learning in sport management. J. Exp. Educ. 2003, 26, 61–69. [Google Scholar] [CrossRef]
- Brown, C.; Willett, J.; Goldfine, R.; Goldfine, B. Sport management internships: Recommendations for improving upon experiential learning. J. Hosp. Leis. Sport. Tour. Educ. 2018, 22, 75–81. [Google Scholar] [CrossRef]
- Peters, R.S. Freedom to learn: A view of what education might become. Interchange 1970, 1, 111–114. [Google Scholar] [CrossRef]
- Voukelatou, G. The contribution of experiential learning to the development of cognitive and social skills in secondary education: A case study. Educ. Sci. 2019, 9, 127. [Google Scholar] [CrossRef]
- Eckhaus, E.; Klein, G.; Kantor, J. Experiential learning in management education. Biophys. Manag. Educ. 2017, 15, 42–56. [Google Scholar] [CrossRef]
- Borges, N.J.; Hartung, P.J. Service learning in medical education: Project description and evaluation. Int. J. Teach. Learn. High. Educ. 2007, 19, 1. [Google Scholar]
- De Groot, M.; Alexander, K.; Culp, B.; Keith, N. Experiential learning in kinesiology: A student perspective. Pedagog. Health Promot. 2015, 1, 123–133. [Google Scholar] [CrossRef]
- Reynolds, P. Community engagement: What’s the difference between service learning, community service, and community-based research? J. Phys. Ther. Educ. 2009, 23, 3–9. [Google Scholar] [CrossRef]
- Meaney, K.S.; Bohler, H.R.; Kopf, K.; Hernandez, L.; Scott, L.S. Service-learning and pre-service educators’ cultural competence for teaching: An exploratory study. J. Exp. Educ. 2008, 31, 189–208. [Google Scholar] [CrossRef]
- Hayes, R.A.; Sherlock, L.A.; Leary, M.P. The role of experiential learning on self-efficacy in undergraduate exercise physiology students: A pilot study. Int. J. Res Ex. Phys. 2020, 15, 1–13. [Google Scholar]
- Schutte, K.J.; Wetmore, L. Experiential learning as a catalyst for moral development in cognitive growth. IJBSS 2012, 3, 220–227. [Google Scholar]
- Roper, E.A.; Santiago, J.A. Influence of service-learning on kinesiology students’ attitudes toward P–12 students with disabilities. Adapt. Phys. Activ. Q. 2014, 31, 162–180. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.A.; Lewis, M.C.; Notley, S.R.; Peoples, G.E. A fractionation of the physiological burden of the personal protective equipment worn by firefighters. Eur. J. Appl. Physiol. 2012, 112, 2913–2921. [Google Scholar] [CrossRef] [PubMed]
- Hur, P.; Rosengren, K.S.; Horn, G.P.; Smith, D.L.; Hsiao-Wecksler, E.T. Effect of protective clothing and fatigue on functional balance of firefighters. J. Ergon. 2013, S2, 1–7. [Google Scholar] [CrossRef]
- Poston, W.S.C.; Haddock, C.K.; Jahnke, S.A.; Jitnarin, N.; Tuley, B.C.; Kales, S.N. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J. Occup. Environ. Med. 2011, 53. [Google Scholar] [CrossRef]
- Donovan, R.; Nelson, T.; Peel, J.; Lipsey, T.; Voyles, W.; Israel, R.G. Cardiorespiratory fitness and the metabolic syndrome in firefighters. Occup. Med. 2009, 59, 487–492. [Google Scholar] [CrossRef]
- Durand, G.; Tsismenakis, A.J.; Jahnke, S.A.; Baur, D.M.; Christophi, C.A.; Kales, S.N. Firefighters’ physical activity: Relation to fitness and cardiovascular disease risk. Med. Sci. Sport. Exer. 2011, 43, 1752–1759. [Google Scholar] [CrossRef]
- National Fire Protection Association. Standard on Health-Related Fitness Programs for Fire Department Members. Available online: https://www.nfpa.org/codes-and-standards/all-codes-and-standards/list-of-codes-and-standards/detail?code=1582 (accessed on 30 October 2020).
- Feito, Y.; Heinrich, K.M.; Butcher, S.J.; Poston, W.S.C. High-intensity functional training (HIFT): Definition and research implications for improved fitness. Sports 2018, 6, 76. [Google Scholar] [CrossRef]
- Hollerbach, B.S.; Jahnke, S.A.; Poston, W.S.C.; Harms, C.A.; Heinrich, K.M. Examining a novel firefighter exercise training program on simulated fire ground test performance, cardiorespiratory endurance, and strength: A pilot investigation. J. Occup. Med. Toxicol. 2019, 14, 12. [Google Scholar] [CrossRef]
- Committee on Accreditation for the Exercise Sciences. Standards and Guidelines. Available online: http://www.coaes.org (accessed on 30 October 2020).
- Commission on Accreditation of Allied Health Education Programs. Standards and Guidelines for the Accreditation of Educational Programs in Exercise Science. Available online: https://www.caahep.org/documents/file/For-Program-Directors/ES_Standards.pdf (accessed on 29 October 2020).
- Bredin, S.S.; Gledhill, N.; Jamnik, V.K.; Warburton, D.E. PAR-Q+ and ePARmed-X+: New risk stratification and physical activity clearance strategy for physicians and patients alike. Can. Fam. Physician 2013, 59, 273–277. [Google Scholar]
- American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2017. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A.G. Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, B.J. Fitness and Work Capacity; Report, No.FS-315; Forest Service U.S. Department of Agriculture: Washington, DC, USA, 1977.
- Sharkey, B.J. Physiology of Fitness: Prescribing Exercise for Fitness Weight Control and Health; Human Kinetics Publishers: Champaign, IL, USA, 1979. [Google Scholar]
- Jackson, A.S.; Pollock, M.L. Generalized equations for predicting body density of men. Brit. J. Nutr. 1978, 40, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.S.; Pollock, M.L.; Ward, A.N.N. Generalized equations for predicting body density of women. Med. Sci. Sports Exerc. 1980, 12, 175–182. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2011; Available online: https://www.who.int/publications/i/item/9789241501491 (accessed on 9 December 2020).
- Pi-Sunyer, F.X.; Becker, D.M.; Bouchard, C.; Carleton, R.A.; Colditz, G.A.; Dietz, W.H.; Foreyt, J.P.; Garrison, R.J.; Grundy, S.M.; Hansen, B.C.; et al. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: Executive summary. Am. J. Clin. Nutr. 1998, 68, 899–917. [Google Scholar] [CrossRef]
- Poirier, P.; Giles, T.D.; Bray, G.A.; Hong, Y.; Stern, J.S.; Pi-Sunyer, F.X.; Eckel, R.H. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: An update of the 1997 American Heart Association Scientific statement on obesity and heart disease from the obesity committee of the council on nutrition, physical activity, and metabolism. Circulation 2006, 113, 898–918. [Google Scholar] [CrossRef] [PubMed]
- Semenick, D. Tests and measurements: The t-test. Strength Cond. J. 1990, 12, 36–37. [Google Scholar] [CrossRef]
- Adams, G.; Beam, W. Exercise Physiology Laboratory Manual; McGraw-Hill: New York, NY, USA, 2008. [Google Scholar]
- Bimali, I.; Opsana, R.; Jeebika, S. Normative reference values on handgrip strength among healthy adults of Dhulikhel, Nepal: A cross-sectional study. J. Family Med. Prim. Care 2020, 9, 310–314. [Google Scholar] [CrossRef]
- Wang, Y.-C.; Bohannon, R.W.; Li, X.; Sindhu, B.; Kapellusch, J. Hand-grip strength: Normative reference values and equations for individuals 18 to 85 Years of age residing in the United States. J. Orthop. Sports Phys. Ther. 2018, 48, 685–693. [Google Scholar] [CrossRef]
- Brzycki, M. Strength testing—Predicting a one-rep max from reps to fatigue. JOPERD 1993, 64, 88–90. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Marcus, B.H. The transtheoretical model: Applications to exercise. In Advances in Exercise Adherence; Dishman, R.K., Ed.; Human Kinetics Publishers: Champaign, IL, USA, 1994; pp. 161–180. [Google Scholar]
- Marcus, B.H.; Lewis, B.A. Physical Activity and the Stages of Motivational Readiness for Change Model. President’s Council on Physical Fitness and Sports. 2003. Available online: https://files.eric.ed.gov/fulltext/ED474896.pdf (accessed on 30 October 2020).
- Brisebois, M.F.; Rigby, B.R.; Nichols, D.L. Physiological and fitness adaptations after eight weeks of high-intensity functional training in physically inactive adults. Sports 2018, 6, 146. [Google Scholar] [CrossRef]
- Gledhill, N.; Jamnik, V. Characterization of the physical demands of firefighting. Can. J. Sport Sci. 1992, 17, 207–213. [Google Scholar] [PubMed]
- Henderson, N.D.; Berry, M.W.; Matic, T. Field measures of strength and fitness predict firefighter performance on physically demanding tasks. Pers. Psychol. 2007, 60, 431–473. [Google Scholar] [CrossRef]
- Michaelides, M.A.; Parpa, K.M.; Henry, L.J.; Thompson, G.B.; Brown, B.S. Assessment of physical fitness aspects and their relationship to firefighters’ job abilities. J. Strength Cond. Res. 2011, 25, 956–965. [Google Scholar] [CrossRef] [PubMed]
- Rhea, M.R.; Alvar, B.A.; Gray, R. Physical fitness and job performance of firefighters. J. Strength Cond. Res. 2004, 18, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Stone, B.L.; Alvar, B.A.; Orr, R.M.; Lockie, R.G.; Johnson, Q.R.; Goatcher, J.; Dawes, J.J. Impact of an 11-Week Strength and Conditioning Program on Firefighter Trainee Fitness. Sustainability 2020, 12, 6541. [Google Scholar] [CrossRef]
- Korre, M.; Sotos-Prieto, M.; Kales, S.N. Survival Mediterranean style: Lifestyle changes to improve the health of the US fire service. Front. Public Health 2017, 5, 331. [Google Scholar] [CrossRef]
- Sen, S.; Palmieri, T.; Greenhalgh, D. Cardiac fatalities in firefighters: An analysis of the U.S. fire administration database. J. Burn Care Res. 2016, 37, 191–195. [Google Scholar] [CrossRef]
- Andrews, K.L.; Gallagher, S.; Herring, M.P. The effects of exercise interventions on health and fitness of firefighters: A meta-analysis. Scand. J. Med. Sci. Sports 2019, 29, 780–790. [Google Scholar] [CrossRef]
- Poston, W.S.; Jitnarin, N.; Haddock, C.K.; Jahnke, S.A.; Tuley, B.C. Obesity and injury-related absenteeism in a population-based firefighter cohort. Obesity 2011, 19, 2076–2081. [Google Scholar] [CrossRef]
- Gnacinski, S.L.; Ebersole, K.T.; Cornell, D.J.; Mims, J.; Zamzow, A.; Meyer, B.B. Firefighters’ cardiovascular health and fitness: An observation of adaptations that occur during firefighter training academies. Work 2016, 54, 43–50. [Google Scholar] [CrossRef]
- Menz, V.; Marterer, N.; Amin, S.B.; Faulhaber, M.; Hansen, A.B.; Lawley, J.S. Functional vs. running low-volume high-intensity interval training: Effects on VO2max and muscular endurance. J. Sports Sci. Med. 2019, 18, 497–504. [Google Scholar] [PubMed]
- Crawford, D.A.; Drake, N.B.; Carper, M.J.; DeBlauw, J.; Heinrich, K.M. Are changes in physical work capacity induced by high-intensity functional training related to changes in associated physiologic measures? Sports 2018, 6, 26. [Google Scholar] [CrossRef] [PubMed]
- Mahjoub, H.; Le Blanc, O.; Paquette, M.; Imhoff, S.; Labrecque, L.; Drapeau, A.; Brassard, P. Cardiac remodeling after six weeks of high-intensity interval training to exhaustion in endurance-trained men. Am. J. Physiol. Heart Circ. Physiol. 2019, 317, H685–H694. [Google Scholar] [CrossRef]
- Heinrich, K.M.; Becker, C.; Carlisle, T.; Gilmore, K.; Hauser, J.; Frye, J.; Harms, C.A. High-intensity functional training improves functional movement and body composition among cancer survivors: A pilot study. Eur. J. Cancer Care 2015, 24, 812–817. [Google Scholar] [CrossRef] [PubMed]
- Feito, Y.; Patel, P.; Sal Redondo, A.; Heinrich, K.M. Effects of eight weeks of high intensity functional training on glucose control and body composition among overweight and obese adults. Sports 2019, 7, 51. [Google Scholar] [CrossRef] [PubMed]
- Soteriades, E.S.; Smith, D.L.; Tsismenakis, A.J.; Baur, D.M.; Kales, S.N. Cardiovascular disease in US firefighters: A systematic review. Cardiol. Rev. 2011, 19, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Kuehl, K.S.; Elliot, D.L.; Goldberg, L.; Moe, E.L.; Perrier, E.; Smith, J. Economic benefit of the PHLAME wellness programme on firefighter injury. Occup. Med. 2013, 63, 203–209. [Google Scholar] [CrossRef]
- Kakria, P.; Tripathi, N.K.; Kitipawang, P. A real-time health monitoring system for remote cardiac patients using smartphone and wearable sensors. Int. J. Telemed. Appl. 2015, 2015, 373474. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).