Fit for Fire: A 10-Week Low-Cost HIFT Experiential Learning Initiative between Underrepresented Kinesiology Undergraduates and Hypertensive Deconditioned Firefighters Improves Their Health and Fitness
Abstract
1. Introduction
2. Materials and Methods
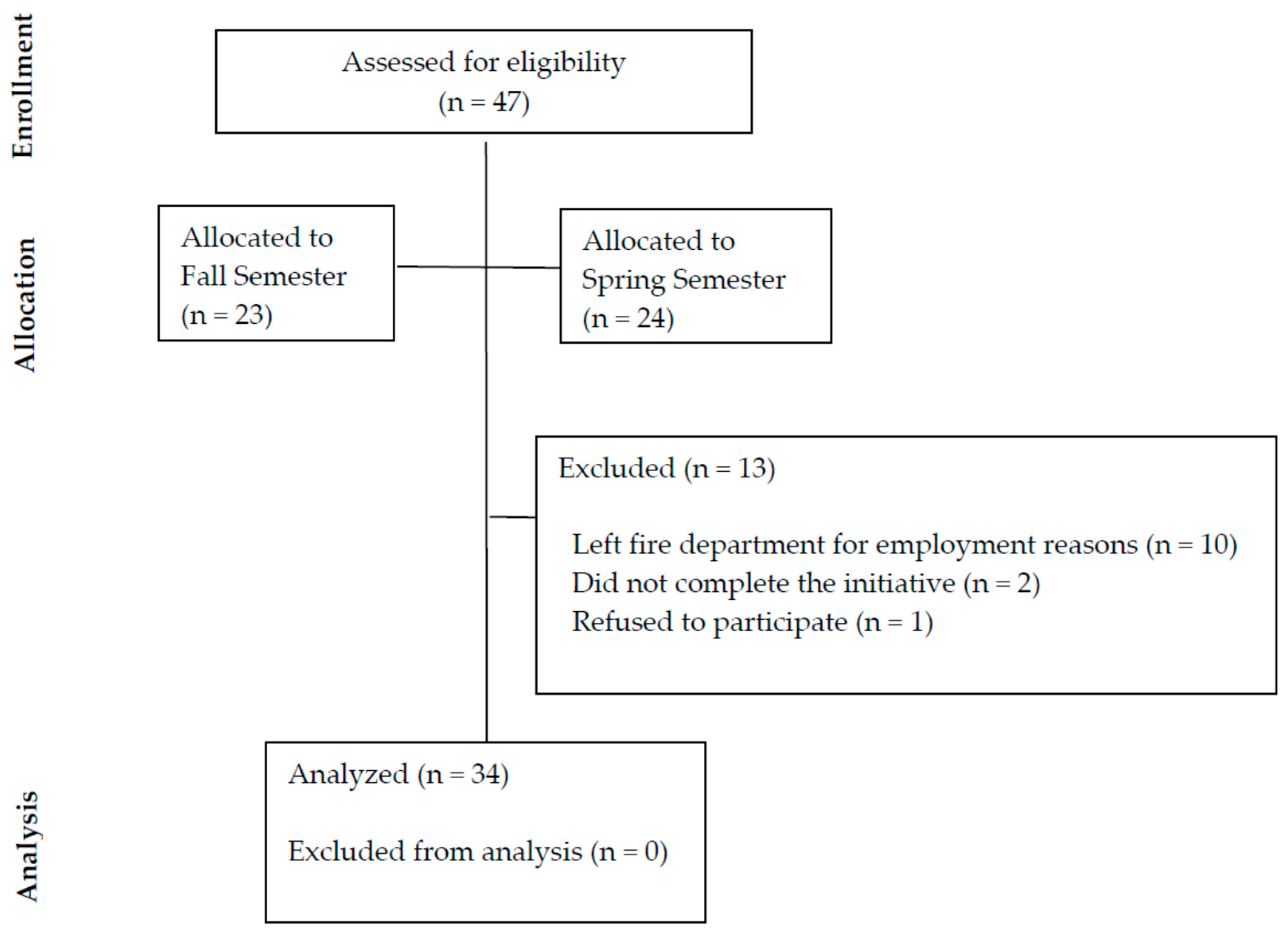
2.1. Participants
2.2. Procedures
2.3. Measures
2.3.1. Cardiovascular Assessments
2.3.2. Body Composition
2.3.3. Agility Test
2.3.4. Flexibility Test
2.3.5. Muscular Strength Test
2.3.6. Muscular Endurance Tests
2.3.7. Physical Activity Readiness for Change
2.3.8. Intervention
2.4. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Intervention Results
3.2.1. Cardiorespiratory Endurance
3.2.2. Body Composition
3.2.3. Agility, Flexibility and Muscular Strength and Endurance
3.3. Semi-Quantitative Report of Intervention
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bennett, G.; Henson, R.K.; Drane, D. Student experiences with service-learning in sport management. J. Exp. Educ. 2003, 26, 61–69. [Google Scholar] [CrossRef]
- Brown, C.; Willett, J.; Goldfine, R.; Goldfine, B. Sport management internships: Recommendations for improving upon experiential learning. J. Hosp. Leis. Sport. Tour. Educ. 2018, 22, 75–81. [Google Scholar] [CrossRef]
- Peters, R.S. Freedom to learn: A view of what education might become. Interchange 1970, 1, 111–114. [Google Scholar] [CrossRef]
- Voukelatou, G. The contribution of experiential learning to the development of cognitive and social skills in secondary education: A case study. Educ. Sci. 2019, 9, 127. [Google Scholar] [CrossRef]
- Eckhaus, E.; Klein, G.; Kantor, J. Experiential learning in management education. Biophys. Manag. Educ. 2017, 15, 42–56. [Google Scholar] [CrossRef]
- Borges, N.J.; Hartung, P.J. Service learning in medical education: Project description and evaluation. Int. J. Teach. Learn. High. Educ. 2007, 19, 1. [Google Scholar]
- De Groot, M.; Alexander, K.; Culp, B.; Keith, N. Experiential learning in kinesiology: A student perspective. Pedagog. Health Promot. 2015, 1, 123–133. [Google Scholar] [CrossRef]
- Reynolds, P. Community engagement: What’s the difference between service learning, community service, and community-based research? J. Phys. Ther. Educ. 2009, 23, 3–9. [Google Scholar] [CrossRef]
- Meaney, K.S.; Bohler, H.R.; Kopf, K.; Hernandez, L.; Scott, L.S. Service-learning and pre-service educators’ cultural competence for teaching: An exploratory study. J. Exp. Educ. 2008, 31, 189–208. [Google Scholar] [CrossRef]
- Hayes, R.A.; Sherlock, L.A.; Leary, M.P. The role of experiential learning on self-efficacy in undergraduate exercise physiology students: A pilot study. Int. J. Res Ex. Phys. 2020, 15, 1–13. [Google Scholar]
- Schutte, K.J.; Wetmore, L. Experiential learning as a catalyst for moral development in cognitive growth. IJBSS 2012, 3, 220–227. [Google Scholar]
- Roper, E.A.; Santiago, J.A. Influence of service-learning on kinesiology students’ attitudes toward P–12 students with disabilities. Adapt. Phys. Activ. Q. 2014, 31, 162–180. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.A.; Lewis, M.C.; Notley, S.R.; Peoples, G.E. A fractionation of the physiological burden of the personal protective equipment worn by firefighters. Eur. J. Appl. Physiol. 2012, 112, 2913–2921. [Google Scholar] [CrossRef] [PubMed]
- Hur, P.; Rosengren, K.S.; Horn, G.P.; Smith, D.L.; Hsiao-Wecksler, E.T. Effect of protective clothing and fatigue on functional balance of firefighters. J. Ergon. 2013, S2, 1–7. [Google Scholar] [CrossRef]
- Poston, W.S.C.; Haddock, C.K.; Jahnke, S.A.; Jitnarin, N.; Tuley, B.C.; Kales, S.N. The prevalence of overweight, obesity, and substandard fitness in a population-based firefighter cohort. J. Occup. Environ. Med. 2011, 53. [Google Scholar] [CrossRef]
- Donovan, R.; Nelson, T.; Peel, J.; Lipsey, T.; Voyles, W.; Israel, R.G. Cardiorespiratory fitness and the metabolic syndrome in firefighters. Occup. Med. 2009, 59, 487–492. [Google Scholar] [CrossRef]
- Durand, G.; Tsismenakis, A.J.; Jahnke, S.A.; Baur, D.M.; Christophi, C.A.; Kales, S.N. Firefighters’ physical activity: Relation to fitness and cardiovascular disease risk. Med. Sci. Sport. Exer. 2011, 43, 1752–1759. [Google Scholar] [CrossRef]
- National Fire Protection Association. Standard on Health-Related Fitness Programs for Fire Department Members. Available online: https://www.nfpa.org/codes-and-standards/all-codes-and-standards/list-of-codes-and-standards/detail?code=1582 (accessed on 30 October 2020).
- Feito, Y.; Heinrich, K.M.; Butcher, S.J.; Poston, W.S.C. High-intensity functional training (HIFT): Definition and research implications for improved fitness. Sports 2018, 6, 76. [Google Scholar] [CrossRef]
- Hollerbach, B.S.; Jahnke, S.A.; Poston, W.S.C.; Harms, C.A.; Heinrich, K.M. Examining a novel firefighter exercise training program on simulated fire ground test performance, cardiorespiratory endurance, and strength: A pilot investigation. J. Occup. Med. Toxicol. 2019, 14, 12. [Google Scholar] [CrossRef]
- Committee on Accreditation for the Exercise Sciences. Standards and Guidelines. Available online: http://www.coaes.org (accessed on 30 October 2020).
- Commission on Accreditation of Allied Health Education Programs. Standards and Guidelines for the Accreditation of Educational Programs in Exercise Science. Available online: https://www.caahep.org/documents/file/For-Program-Directors/ES_Standards.pdf (accessed on 29 October 2020).
- Bredin, S.S.; Gledhill, N.; Jamnik, V.K.; Warburton, D.E. PAR-Q+ and ePARmed-X+: New risk stratification and physical activity clearance strategy for physicians and patients alike. Can. Fam. Physician 2013, 59, 273–277. [Google Scholar]
- American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; Lippincott Williams and Wilkins: Philadelphia, PA, USA, 2017. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A.G. Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Sharkey, B.J. Fitness and Work Capacity; Report, No.FS-315; Forest Service U.S. Department of Agriculture: Washington, DC, USA, 1977.
- Sharkey, B.J. Physiology of Fitness: Prescribing Exercise for Fitness Weight Control and Health; Human Kinetics Publishers: Champaign, IL, USA, 1979. [Google Scholar]
- Jackson, A.S.; Pollock, M.L. Generalized equations for predicting body density of men. Brit. J. Nutr. 1978, 40, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.S.; Pollock, M.L.; Ward, A.N.N. Generalized equations for predicting body density of women. Med. Sci. Sports Exerc. 1980, 12, 175–182. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2011; Available online: https://www.who.int/publications/i/item/9789241501491 (accessed on 9 December 2020).
- Pi-Sunyer, F.X.; Becker, D.M.; Bouchard, C.; Carleton, R.A.; Colditz, G.A.; Dietz, W.H.; Foreyt, J.P.; Garrison, R.J.; Grundy, S.M.; Hansen, B.C.; et al. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: Executive summary. Am. J. Clin. Nutr. 1998, 68, 899–917. [Google Scholar] [CrossRef]
- Poirier, P.; Giles, T.D.; Bray, G.A.; Hong, Y.; Stern, J.S.; Pi-Sunyer, F.X.; Eckel, R.H. Obesity and cardiovascular disease: Pathophysiology, evaluation, and effect of weight loss: An update of the 1997 American Heart Association Scientific statement on obesity and heart disease from the obesity committee of the council on nutrition, physical activity, and metabolism. Circulation 2006, 113, 898–918. [Google Scholar] [CrossRef] [PubMed]
- Semenick, D. Tests and measurements: The t-test. Strength Cond. J. 1990, 12, 36–37. [Google Scholar] [CrossRef]
- Adams, G.; Beam, W. Exercise Physiology Laboratory Manual; McGraw-Hill: New York, NY, USA, 2008. [Google Scholar]
- Bimali, I.; Opsana, R.; Jeebika, S. Normative reference values on handgrip strength among healthy adults of Dhulikhel, Nepal: A cross-sectional study. J. Family Med. Prim. Care 2020, 9, 310–314. [Google Scholar] [CrossRef]
- Wang, Y.-C.; Bohannon, R.W.; Li, X.; Sindhu, B.; Kapellusch, J. Hand-grip strength: Normative reference values and equations for individuals 18 to 85 Years of age residing in the United States. J. Orthop. Sports Phys. Ther. 2018, 48, 685–693. [Google Scholar] [CrossRef]
- Brzycki, M. Strength testing—Predicting a one-rep max from reps to fatigue. JOPERD 1993, 64, 88–90. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Marcus, B.H. The transtheoretical model: Applications to exercise. In Advances in Exercise Adherence; Dishman, R.K., Ed.; Human Kinetics Publishers: Champaign, IL, USA, 1994; pp. 161–180. [Google Scholar]
- Marcus, B.H.; Lewis, B.A. Physical Activity and the Stages of Motivational Readiness for Change Model. President’s Council on Physical Fitness and Sports. 2003. Available online: https://files.eric.ed.gov/fulltext/ED474896.pdf (accessed on 30 October 2020).
- Brisebois, M.F.; Rigby, B.R.; Nichols, D.L. Physiological and fitness adaptations after eight weeks of high-intensity functional training in physically inactive adults. Sports 2018, 6, 146. [Google Scholar] [CrossRef]
- Gledhill, N.; Jamnik, V. Characterization of the physical demands of firefighting. Can. J. Sport Sci. 1992, 17, 207–213. [Google Scholar] [PubMed]
- Henderson, N.D.; Berry, M.W.; Matic, T. Field measures of strength and fitness predict firefighter performance on physically demanding tasks. Pers. Psychol. 2007, 60, 431–473. [Google Scholar] [CrossRef]
- Michaelides, M.A.; Parpa, K.M.; Henry, L.J.; Thompson, G.B.; Brown, B.S. Assessment of physical fitness aspects and their relationship to firefighters’ job abilities. J. Strength Cond. Res. 2011, 25, 956–965. [Google Scholar] [CrossRef] [PubMed]
- Rhea, M.R.; Alvar, B.A.; Gray, R. Physical fitness and job performance of firefighters. J. Strength Cond. Res. 2004, 18, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Stone, B.L.; Alvar, B.A.; Orr, R.M.; Lockie, R.G.; Johnson, Q.R.; Goatcher, J.; Dawes, J.J. Impact of an 11-Week Strength and Conditioning Program on Firefighter Trainee Fitness. Sustainability 2020, 12, 6541. [Google Scholar] [CrossRef]
- Korre, M.; Sotos-Prieto, M.; Kales, S.N. Survival Mediterranean style: Lifestyle changes to improve the health of the US fire service. Front. Public Health 2017, 5, 331. [Google Scholar] [CrossRef]
- Sen, S.; Palmieri, T.; Greenhalgh, D. Cardiac fatalities in firefighters: An analysis of the U.S. fire administration database. J. Burn Care Res. 2016, 37, 191–195. [Google Scholar] [CrossRef]
- Andrews, K.L.; Gallagher, S.; Herring, M.P. The effects of exercise interventions on health and fitness of firefighters: A meta-analysis. Scand. J. Med. Sci. Sports 2019, 29, 780–790. [Google Scholar] [CrossRef]
- Poston, W.S.; Jitnarin, N.; Haddock, C.K.; Jahnke, S.A.; Tuley, B.C. Obesity and injury-related absenteeism in a population-based firefighter cohort. Obesity 2011, 19, 2076–2081. [Google Scholar] [CrossRef]
- Gnacinski, S.L.; Ebersole, K.T.; Cornell, D.J.; Mims, J.; Zamzow, A.; Meyer, B.B. Firefighters’ cardiovascular health and fitness: An observation of adaptations that occur during firefighter training academies. Work 2016, 54, 43–50. [Google Scholar] [CrossRef]
- Menz, V.; Marterer, N.; Amin, S.B.; Faulhaber, M.; Hansen, A.B.; Lawley, J.S. Functional vs. running low-volume high-intensity interval training: Effects on VO2max and muscular endurance. J. Sports Sci. Med. 2019, 18, 497–504. [Google Scholar] [PubMed]
- Crawford, D.A.; Drake, N.B.; Carper, M.J.; DeBlauw, J.; Heinrich, K.M. Are changes in physical work capacity induced by high-intensity functional training related to changes in associated physiologic measures? Sports 2018, 6, 26. [Google Scholar] [CrossRef] [PubMed]
- Mahjoub, H.; Le Blanc, O.; Paquette, M.; Imhoff, S.; Labrecque, L.; Drapeau, A.; Brassard, P. Cardiac remodeling after six weeks of high-intensity interval training to exhaustion in endurance-trained men. Am. J. Physiol. Heart Circ. Physiol. 2019, 317, H685–H694. [Google Scholar] [CrossRef]
- Heinrich, K.M.; Becker, C.; Carlisle, T.; Gilmore, K.; Hauser, J.; Frye, J.; Harms, C.A. High-intensity functional training improves functional movement and body composition among cancer survivors: A pilot study. Eur. J. Cancer Care 2015, 24, 812–817. [Google Scholar] [CrossRef] [PubMed]
- Feito, Y.; Patel, P.; Sal Redondo, A.; Heinrich, K.M. Effects of eight weeks of high intensity functional training on glucose control and body composition among overweight and obese adults. Sports 2019, 7, 51. [Google Scholar] [CrossRef] [PubMed]
- Soteriades, E.S.; Smith, D.L.; Tsismenakis, A.J.; Baur, D.M.; Kales, S.N. Cardiovascular disease in US firefighters: A systematic review. Cardiol. Rev. 2011, 19, 202–215. [Google Scholar] [CrossRef] [PubMed]
- Kuehl, K.S.; Elliot, D.L.; Goldberg, L.; Moe, E.L.; Perrier, E.; Smith, J. Economic benefit of the PHLAME wellness programme on firefighter injury. Occup. Med. 2013, 63, 203–209. [Google Scholar] [CrossRef]
- Kakria, P.; Tripathi, N.K.; Kitipawang, P. A real-time health monitoring system for remote cardiac patients using smartphone and wearable sensors. Int. J. Telemed. Appl. 2015, 2015, 373474. [Google Scholar] [CrossRef]
| Anthropometric | Entire Group (n = 34) | Low (n = 8) | Moderate (n = 8) | High (n = 18) |
|---|---|---|---|---|
| Age (years: Mean ± SD) | 36.8 ± 11.0 | 33.3 ± 9.0 | 35.9 ± 13.2 | 39.2 ± 11.1 |
| Height (cm: Mean ± SD) | 181.7 ± 6.6 | 177.2 ± 6.7 | 182.9 ± 7.3 | 183.2 ± 5.7 |
| Weight (kg: Mean ± SD) | 97.3 ± 21.5 | 90.5 ± 21.7 | 100.7 ± 24.1 | 98.9 ± 20.8 |
| BMI (n: %) | ||||
| Underweight (< 18.5) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Normal (18.5–24.9) | 10 (30) | 2 (6) | 2 (6) | 6 (18) |
| Overweight (25.0–29.9) | 8 (23.5) | 4 (12) | 1 (3) | 3 (8.5) |
| Obesity | 16 (47) | 2 (6) | 5 (14.5) | 9 (26.5) |
| Class I | 11 (32) | 1 (3) | 3 (8.5) | 7 (20.5) |
| Class II | 5 (15) | 1 (3) | 2 (6) | 2 (6) |
| Resting BP (n: %) | Entire Group (n = 34) | Low (n = 8) | Moderate (n = 8) | High (n = 18) |
| Normal (< 120/80) | 1 (3) | 1 (3) | 0 (0) | 0 (0) |
| Elevated (SBP: 120–129 and DBP < 80) | 8 (24) | 1 (3) | 1 (3) | 6 (18) |
| Hypertension I | ||||
| (SBP: 130–139 or DBP: 80–89) | 15 (43.5) | 5 (14.5) | 5 (14.5) | 5 (14.5) |
| Hypertension II | ||||
| (SBP ≥140 or DBP ≥ 90) | 10 (29.5) | 1 (3) | 2 (6) | 7 (20.5) |
| Demographics | Entire Group (n = 34) | Low (n = 8) | Moderate (n = 8) | High (n = 18) |
| Race (n: %) | ||||
| Black | 24 (70.5) | 6 (18) | 4 (11.5) | 14 (41) |
| White | 6 (17.5) | 2 (6) | 3 (8.5) | 1 (3) |
| Hispanic | 2 (6) | 0 (0) | 1 (3) | 1 (3) |
| Others | 2 (6) | 0 (0) | 0 (0) | 2 (6) |
| Gender (n: %) | ||||
| Male | 33 (97) | 7 (20.5) | 8 (23.5) | 18 (53) |
| Female | 1 (3) | 1 (3) | 0 (0) | 0 (0) |
| Marital status (n: %) | ||||
| Single | 16 (47) | 5 (14.5) | 5 (14.5) | 6 (18) |
| Married | 17 (50) | 3 (8.5) | 3 (8.5) | 11 (33) |
| Did not disclose | 1 (3) | 0 (0) | 0 (0) | 1 (3) |
| Education (n: %) | ||||
| High school | 14 (41) | 5 (14.5) | 4 (12) | 5 (14.5) |
| College (2–4 years) | 15 (44) | 3 (8.5) | 3 (8.5) | 9 (27) |
| Graduate school | 2 (6) | 0 (0) | 0 (0) | 2 (6) |
| Degree | 2 (6) | 0 (0) | 1 (3) | 1 (3) |
| Did not disclose | 1 (3) | 0 (0) | 0 (0) | 1 (3) |
| Cardiorespiratory Capacity | Resting HR (bpm) | Resting Systolic BP (mmHg) | Resting Diastolic BP (mmHg) | Adjusted VO2max (mL/kg/min) | |
|---|---|---|---|---|---|
| Pre-HIFT | Cohort | 75.4 ± 8.7 | 131.2 ± 14.4 | 82.6 ± 9.1 | 39.9 ± 5.0 |
| Low | 80.1 ± 6.2 | 130.4 ± 20.0 | 80.8 ± 9.1 | 41.9 ± 4.8 | |
| Moderate | 72.6 ± 5.6 | 135.6 ± 19.2 | 82.0 ± 11.8 | 41.3 ± 6.0 | |
| High | 74.5 ± 10.4 | 129.6 ± 8.6 | 82.7 ± 8.4 | 38.3 ± 4.4 | |
| Post-HIFT | Cohort | 75.4 ± 7.8 * | 127.0 ± 9.7 | 80.0 ± 10.0 * | 38.2 ± 5.1 * |
| Low | 75.1 ± 4.3 | 126.9 ± 13.5 | 81.3 ± 5.2 | 42.1 ± 3.7 | |
| Moderate | 70.0 ± 5.1 | 130.8 ± 12.1 | 81.0 ± 16.4 | 39.6 ± 4.1 | |
| High | 77.8 ± 8.9 | 125.4 ± 6.2 | 79.0 ± 8.6 | 35.9 ± 4.8 | |
| Body Composition | Body Fat (%) | WHR | BMI | Fat Mass (kg) | Fat Free Mass (kg) | |
|---|---|---|---|---|---|---|
| Pre-HIFT | Cohort | 20.3 ± 6.2 | 0.90 ± 0.09 | 29.2 ± 4.9 | 45.5 ± 21.3 | 168.7 ± 29.0 |
| Low | 17.8 ± 6.5 | 0.86 ± 0.05 | 28.6 ± 4.8 | 36.8 ± 21.3 | 162.4 ± 32.1 | |
| Moderate | 20.5 ±8.3 | 0.93 ± 0.07 | 29.9 ± 5.8 | 48.0 ± 25.3 | 173.5 ± 32.4 | |
| High | 21.4 ± 4.9 | 0.90 ± 0.10 | 29.9 ± 4.8 | 48.2 ± 19.7 | 169.3 ± 27.2 | |
| Post-HIFT | Cohort | 20.0 ± 6.4 † | 0.91 ± 0.10 † | 29.4 ±4.8 † | 45.3 ±22.6 † | 170.2 ±27.3 † |
| Low | 16.4 ± 5.3 | 0.89 ± 0.12 | 28.4 ± 4.4 | 33.5 ± 17.4 * | 164.4 ± 31.5 | |
| Moderate | 21.1 ± 8.1 | 0.91 ± 0.08 | 30.4 ± 5.8 | 50.5 ± 27.3 | 174.9 ± 28.7 | |
| High | 21.1 ± 5.8 | 0.91 ± 0.10 | 29.5 ± 4.8 | 48.3 ± 21.8 | 170.7 ± 25.7 | |
| Variable | HSG | T-Test (sec) | Flexibility (cm) | Push-Up (Count) | Leg-Press (lbs.) | |
|---|---|---|---|---|---|---|
| Pre-HIFT | Cohort | 57.8 ± 12.1 | 13.5 ± 2.0 | 16.7 ± 4.2 | 32.2 ± 15.3 | 228.5 ± 48.3 |
| Low | 50.9 ± 13.9 | 12.9 ± 1.8 | 18.0 ± 4.2 | 38.4 ± 24.1 | 230.8 ± 56.0 | |
| Moderate | 59.9 ± 10.4 | 13.6 ± 2.7 | 15.9 ± 3.7 | 31.8 ± 15.3 | 236.6 ±49.3 | |
| High | 59.9 ± 11.3 | 13.7 ± 1.9 | 16.4 ± 4.6 | 29.6 ± 9.8 | 223.8 ± 46.7 | |
| Post-HIFT | Cohort | 57.6 ± 12.2 † | 12.6 ± 1.4 † | 16.6 ± 4.3 † | 35.0 ± 14.9 † | 242.3 ± 42.8 * |
| Low | 53.9 ± 11.8 | 12.2 ± 1.4 | 17.6 ± 4.2 | 43.6 ± 19.7 | 248.6 ± 42.0 | |
| Moderate | 57.9 ± 13.1 | 13.0 ±1.9 | 15.6 ± 4.2 | 31.8 ± 14.9 | 245.4 ± 37.7 | |
| High | 59.1 ± 13.4 | 12.5 ± 1.3 | ± 4.4 | 32.6 ± 11.5 | 238.2 ± 46.9 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poudevigne, M.; Day, C.; Campbell, E.; Mills, D.; Porter, R.; Zornosa, X.; Andre, T. Fit for Fire: A 10-Week Low-Cost HIFT Experiential Learning Initiative between Underrepresented Kinesiology Undergraduates and Hypertensive Deconditioned Firefighters Improves Their Health and Fitness. Educ. Sci. 2021, 11, 33. https://doi.org/10.3390/educsci11010033
Poudevigne M, Day C, Campbell E, Mills D, Porter R, Zornosa X, Andre T. Fit for Fire: A 10-Week Low-Cost HIFT Experiential Learning Initiative between Underrepresented Kinesiology Undergraduates and Hypertensive Deconditioned Firefighters Improves Their Health and Fitness. Education Sciences. 2021; 11(1):33. https://doi.org/10.3390/educsci11010033
Chicago/Turabian StylePoudevigne, Melanie, Christina Day, Eon Campbell, Da’Lynn Mills, Reginald Porter, Ximena Zornosa, and Thomas Andre. 2021. "Fit for Fire: A 10-Week Low-Cost HIFT Experiential Learning Initiative between Underrepresented Kinesiology Undergraduates and Hypertensive Deconditioned Firefighters Improves Their Health and Fitness" Education Sciences 11, no. 1: 33. https://doi.org/10.3390/educsci11010033
APA StylePoudevigne, M., Day, C., Campbell, E., Mills, D., Porter, R., Zornosa, X., & Andre, T. (2021). Fit for Fire: A 10-Week Low-Cost HIFT Experiential Learning Initiative between Underrepresented Kinesiology Undergraduates and Hypertensive Deconditioned Firefighters Improves Their Health and Fitness. Education Sciences, 11(1), 33. https://doi.org/10.3390/educsci11010033





