The Monetary Value of Human Life Losses Associated with COVID-19 in Africa: A Human Capital Approach
Abstract
1. Background
2. Methods
2.1. Study Area and Population
2.2. Study Design
2.3. Conceptual Framework for Valuation of Human Life
2.3.1. Overview
2.3.2. An HCA Model for Estimating the Discounted Monetary Value of Human Life Losses Associated with COVID-19
2.3.3. Data and Data Sources
2.3.4. Data Analysis
2.4. Conceptual Framework for Estimating the Cost of COVID-19 in Africa
2.4.1. Total Indirect Cost Algorithm
2.4.2. Total Direct Cost Algorithm
- CEHPC is a good proxy for the value of all health-related systems inputs used in prevention (including policing of travel bans), diagnosis, contact tracing, isolation/quarantine, management, and rehabilitation of COVID-19 cases;
- CEHPC is efficiently utilized in each country to manage COVID cases, ensuring no wastage in the allocation and use of resources;
- All COVID-19 patients have an equal quantity (and value) of resources spent on them, irrespective of whether the cases are asymptomatic, mild, moderate, severe, or critical.
2.4.3. Total Intangible Cost Algorithm
2.5. Estimation of Potential Savings Assuming a 100% Vaccine Target Population Coverage
2.5.1. Expected Savings in Total Direct Costs Due to COVID-19 Vaccinations
2.5.2. Expected Savings in Total Indirect Costs Due to COVID-19 Vaccination
3. Results
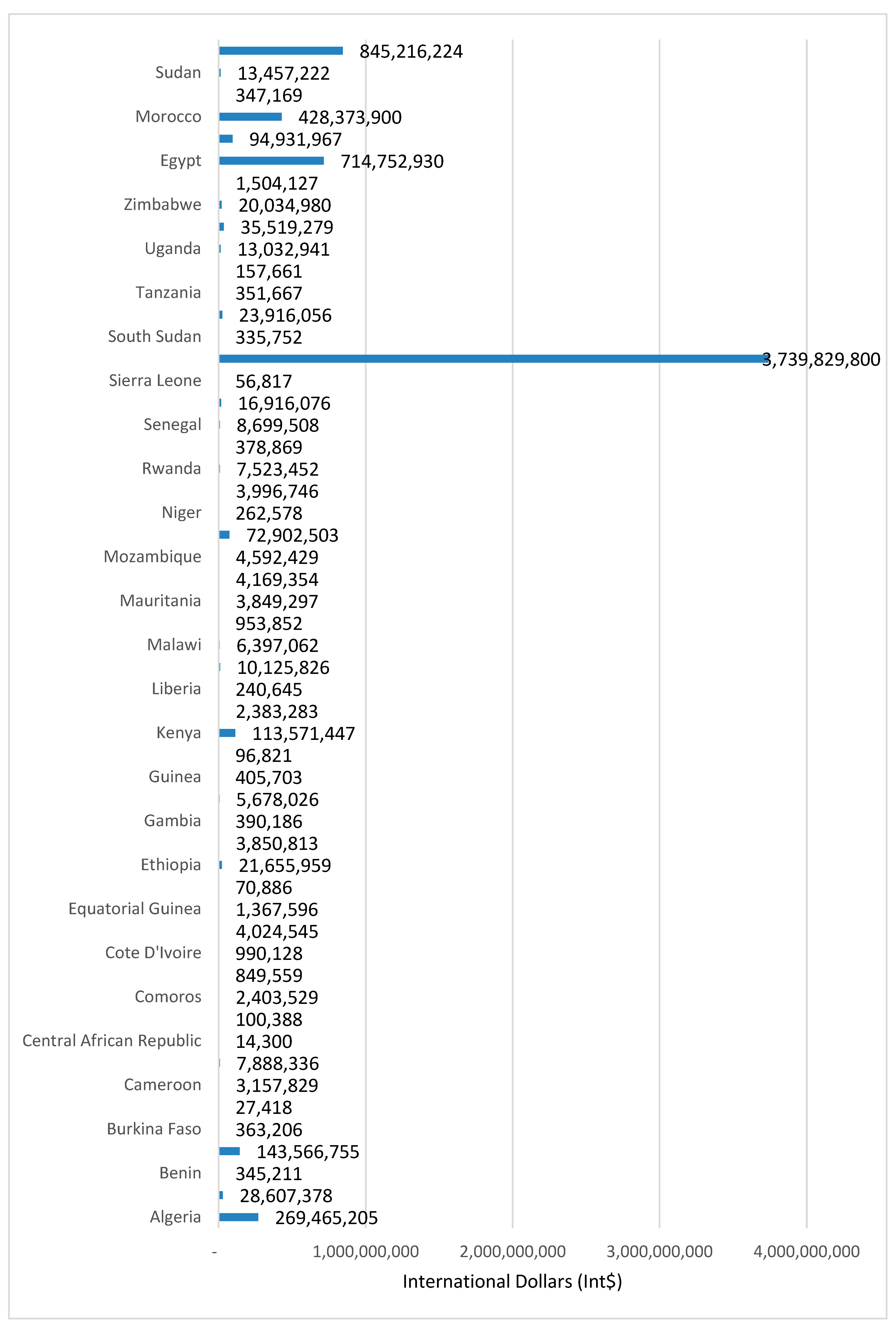
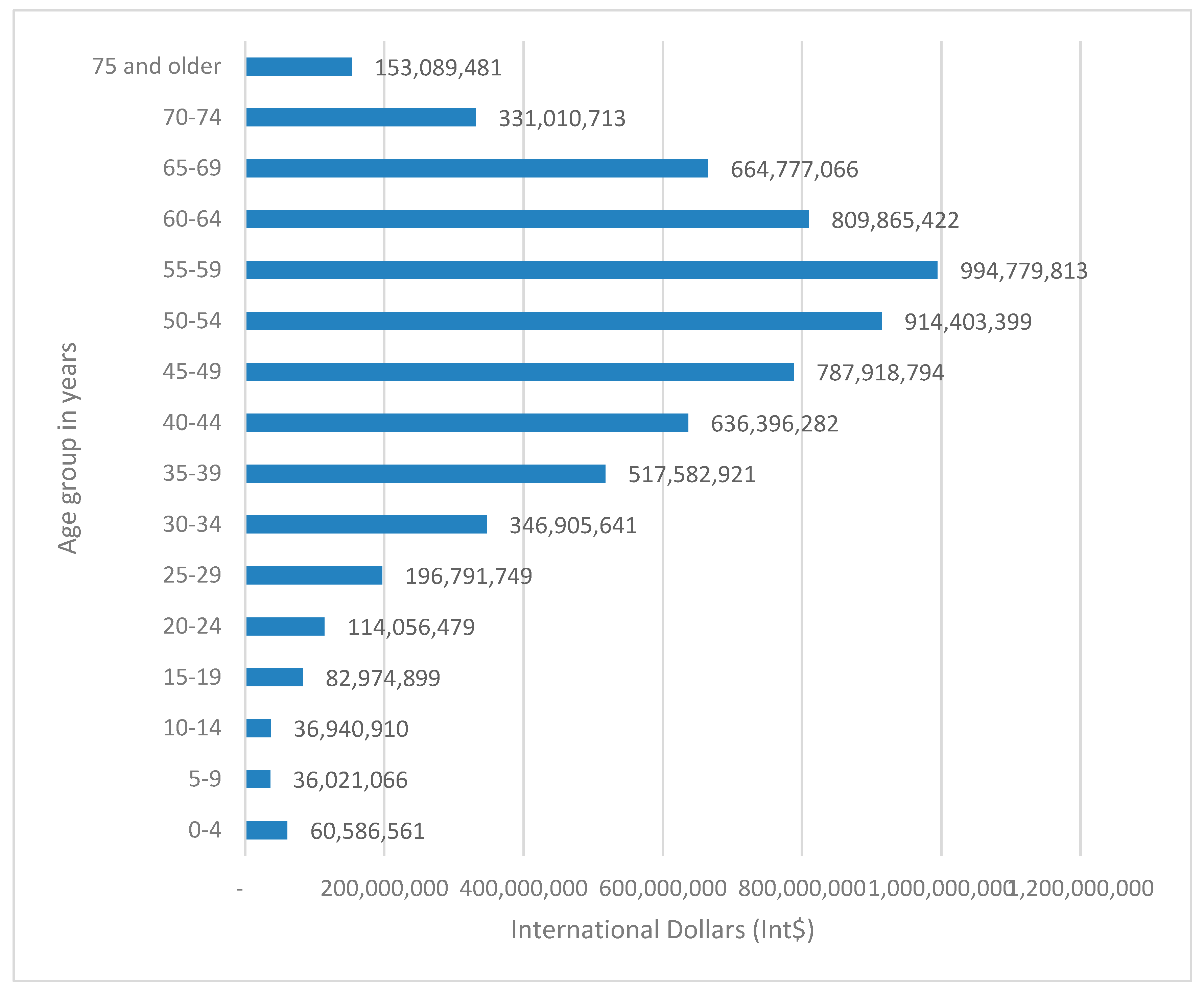
3.1. Discounted Monetary Value of Human Life Losses Associated with COVID-19
Monetary Value of Human Life Losses at a 3% Discount Rate and National Life Expectancies at Birth
3.2. Economic Cost of COVID-19 in Africa
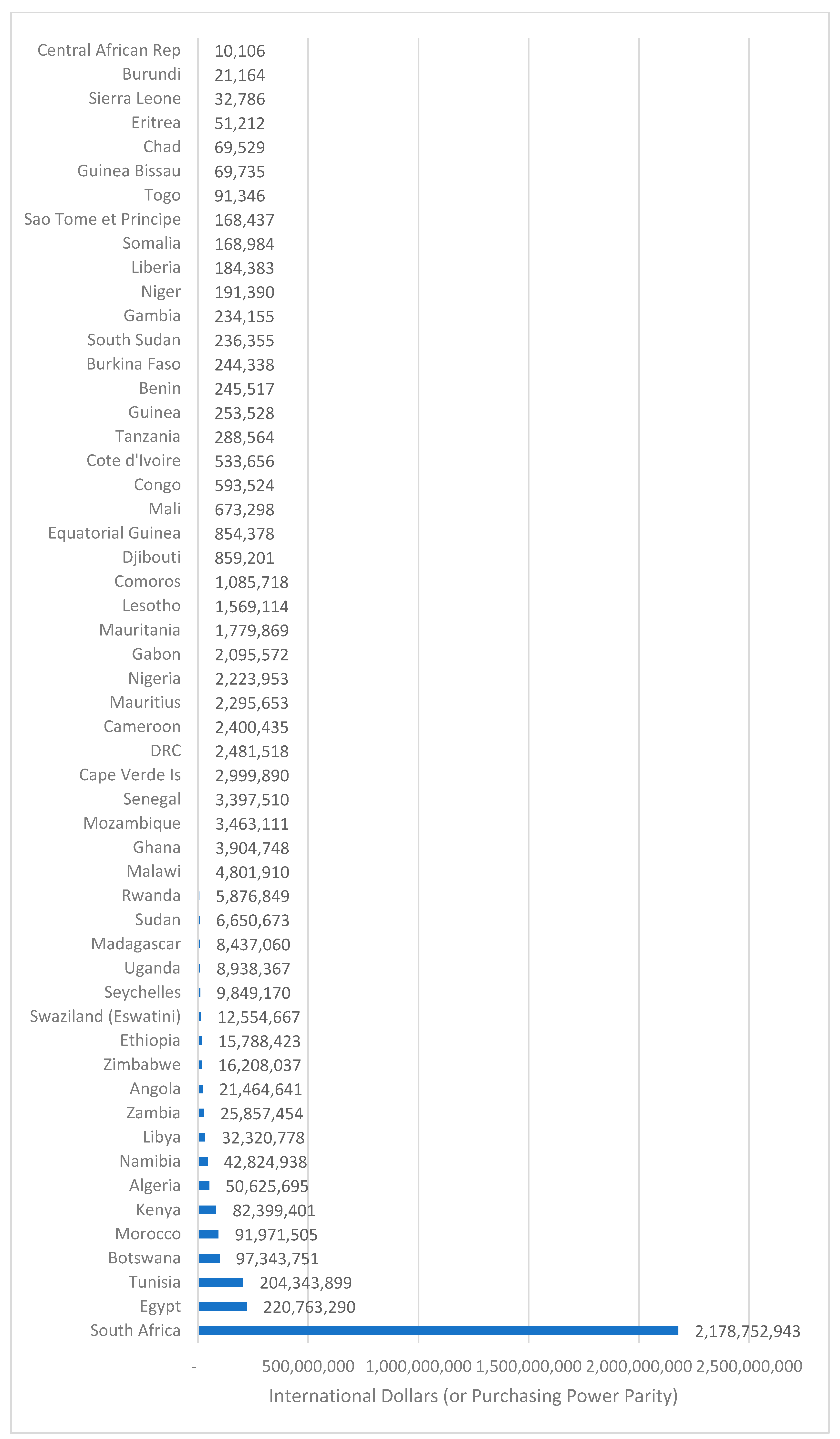
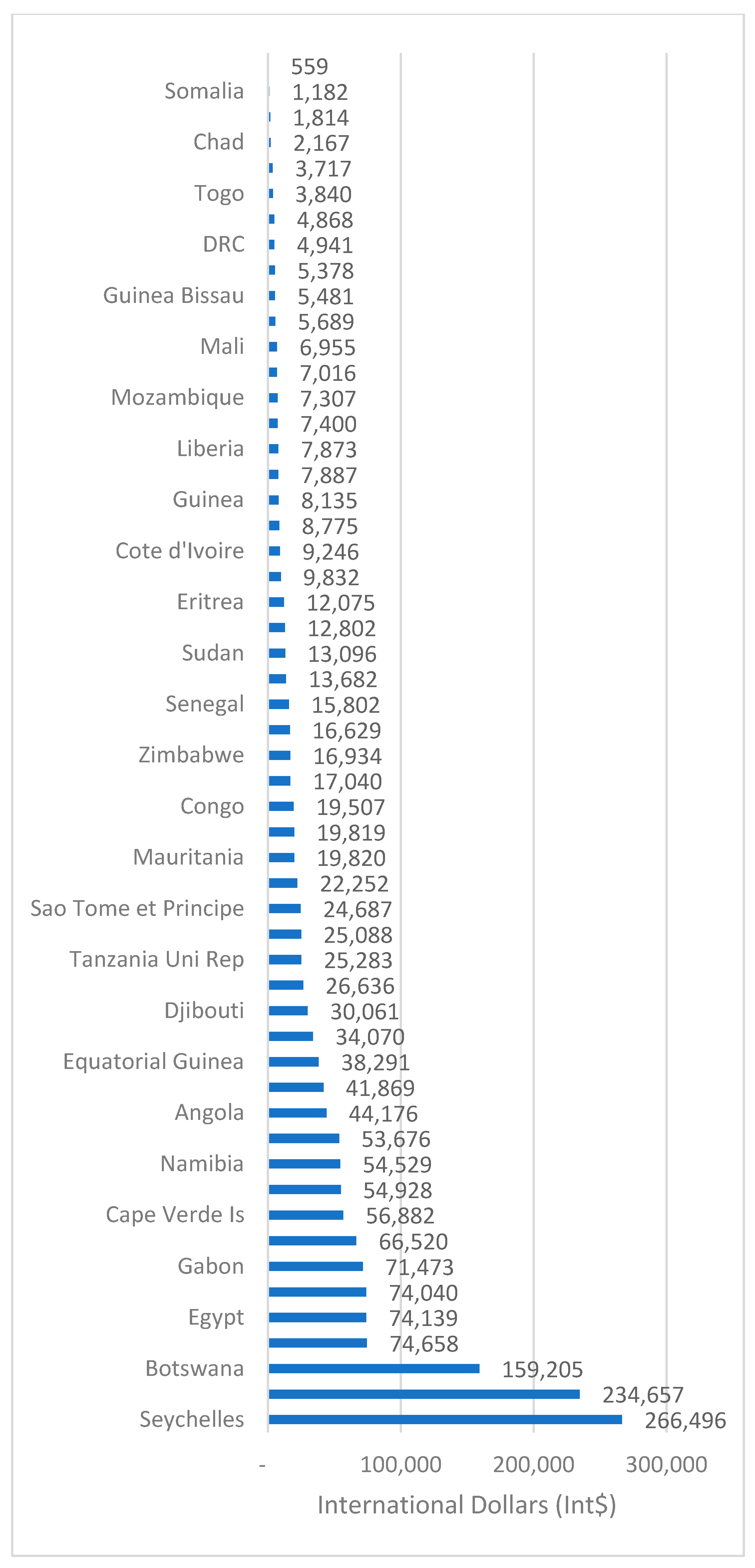
3.2.1. Indirect Cost of COVID-19 in Africa
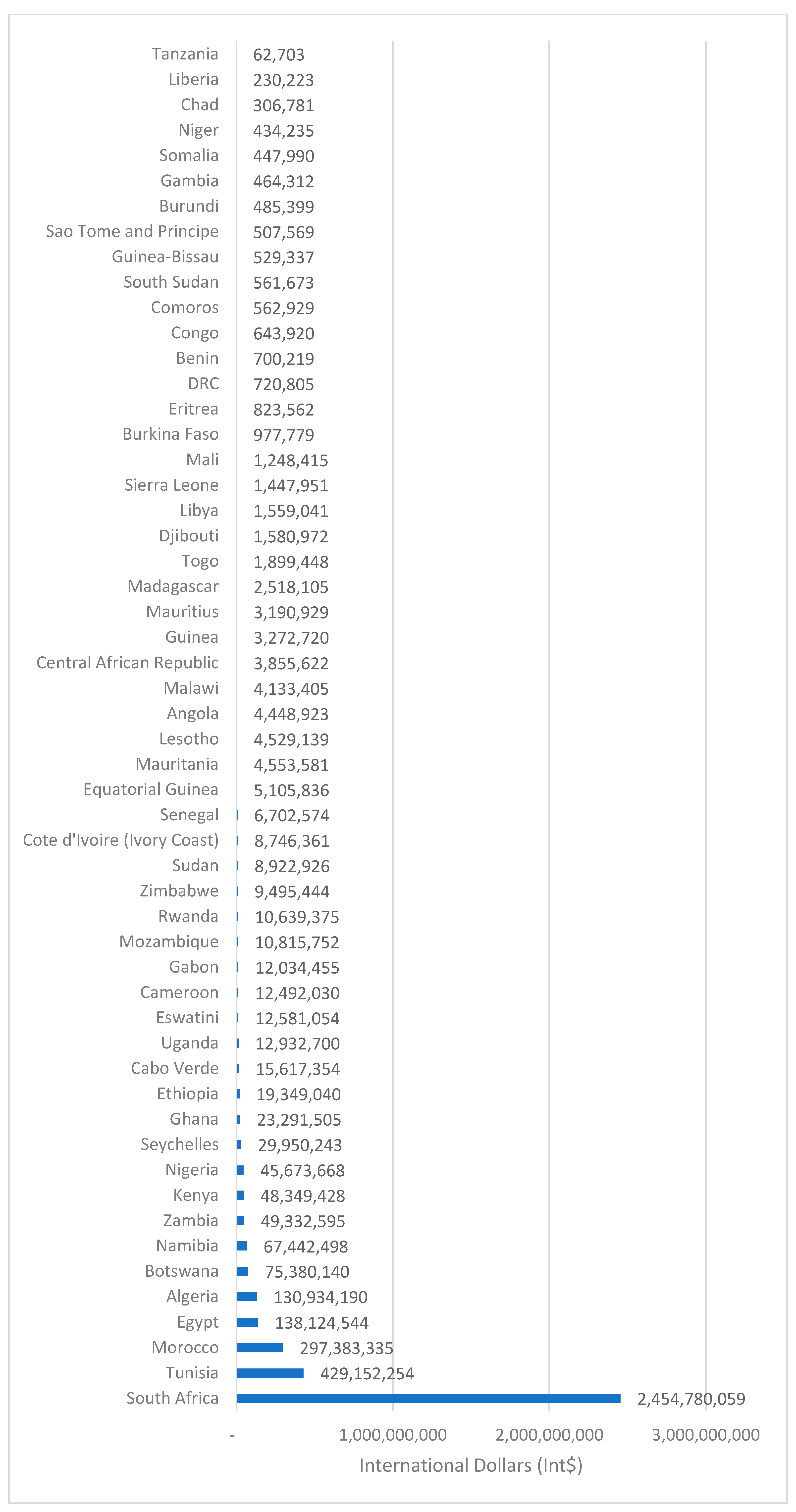
3.2.2. Direct Cost of COVID-19 in Africa
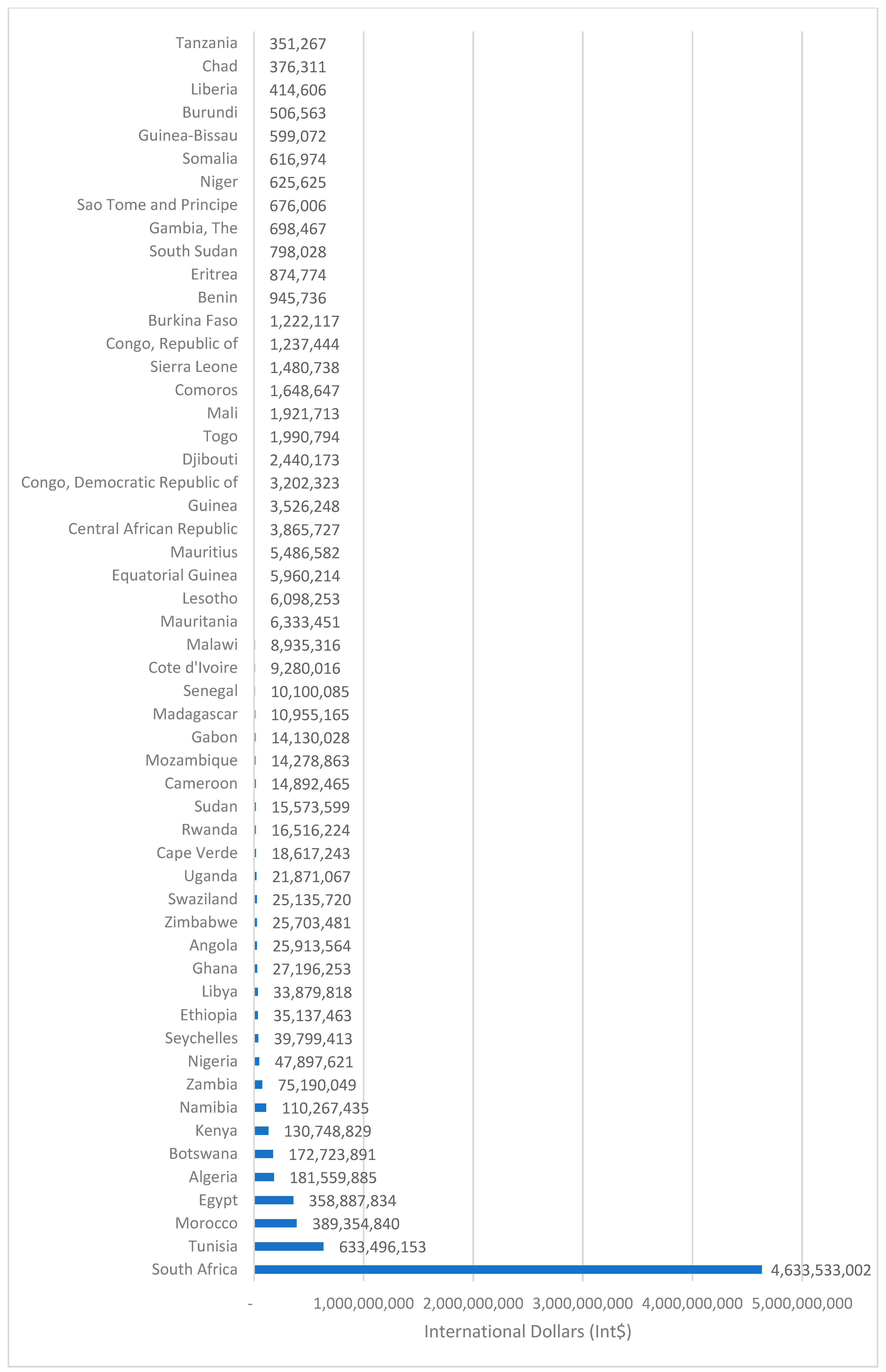
3.2.3. Total Cost of COVID-19 in Africa
3.3. Savings in Potential Direct and Indirect Costs of COVID-19 in Africa Expected from COVID-19 Vaccination
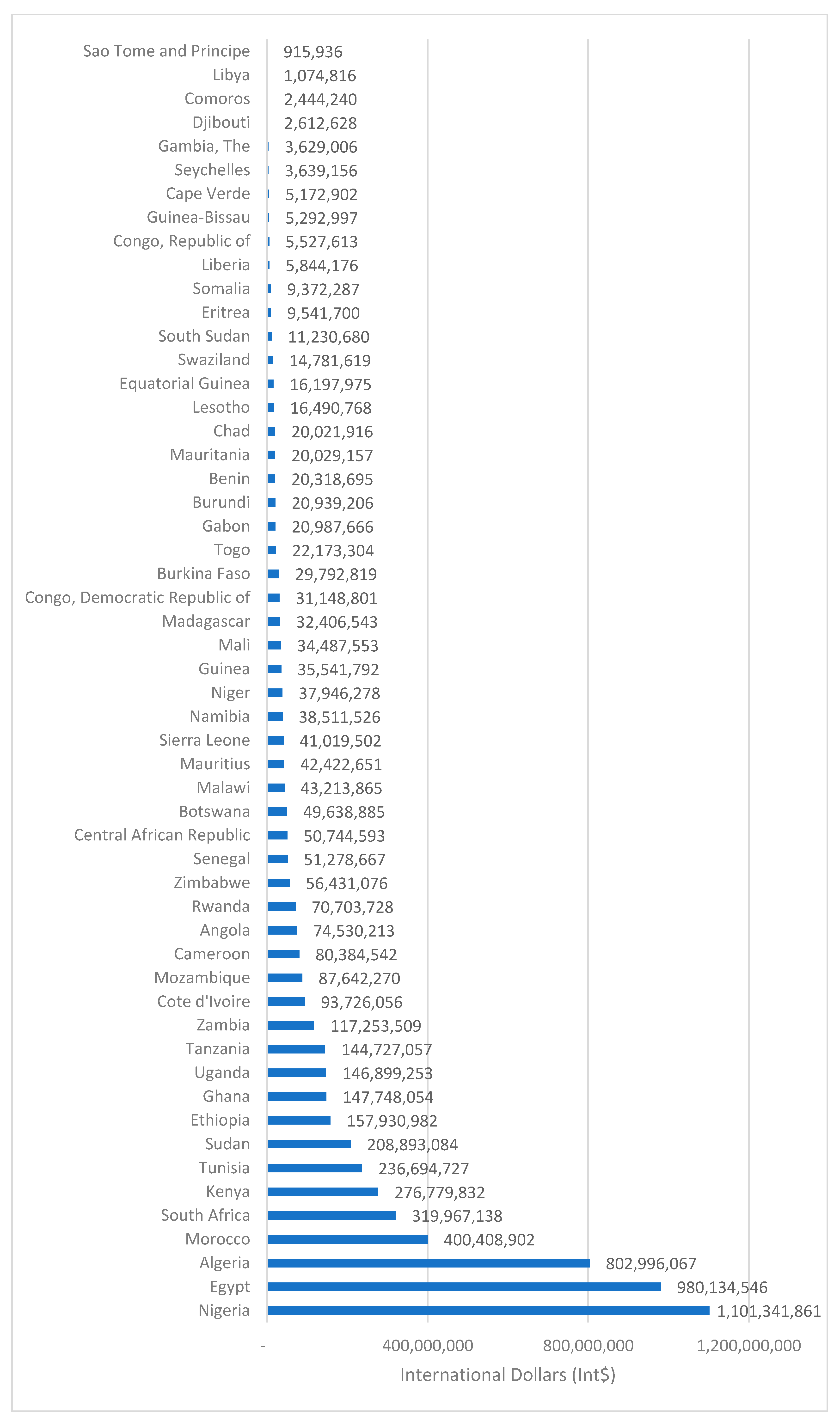
3.3.1. Savings in Potential Direct Costs of COVID-19 in Africa Expected from COVID-19 Vaccination
3.3.2. Savings in Potential Indirect Costs of COVID-19 in Africa Expected from COVID-19 Vaccination
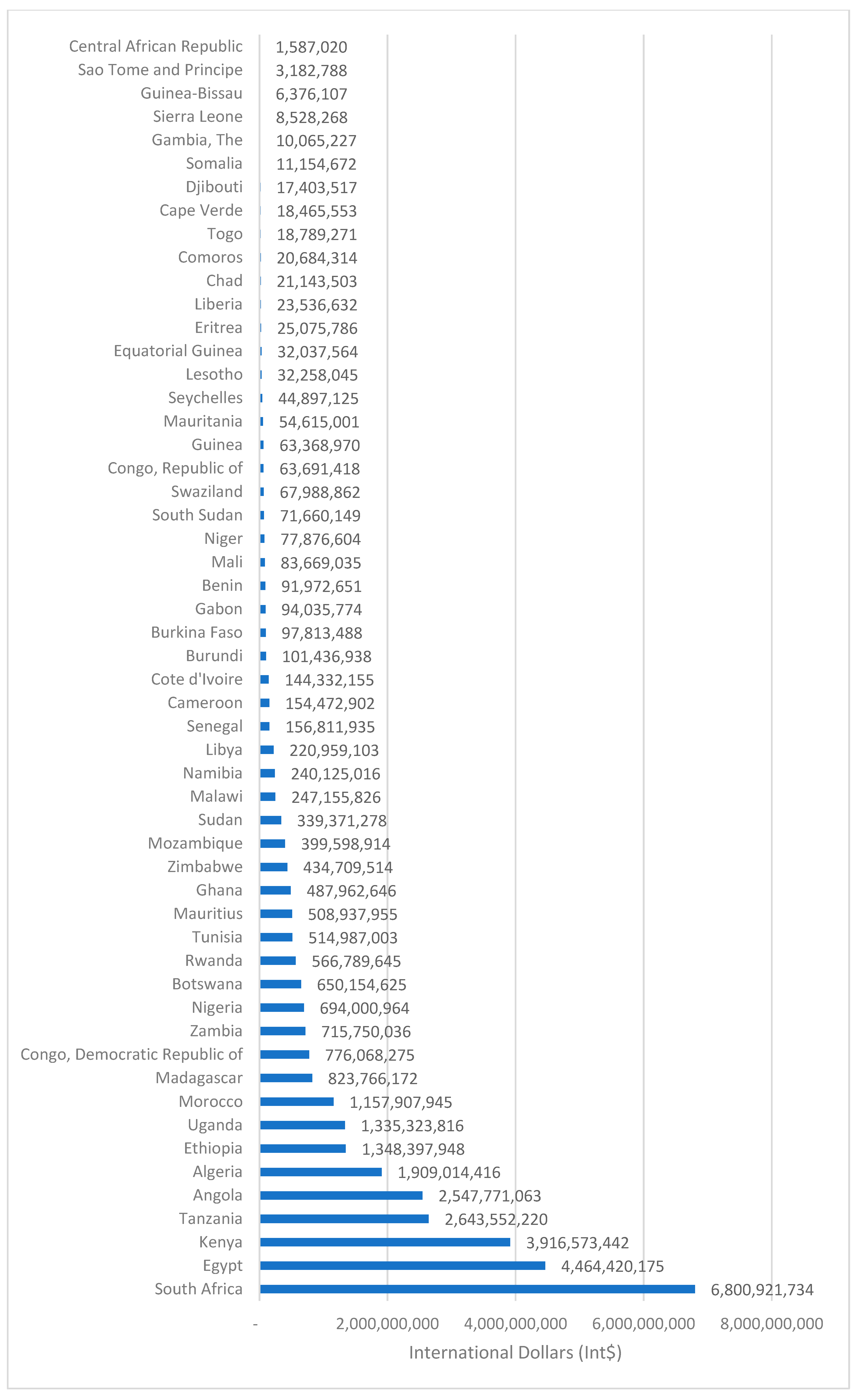
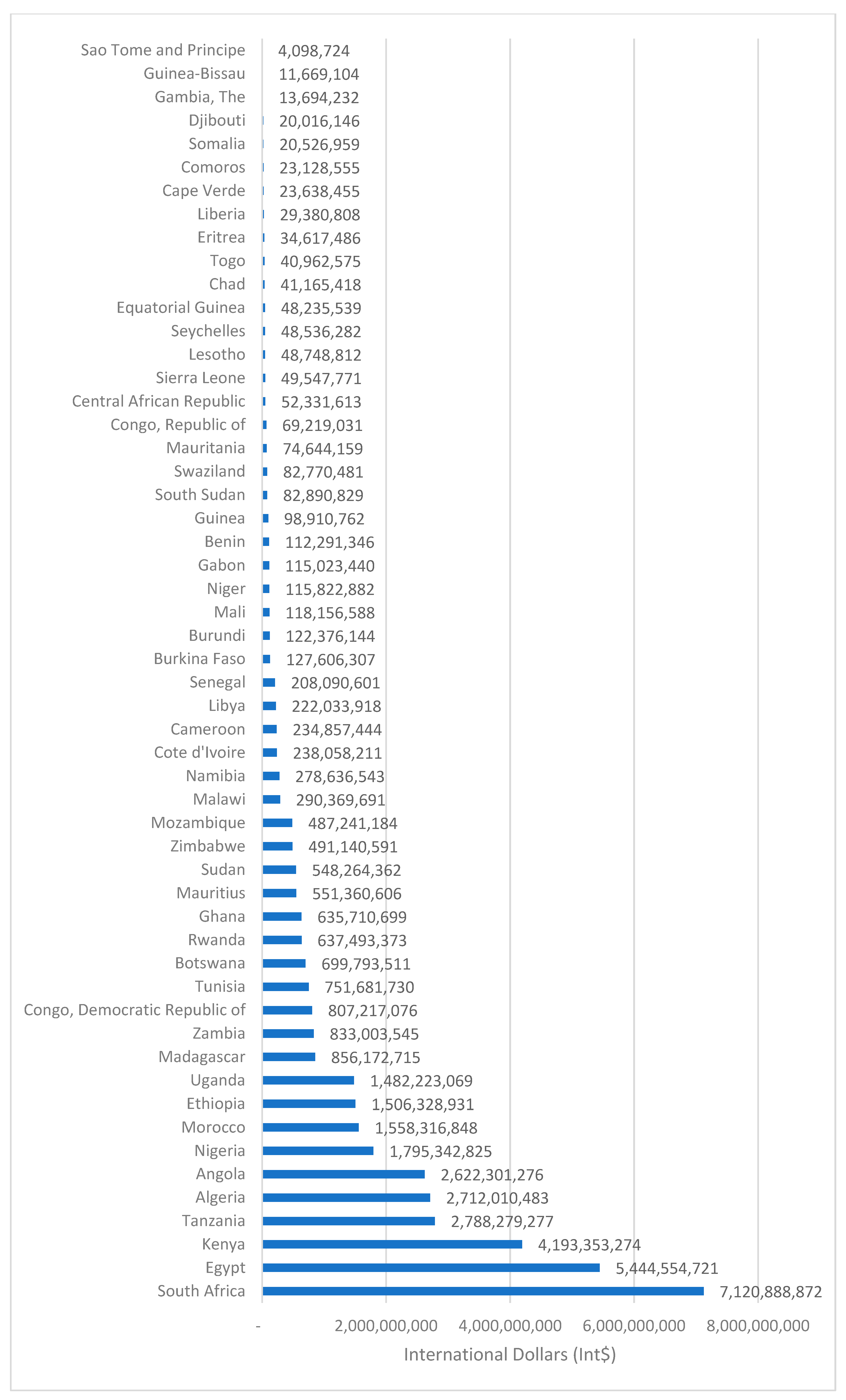
3.3.3. Savings in Potential Total Costs of COVID-19 in Africa Expected from COVID-19 Vaccination
3.4. Sensitivity Analysis
4. Discussion
4.1. Key Findings
4.1.1. Value of Human Life Losses, Indirect Costs, and Direct Costs Associated with Actual Reported COVID-19 Cases
- (a)
- The total discounted monetary value of human life losses associated with 142,171 COVID-19 deaths reported in Africa as of 30 June 2021 at Int$6,684,101,196.
- (b)
- The discounted monetary value per human life lost was Int$47,015, and the monetary value of human life lost per person in the population was Int$4.88.
- (c)
- Approximately 54,210 of 15–64-year-old persons reported dead from COVID-19 in Africa had a total indirect cost of Int$3,173,546,125 (i.e., after adjustment for labor participation rate), and an average of Int$58,542 per life lost (productivity losses).
- (d)
- As of 30 June 2021, the 5,514,709 COVID-19 cases reported in Africa had an estimated total direct cost (TDC) of Int$3,981,927,049. Dividing the estimated TDC by the total number of COVID-19 cases reported in Africa yields an average direct cost of Int$722.06 (US$289.53) per case managed.
- (e)
- The total cost (direct plus indirect) associated with the actual 5,514,709 COVID-19 cases reported in Africa as of 30 June 2021, was approximately Int$7,155,473,174. The average total cost per COVID-19 case was Int$1309 and Int$5.22 per person in the population.
4.1.2. Savings in Potential/Projected Total Costs of COVID-19 in Africa Expected from COVID-19 Vaccination Findings
- (a)
- How many people in the population would be infected with COVID-19 without and with vaccination? Utilizing the risk rates of infection from Voysey et al. (2021), it is projected that approximately 39,608,709 people would be infected by COVID-19 without vaccination (Control Group) compared to 13,390,885 people with vaccination (Treatment Group). Thus, 100% vaccination coverage of eligible persons would potentially avert an estimated 26,217,824 COVID-19 infections in Africa.
- (b)
- How many people in the population would die from COVID-19 without and with vaccination? Applying the risk of death reported by Bernal et al. (2021), it is estimated that 5,203,814 people would die without vaccination, vis-à-vis 910,580 deaths with vaccination.
- (c)
- How many deaths would be averted by COVID-19 vaccination? An estimated 4,293,234 deaths from COVID-19 would be prevented by vaccination, i.e., 5,203,814 minus 910,580.
- (d)
- How many averted COVID-19 deaths would be within the productive age bracket of 15–64 years? Applying the risk of death reported by Bernal et al. (2021), it is estimated that 1,656,615 people in the 15–64 years age bracket would die without vaccination compared to 289,880 with vaccination. Thus, 1,366,735 deaths in the 15–64-year age bracket would be saved with COVID-19 vaccination, i.e., 1,656,615 minus 289,880.
- (e)
- We estimate that vaccinating all eligible people in the population would save the African continent approximately Int$41,624,735,824 (i.e., equivalent to 0.61% of Africa’s total GDP in 2021). That total saving consists of Int$6.262 billion (15.0%) in direct cost savings and Int$35.363 billion (85.0%) in indirect cost savings.
- (f)
- The benefit–cost ratio of COVID-19 vaccination is 5.8, implying that Africa reaps $6 in return for every $1 spent on COVID-19 vaccination.
- (g)
- The average total saving per person in the population is approximately Int$30.4.
4.2. Comparison with Other Studies
4.2.1. A Comparison of Our Estimates with Results from Similar Studies
4.2.2. Comparison of Estimates from Direct and Indirect Cost Studies
Limitations of the Study
Suggestions for Further Economic Research
- (1)
- Undertake a sub-national analysis of the monetary value of human life losses, direct health system costs, indirect costs, and potential savings from COVID-19 vaccination using an adapted version of the analytical framework developed in the current study.
- (2)
- Conduct simulations assuming different COVID-19 infection and death rates in countries as the pandemic evolves.
- (3)
- Collect primary data to allow valuation of human life loss risk reductions associated with COVID-19 using the willingness-to-pay approach (Robinson et al., 2019).
- (4)
- Use cost-effectiveness analysis, cost-utility analysis, and cost-benefit analysis of mass vaccination against COVID-19 to guide decision-making concerning the choice between the three vaccines, i.e., Pfizer-BioNTech, Moderna, and Oxford–AstraZeneca. An example of such a study is the economic evaluation for mass vaccination against COVID-19 in Taiwan by Wang et al. (2021).
- (5)
- Compute the cost of public health interventions required to (i) prevent the spread of COVID-19, (ii) cover the cost of COVID-19 testing, and (iii) the cost of clinical management of COVID-19 by severity per country. Ismaila et al. (2021) and Barasa et al. (2021) are examples of studies that attempted to estimate unit costs of COVID-19 infection management by level of severity in Ghana and Kenya, respectively.
- (6)
- Calculate and compare the economic welfare loss due to the COVID-19 pandemic relative to a counterfactual scenario. Possible scenarios could include an economy without a pandemic (baseline); an economy with a pandemic but no government response, i.e., a passive government that adopts a laissez-faire approach; an economy with a pandemic but with a government implementing economic policies to mitigate the effects of a pandemic (Benmelech & Tzur-Ilan, 2020; Cortes et al., 2022).
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AADi | Average age at onset of death in the ith age group |
| AERC | African Economic Research Consortium |
| ALEj | Average life expectancy in country j |
| Average cost per COVID-19 test | |
| AMU | Arab Maghreb Union |
| ATICj | Average indirect cost per COVID-19 death in country j |
| AU | African Union |
| Average willingness-to-pay | |
| ECA | East African Community |
| CEHPCj | Current expenditure on health per capita in the jth country in 2021 |
| CEMAC | Central African Economic and Monetary Community |
| COVID-19 | Coronavirus disease 2019 |
| Number of COVID-19-associated deaths prevented | |
| Risk of COVID-19 resulting in death among those vaccinated with the Pfizer-BioNTech BNT162b2 | |
| Risk of COVID-19 resulting in death among the unvaccinated | |
| DYLL | Discounted years of life lost |
| ECOWAS | Economic Community of West African States |
| GDP | Gross domestic product |
| GDPPCj | GDP per capita for the jth country in 2021 |
| HCA | Human capital approach |
| HIV/AIDS | Human immunodeficiency virus infection and acquired immune deficiency syndrome |
| IMF | International Monetary Fund |
| INT$ | International Dollars or Purchasing Power Parity (PPP) |
| COVID-19 infection risk with Oxford–AstraZeneca | |
| COVID-19 infection risk without | |
| IVA | Implied values approach |
| MVi | Monetary value of a life lost for the ith age group |
| Number of active COVID-19 cases | |
| Average number of working-age family members and friends accompanying and visiting COVID-19 patients | |
| Number of disability days per active COVID-19 case | |
| Number of disability days per recovered person | |
| NHGPPC | Non-health GDP per capita |
| NHRS | National health research system |
| NHS | National health systems |
| Number of persons that recovered from COVID-19 infection in country j | |
| Number of COVID-19 laboratory-diagnosed cases in country j | |
| Average number of days visited by a family/friend per COVID-19 patient | |
| OOPs | Direct out-of-pocket payments (OOPs) |
| Pi | Proportion of COVID-19 deaths borne by age group i |
| Number of country j’s population | |
| Number of people in the jth country that would be expected to die from COVID-19 even though vaccinated | |
| Number of people infected in the jth country expected to die from COVID-19 without vaccination | |
| Number of people in the population infected by COVID-19 without vaccination | |
| r | Discount rate |
| SADC | Southern African Development Community |
| SDH | Social determinants of health |
| TCCOVID-19 | Total economic cost of COVID-19 |
| TCOVDj | Total number of human lives lost from COVID-19 in the jth country |
| Total number of reported COVID-19 cases per country | |
| Total number of cases that tested negative for COVID-19 per country | |
| Total direct costs of COVID-19 | |
| Total indirect costs of COVID-19 | |
| TMVAfrica | African continent’s total monetary value of human life |
| TMVj=1,..,54 | Country j total monetary value |
| Transport of persons with COVID-19 symptoms to testing and treatment centers, and transport of accompanying family persons | |
| Total out-of-pocket payments related to COVID-19 testing, isolation, treatment, health workers’ consultation, medicines, and bribes | |
| Monetary value of quantities of inputs borne by other sectors involved in combating the community spread of COVID-19 infections | |
| Psychic/intangible costs | |
| UDYLL | Undiscounted years of life lost |
| VE | Vaccine efficacy |
| Value of work time lost among all family members (and friends) of working-age accompanying and/or visiting patients. | |
| Value of potentially productive years of life lost among 15–64-year-olds | |
| Value of productive time lost among non-fatal COVID-19 cases in a specific working-age bracket | |
| Wage per day | |
| WHO | World Health Organization |
| WTP | Willingness to pay |
| YLL | Year of life lost |
References
- Adekunjo, F. O., Rasiah, R., Dahlui, M., & Ng, C. W. (2020). Assessing the willingness to pay for HIV counselling and testing service: A contingent valuation study in Lagos State, Nigeria. African Journal of AIDS Research, 19, 287–295. [Google Scholar] [CrossRef] [PubMed]
- African Union (AU). (2020). Impact of the coronavirus (COVID-19) on the African economy. AU. [Google Scholar]
- Asante, A., Wasike, W. S. K., & Ataguba, J. E. (2020). Health financing in Sub-Saharan Africa: From analytical frameworks to empirical evaluation. Applied Health Economics and Health Policy, 18, 743–746. [Google Scholar] [CrossRef]
- Attema, A. E., Brouwer, W. B. F., & Claxton, K. (2018). Discounting in economic evaluations. PharmacoEconomics, 36, 745–758. [Google Scholar] [CrossRef]
- Barasa, E., Kairu, A., Ng’ang’a, W., Maritim, M., Were, V., Akech, S., & Mwangangi, M. (2021). Examining unit costs for COVID-19 case management in Kenya. BMJ Global Health, 6, e004159. [Google Scholar] [CrossRef] [PubMed]
- Benmelech, E., & Tzur-Ilan, N. (2020). The determinants of fiscal and monetary policies during the COVID-19 crisis. NBER Working Paper No. 27461. U.S. National Bureau Of Economic Research. [Google Scholar] [CrossRef]
- Bernal, J. L., Andrews, N., Gower, C., Robertson, C., Stowe, J., Tessier, E., Simmons, R., Cottrell, S., Roberts, R., O’Doherty, M., & Brown, K. (2021). Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on COVID-19-related symptoms, hospital admissions, and mortality in older adults in England: Test negative case-control study. British Medical Journal, 373, n1088. [Google Scholar] [CrossRef] [PubMed]
- Bhanot, D., Singh, R., Verma, S. K., & Sharad, S. (2021). Stigma and discrimination during the COVID-19 Pandemic. Frontiers in Public Health, 8, 577018. [Google Scholar] [CrossRef]
- Cabarkapa, S., Nadjidai, S. E., Murgier, J., & Ng, C. H. (2020). The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain, Behavior, & Immunity—Health, 8, 100144. [Google Scholar] [CrossRef]
- Campello, M., Kankanhalli, G., & Muthukrishnan, P. (2024). Corporate hiring under COVID-19: Financial constraints and the nature of new jobs. Journal of Financial and Quantitative Analysis, 59(4), 1541–1585. [Google Scholar] [CrossRef]
- Catma, S., & Varol, S. (2021). Willingness to pay for a hypothetical COVID-19 vaccine in the United States: A contingent valuation approach. Vaccines, 9, 318. [Google Scholar] [CrossRef]
- Cerda, A. A., & García, L. Y. (2021). Willingness to pay for a COVID-19 vaccine. Applied Health Economics and Health Policy, 19, 343–351. [Google Scholar] [CrossRef]
- Cesare, C. (2020). COVID-19 psychological implications: The role of shame and guilt. Frontiers in Psychology, 11, 571828. [Google Scholar] [CrossRef]
- Chima, R. I., Goodman, C., & Mills, A. (2003). The economic impact of malaria in Africa: A critical review of the evidence. Health Policy, 63, 17–36. [Google Scholar] [CrossRef]
- Claxton, K., Paulden, M., Gravelle, H., Brouwer, W., & Culyer, A. J. (2011). Discounting and decision making in the economic evaluation of health-care technologies. Health Economics, 20, 2–15. [Google Scholar] [CrossRef]
- Cortes, G. S., Gao, G. P., Silva, F. B. G., & Song, Z. (2022). Unconventional monetary policy and disaster risk: Evidence from the subprime and COVID–19 crises. Journal of International Money and Finance, 122, 102543. [Google Scholar] [CrossRef]
- Costa-Font, J., Rudisill, C., Harrison, S., & Salmasi, L. (2021). The social value of a SARS-CoV-2 vaccine: Willingness to pay estimates from four western countries (pp. 1–41). IZA Discussion Paper Series No. 14475. IZA Institute of Labor Economics, Department of Economics and Finance, Rome (Italy), Catholic University. Available online: http://ftp.iza.org/dp14475.pdf (accessed on 28 August 2021).
- Cross, M. J., March, L. M., Lapsley, H. M., Tribe, K. L., Brnabic, A. J., Courtenay, B. G., & Brooks, P. M. (2000). Determinants of willingness to pay for hip and knee joint replacement surgery for osteoarthritis. Rheumatology, 39, 1242–1248. [Google Scholar] [CrossRef] [PubMed]
- Drummond, M. F., Sculpher, M. J., Claxton, K., Stoddart, G. L., & Torrance, G. W. (2015). Methods for the economic evaluation of health care programmes (4th ed., pp. 1–437). Oxford University Press. [Google Scholar]
- Dubey, S., Biswas, P., Ghosh, R., Chatterjee, S., Dubey, M. J., Chatterjee, S., Lahiri, D., & Lavie, C. J. (2020). Psychosocial impact of COVID-19. Diabetes & Metabolic Syndrome, 14, 779–788. [Google Scholar] [CrossRef]
- Edejer, T. T. T., Baltussen, R., Adam, T., Hutubessy, R., Acharya, A., Evans, D. B., & Murray, C. J. L. (Eds.). (2003). Making choices in health: WHO guide to cost-effectiveness analysis (pp. 1–318). WHO. [Google Scholar]
- Eichenbaum, M. S., Rebelo, S., & Trabandt, M. (2021). The macroeconomics of epidemics. The Review of Financial Studies, 34(11), 5149–5187. [Google Scholar] [CrossRef]
- Fein, R. (1958). Economics of mental illness (pp. 1–139). Basic Books. [Google Scholar]
- Funke, M., Schularick, M., & Trebesch, C. (2023). Populist leaders and the economy. American Economic Review, 113(12), 3249–3288. [Google Scholar] [CrossRef]
- Geirdal, A. Ø., Ruffolo, M., Leung, J., Thygesen, H., Price, D., Bonsaksen, T., & Schoultz, M. (2021). Mental health, quality of life, wellbeing, loneliness and use of social media in a time of social distancing during the COVID-19 outbreak. A cross-country comparative study. Journal of Mental Health, 30, 148–155. [Google Scholar] [CrossRef]
- Govindarajan, V., Ilyas, H., Silva, F. B. G., Srivastava, A., & Enache, L. (2022). How companies can prepare for a long run of high inflation. Harvard Business Review. Available online: https://hbr.org/2022/05/how-companies-can-prepare-for-a-long-run-of-high-inflation (accessed on 20 June 2025).
- Gronholm, P., Nosé, M., Van Brakel, W., Eaton, J., Ebenso, B., Fiekert, K., Milenova, M., Sunkel, C., Barbui, C., & Thornicroft, G. (2021). Reducing stigma and discrimination associated with COVID-19: Early-stage pandemic rapid review and practical recommendations. Epidemiology and Psychiatric Sciences, 30, e15. [Google Scholar] [CrossRef]
- Grossman, M. (2000). The human capital model. In A. J. Culyer, & J. P. Newhouse (Eds.), Handbook of health economics (Vol. 1, pp. 348–408). Elsevier. [Google Scholar]
- Haacker, M., Hallett, T. B., & Atun, R. (2020). On discount rates for economic evaluations in global health. Health Policy and Planning, 35, 107–111. [Google Scholar] [CrossRef] [PubMed]
- Hanly, P., Ahern, M., Sharp, L., Ursul, D., & Loughnane, G. (2022). The cost of lost productivity due to premature mortality associated with COVID-19: A Pan-European study. The European Journal of Health Economics, 23(2), 249–259. [Google Scholar] [CrossRef] [PubMed]
- Himmler, S., van Exel, J., & Brouwer, W. (2022). Did the COVID-19 pandemic change the willingness to pay for an early warning system for infectious diseases in Europe? The European Journal of Health Economics, 23, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Ilesanmi, O., Afolabi, A., & Uchendu, O. (2021). The prospective COVID-19 vaccine: Willingness to pay and perception of community members in Ibadan, Nigeria. PeerJ, 9, e11153. [Google Scholar] [CrossRef]
- International Monetary Fund (IMF). (2021). World economic outlook database. Update, January 2021. Available online: https://www.imf.org/en/Publications/WEO/weo-database/2020/October (accessed on 16 June 2021).
- Ismaila, H., Asamani, J. A., Lokossou, V. K., Oduro-Mensah, E. O., Nabyonga-Orem, J., & Akoriyea, S. K. (2021). The cost of clinical management of SARSCOV-2 (COVID-19) infection by the level of disease severity in Ghana: A protocol-based cost of illness analysis. BMC Health Services Research, 21, 1115. [Google Scholar] [CrossRef]
- Jimoh, A., Sofola, O., Petu, A., & Okorosobo, T. (2007). Quantifying the economic burden of malaria in Nigeria using the willingness to pay approach. Cost Effectiveness and Resource Allocation, 5, 6. [Google Scholar] [CrossRef] [PubMed]
- Jones-Lee, M. W. (1982). The value of life and safety (pp. 1–309). North Holland. [Google Scholar]
- Jones-Lee, M. W. (1985). The value of life and safety: A survey of recent developments. The Geneva Papers on Risk and Insurance, 10, 141–173. [Google Scholar] [CrossRef]
- Kankeu, H. T., Saksena, P., Xu, K., & Evans, D. B. (2013). The financial burden from non-communicable diseases in low-and middle-income countries: A literature review. Health Research Policy and Systems, 11, 31. [Google Scholar] [CrossRef]
- Kirigia, J. M., & Muthuri, R. N. D. K. (2020a). The fiscal value of human lives lost from coronavirus disease (COVID-19) in China. BMC Research Notes, 13, 198. [Google Scholar] [CrossRef]
- Kirigia, J. M., & Muthuri, R. N. D. K. (2020b). The discounted money value of human lives lost due to COVID-19 in Spain. Journal of Health Research, 34, 455–460. [Google Scholar] [CrossRef]
- Kumar, A., & Nayar, K. R. (2021). COVID-19 and its mental health consequences. Journal of Mental Health, 30, 1–2. [Google Scholar] [CrossRef]
- Landefeld, J. S., & Seskin, E. P. (1982). The economic value of life: Linking theory to practice. American Journal of Public Health, 72, 555–566. [Google Scholar] [CrossRef]
- Lin, Y., Hu, Z., Zhao, Q., Alias, H., Danaee, M., & Wong, L. P. (2020). Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLOS Neglected Tropical Diseases, 14, e0008961. [Google Scholar] [CrossRef]
- Mooney, G. H. (1977). The valuation of human life (pp. 1–165). Macmillan. [Google Scholar]
- Mostafa, A., Sabry, W., & Mostafa, N. S. (2020). COVID-19-related stigmatisation among a sample of Egyptian healthcare workers. PLoS ONE, 15, e0244172. [Google Scholar] [CrossRef] [PubMed]
- Msemburi, W., Karlinsky, A., Knutson, V., Aleshin-Guendel, S., Chatterji, S., & Wakefield, J. (2023). The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature, 613, 130–137. [Google Scholar] [CrossRef]
- Musango, L., Mandrosovololona, V., Randriatsarafara, F. M., Ranarison, V. M., Kirigia, J. M., & Ratsimbasoa, A. C. (2024). The present value of human life losses associated with COVID-19 and likely productivity losses averted through COVID-19 vaccination in Madagascar. BMC Public Health, 24, 3296. [Google Scholar] [CrossRef]
- Mushkin, S. J., & Collings, F. A. (1959). Economic costs of disease and injury. Public Health Reports, 74, 795–809. [Google Scholar] [CrossRef] [PubMed]
- Nabyonga-Orem, J., Christmal, C., Addai, K. F., Mwinga, K., Aidam, K., Nachinab, G., Namuli, S., & Asamani, J. A. (2023). The state and significant drivers of health systems efficiency in Africa: A systematic review and meta-analysis. Journal of Glob Health, 13, 04131. [Google Scholar] [CrossRef] [PubMed]
- Niewiadomski, P., Ortega-Ortega, M., & Łyszczarz, B. (2025). Productivity losses due to health problems arising from COVID-19 pandemic: A systematic review of population-level studies worldwide. Applied Health Economics and Health Policy, 23, 231–251. [Google Scholar] [CrossRef]
- Odum, A. L., Becker, R. J., Haynes, J. M., Galizio, A., Frye, C. C. J., Downey, H., Friedel, J. E., & Perez, D. M. (2020). Delay discounting of different outcomes: Review and theory. Journal of the Experimental Analysis of Behavior, 113, 657–679. [Google Scholar] [CrossRef]
- Onwujekwe, O., Orjiakor, C., Ogbozor, P., Agu, I., Agwu, P., Wright, T., Balabanova, D., & Kohler, J. (2023). Examining corruption risks in the procurement and distribution of COVID-19 vaccines in select states in Nigeria. Journal of Pharmaceutical Policy & Practice, 16(1), 141. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development (OECD). (2000). A system of health accounts. Version 1.0 (pp. 1–184). OECD. [Google Scholar]
- Petty, W. (1699). Political arithmetick, or a discourse: Concerning the extent and value of lands, people, buildings; husbandry, manufacture, commerce, fishery, artizans, seamen, soldiers; publick revenues, interest, taxes, superlucration, registries, banks. Robert Caluel. [Google Scholar]
- Rice, D. P. (2000). Cost of illness studies: What is good about them? Injury Prevention, 6, 177–179. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L., Hammitt, J., & O’Keeffe, L. (2019). Valuing mortality risk reductions in global benefit-cost analysis. Journal of Benefit-Cost Analysis, 10(S1), 15–50. [Google Scholar] [CrossRef] [PubMed]
- Rusakaniko, S., Makanga, M., Ota, M., Bockarie, M., Banda, G., Okeibunor, J., Mutapi, F., Tumusiime, P., Nyirenda, T., Kirigia, J. M., & Nabyonga-Orem, J. (2019). Strengthening national health research systems in the WHO African region—Progress towards universal health coverage. Globalization and Health, 15, 50. [Google Scholar] [CrossRef] [PubMed]
- Shiell, A., Gerard, K., & Donaldson, C. (1987). Cost of illness studies: An aid to decision-making? Health Policy, 8, 317–323. [Google Scholar] [CrossRef]
- Slothuus, U., & Brooks, R. G. (2000). Willingness to pay in arthritis: A Danish contribution. Rheumatology, 39, 791–799. [Google Scholar] [CrossRef]
- Statista. (2021a). Distribution of coronavirus (COVID-19) deaths in South Africa as of November 16, 2020, by age. Available online: https://www.statista.com/statistics/1127280/coronavirus-covid-19-deaths-by-age-distribution-south-africa/ (accessed on 2 June 2021).
- Statista. (2021b). Coronavirus (COVID-19) mortality rate in Tunisia as of January 2021, by age group (in deaths per 100,000 individuals). Available online: https://www.statista.com/statistics/1203320/covid-19-mortality-rate-in-tunisia-by-age-group/ (accessed on 2 June 2021).
- Stiglitz, J. E., Sen, A., & Fitoussi, J. P. (Eds.). (2010). Mismeasuring our lives: Why GDP doesn’t add up (pp. 1–176). The New Press. [Google Scholar]
- Thabane, L., Mbuagbaw, L., Zhang, S., Samaan, Z., Marcucci, M., Ye, C., Thabane, M., Giangregorio, L., Dennis, B., Kosa, D., Debono, V. B., Dillenburg, R., Fruci, V., Bawor, M., Lee, J., Wells, G., & Goldsmith, C. H. (2013). A tutorial on sensitivity analyses in clinical trials: The what, why, when and how. BMC Medical Research Methodology, 13, 92. [Google Scholar] [CrossRef]
- Thorbecke, E. (2022). What can Africa learn from a better understanding of the interaction among growth, inequality and poverty in the fight against the COVID-19 pandemic? Research Report, January 6, 2022, Prepared for the AERC Collaborative Project on Addressing Health Financing Gaps and Vulnerabilities in Africa Due to the Covid-19. AERC. [Google Scholar]
- United Nations (UN). (2015). Transforming our world: The 2030 agenda for sustainable development (pp. 1–35). General Assembly Resolution A/RES/70/1. UN. [Google Scholar]
- Voysey, M., Clemens, S. A. C., Madhi, S. A., Weckx, L. Y., Folegatti, P. M., Aley, P. K., Angus, B., Baillie, V. L., Barnabas, S. L., Bhorat, Q. E., Bibi, S., Briner, C., Cicconi, P., Clutterbuck, E. A., Collins, A. M., Cutland, C. L., Darton, T. C., Dheda, K., Dold, C., … Duncan, C. J. A. (2021). Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: A pooled analysis of four randomised trials. Lancet, 397, 881–891. [Google Scholar] [CrossRef]
- Wang, W.-C., Fann, F. C.-Y., Chang, R.-E., Jeng, Y.-C., Hsu, C.-Y., Chen, H.-H., Liu, J.-T., & Yen, A. M.-F. (2021). Economic evaluation for mass vaccination against COVID-19. Journal of the Formosan Medical Association, 120(S1), S95–S105. [Google Scholar] [CrossRef]
- Weisbrod, B. A. (1971). Costs and benefits of medical research: A case study of poliomyelitis. Journal of Political Economy, 79, 527–544. [Google Scholar] [CrossRef]
- WHO. (2001). Macroeconomics and health: Investing in health for economic development (pp. 1–210). WHO. [Google Scholar]
- WHO. (2009). Guide to identifying the economic consequences of disease and injury (pp. 1–132). WHO. [Google Scholar]
- WHO. (2019a). Global health expenditure database. Available online: https://apps.who.int/nha/database/Select/Indicators/en (accessed on 17 July 2021).
- WHO. (2019b). World health statistics overview 2019: Monitoring health for the SDGs, sustainable development goals (pp. 1–120). WHO. [Google Scholar]
- WHO. (2020). Global health observatory data repository. International health regulations (2005) monitoring framework, SPAR. Available online: http://apps.who.int/gho/data/node.main.IHRSPAR?lang=en (accessed on 19 December 2020).
- WHO. (2021a). Global health observatory. UHC service coverage index. Available online: http://apps.who.int/gho/portal/uhc-overview.jsp (accessed on 30 July 2021).
- WHO. (2021b). Global health observatory data repository. Water, sanitation, and hygiene. Available online: https://apps.who.int/gho/data/node.main.166?lang=en (accessed on 14 November 2021).
- WHO. (2021c). World health statistics 2021: Monitoring health for the SDGs, sustainable development goals (pp. 1–121). WHO. [Google Scholar]
- WHO/AFRO. (2006). Health financing: A strategy for the African region (pp. 1–16). Document AFR/RC56/10. WHO/AFRO. [Google Scholar]
- WHO/AFRO. (2012). The African health observatory: Opportunity for strengthening health information systems through national health observatories (pp. 1–6). Sixty-Second Session Regional Committee for Africa Document AFR/RC62/13. WHO/AFRO. [Google Scholar]
- World Bank. (2021). Labour force participation rate, total (% of total population ages 15–64) (modelled ILO estimate). Available online: https://data.worldbank.org/indicator/SL.TLF.ACTI.ZS (accessed on 6 September 2021).
- Worldometer. (2021). COVID-19 coronavirus pandemic. Last updated: June 30, 2021, 06:03 GMT. Available online: https://www.worldometers.info/coronavirus/?#countries (accessed on 30 June 2021).
- Zhao, J., HuajieJin, H., Li, X., Zheng, W., Wang, H., & Pennington, M. (2021). Disease burden attributable to the first wave of COVID-19 in China and the effect of timing on the cost-effectiveness of movement restriction policies. Value in Health, 24, 615–624. [Google Scholar] [CrossRef] [PubMed]

| Age Group (Years) | South Africa (Percent) * | Tunisia (Percent) ** |
|---|---|---|
| 0–4 years | 0.275 | 0.014 |
| 5–9 years | 0.175 | 0.000 |
| 10–14 years | 0.175 | 0.014 |
| 15–19 years | 0.375 | 0.078 |
| 20–24 years | 0.575 | 0.071 |
| 25–29 years | 1.075 | 0.107 |
| 30–34 years | 2.075 | 0.170 |
| 35–39 years | 3.275 | 0.448 |
| 40–44 years | 4.575 | 0.618 |
| 45–49 years | 6.575 | 1.051 |
| 50–54 years | 8.975 | 2.223 |
| 55–59 years | 12.675 | 4.482 |
| 60–64 years | 14.175 | 9.192 |
| 65–69 years | 13.175 | 18.802 |
| 70–74 years | 10.675 | 23.114 |
| 75 years and older | 21.175 | 39.615 |
| Age Group | Average Age of Onset (Years) * |
|---|---|
| 0–4 years | 2 |
| 5–9 years | 7 |
| 10–14 years | 12 |
| 15–19 years | 17 |
| 20–24 years | 22 |
| 25–29 years | 27 |
| 30–34 years | 32 |
| 35–39 years | 37 |
| 40–44 years | 42 |
| 45–49 years | 47 |
| 50–54 years | 52 |
| 55–59 years | 57 |
| 60–64 years | 62 |
| 65–69 years | 67 |
| 70–74 years | 72 |
| Group | (A) Group Size | (B) No. Infected | (C) Infection Risk [C = (B/A)] | (D) Infection Risk (%) [D = C × 100] |
|---|---|---|---|---|
| Control | 8581 | 248 | 0.02890106 | 2.890106048 |
| ChAdOx1 nCov-19 (AZ) | 8597 | 84 | 0.00977085 | 0.97708503 |
| Group | (A) Total No of Cases * | (B) No. of Deaths * | (C) Death Risk [C = (B/A)] ** | (D) Death Risk (%) [D = C × 100] ** |
|---|---|---|---|---|
| Unvaccinated | 8091 | 1063 | 0.131380546 | 13.13805463 |
| ≥14 days after vaccination | 750 | 51 | 0.068 | 6.8 |
| Vaccine efficacy (VE) | 48.24195673 |
| Country | Population in 2021 * (A) | COVID-19 Deaths as of 30 June 2021 * (B) | Total Discounted Monetary Value of Human Lives Lost (Int$) [C] ** | Discounted Monetary Value per Human Life Lost (Int$) [D = C/B] ** | The Discounted Monetary Value of Human Life Lost per Person in the Population (Int$) [E = C/A] ** |
|---|---|---|---|---|---|
| Algeria | 44,634,463 | 3708 | 269,465,205 | 72,671 | 6.04 |
| Angola | 33,874,015 | 894 | 28,607,378 | 31,999 | 0.84 |
| Benin | 12,436,641 | 104 | 345,211 | 3319 | 0.03 |
| Botswana | 2,398,576 | 1125 | 143,566,755 | 127,615 | 59.85 |
| Burkina Faso | 21,468,861 | 168 | 363,206 | 2162 | 0.02 |
| Burundi | 12,239,994 | 8 | 27,418 | 3427 | 0.00 |
| Cameroon | 27,198,364 | 1324 | 3,157,829 | 2385 | 0.12 |
| Cape Verde | 561,973 | 286 | 7,888,336 | 27,582 | 14.04 |
| Central African Republic | 4,912,863 | 98 | 14,300 | 146 | 0.00 |
| Chad | 16,890,785 | 174 | 100,388 | 577 | 0.01 |
| Comoros | 887,911 | 146 | 2,403,529 | 16,463 | 2.71 |
| Congo, Republic of | 5,652,216 | 165 | 849,559 | 5149 | 0.15 |
| Cote d’Ivoire | 27,023,309 | 313 | 990,128 | 3163 | 0.04 |
| Congo, Democratic Republic of | 92,245,852 | 924 | 4,024,545 | 4356 | 0.04 |
| Equatorial Guinea | 1,448,396 | 121 | 1,367,596 | 11,302 | 0.94 |
| Eritrea | 3,595,038 | 23 | 70,886 | 3082 | 0.02 |
| Ethiopia | 117,775,639 | 4320 | 21,655,959 | 5013 | 0.18 |
| Gabon | 2,277,613 | 159 | 3,850,813 | 24,219 | 1.69 |
| Gambia, The | 2,483,649 | 181 | 390,186 | 2156 | 0.16 |
| Ghana | 31,714,153 | 795 | 5,678,026 | 7142 | 0.18 |
| Guinea | 13,484,325 | 169 | 405,703 | 2401 | 0.03 |
| Guinea-Bissau | 2,013,948 | 69 | 96,821 | 1403 | 0.05 |
| Kenya | 54,941,831 | 3621 | 113,571,447 | 31,365 | 2.07 |
| Lesotho | 2,159,095 | 329 | 2,383,283 | 7244 | 1.10 |
| Liberia | 5,175,111 | 127 | 240,645 | 1895 | 0.05 |
| Madagascar | 28,393,805 | 911 | 10,125,826 | 11,115 | 0.36 |
| Malawi | 19,617,945 | 1194 | 6,397,062 | 5358 | 0.33 |
| Mali | 20,826,158 | 525 | 953,852 | 1817 | 0.05 |
| Mauritania | 4,770,294 | 487 | 3,849,297 | 7904 | 0.81 |
| Mauritius | 1,273,865 | 18 | 4,169,354 | 231,631 | 3.27 |
| Mozambique | 32,119,351 | 872 | 4,592,429 | 5267 | 0.14 |
| Namibia | 2,586,431 | 1445 | 72,902,503 | 50,452 | 28.19 |
| Niger | 25,069,087 | 193 | 262,578 | 1361 | 0.01 |
| Nigeria | 211,184,869 | 2120 | 3,996,746 | 1885 | 0.02 |
| Rwanda | 13,269,271 | 431 | 7,523,452 | 17,456 | 0.57 |
| São Tomé and Príncipe | 223,185 | 37 | 378,869 | 10,240 | 1.70 |
| Senegal | 17,179,451 | 1166 | 8,699,508 | 7461 | 0.51 |
| Seychelles | 98,951 | 68 | 16,916,076 | 248,766 | 170.95 |
| Sierra Leone | 8,137,375 | 98 | 56,817 | 580 | 0.01 |
| South Africa | 60,049,601 | 60,264 | 3,739,829,800 | 62,057 | 62.28 |
| South Sudan | 11,323,788 | 117 | 335,752 | 2870 | 0.03 |
| Swaziland | 1,172,073 | 678 | 23,916,056 | 35,274 | 20.40 |
| Tanzania | 61,412,589 | 21 | 351,667 | 16,746 | 0.01 |
| Togo | 8,470,400 | 129 | 157,661 | 1222 | 0.02 |
| Uganda | 47,164,701 | 989 | 13,032,941 | 13,178 | 0.28 |
| Zambia | 18,891,903 | 2138 | 35,519,279 | 16,613 | 1.88 |
| Zimbabwe | 15,077,192 | 1761 | 20,034,980 | 11,377 | 1.33 |
| Djibouti | 1,002,228 | 155 | 1,504,127 | 9704 | 1.50 |
| Egypt | 104,243,582 | 16,148 | 714,752,930 | 44,263 | 6.86 |
| Libya | 6,963,848 | 3191 | 94,931,967 | 29,750 | 13.63 |
| Morocco | 37,344,128 | 9292 | 428,373,900 | 46,101 | 11.47 |
| Somalia | 16,330,692 | 775 | 347,169 | 448 | 0.02 |
| Sudan | 44,860,676 | 2754 | 13,457,222 | 4886 | 0.30 |
| Tunisia | 11,941,219 | 14,843 | 845,216,224 | 56,944 | 70.78 |
| TOTAL | 1,370,493,279 | 142,171 | 6,684,101,196 | 47,015 | 4.88 |
| Country | (A). COVID-19 Deaths 2021 * | (B). Total Monetary Value of Lives Lost to COVID-19 (Int$) *** | (C). Labor Force Participation Rate for Ages 15–64 (%) ** | (D). To Indirect Cost (Int$) [D = Bx(C/100)] *** | (E). Average Indirect Cost [E = (D/A)] *** |
|---|---|---|---|---|---|
| Algeria | 684 | 109,107,102 | 46.4 | 50,625,695 | 74,040 |
| Angola | 486 | 27,554,096 | 77.9 | 21,464,641 | 44,176 |
| Benin | 19 | 342,422 | 71.7 | 245,517 | 12,802 |
| Botswana | 611 | 133,347,604 | 73.0 | 97,343,751 | 159,205 |
| Burkina Faso | 31 | 360,381 | 67.8 | 244,338 | 7887 |
| Burundi | 4 | 26,455 | 80.0 | 21,164 | 4868 |
| Cameroon | 244 | 3,121,502 | 76.9 | 2,400,435 | 9832 |
| Cape Verde | 53 | 4,694,663 | 63.9 | 2,999,890 | 56,882 |
| Central African Rep | 18 | 13,977 | 72.3 | 10,106 | 559 |
| Chad | 32 | 98,344 | 70.7 | 69,529 | 2167 |
| Comoros | 79 | 2,329,866 | 46.6 | 1,085,718 | 13,682 |
| Congo | 30 | 844,274 | 70.3 | 593,524 | 19,507 |
| Cote d’Ivoire | 58 | 977,392 | 54.6 | 533,656 | 9246 |
| DRC | 502 | 3,871,323 | 64.1 | 2,481,518 | 4941 |
| Equatorial Guinea | 22 | 1,351,863 | 63.2 | 854,378 | 38,291 |
| Eritrea | 4 | 62,991 | 81.3 | 51,212 | 12,075 |
| Ethiopia | 797 | 19,419,954 | 81.3 | 15,788,423 | 19,819 |
| Gabon | 29 | 3,831,028 | 54.7 | 2,095,572 | 71,473 |
| Gambia The | 33 | 387,034 | 60.5 | 234,155 | 7016 |
| Ghana | 147 | 5,642,699 | 69.2 | 3,904,748 | 26,636 |
| Guinea | 31 | 402,426 | 63.0 | 253,528 | 8135 |
| Guinea Bissau | 13 | 95,658 | 72.9 | 69,735 | 5481 |
| Kenya | 1968 | 110,454,961 | 74.6 | 82,399,401 | 41,869 |
| Lesotho | 179 | 2,244,799 | 69.9 | 1,569,114 | 8775 |
| Liberia | 23 | 239,148 | 77.1 | 184,383 | 7873 |
| Madagascar | 495 | 9,675,527 | 87.2 | 8,437,060 | 17,040 |
| Malawi | 649 | 6,212,044 | 77.3 | 4,801,910 | 7400 |
| Mali | 97 | 944,317 | 71.3 | 673,298 | 6955 |
| Mauritania | 90 | 3,827,676 | 46.5 | 1,779,869 | 19,820 |
| Mauritius | 10 | 3,467,754 | 66.2 | 2,295,653 | 234,657 |
| Mozambique | 474 | 4,422,875 | 78.3 | 3,463,111 | 7307 |
| Namibia | 785 | 70,668,214 | 60.6 | 42,824,938 | 54,529 |
| Niger | 36 | 260,749 | 73.4 | 191,390 | 5378 |
| Nigeria | 391 | 3,922,315 | 56.7 | 2,223,953 | 5689 |
| South Sudan | 64 | 320,264 | 73.8 | 236,355 | 3717 |
| Rwanda | 234 | 6,987,929 | 84.1 | 5,876,849 | 25,088 |
| Sao Tome et Principe | 7 | 281,197 | 59.9 | 168,437 | 24,687 |
| Senegal | 215 | 7,213,397 | 47.1 | 3,397,510 | 15,802 |
| Seychelles | 37 | 14,790,765 | 66.6 | 9,849,170 | 266,496 |
| Sierra Leone | 18 | 55,759 | 58.8 | 32,786 | 1814 |
| South Africa | 32,753 | 3,625,212,884 | 60.1 | 2,178,752,943 | 66,520 |
| Swaziland (Eswatini) | 368 | 22,951,859 | 54.7 | 12,554,667 | 34,070 |
| Tanzania | 11 | 341,496 | 84.5 | 288,564 | 25,283 |
| Togo | 24 | 156,146 | 58.5 | 91,346 | 3840 |
| Uganda | 538 | 12,607,006 | 70.9 | 8,938,367 | 16,629 |
| Zambia | 1162 | 34,430,697 | 75.1 | 25,857,454 | 22,252 |
| Zimbabwe | 957 | 19,295,282 | 84.0 | 16,208,037 | 16,934 |
| Djibouti | 29 | 1,348,824 | 63.7 | 859,201 | 30,061 |
| Egypt | 2978 | 460,883,696 | 47.9 | 220,763,290 | 74,139 |
| Libya | 588 | 61,213,594 | 52.8 | 32,320,778 | 54,928 |
| Morocco | 1713 | 188,853,193 | 48.7 | 91,971,505 | 53,676 |
| Somalia | 143 | 342,073 | 49.4 | 168,984 | 1182 |
| Sudan | 508 | 13,381,636 | 49.7 | 6,650,673 | 13,096 |
| Tunisia | 2737 | 396,784,269 | 51.5 | 204,343,899 | 74,658 |
| TOTAL (Int$) | 54,210 | 5,401,675,398 | 3,173,546,125 | 58,542 |
| Country | (A) Total COVID-19 Cases * | (B) Current Health Expenditure per Capita in 2021 (Int$) ** | (C) Direct Cost (Int$) [C = A × B)] *** |
|---|---|---|---|
| Algeria | 139,229 | 940 | 130,934,190 |
| Angola | 38,682 | 115 | 4,448,923 |
| Benin | 8199 | 85 | 700,219 |
| Botswana | 69,680 | 1082 | 75,380,140 |
| Burkina Faso | 13,479 | 73 | 977,779 |
| Burundi | 5428 | 89 | 485,399 |
| Cabo Verde | 32,457 | 481 | 15,617,354 |
| Cameroon | 80,858 | 154 | 12,492,030 |
| Central African Republic | 7141 | 540 | 3,855,622 |
| Chad | 4951 | 62 | 306,781 |
| Comoros | 3912 | 144 | 562,929 |
| Congo | 12,596 | 51 | 643,920 |
| Djibouti | 11,602 | 136 | 1,580,972 |
| DRC | 40,836 | 18 | 720,805 |
| Egypt | 281,031 | 491 | 138,124,544 |
| Equatorial Guinea | 8734 | 585 | 5,105,836 |
| Eritrea | 5936 | 139 | 823,562 |
| Eswatini | 19,084 | 659 | 12,581,054 |
| Ethiopia | 276,037 | 70 | 19,349,040 |
| Gabon | 24,984 | 482 | 12,034,455 |
| Gambia | 6079 | 76 | 464,312 |
| Ghana | 95,642 | 244 | 23,291,505 |
| Guinea | 23,753 | 138 | 3,272,720 |
| Guinea-Bissau | 3853 | 137 | 529,337 |
| Cote d’Ivoire (Ivory Coast) | 48,242 | 181 | 8,746,361 |
| Kenya | 183,603 | 263 | 48,349,428 |
| Lesotho | 11,344 | 399 | 4,529,139 |
| Liberia | 3900 | 59 | 230,223 |
| Libya | 193,238 | 8 | 1,559,041 |
| Madagascar | 42,207 | 60 | 2,518,105 |
| Malawi | 35,897 | 115 | 4,133,405 |
| Mali | 14,422 | 87 | 1,248,415 |
| Mauritania | 20,747 | 219 | 4,553,581 |
| Mauritius | 1833 | 1741 | 3,190,929 |
| Morocco | 530,585 | 560 | 297,383,335 |
| Mozambique | 75,828 | 143 | 10,815,752 |
| Namibia | 86,649 | 778 | 67,442,498 |
| Niger | 5488 | 79 | 434,235 |
| Nigeria | 167,543 | 273 | 45,673,668 |
| Rwanda | 38,198 | 279 | 10,639,375 |
| São Tomé and Príncipe | 2366 | 215 | 507,569 |
| Senegal | 42,957 | 156 | 6,702,574 |
| Seychelles | 15,579 | 1922 | 29,950,243 |
| Sierra Leone | 5495 | 264 | 1,447,951 |
| Somalia | 14,933 | 30 | 447,990 |
| South Africa | 1,954,466 | 1256 | 2,454,780,059 |
| South Sudan | 10,834 | 52 | 561,673 |
| Sudan | 36,658 | 243 | 8,922,926 |
| Tanzania | 509 | 123 | 62,703 |
| Togo | 13,881 | 137 | 1,899,448 |
| Tunisia | 414,182 | 1036 | 429,152,254 |
| Uganda | 79,434 | 163 | 12,932,700 |
| Zambia | 152,056 | 324 | 49,332,595 |
| Zimbabwe | 48,533 | 196 | 9,495,444 |
| TOTAL | 5,465,790 | 3,981,927,049 |
| Country | Total Cost | Total Cost per COVID-19 Case (Int$) | Total Cost per Person in Population (Int$) |
|---|---|---|---|
| Algeria | 181,559,885 | 1304 | 4.07 |
| Angola | 25,913,564 | 670 | 0.76 |
| Benin | 945,736 | 115 | 0.08 |
| Botswana | 172,723,891 | 2479 | 72.01 |
| Burkina Faso | 1,222,117 | 91 | 0.06 |
| Burundi | 506,563 | 93 | 0.04 |
| Cameroon | 14,892,465 | 184 | 0.55 |
| Cape Verde | 18,617,243 | 574 | 33.13 |
| Central African Republic | 3,865,727 | 541 | 0.79 |
| Chad | 376,311 | 76 | 0.02 |
| Comoros | 1,648,647 | 421 | 1.86 |
| Congo, Republic of | 1,237,444 | 98 | 0.22 |
| Cote d’Ivoire | 9,280,016 | 192 | 0.34 |
| Congo, Democratic Republic of | 3,202,323 | 78 | 0.03 |
| Equatorial Guinea | 5,960,214 | 682 | 4.12 |
| Eritrea | 874,774 | 147 | 0.24 |
| Ethiopia | 35,137,463 | 127 | 0.30 |
| Gabon | 14,130,028 | 566 | 6.20 |
| Gambia, The | 698,467 | 115 | 0.28 |
| Ghana | 27,196,253 | 284 | 0.86 |
| Guinea | 3,526,248 | 148 | 0.26 |
| Guinea-Bissau | 599,072 | 155 | 0.30 |
| Kenya | 130,748,829 | 712 | 2.38 |
| Lesotho | 6,098,253 | 538 | 2.82 |
| Liberia | 414,606 | 106 | 0.08 |
| Madagascar | 10,955,165 | 260 | 0.39 |
| Malawi | 8,935,316 | 249 | 0.46 |
| Mali | 1,921,713 | 133 | 0.09 |
| Mauritania | 6,333,451 | 305 | 1.33 |
| Mauritius | 5,486,582 | 2993 | 4.31 |
| Mozambique | 14,278,863 | 188 | 0.44 |
| Namibia | 110,267,435 | 1273 | 42.63 |
| Niger | 625,625 | 114 | 0.02 |
| Nigeria | 47,897,621 | 286 | 0.23 |
| Rwanda | 16,516,224 | 432 | 1.24 |
| Sao Tome and Principe | 676,006 | 286 | 3.03 |
| Senegal | 10,100,085 | 235 | 0.59 |
| Seychelles | 39,799,413 | 2555 | 402.21 |
| Sierra Leone | 1,480,738 | 269 | 0.18 |
| South Africa | 4,633,533,002 | 2371 | 77.16 |
| South Sudan | 798,028 | 74 | 0.07 |
| Swaziland | 25,135,720 | 1317 | 21.45 |
| Tanzania | 351,267 | 690 | 0.01 |
| Togo | 1,990,794 | 143 | 0.24 |
| Uganda | 21,871,067 | 275 | 0.46 |
| Zambia | 75,190,049 | 494 | 3.98 |
| Zimbabwe | 25,703,481 | 530 | 1.70 |
| Djibouti | 2,440,173 | 210 | 2.43 |
| Egypt | 358,887,834 | 1277 | 3.44 |
| Libya | 33,879,818 | 175 | 4.87 |
| Morocco | 389,354,840 | 734 | 10.43 |
| Somalia | 616,974 | 41 | 0.04 |
| Sudan | 15,573,599 | 425 | 0.35 |
| Tunisia | 633,496,153 | 1530 | 53.05 |
| TOTAL (Int$) | 7,155,473,174 | 1309 | 5.22 |
| Country | Control Group Direct Cost (Int$) | Vaccine Group Direct Cost (Int$) |
|---|---|---|
| Algeria | 1,213,130,315 | 410,134,248 |
| Angola | 112,596,891 | 38,066,678 |
| Benin | 30,696,569 | 10,377,875 |
| Botswana | 74,992,194 | 25,353,308 |
| Burkina Faso | 45,009,650 | 15,216,831 |
| Burundi | 31,634,010 | 10,694,804 |
| Cameroon | 121,441,348 | 41,056,806 |
| Cape Verde | 7,814,988 | 2,642,086 |
| Central African Republic | 76,662,647 | 25,918,054 |
| Chad | 30,248,209 | 10,226,293 |
| Comoros | 3,692,648 | 1,248,408 |
| Congo, Republic of | 8,350,869 | 2,823,256 |
| Cote d’Ivoire | 141,597,107 | 47,871,051 |
| Congo, Democratic Republic of | 47,058,206 | 15,909,405 |
| Equatorial Guinea | 24,471,172 | 8,273,197 |
| Eritrea | 14,415,171 | 4,873,471 |
| Ethiopia | 238,595,019 | 80,664,037 |
| Gabon | 31,707,221 | 10,719,555 |
| Gambia, The | 5,482,538 | 1,853,533 |
| Ghana | 223,211,109 | 75,463,056 |
| Guinea | 53,694,939 | 18,153,147 |
| Guinea-Bissau | 7,996,421 | 2,703,424 |
| Kenya | 418,146,512 | 141,366,680 |
| Lesotho | 24,913,510 | 8,422,742 |
| Liberia | 8,829,117 | 2,984,942 |
| Madagascar | 48,958,347 | 16,551,804 |
| Malawi | 65,285,562 | 22,071,697 |
| Mali | 52,102,243 | 17,614,690 |
| Mauritania | 30,259,150 | 10,229,992 |
| Mauritius | 64,090,232 | 21,667,581 |
| Mozambique | 132,405,996 | 44,763,727 |
| Namibia | 58,181,480 | 19,669,954 |
| Niger | 57,327,529 | 19,381,251 |
| Nigeria | 1,663,857,712 | 562,515,851 |
| Rwanda | 106,816,010 | 36,112,282 |
| Sao Tome and Principe | 1,383,754 | 467,819 |
| Senegal | 77,469,502 | 26,190,835 |
| Seychelles | 5,497,873 | 1,858,717 |
| Sierra Leone | 61,970,418 | 20,950,916 |
| South Africa | 483,391,950 | 163,424,812 |
| South Sudan | 16,966,806 | 5,736,126 |
| Swaziland | 22,331,405 | 7,549,786 |
| Tanzania | 218,647,124 | 73,920,067 |
| Togo | 33,498,430 | 11,325,126 |
| Uganda | 221,928,779 | 75,029,526 |
| Zambia | 177,141,323 | 59,887,815 |
| Zimbabwe | 85,253,530 | 28,822,454 |
| Djibouti | 3,947,041 | 1,334,413 |
| Egypt | 1,480,743,156 | 500,608,610 |
| Libya | 1,623,783 | 548,967 |
| Morocco | 604,919,747 | 204,510,845 |
| Somalia | 14,159,230 | 4,786,942 |
| Sudan | 315,586,269 | 106,693,185 |
| Tunisia | 357,587,739 | 120,893,013 |
| Country | Direct Cost Savings (Int$) | Indirect Cost Savings (Int$) | Total Cost Savings (Int$) |
|---|---|---|---|
| Algeria | 802,996,067 | 1,909,014,416 | 2,712,010,483 |
| Angola | 74,530,213 | 2,547,771,063 | 2,622,301,276 |
| Benin | 20,318,695 | 91,972,651 | 112,291,346 |
| Botswana | 49,638,885 | 650,154,625 | 699,793,511 |
| Burkina Faso | 29,792,819 | 97,813,488 | 127,606,307 |
| Burundi | 20,939,206 | 101,436,938 | 122,376,144 |
| Cameroon | 80,384,542 | 154,472,902 | 234,857,444 |
| Cape Verde | 5,172,902 | 18,465,553 | 23,638,455 |
| Central African Republic | 50,744,593 | 1,587,020 | 52,331,613 |
| Chad | 20,021,916 | 21,143,503 | 41,165,418 |
| Comoros | 2,444,240 | 20,684,314 | 23,128,555 |
| Congo, Republic of | 5,527,613 | 63,691,418 | 69,219,031 |
| Cote d’Ivoire | 93,726,056 | 144,332,155 | 238,058,211 |
| Democratic Republic of Congo | 31,148,801 | 776,068,275 | 807,217,076 |
| Equatorial Guinea | 16,197,975 | 32,037,564 | 48,235,539 |
| Eritrea | 9,541,700 | 25,075,786 | 34,617,486 |
| Ethiopia | 157,930,982 | 1,348,397,948 | 1,506,328,931 |
| Gabon | 20,987,666 | 94,035,774 | 115,023,440 |
| Gambia | 3,629,006 | 10,065,227 | 13,694,232 |
| Ghana | 147,748,054 | 487,962,646 | 635,710,699 |
| Guinea | 35,541,792 | 63,368,970 | 98,910,762 |
| Guinea-Bissau | 5,292,997 | 6,376,107 | 11,669,104 |
| Kenya | 276,779,832 | 3,916,573,442 | 4,193,353,274 |
| Lesotho | 16,490,768 | 32,258,045 | 48,748,812 |
| Liberia | 5,844,176 | 23,536,632 | 29,380,808 |
| Madagascar | 32,406,543 | 823,766,172 | 856,172,715 |
| Malawi | 43,213,865 | 247,155,826 | 290,369,691 |
| Mali | 34,487,553 | 83,669,035 | 118,156,588 |
| Mauritania | 20,029,157 | 54,615,001 | 74,644,159 |
| Mauritius | 42,422,651 | 508,937,955 | 551,360,606 |
| Mozambique | 87,642,270 | 399,598,914 | 487,241,184 |
| Namibia | 38,511,526 | 240,125,016 | 278,636,543 |
| Niger | 37,946,278 | 77,876,604 | 115,822,882 |
| Nigeria | 1,101,341,861 | 694,000,964 | 1,795,342,825 |
| Rwanda | 70,703,728 | 566,789,645 | 637,493,373 |
| São Tomé and Principe | 915,936 | 3,182,788 | 4,098,724 |
| Senegal | 51,278,667 | 156,811,935 | 208,090,601 |
| Seychelles | 3,639,156 | 44,897,125 | 48,536,282 |
| Sierra Leone | 41,019,502 | 8,528,268 | 49,547,771 |
| South Africa | 319,967,138 | 6,800,921,734 | 7,120,888,872 |
| South Sudan | 11,230,680 | 71,660,149 | 82,890,829 |
| Swaziland | 14,781,619 | 67,988,862 | 82,770,481 |
| Tanzania | 144,727,057 | 2,643,552,220 | 2,788,279,277 |
| Togo | 22,173,304 | 18,789,271 | 40,962,575 |
| Uganda | 146,899,253 | 1,335,323,816 | 1,482,223,069 |
| Zambia | 117,253,509 | 715,750,036 | 833,003,545 |
| Zimbabwe | 56,431,076 | 434,709,514 | 491,140,591 |
| Djibouti | 2,612,628 | 17,403,517 | 20,016,146 |
| Egypt | 980,134,546 | 4,464,420,175 | 5,444,554,721 |
| Libya | 1,074,816 | 220,959,103 | 222,033,918 |
| Morocco | 400,408,902 | 1,157,907,945 | 1,558,316,848 |
| Somalia | 9,372,287 | 11,154,672 | 20,526,959 |
| Sudan | 208,893,084 | 339,371,278 | 548,264,362 |
| Tunisia | 236,694,727 | 514,987,003 | 751,681,730 |
| TOTAL | 6,261,584,816 | 35,363,151,009 | 41,624,735,824 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kirigia, J.M.; Mwabu, G. The Monetary Value of Human Life Losses Associated with COVID-19 in Africa: A Human Capital Approach. Economies 2025, 13, 241. https://doi.org/10.3390/economies13080241
Kirigia JM, Mwabu G. The Monetary Value of Human Life Losses Associated with COVID-19 in Africa: A Human Capital Approach. Economies. 2025; 13(8):241. https://doi.org/10.3390/economies13080241
Chicago/Turabian StyleKirigia, Joses Muthuri, and Germano Mwabu. 2025. "The Monetary Value of Human Life Losses Associated with COVID-19 in Africa: A Human Capital Approach" Economies 13, no. 8: 241. https://doi.org/10.3390/economies13080241
APA StyleKirigia, J. M., & Mwabu, G. (2025). The Monetary Value of Human Life Losses Associated with COVID-19 in Africa: A Human Capital Approach. Economies, 13(8), 241. https://doi.org/10.3390/economies13080241






