Handwashing and Household Health Expenditures Under COVID-19: Evidence from Cameroon
Abstract
1. Introduction
2. Methodology
2.1. Theoretical Background
2.2. Method
2.2.1. The Use of a Handwashing Device
2.2.2. Effect of Handwashing Device Use on Healthcare Expenditures
2.3. Data and Summary Statistics
2.4. Description of Variables
3. Results
3.1. The Probability of Using a Handwashing Device
3.2. Handwashing and Healthcare Expenditures
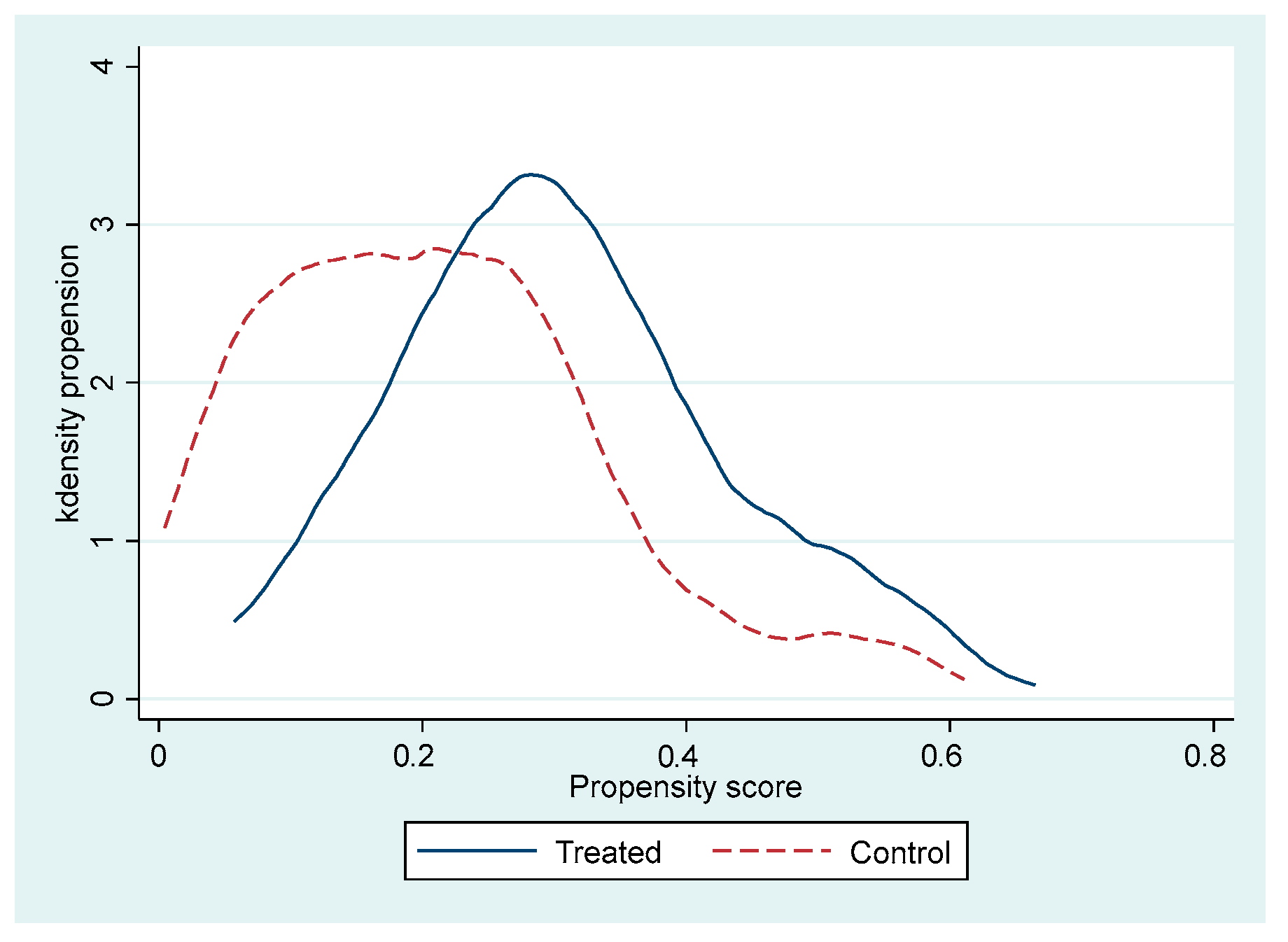
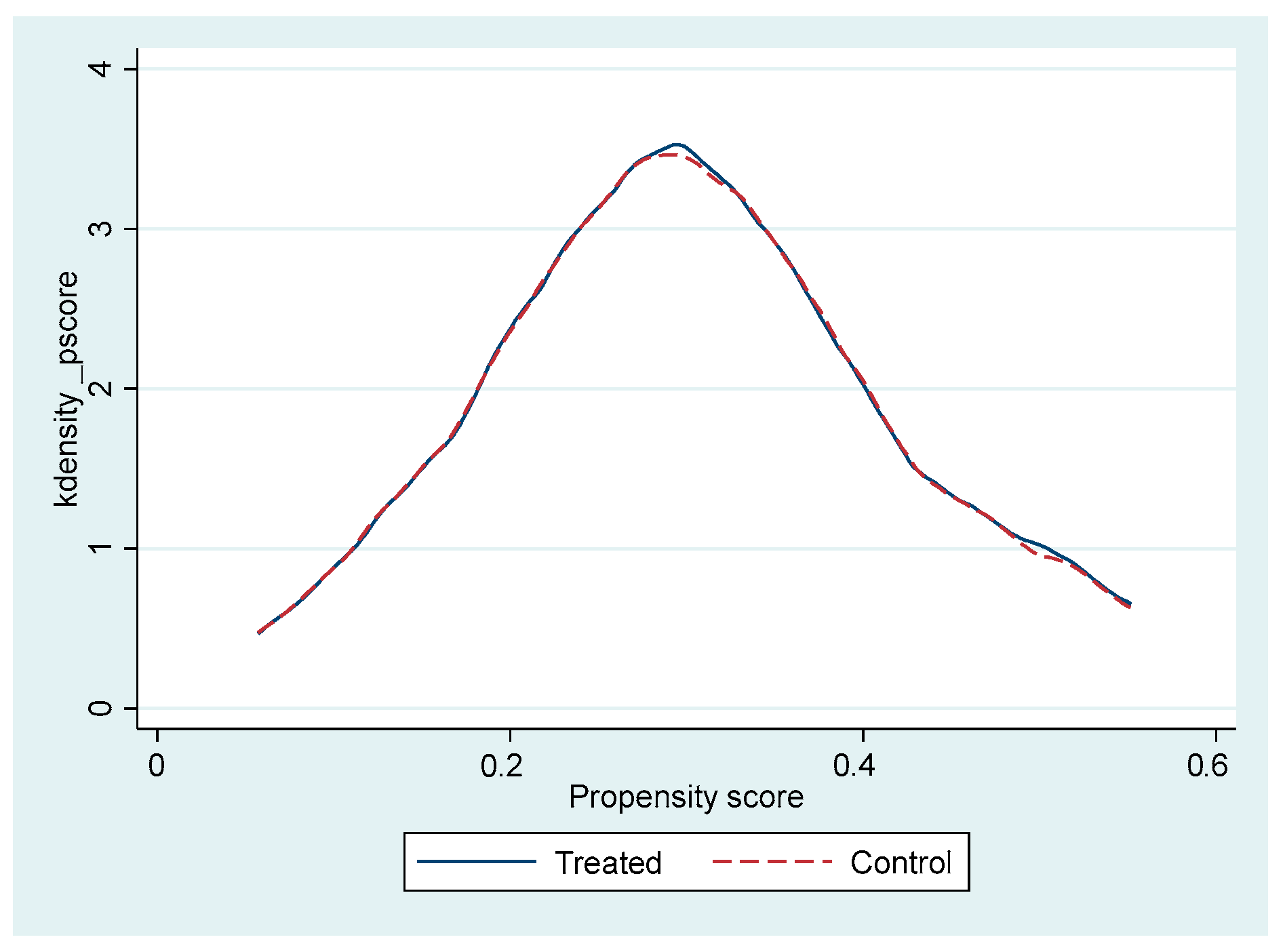
3.3. Robustness
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ESR | Endogenous Switching Regression |
| PSM | Propensity Score Matching |
| IPWRA | Inverse Probability Weighted Regression Adjustment |
Appendix A
| Variables | Used a Handwashing Device |
|---|---|
| Region (Centre) | 0.571 (2.39) ** |
| Place of residence (Rural) | −1.313 (4.07) *** |
| Household size | 0.054 (1.46) |
| Age of HH | 0.123 (2.02) ** |
| Age of HH squared | −0.097 (1.58) |
| Gender of HH (Female) | 0.122 (0.36) |
| Educational level | |
| Primary | 1.423 (1.33) |
| Secondary | 1.568 (1.49) |
| Higher | 1.408 (1.30) |
| Marital status (In couple) | 0.066 (0.20) |
| Religion (Catholic) | −0.251 (1.14) |
| Sector of activity | |
| Public/Association | 0.443 (1.15) |
| Formal Private | 0.235 (0.70) |
| Informal private | −0.138 (0.48) |
| Test COVID-19 | −0.060 (0.23) |
| Using social networks | 0.442 (1.70) * |
| Knowledge of barrier measures | −0.036 (0.75) |
| Constant | −6.594 (3.72) *** |
| LR chi2(17) | 59.04 *** |
| Observations | 560 |
| Variables | OME0 | OME1 | TME1 |
|---|---|---|---|
| Region (Centre) | 0.028 (0.17) | −0.173 (0.81) | 0.681 (2.61) *** |
| Place of residence (Rural) | −0.161 (0.87) | −0.200 (0.70) | −1.585 (4.09) *** |
| Household size | 0.066 (3.06) *** | 0.055 (1.61) | 0.076 (1.77) * |
| Age of HH | 0.051 (1.41) | 0.092 (1.43) | 0.138 (2.05) ** |
| Age of HH squared | −0.039 (1.06) | −0.091 (1.46) | −0.115 (1.67) * |
| Gender of HH (Female) | −0.004 (0.02) | −0.083 (0.33) | 0.146 (0.42) |
| Educational level | |||
| Primary | −0.162 (0.36) | 0.707 (1.78) * | 1.459 (1.37) |
| Secondary | 0.173 (0.42) | 1.127 (3.13) *** | 1.706 (1.64) |
| Higher | 0.613 (1.34) | 1.846 (4.86) *** | 1.463 (1.33) |
| Marital status (In couple) | 0.267 (1.36) | 0.265 (1.03) | 0.022 (0.06) |
| Religion (Catholic) | −0.149 (0.89) | 0.202 (1.05) | −0.179 (0.71) |
| Sector of activity | |||
| Public/Association | −0.011 (0.05) | −0.782 (2.45) ** | 0.553 (1.25) |
| Formal Private | 0.070 (0.27) | −0.390 (1.24) | 0.057 (0.16) |
| Informal private | −0.248 (1.26) | −0.572 (2.34) ** | −0.135 (0.43) |
| Test COVID-19 | 0.216 (1.03) | 0.289 (1.37) | −0.326 (1.02) |
| Using social networks | 0.549 (1.85) * | ||
| Knowledge of barrier measures | −0.123 (2.33) ** | ||
| Constant | 7.389 (7.68) *** | 6.073 (3.56) *** | −6.462 (3.62) *** |
| Observations | 422 | ||
References
- Abdulai, A., & Huffman, W. (2014). The adoption and impact of soil and water conservation technology: An endogenous switching regression application. Land Economics, 90(1), 26–43. [Google Scholar] [CrossRef]
- Acton, J. P. (1975). Nonmonetary factors in the demand for medical services: Some empirical evidence. Journal of Political Economy, 83(3), 595. [Google Scholar] [CrossRef]
- Ajzen, I. (1991). The theory of planned behaviour. Organizational Behavior and Human Decision Processes, 50, 179–211. [Google Scholar] [CrossRef]
- Azor-Martínez, E., Gonzalez-Jimenez, Y., Seijas-Vazquez, M. L., Cobos-Carrascosa, E., Santisteban-Martínez, J., Martínez-López, J. M., Jimenez-Noguera, E., Galan-Requena, M. D. M., Garrido-Fernández, P., Strizzi, J. M., & Gimenez-Sanchez, F. (2014). The impact of common infections on school absenteeism during an academic year. American Journal of Infection Control, 42(6), 632–637. [Google Scholar] [CrossRef]
- Bowen, A., Ma, H., Ou, J., Billhimer, W., Long, T., Mintz, E., Hoekstra, R. M., & Luby, S. (2007). A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. American Journal of Tropical Medicine and Hygiene, 76(6), 1166–1173. [Google Scholar] [CrossRef]
- Brauer, M., Zhao, J. T., Bennitt, F. B., & Stanaway, J. D. (2020). Global access to handwashing: Implications for COVID-19 control in low-income countries. Environmental Health Perspectives, 128(5), 057005. [Google Scholar] [CrossRef]
- Cochran, W. G. (1977). Sampling techniques (3rd ed.). John Wiley & Sons. [Google Scholar]
- Cohen, D. R. (1984). Utility model of preventive behaviour. Journal of Epidemiology & Community Health, 38(1), 61–65. [Google Scholar]
- Crémieux, P. Y., Ouellette, P., & Pilon, C. (1999). Health care spending as determinants of health outcomes. Health Economics, 8(7), 627–639. [Google Scholar] [CrossRef]
- Curtis, V., & Cairncross, S. (2003). Effect of washing hands with soap on diarrhoea risk in the community: A systematic review. Lancet Infectious Diseases, 3(5), 275–281. [Google Scholar] [CrossRef]
- Deri, C. (2005). Social networks and health service utilization. Journal of Health Economics, 24(6), 1076–1107. [Google Scholar] [CrossRef] [PubMed]
- Di Falco, S., Veronesi, M., & Yesuf, M. (2011). Does adaptation to climate change provide food security? A micro-perspective from Ethiopia. American Journal of Agricultural Economics, 93(3), 829–846. [Google Scholar] [CrossRef]
- Dreibelbis, R., Kroeger, A., Hossain, K., Venkatesh, M., & Ram, P. K. (2016). Behavior change without behavior change communication: Nudging handwashing among primary school students in Bangladesh. International Journal of Environmental Research and Public Health, 13(1), 129. [Google Scholar] [CrossRef]
- Ejemot-Nwadiaro, R. I., Ehiri, J. E., Arikpo, D., Meremikwu, M. M., & Critchley, J. A. (2021). Hand-washing promotion for preventing diarrhoea. The Cochrane Database of Systematic Reviews, 12(1), CD004265. [Google Scholar] [CrossRef]
- Fu, X., Mohnen, P., & Zanello, G. (2018). Innovation and productivity in formal and informal firms in Ghana. Technological Forecasting and Social Change, 131, 315–325. [Google Scholar] [CrossRef]
- Godoy, P., Castilla, J., Delgado-Rodríguez, M., Martín, V., Soldevila, N., Alonso, J., Astray, J., Baricot, M., Cantón, R., Castro, A., González-Candelas, F., Mayoral, J. M., Quintana, J. M., Pumarola, T., Tamames, S., Domínguez, A., Azor, E., Carrillo, J., Moyano, R., … Alustizac, J. (2012). Effectiveness of hand hygiene and provision of information in preventing influenza cases requiring hospitalization. Preventive Medicine, 54(6), 434–439. [Google Scholar] [CrossRef]
- Gozdzielewska, L., Kilpatrick, C., Reilly, J., Stewart, S., Butcher, J., Kalule, A., Cumming, O., Watson, J., & Price, L. (2022). The effectiveness of hand hygiene interventions for preventing community transmission or acquisition of novel coronavirus or influenza infections: A systematic review. BMC Public Health, 22(1), 1283. [Google Scholar] [CrossRef]
- Grossman, M. (1972). On the concept of health capital and the demand for health. Journal of Political Economy, 80(2), 223–255. [Google Scholar] [CrossRef]
- Heckman, J., Tobias, J. L., & Vytlacil, E. (2001). Four parameters of interest in the evaluation of social programs. Southern Economic Journal, 68(2), 210–223. [Google Scholar] [CrossRef] [PubMed]
- Jefferson, T., Del Mar, C. B., Dooley, L., Ferroni, E., Al-Ansary, L. A., Bawazeer, G. A., van Driel, M. L., Nair, N. S., Jones, M. A., Thorning, S., & Conly, J. M. (2011). Physical interventions to interrupt or reduce the spread of respiratory viruses. The Cochrane Database of Systematic Reviews, 2011(7), CD006207. [Google Scholar] [CrossRef] [PubMed]
- Kuwawenaruwa, A., Wyss, K., Wiedenmayer, K., Metta, E., & Tediosi, F. (2020). The effects of medicines availability and stock-outs on household’s utilization of healthcare services in Dodoma region, Tanzania. Health Policy and Planning, 35(3), 323–333. [Google Scholar] [CrossRef] [PubMed]
- Lee Ventola, C. (2014). Mobile devices and apps for health care professionals: Uses and benefits. Pharmacy and Therapeutics, 39(5), 356. [Google Scholar]
- Leonard, K. L. (2003). African traditional healers and outcome-contingent contracts for health care. Journal of Development Economics, 71(1), 1–22. [Google Scholar] [CrossRef][Green Version]
- Liu, M., Min, S., Ma, W., & Liu, T. (2021). The adoption and impact of E-commerce in rural China: Application of an endogenous switching regression model. Journal of Rural Studies, 83, 106–116. [Google Scholar] [CrossRef]
- Lokshin, M., & Sajaia, Z. (2004). Maximum likelihood estimation of endogenous switching regression models. The Stata Journal, 4(3), 282–289. [Google Scholar] [CrossRef]
- Luby, S. P., Agboatwalla, M., Feikin, D. R., Painter, J., Billhimer, W., Altaf, A., & Hoekstra, R. M. (2005). Effect of handwashing on child health: A randomised controlled trial. The Lancet, 366(9481), 225–233. [Google Scholar] [CrossRef] [PubMed]
- Maddala, G. S. (1983). Limited dependent and qualitative variables in econometrics. Cambridge University Press. [Google Scholar]
- Mbakaya, B. C., Lee, P. H., & Lee, R. L. T. (2017). Hand hygiene intervention strategies to reduce diarrhoea and respiratory infections among schoolchildren in developing countries: A systematic review. International Journal of Environmental Research and Public Health, 14(4), 371. [Google Scholar] [CrossRef] [PubMed]
- Moorhead, S. A., Hazlett, D. E., Harrison, L., Carroll, J. K., Irwin, A., & Hoving, C. (2013). A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. Journal of Medical Internet Research, 15(4), e85. [Google Scholar] [CrossRef] [PubMed]
- Mwabu, G. (1989). Nonmonetary factors in the household choice of health facilities. Economic Development and Cultural Change, 37(2), 383–392. [Google Scholar] [CrossRef]
- Mwabu, G. (2008). The demand for health care. In International Encyclopedia of Public Health (pp. 84–89). [Google Scholar] [CrossRef]
- Okunade, A. A., Suraratdecha, C., & Benson, D. A. (2010). Determinants of Thailand household healthcare expenditure: The relevance of permanant resources and other correlates. Health Economics, 19, 365–376. [Google Scholar] [CrossRef]
- Pfefferbaum, B., & North, C. S. (2020). Mental health and the COVID-19 pandemic. The New England Journal of Medicine, 383(6), 510–512. [Google Scholar] [CrossRef]
- Rabie, T., & Curtis, V. (2006). Handwashing and risk of respiratory infections: A quantitative systematic review. Tropical Medicine and International Health, 11(3), 258–267. [Google Scholar] [CrossRef]
- Rosenbaum, P. R., & Rubin, D. B. (1983). The central role of the propensity score in observational studies for causal effects. Biometrika, 70(1), 41–55. [Google Scholar] [CrossRef]
- Rosenzweig, M. R., & Schultz, T. P. (1983). Estimating a household production function: Heterogeneity, the demand for health inputs, and their effects on birth weight. Journal of Political Economy, 91(5), 723–746. [Google Scholar] [CrossRef]
- Saksena, P., Smith, T., & Tediosi, F. (2014). Inputs for universal health coverage: A methodological contribution to finding proxy indicators for financial hardship due to health expenditure. BMC Health Services Research, 14, 577. [Google Scholar] [CrossRef]
- Saunders-Hastings, P., Crispo, J. A. G., Sikora, L., & Krewski, D. (2017). Effectiveness of personal protective measures in reducing pandemic influenza transmission: A systematic review and meta-analysis. Epidemics, 20, 1–20. [Google Scholar] [CrossRef]
- Schneider, P., & Hanson, K. (2006). Horizontal equity in utilization of care and fairness of health financing: A comparison of micro-health insurance and user fees in Rwanda. Health Economics, 15(1), 19–31. [Google Scholar] [CrossRef]
- Sen, A. (2005). Is health care a luxury? New evidence from OECD data. International Journal of Health Care Finance and Economics, 5, 147–164. [Google Scholar] [CrossRef]
- Smith, S. M. S., Sonego, S., Wallen, G. R., Waterer, G., Cheng, A. C., & Thompson, P. (2015). Use of non-pharmaceutical interventions to reduce the transmission of influenza in adults: A systematic review. Respirology, 20(6), 896–903. [Google Scholar] [CrossRef]
- Takam-Fongang, G. M., Kamdem, C. B., & Kane, G. Q. (2019). Adoption and impact of improved maize varieties on maize yields: Evidence from central Cameroon. Review of Development Economics, 23(1), 172–188. [Google Scholar] [CrossRef]
- Wagstaff, A., & Van Doorslaer, E. (2000). Measuring and testing for inequity in the delivery of health care. The Journal of Human Resources, 35(4), 716–733. [Google Scholar] [CrossRef]
- Wagstaff, A., Paci, P., & van Doorslaer, E. (1991). On the measurement of inequalities in health. Social Science & Medicine, 33(5), 545–557. [Google Scholar] [CrossRef] [PubMed]
- White, S., Thorseth, A. H., Dreibelbis, R., & Curtis, V. (2020). The determinants of handwashing behaviour in domestic settings: An integrative systematic review. International Journal of Hygiene and Environmental Health, 227, 113512. [Google Scholar] [CrossRef] [PubMed]
- WHO & UNICEF. (2017). Progress on drinking-water, sanitation and hygiene: 2017 update and SDG baselines (Licence: CC BY-NC-SA 3.0 IGO). WHO. [Google Scholar]
- Wolf, J., Johnston, R., Freeman, M. C., Ram, P. K., Slaymaker, T., Laurenz, E., & Prüss-Ustün, A. (2019). Handwashing with soap after potential faecal contact: Global, regional and country estimates. International Journal of Epidemiology, 48(4), 1204–1218. [Google Scholar] [CrossRef]
- Xu, K., Evans, D. B., Kawabata, K., Zeramdini, R., Klavus, J., & Murray, C. (2003). Household catastrophic health expenditure: A multicountry analysis. The Lancet, 362, 111–117. [Google Scholar] [CrossRef]
| Expenditure Items | Before | During | ||||
|---|---|---|---|---|---|---|
| Mean | Min | Max. | Mean | Min | Max. | |
| Health expenditure | 23,532.266 | 0 | 650,000 | 28,958.936 | 0 | 420,500 |
| Consumption expenditure | 60,943.370 | 2500 | 550,000 | 48,878.942 | 2500 | 600,000 |
| Education expenditure | 142,763.862 | 0 | 1,500,000 | 104,308.511 | 0 | 1,500,000 |
| Other expenses | 20,073.570 | 1000 | 567,500 | 21,485.891 | 1000 | 1,646,000 |
| Overall expenditure | 232,710.659 | 7500 | 1,646,000 | 184,999.695 | 8500 | 1,713,000 |
| Variables | Description | Overall | With Handwashing Device | Without Handwashing Device | Difference ¥ |
|---|---|---|---|---|---|
| Used a hand-washing device | 1 if the household used the handwashing device; 0 else | 0.232 | - | - | - |
| (0.423) | |||||
| Health expenditure | Health expenditures during COVID-19 restrictions (in XAF) | 28,958.936 | 29,726.89 | 21,655.03 | −8071.86 ** |
| (40,008.91) | (45,842.85) | (36,138.38) | |||
| Region (Centre) | 1 if the household is in the Central region; 0 else | 0.487 | 0.592 | 0.456 | −0.136 *** |
| (0.500) | (0.493) | (0.499) | |||
| Place of residence (Rural) | 1 if the household is in rural area; 0 else | 0.250 | 0.108 | 0.293 | 0.185 *** |
| (0.433) | (0.311) | (0.456) | |||
| Household size | Number of persons living in the household | 6.030 | 6.692 | 5.83 | −0.862 *** |
| (3.005) | (3.082) | (2.955) | |||
| Characteristics of household’s head | |||||
| Age | Age of head of household in years | 45.607 | 48.369 | 44.772 | −3.597 *** |
| (13.604) | (13.251) | (13.614) | |||
| Gender (Female) | 1 if the head of household is a woman; 0 else | 0.302 | 0.292 | 0.305 | 0.0123 |
| (0.459) | (0.457) | (0.461) | |||
| Level of education (Primary) | 1 if the head of household has a Primary level; 0 else | 0.168 | 0.162 | 0.17 | 0.008 |
| (0.374) | (0.369) | (0.376) | |||
| Level of education (Secondary) | 1 if the head of household has a Secondary level; 0 else | 0.543 | 0.562 | 0.537 | −0.024 |
| (0.499) | (0.498) | (0.499) | |||
| Level of education (Higher) | 1 if the head of household has a higher level of education; 0 else | 0.241 | 0.269 | 0.233 | −0.037 |
| (0.428) | (0.445) | (0.423) | |||
| Marital status (Couple) | 1 if the head of household lives with a spouse; 0 else | 0.668 | 0.700 | 0.658 | −0.042 |
| (0.471) | (0.460) | (0.475) | |||
| Religion (Catholic) | 1 if the head of the household is from the Catholic religion; 0 else | 0.552 | 0.546 | 0.553 | 0.007 |
| (0.498) | (0.500) | (0.498) | |||
| Sector of activity (Public/Association) | 1 if the head of household works in the Public/Association sector; 0 else | 0.136 | 0.208 | 0.114 | −0.094 *** |
| (0.343) | (0.407) | (0.318) | |||
| Sector of activity (Formal Private) | 1 if the head of household works in the formal private sector; 0 else | 0.179 | 0.192 | 0.174 | −0.018 |
| (0.383) | (0.396) | (0.380) | |||
| Sector of activity (Informal private) | 1 if the head of household works in the informal private sector; 0 else | 0.382 | 0.300 | 0.407 | 0.107 ** |
| (0.486) | (0.46) | (0.492) | |||
| Test COVID-19 | 1 if at least one household member has performed the COVID-19 test: 0 else | 0.229 | 0.269 | 0.216 | −0.053 |
| (0.420) | (0.445) | (0.412) | |||
| Instruments | |||||
| Using social networks | 1 if the head of household uses social networks; 0 else | 0.577 | 0.631 | 0.56 | −0.070 * |
| (0.495) | (0.484) | (0.497) | |||
| Level of knowledge of measurements | Number of barrier measures known by the head of household | 4.984 | 4.877 | 5.016 | 0.139 |
| (2.311) | (2.157) | (2.357) | |||
| Variables | Possessed a Handwashing Device (1) | Health Expenditure | |
|---|---|---|---|
| Non-Owner (2) | Owner (3) | ||
| Region (Centre) | 0.405 (−0.15) *** | −0.288 (−0.168) * | −0.249 (−0.239) |
| Place of residence (Rural) | −0.855 (−0.199) *** | 0.292 (−0.210) | −0.051 (−0.347) |
| Household size | 0.036 (−0.024) | 0.065 (−0.025) *** | 0.048 (−0.036) |
| Age of HH | 0.084 (−0.037) ** | −0.031 (−0.039) | 0.079 (−0.068) |
| Age of HH squared | −0.069 (−0.038) * | 0.042 (−0.039) | −0.079 (−0.065) |
| Gender of HH (Female) | 0.050 (−0.186) | 0.214 (−0.200) | −0.093 (−0.257) |
| Educational level | |||
| Primary | 0.225 (−0.483) | 0.061 (−0.347) | 0.644 (−0.413) |
| Secondary | 0.441 (−0.438) | 0.342 (−0.293) | 1.007 (−0.379) *** |
| Higher | 0.283 (−0.471) | 0.747 (−0.336) ** | 1.740 (−0.393) *** |
| Marital status (in couple) | −0.0591 (−0.199) | 0.521 (−0.206) ** | 0.259 (−0.264) |
| Religion (Catholic) | −0.114 (−0.144) | 0.062 (−0.152) | 0.223 (−0.197) |
| Sector of activity | |||
| Public/Association | 0.379 (−0.243) | −0.247 (−0.281) | −0.825 (−0.330) ** |
| Formal Private | 0.046 (−0.202) | −0.077 (−0.229) | −0.383 (−0.316) |
| Informal private | −0.056 (−0.185) | −0.118 (−0.178) | −0.554 (−0.244) ** |
| Test COVID-19 | −0.28 (−0.2) | 0.502 (−0.193) *** | 0.331 (−0.217) |
| Using social networks | 0.404 (−0.145) *** | ||
| Knowledge of barrier measures | −0.053 (−0.028) * | ||
| Constant | −3.417 (−1.008) *** | 8.241 (−0.956) *** | 6.879 (−2.016) *** |
| lns0 | 0.272 (−0.095) *** | ||
| Rho(0) | −1.209 (−0.493) ** | ||
| lns1 | −0.042 (−0.089) | ||
| Rho(1) | −0.28 (−0.344) | ||
| Log pseudolikelihood | −836.073 | ||
| Wald test of independence of equations (Chi2) | 6.93 ** | ||
| Index | Proportion | Value |
|---|---|---|
| Average Treatment Effect on the Treated (ATT) | −0.5263 (0.0531) *** | −12,898.58 (1726.217) *** |
| Average Treatment Effect on the Untreated (ATU) | 0.3313 (0.0228) *** | 6333.276 (547.628) *** |
| Average Treatment Effect (ATE) | 0.1322 (0.0263) *** | 1868.739 (674.0174) *** |
| Model | ATT | Standard Error. | T-Stat |
|---|---|---|---|
| (1) ESR | −0.526 *** | 0.053 | −9.91 |
| (2) PSM | 0.197 | 0.181 | 1.09 |
| (3) IPWRA | 0.034 | 0.117 | 0.29 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ndonou Tchoumdop, M.E.; Nda’chi Deffo, R.; Tsambou, A.D.; Fomba Kamga, B. Handwashing and Household Health Expenditures Under COVID-19: Evidence from Cameroon. Economies 2025, 13, 231. https://doi.org/10.3390/economies13080231
Ndonou Tchoumdop ME, Nda’chi Deffo R, Tsambou AD, Fomba Kamga B. Handwashing and Household Health Expenditures Under COVID-19: Evidence from Cameroon. Economies. 2025; 13(8):231. https://doi.org/10.3390/economies13080231
Chicago/Turabian StyleNdonou Tchoumdop, Michèle Estelle, Rodrigue Nda’chi Deffo, André Dumas Tsambou, and Benjamin Fomba Kamga. 2025. "Handwashing and Household Health Expenditures Under COVID-19: Evidence from Cameroon" Economies 13, no. 8: 231. https://doi.org/10.3390/economies13080231
APA StyleNdonou Tchoumdop, M. E., Nda’chi Deffo, R., Tsambou, A. D., & Fomba Kamga, B. (2025). Handwashing and Household Health Expenditures Under COVID-19: Evidence from Cameroon. Economies, 13(8), 231. https://doi.org/10.3390/economies13080231







