Exploring Pharmacy Trainee Experiential Learning in a Full Scope Collaborative Rural Primary Care Practice: A Retrospective Chart Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
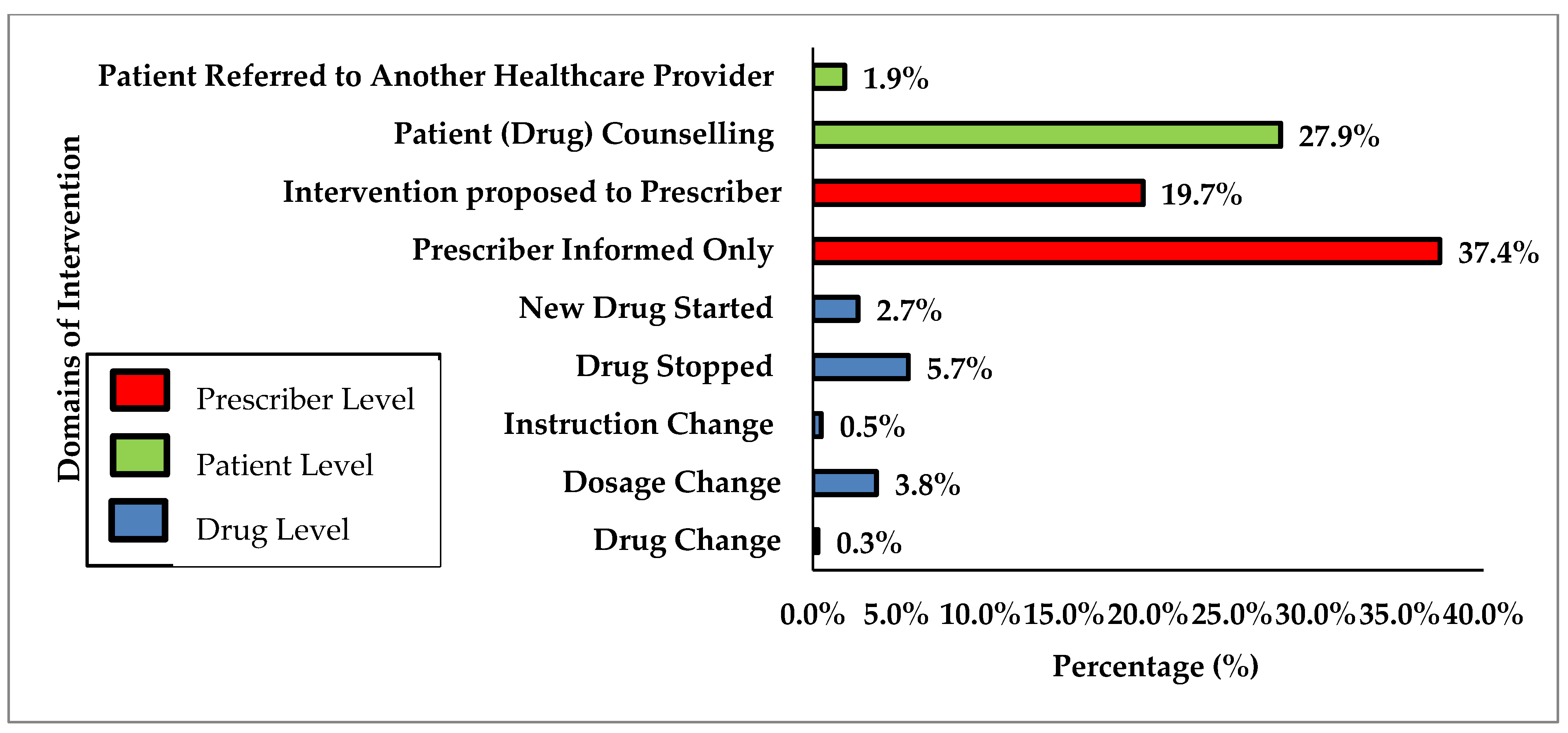
3.1. DTPs Identified and Interventions Made by Pharmacy Trainees
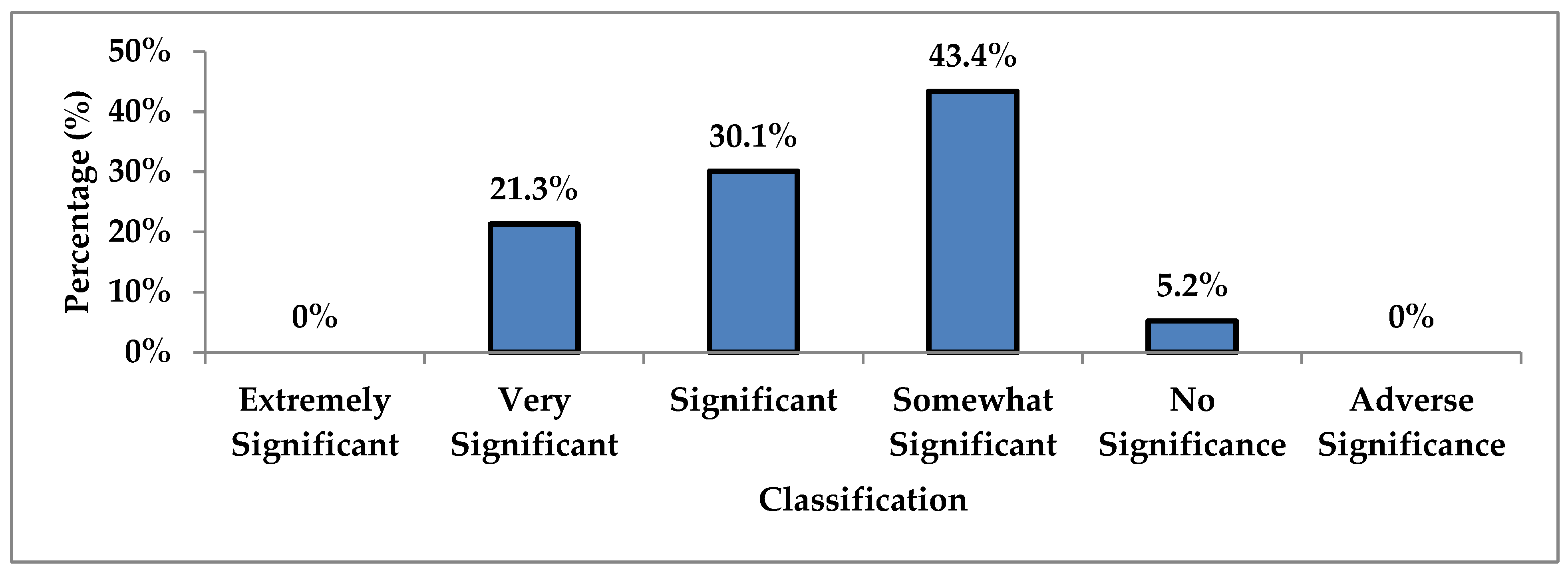
3.2. Valuation of Pharmacy Trainee Interventions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Canadian Pharmacists Association. Pharmacists’ Scope of Practice in Canada. Available online: https://www.pharmacists.ca/cpha-ca/assets/File/pharmacy-in-canada/Scope%20of%20Practice%20in%20 Canada_June2020.pdf (accessed on 24 August 2021).
- Supapaan, T.; Low, B.Y.; Wongpoowarak, P.; Moolasarn, S.; Anderson, C. A transition from the BPharm to the PharmD degree in give selected countries. Pharm. Pract. 2019, 17, 1–9. [Google Scholar]
- Association of Faculties of Pharmacy of Canada (AFPC). Available online: http://afpc.info/sites/default/files/AFPC_ADPC_PharmD_Position_Statement_Resolution_Sept_2010.pdf (accessed on 24 August 2021).
- University of Waterloo School of Pharmacy. Available online: https://uwaterloo.ca/pharmacy/future-pharmd-students/program-overview (accessed on 24 August 2021).
- University of Toronto. Available online: https://pharmacy.utoronto.ca/programs-and-admissions/pharmd/current-students/ (accessed on 24 August 2021).
- Canadian Society of Hospital Pharmacists. Canadian Pharmacy Residency Board. Available online: https://cshp-scph.ca/cprb (accessed on 24 August 2021).
- Canadian Society of Hospital Pharmacists. Accredited & Accreditation Pending Programs. Available online: https://cshp.ca/year-1-programs (accessed on 24 August 2021).
- Frankel, G.; Louizos, C.; Austin, Z. Canadian educational approaches for the advancement of pharmacy practice. Am. J. Pharm. Educ. 2014, 78, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waite, N.M.; McCarthy, L.; Milne, E.; Hillier, C.; Houle, S.K.D.; Dolovich, L. Perceived preparedness for full-scope pharmacist services among recent Doctor of Pharmacy graduates from Ontario schools of pharmacy. J. Am. Pharm. Assoc. 2018, 58, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Petrov, K.; Varadarajan, R.; Healy, M.; Darvish, E.; Cowden, C. Improving medication history at admission utilizing pharmacy students and technicians: A pharmacy-driven improvement initiative. P T 2018, 43, 676–684. [Google Scholar] [PubMed]
- Pham, D.Q. Evaluating the impact of clinical interventions by PharmD students on internal medicine clerkships: The results of a 3 year study. Ann. Pharm. 2006, 40, 1541–1545. [Google Scholar] [CrossRef] [PubMed]
- Vinluan, C.M.; Jabalie, M.M.; Navarrete, J.P.; Padilla, M.E. Evaluating the types of pharmacy student interventions made during an interprofessional 6-week adult internal medicine rotation. J. Pharm. Pract. 2018, 31, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Ginzburg, R. Impact of pharmacy student interventions in an urban family medicine clinic. Am. J. Pharm. Educ. 2014, 78, 1–5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosco, C.; Oandasan, I. Review of Family Medicine within Rural and Remote Canada: Education, Practice, and Policy; College of Family Physicians of Canada: Mississauga, ON, Canada, 2016. [Google Scholar]
- Rosser, W.W.; Colwill, J.M.; Kasperski, J.; Wilson, L. Progress of Ontario’s Family Health Team model: A patient-centered medical home. Ann. Fam. Med. 2011, 9, 165–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Statistics Canada. Huron County Health Unit, [Health Region, December 2017], Ontario and Canada [Country] (Table). Huron County Health Unit, [Health Region, December 2017], Ontario and Canada [Country] (Table). Census Profile. 2016 Census. Statistics Canada Catalogue No. 98-316-X2016001. Ottawa. Released 29 November 2017. 2017. Available online: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E (accessed on 24 August 2021).
- Pharmaceutical Care Network Europe (PCNE). Available online: https://www.pcne.org/ (accessed on 24 August 2021).
- van Mil, J.W.F.; Westerlund, L.O.T.; Hersberger, K.E.; Schaefer, M.A. Drug-related problem classification systems. Ann. Pharm. 2004, 38, 859–867. [Google Scholar] [CrossRef] [PubMed]
- Pharmaceutical Care Network Europe Association. Available online: https://www.pcne.org/upload/files/334_PCNE_classification_V9-0.pdf (accessed on 24 August 2021).
- Overhage, J.M.; Lukes, A. Practical, reliable, comprehensive method for characterizing pharmacists’ clinical activities. Am. J. Health-Syst. Pharm. 1999, 56, 2444–2450. [Google Scholar] [CrossRef] [PubMed]
- Hatoum, H.T.; Hutchinson, R.A.; Witte, K.; Newby, G.P. Evaluation of the contribution of clinical pharmacists: Inpatient care and cost reduction. Drug Intell. Clin. Pharm. 1988, 22, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Skaggs School of Pharmacy and Pharmaceutical Sciences. Available online: https://pharmacy.cuanschutz.edu/academics/pharmd/experiential-program/international-rotations/western-australia (accessed on 25 August 2021).
- Thackrah, R.D.; Hall, M.; Fitzgerald, K.; Thompson, S.C. Up close and real: Living and learning in a remote community builds students’ cultural capabilities and understanding of health disparities. Int. J. Equal. Health 2017, 16, 119. [Google Scholar] [CrossRef] [PubMed]
- Rath, C.; Tillman, F.; Stickel, J.; Jones, M.; Armistead, L. Implementation of a student-developed service-based internship for pharmacy students. Innov. Pharm. 2019, 10, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolcott, M.D.; McLaughlin, J.E.; Hubbard, D.K.; Williams, C.R.; Kiser, S.N. Using design thinking to explore rural experiential education barriers and opportunities. J. Med. Educ. Curric. Dev. 2021, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Pullon, S.; Wilson, C.; Gallagher, P.; Skinner, M.; McKinlay, E.; Gray, L.; McHugh, P. Transition to practice: Can rural interprofessional education make a difference? A cohort study. BMC Med. Edu. 2016, 16, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristic | n (%) |
|---|---|
| Number of appointments | 153 |
| Polypharmacy | 54 (35) |
| Opioid review | 72 (47) |
| Travel clinic | 2 (1) |
| Referral | 5 (3) |
| Follow-up | 20 (13) |
| Average time spent per appointment (min) | 72 |
| Direct contact time spent with the patient/caregivers | 40.5 (56) |
| Indirect | 31.5 (44) |
| PCNE Code | Domain and Classification | n (%) |
|---|---|---|
| Treatment Effectiveness | 76 (20.7) | |
| P1.1 | No effect of drug treatment/therapy failure | 14 |
| P1.2 | Effect of drug not optimal | 38 |
| P1.3 | Untreated symptoms or indication | 24 |
| Treatment Safety | 139 (38.0) | |
| P2.1 | Adverse drug event occurring (or possibility to occur) | 139 |
| Other | 151 (41.3) | |
| P3.1 | Problem with cost-effectiveness of treatment | 3 |
| P3.2 | Unnecessary drug treatment | 15 |
| P3.3 | Other (specify; medication reconciliation required) | 133 |
| PCNE Code | Domain and Classification | n (%) |
|---|---|---|
| Drug Selection | 81 (22.1) | |
| C1.1 | Inappropriate drug according to guidelines | 13 |
| C1.3 | No indication for drug | 9 |
| C1.4 | Inappropriate combination of drugs or drugs and herbals | 13 |
| C1.5 | Inappropriate duplication of therapeutic group/ingredient | 5 |
| C1.6 | No or incomplete drug treatment in spite of existing indication | 41 |
| Dose Selection | 33 (9.0) | |
| C3.1 | Drug dose too low | 11 |
| C3.2 | Drug dose too high | 20 |
| C3.3 | Dosage regimen not frequent enough | 1 |
| C3.4 | Dosage regimen too frequent | 1 |
| Treatment Duration | 7 (2.0) | |
| C4.1 | Duration of treatment too short | 1 |
| C4.2 | Duration of treatment too long | 6 |
| Patient Related | 90 (24.6) | |
| C7.1 | Uses/takes less drug than prescribed or does not take | 9 |
| C7.7 | Inappropriate timing or dosing intervals | 2 |
| C7.10 | Unable to understand instructions properly (requires education) | 79 |
| Patient Transfer Related | 133 (36.3) | |
| C8.2 | No updated medication list available | 133 |
| Other | 22 (6.0) | |
| C9.1 | No or inappropriate outcome monitoring | 9 |
| C9.2 | Other (specify; prescriber requires drug information, patient needs referral to another healthcare professional) | 13 |
| PCNE Code | Domain and Classification | n (%) |
|---|---|---|
| Intervention Accepted | 60 (83.3) | |
| A1.1 | Intervention accepted, fully implemented | 53 |
| A1.3 | Intervention accepted, but not implemented (patient declined) | 7 |
| A2.2 | Intervention not Accepted | 12 (16.7) |
| Intervention not accepted: no agreement | 12 |
| Outcome | n |
|---|---|
| Reduction in Patient Health Questionnaire (PHQ-9) Score (depression control) | 4 |
| Improvement in vitals (heart rate, blood pressure) | 10 |
| Improvement in blood work (hemoglobin, B12, potassium) | 3 |
| Resolution of ADR (dizziness, fatigue, diarrhea) | 5 |
| Reduced pill burden (with no rebound symptoms) | 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robinson, S.; Chang, F. Exploring Pharmacy Trainee Experiential Learning in a Full Scope Collaborative Rural Primary Care Practice: A Retrospective Chart Review. Pharmacy 2021, 9, 155. https://doi.org/10.3390/pharmacy9030155
Robinson S, Chang F. Exploring Pharmacy Trainee Experiential Learning in a Full Scope Collaborative Rural Primary Care Practice: A Retrospective Chart Review. Pharmacy. 2021; 9(3):155. https://doi.org/10.3390/pharmacy9030155
Chicago/Turabian StyleRobinson, Sara, and Feng Chang. 2021. "Exploring Pharmacy Trainee Experiential Learning in a Full Scope Collaborative Rural Primary Care Practice: A Retrospective Chart Review" Pharmacy 9, no. 3: 155. https://doi.org/10.3390/pharmacy9030155
APA StyleRobinson, S., & Chang, F. (2021). Exploring Pharmacy Trainee Experiential Learning in a Full Scope Collaborative Rural Primary Care Practice: A Retrospective Chart Review. Pharmacy, 9(3), 155. https://doi.org/10.3390/pharmacy9030155






