Peer Teaching in an Interprofessional Education Activity Focused on Professional Skills Development
Abstract
1. Introduction
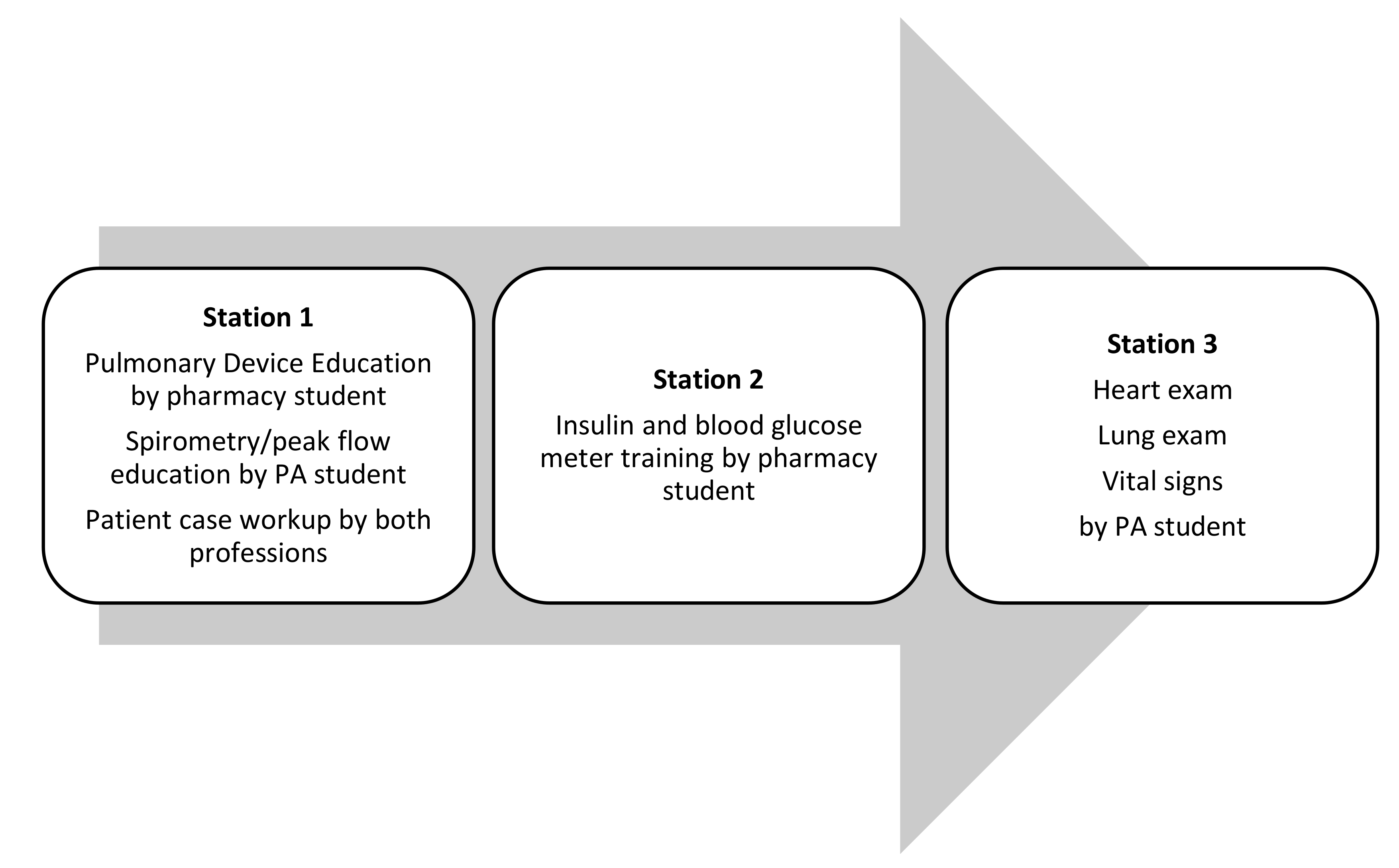
2. Materials and Methods
Resources Required
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Accreditation Council for Pharmacy Education. Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Available online: https://www.acpe-accredit.org/pharmd-program-accreditation/ (accessed on 30 April 2021).
- Accreditation Review Commission on Education for the Physician Assistant, Inc. Accreditation Manual—Accreditation Standards for Physician Assistant Education, 5th Edition. Revised. March 2021. Available online: http://www.arc-pa.org/wp-content/uploads/2021/03/Standards-5th-Ed-March-2021.pdf (accessed on 30 April 2021).
- Interprofessional Education Collaborative. Core Competencies for Interprofessional Collaborative Practice. 2019. Available online: https://nebula.wsimg.com/2f68a39520b03336b41038c370497473?AccessKeyId=DC06780E69ED19E2B3A5&disposition=0&alloworigin=1 (accessed on 13 May 2021).
- Sadowski, C.A.; Li, J.C.; Pasay, D.; Jones, C.A. Interprofessional Peer Teaching of Pharmacy and Physical Therapy Students. Am. J. Pharm. Educ. 2015, 79, 155. [Google Scholar] [CrossRef] [PubMed]
- Lipton, H.L.; Lai, C.J.; Cutler, T.W.; Smith, A.R.; Stebbins, M.R. Peer-to-peer interprofessional health policy education for Medicare part D. Am. J. Pharm. Educ. 2010, 74, 102. [Google Scholar] [CrossRef] [PubMed]
- Lehrer, M.D.; Murray, S.; Benzar, R.; Stormont, R.; Lightfoot, M.; Hafertepe, M.; Welch, G.; Peters, N.; Maio, A. Peer-led problem-based learning in interprofessional education of health professions students. Med. Educ. Online 2015, 20, 28851–28854. [Google Scholar] [CrossRef] [PubMed]
- Hsia, S.; Tran, D.N.; Beechinor, R.; Gahbauer, A.; Fitzsimmons, A.; Brock, T. Interprofessional peer teaching: The value of a pharmacy student-led pharmacology course for physical therapy students. Curr. Pharm. Teach. Learn. 2020, 12, 1252–1257. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; Roberts, C.; van Diggele, C.; Mellis, C. Peer teacher training (PTT) program for health professional students: Interprofessional and flipped learning. BMC Med. Educ. 2017, 17, 239. [Google Scholar] [CrossRef] [PubMed]
- Loda, T.; Erschens, R.; Loenneker, H.; Keifenheim, K.E.; Nikendei, C.; Junne, F.; Zipfel, S.; Herrmann-Werner, A. Cognitive and social congruence in peer-assisted learning—A scoping review. PLoS ONE 2019, 14, e0222224. [Google Scholar] [CrossRef] [PubMed]
- Burgess, A.; Nestel, D. Facilitating the development of professional identity through peer assisted learning in medical education. Adv. Med. Educ. Pract. 2014, 5, 403–406. [Google Scholar] [CrossRef] [PubMed]
- Truong, T.H.; Nguyen, T.T.; Armor, B.L.; Farley, J.R. Errors in the Administration Technique of Insulin Pen Devices: A Result of Insufficient Education. Diabetes Ther. 2017, 8, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Usmani, O.S.; Lavorini, F.; Marshall, J.; Dunlop, W.C.N.; Heron, L.; Farrington, E.; Dekhuijzen, R. Critical inhaler errors in asthma and COPD: A systematic review of impact on health outcomes. Respir Res. 2018, 19, 10. [Google Scholar] [CrossRef] [PubMed]
- Barry, A.R.; Egan, G.; Turgeon, R.D.; Leung, M. Evaluation of Physical Assessment Education for Practising Pharmacists: A Cross-Sectional Survey. Can. J. Hosp. Pharm. 2019, 72, 27–33. [Google Scholar] [CrossRef] [PubMed]
| Statement: Rate the Impact of the IPE Activities on Your Ability to: 1 | Mean (SD) |
|---|---|
| Participate in building a patient care team and perform effectively in various roles on the team. | 4.43 (0.6) |
| Effectively communicate with other health professionals to support a team approach to patient care. | 4.45 (0.59) |
| Use the knowledge of one’s own role and those of other professions in providing patient care. | 4.49 (0.57) |
| Work with individuals of other professions to maintain a climate of mutual respect and shared values. | 4.54 (0.59) |
| Statement: What Is Your Current Confidence Level Doing the Following? | Pre-Activity (Pharmacy) Mean (SD) N = 207 | Post-Activity (Pharmacy) Mean (SD) N = 207 | Gains (Pharmacy) | Pre-Activity (PA) Mean (SD) N = 43 | Post-Activity (PA) Mean (SD) N = 43 | Gains (PA) |
|---|---|---|---|---|---|---|
| Differentiating the indications of various inhaled medication delivery systems | 3.7 (0.78) | 4.3 (0.73) * | 0.6 | 3.2 (0.8) | 3.7 (0.87) * | 0.5 |
| Identifying comorbidities influencing the use of various inhaled medication delivery systems | 3.1 (0.77) | 3.9 (0.79) * | 0.8 | 3.3 (0.72) | 3.7 (0.84) * | 0.4 |
| Educating a patient on the appropriate administration of various inhaled medication delivery systems | 3.9 (0.8) | 4.5 (0.64) * | 0.6 | 3.5 (0.9) | 4.0 (0.79) * | 0.5 |
| Differentiating the indications and use of various insulin delivery systems | 3.4 (0.85) | 4.2 (0.73) * | 0.8 | 1.7 (1.04) | 3.4 (0.89) * | 1.7 |
| Educating a patient on the appropriate administration and storage of various insulin delivery systems | 3.6 (0.84) | 4.3 (0.72) * | 0.7 | 1.8 (1.21) | 3.6 (0.84) * | 1.8 |
| Educating a patient on the use of a glucose meter to test blood glucose | 3.9 (0.89) | 4.5 (0.66) * | 0.6 | 2.8 (1.32) | 4.1 (0.82) * | 1.3 |
| Taking a manual blood pressure | 3.7 (0.95) | 4.1 (0.81) * | 0.4 | 4.5 (0.59) | 4.8 (0.47) * | 0.3 |
| Checking a patient’s heart rate and rhythm | 3.3 (0.94) | 3.9 (0.87) * | 0.6 | 4.7 (0.49) | 4.9 (0.35) | 0.2 |
| Assessing a patient’s respiratory rate | 3.2 (0.93) | 3.8 (0.90) | 0.6 | 4.5 (0.66) | 4.8 (0.37) * | 0.3 |
| Performing a heart exam on a patient | 2.3 (0.92) | 3.2 (1.03) * | 0.9 | 3.5 (0.73) | 4.3 (0.76) * | 0.8 |
| Performing a lung exam on a patient | 2.3 (0.90) | 3.2 (1.04) * | 0.9 | 3.9 (0.73) | 4.4 (0.62) * | 0.5 |
| Interpreting spirometry results | 2.6 (0.94) | 2.7 (0.93) * | 0.1 | 3.6 (0.69) | 3.9 (0.78) * | 0.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
DelNero, T.; Vyas, D. Peer Teaching in an Interprofessional Education Activity Focused on Professional Skills Development. Pharmacy 2021, 9, 112. https://doi.org/10.3390/pharmacy9020112
DelNero T, Vyas D. Peer Teaching in an Interprofessional Education Activity Focused on Professional Skills Development. Pharmacy. 2021; 9(2):112. https://doi.org/10.3390/pharmacy9020112
Chicago/Turabian StyleDelNero, Tracey, and Deepti Vyas. 2021. "Peer Teaching in an Interprofessional Education Activity Focused on Professional Skills Development" Pharmacy 9, no. 2: 112. https://doi.org/10.3390/pharmacy9020112
APA StyleDelNero, T., & Vyas, D. (2021). Peer Teaching in an Interprofessional Education Activity Focused on Professional Skills Development. Pharmacy, 9(2), 112. https://doi.org/10.3390/pharmacy9020112






