Nonmedical Prescription Opioid Use among a Sample of College Students: Prevalence and Predictors
Abstract
1. Introduction
1.1. Motivations for Prescription Opioid Misuse
1.2. Psychological and Neuropsychological Factors
1.3. Comorbid Substance Use
1.4. Individual Factors
2. Materials and Methods
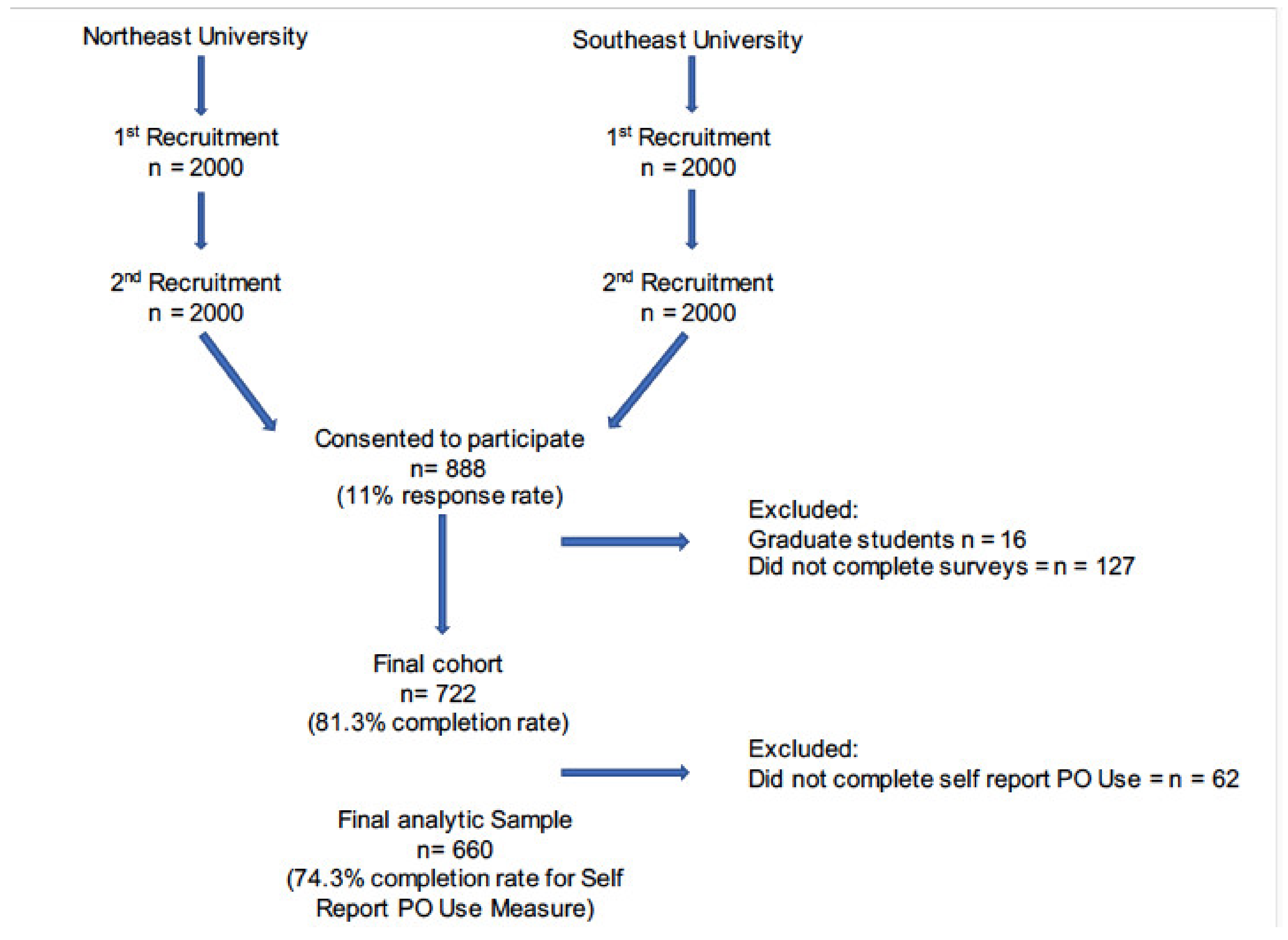
2.1. Participants
2.2. Procedures
2.3. Measures
2.3.1. Demographic Variables
2.3.2. Prescription Opioid Use
2.3.3. Motivations for Use
2.3.4. Frequency of Use
2.3.5. Prescription Source/Age of Misuse
2.3.6. Behavior Rating Inventory of Executive Function—Adult
2.3.7. Sexual Risk Survey
2.3.8. DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measure—Adult
2.3.9. PROMIS®® (Patient-Reported Outcomes Measurement Information System)
2.4. Statistical Analyses
3. Results
3.1. NMPO Characteristics
3.2. Correlates of Nonmedical Prescription Opioid Use
3.3. Characteristics of Students Reporting NMPO
3.3.1. Age of Onset
3.3.2. Sources for Obtaining Prescription Opioids
3.3.3. Medication Types
3.3.4. Motivations for Use
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Castaldelli-Maia, J.M.; Nicastri, S.; Cerdá, M.; Kim, J.H.; de Oliviera, L.G.; de Andrade, A.G.; Martins, S.S. In-transition culture of experimentation with cannabis in Latin American college students: A new role within a potential drug use sequencing pattern. Drug Alcohol. Rev. 2018, 37, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Weyandt, L.L.; Marraccini, M.E.; Gudmundsdottir, B.G.; Martinez Zavras, B.; Turcotte, K.D.; Monro, B.A.; Amoroso, A.J. Misuse of prescription stimulants among college students: A review of the literature and implications for morphological and cognitive effects on brain functioning. Exp. Clin. Psychopharmacol. 2013, 21, 385–407. [Google Scholar] [CrossRef] [PubMed]
- Victor, G.A.; Walker, R.; Cole, J.; Logan, T.K. Opioid analgesics and heroin: Examining drug misuse trends among a sample of drug treatment clients in Kentucky. Int. J. Drug. Policy. 2017, 46, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Webster, L.R. Risk factors for opioid-use disorder and overdose. Anesth. Analg. 2017, 125, 1741–1748. [Google Scholar] [CrossRef]
- Wilson, N.; Kariisa, M.; Seth, P.; Smith, H.; Davis, N.L. Drug and opioid-involved overdose deaths—United States, 2017-2018. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 290–297. [Google Scholar] [CrossRef]
- Gladden, R.M.; O’Donnell, J.; Mattson, C.L.; Seth, P. Changes in opioid-involved overdose deaths by opioid type and presence of benzodiazepines, cocaine, and methamphetamine—25 states, July-December 2017 to January–June 2018. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 737–744. [Google Scholar] [CrossRef]
- Scholl, L.; Seth, P.; Kariisa, M.; Wilson, N.; Baldwin, G. Drug and opioid-involved overdose deaths- United States, 2013-2017. MMWR Morb. Mortal. Wkly. Rep. 2019, 67, 1419–1427. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Drug Overdose Deaths up 4.6% in 2019; American Hospital Association: Chicago, IL, USA, 2020; Available online: https://www.aha.org/news/headline/2020-07-16-cdc-drug-overdose-deaths-46-2019#:~:text=Drug%20overdose%20deaths%20in%20the,by%20drug%20category%20and%20state (accessed on 29 September 2020).
- Center for Behavioral Health Statistics and Quality. 2017 National Survey on Drug Use and Health: Detailed Tables; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2018. Available online: https://www.samhsa.gov/data/sites/default/les/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDetailedTabs2017.pdf (accessed on 4 October 2020).
- National Institute on Drug Abuse. Opioid Overdose Crisis; National Institutes of Health: Bethesda, MD, USA, 2020. Available online: https://www.drugabuse.gov/drug-topics/opioids/opioid-overdose-crisis (accessed on 20 September 2020).
- Centers for Disease Control and Prevention. Opioid Data Analysis and Resources. 2020. Available online: https://www.cdc.gov/drugoverdose/data/analysis.html (accessed on 20 September 2020).
- Messina, B.G.; Silvestri, M.M.; Diulio, A.R.; Murphy, J.G.; Garza, K.B.; Correia, C.J. Alcohol use, impulsivity, and the non-medical use of prescription stimulants among college students. Addict. Behav. 2014, 39, 1798–1803. [Google Scholar] [CrossRef]
- Schepis, T.S.; Acheson, S.; Zapp, D.; Swartzwelder, H.S. Alcohol use and consequences in matriculating US college students by prescription stimulant/opioid nonmedical misuse status. Addict. Behav. 2019, 98, 106026. [Google Scholar] [CrossRef]
- Weyandt, L.L.; Gudmundsdottir, B.G.; Holding, E.Z.; Marraccini, M.E.; Keith, M.; May, S.E.; Shepard, E.; Francis, A.; Wilson, E.D.; Channell, I.; et al. Prescription opioid misuse among university students: A systematic review. J. Am. Coll. Health. 2020, 1–19. [Google Scholar] [CrossRef]
- Benotsch, E.G.; Koester, S.; Luckman, D.; Martin, A.M.; Cejka, A. Non-medical use of prescription drugs and sexual risk behavior in young adults. Addict. Behav. 2011, 36, 152–155. [Google Scholar] [CrossRef]
- Harries, M.D.; Lust, K.; Christenson, G.A.; Redden, S.A.; Grant, J.E. Prescription opioid medication misuse among university students. Am. J. Addict. 2018, 27, 618–624. [Google Scholar] [CrossRef]
- Jones, C.M.; McAninch, J.K. Emergency department visits and overdose deaths from combined use of opioids and benzodiazepines. Am. J. Prev. Med. 2015, 49, 493–501. [Google Scholar] [CrossRef]
- Kenne, D.R.; Fischbein, R.L.; Tan, A.S.; Banks, M. The use of substances other than nicotine in electronic cigarettes among college students. Subst. Abuse. 2017, 11, 1–8. [Google Scholar] [CrossRef]
- McCabe, S.E.; Cranford, J.A.; Boyd, C.J.; Teter, C.J. Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addict. Behav. 2007, 32, 562–575. [Google Scholar] [CrossRef]
- Schepis, T.S.; Teter, C.J.; Simoni-Wastila, L.; McCabe, S.E. Prescription tranquilizer/sedative misuse prevalence and correlates across age cohorts in the US. Addict. Behav. 2018, 87, 24–32. [Google Scholar] [CrossRef]
- Schulenberg, J.E.; Johnston, L.D.; O’Malley, P.M.; Bachman, J.G.; Miech, R.A.; Patrickm, M.E. Monitoring the future: National survey results on drug use 1975–2016. In College Students and Adults Ages 19–55; The University of Michigan: Ann Arbor, MI, USA, 2018; Volume 2, pp. 1–454. [Google Scholar] [CrossRef]
- Matson, S.C.; Bentley, C.; Hughes Dughman, V.; Bonny, A.E. Receipt of prescribed controlled substances by adolescents and young adults prior to presenting for opiate dependence treatment. J. Addict. 2013. [Google Scholar] [CrossRef]
- Arteta, J.; Cobos, B.; Hu, Y.; Jordan, K.; Howard, K. Evaluation of how depression and anxiety mediate the relationship between pain catastrophizing and prescription opioid misuse in a chronic pain population. Pain Med. 2016, 17, 295–303. [Google Scholar] [CrossRef]
- Mason, M.J.; Golladay, G.; Jiranek, W.; Cameron, B.; Silverman, J.J.; Zaharakis, N.M.; Plonski, P. Depression moderates the relationship between pain and the nonmedical use of opioid medication among adult outpatients. J. Addict. Med. 2016, 10, 408–413. [Google Scholar] [CrossRef]
- Martel, M.O.; Edwards, R.R.; Jamison, R.N. The relative contribution of pain and psychological factors to opioid misuse: A 6-month observational study. Am. Psychol. 2020, 75, 772–783. [Google Scholar] [CrossRef]
- Pielech, M.; Lunde, C.E.; Becker, S.J.; Vowles, K.E.; Sieberg, C.B. Comorbid chronic pain and opioid misuse in youth: Knowns, unknowns, and implications for behavioral treatment. Am. Psychol. 2020, 75, 811–824. [Google Scholar] [CrossRef]
- Reynolds, B.W.; Basso, M.R.; Miller, A.K.; Whiteside, D.M.; Combs, D. Executive function, impulsivity, and risky behaviors in young adults. Neuropsychology 2019, 33, 212–221. [Google Scholar] [CrossRef]
- Moride, Y.; Lemieux-Uresandi, D.; Castillon, G.; Soares de Moura, C.; Pilote, L.; Faure, M.; Berartsky, S. A systematic review of interventions and programs targeting appropriate prescribing of opioids. Pain Physician 2019, 22, 229–240. [Google Scholar] [CrossRef]
- Stoicea, N.; Costa, A.; Periel, L.; Uribe, A.; Weaver, T.; Bergese, S.D. Current perspectives on the opioid crisis in the US healthcare system: A comprehensive literature review. Medicine 2019, 98, e15425. [Google Scholar] [CrossRef]
- Aroke, H.A.; Buchanan, A.L.; Bratberg, J.P.; Hogan, J.W.; Rich, J.D.; Wen, X.; Kogut, S.J. Patterns of initial prescription opioid use and risk of mortality. J. Addict. Med. 2020. online ahead of print. [Google Scholar]
- Brummett, C.M.; Waljee, J.F.; Goesling, J.; Moser, S.; Lin, P.; Englesbe, M.J.; Bohnert, A.S.B.; Kheterpal, S.; Nallamothu, B.K. New persistent opioid use after minor and major surgical procedures in us adults. JAMA Surg. 2017, 152, e170504. [Google Scholar] [CrossRef]
- Fischer, B.; Jones, W.; Varatharajan, T.; Malta, M.; Kurdyak, P. Correlations between population-levels of prescription opioid dispensing and related deaths in Ontario (Canada), 2005–2016. Prev. Med. 2018, 116, 112–118. [Google Scholar] [CrossRef]
- Martin, B.C.; Fan, M.Y.; Edlund, M.J.; Devries, A.; Brennan Braden, J.; Sullivan, M.D. Long-term chronic opioid therapy discontinuation rates from the TROUP study. J. Gen. Intern. Med. 2011, 26, 1450–1457. [Google Scholar] [CrossRef] [PubMed]
- Rogers, A.H.; Bakhshaie, J.; Lam, H.; Langdon, K.J.; Ditre, J.W.; Zvolensky, M.J. Pain-related anxiety and opioid misuse in a racially/ethnically diverse young adult sample with moderate/severe pain. Cogn. Behav. Ther. 2018, 47, 372–382. [Google Scholar] [CrossRef]
- Davis, R.E.; Bass, M.A.; Wade, M.A.; Nahar, V.K. Screening for depression among a sample of US college students who engage in recreational prescription opioid misuse. Health Promot. Perspect. 2020, 10, 59–65. [Google Scholar] [CrossRef]
- Davis, R.E.; Doyle, N.A.; Nahar, V.K. Association between prescription opioid misuse and dimensions of suicidality among college students. Psychiatry Res. 2020, 287, 112469. [Google Scholar] [CrossRef] [PubMed]
- Weyandt, L.L. Executive functions and attention deficit hyperactivity disorder. ADHD Rep. 2009, 17, 1–7. [Google Scholar] [CrossRef]
- Ersche, K.D.; Clark, L.; London, M.; Robbins, T.W.; Sahakian, B.J. Profile of executive and memory function associated with amphetamine and opiate dependence. Neuropsychopharmacology 2006, 31, 1036–1047. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Serrano, M.J.; Perales, J.C.; Moreno-López, L.; Pérez-García, M.; Verdejo-García, A. Neuropsychological profiling of impulsivity and compulsivity in cocaine dependent individuals. Psychopharmacology 2012, 219, 673–683. [Google Scholar] [CrossRef]
- Garland, E.L.; Howard, M.O. Mindfulness-based treatment of addiction: Current state of the field and envisioning the next wave of research. Addict. Sci. Clin. Prac. 2018, 13, 14. [Google Scholar] [CrossRef]
- Nigg, J.T.; Wong, M.M.; Martel, M.M.; Jester, J.M.; Puttler, L.I.; Glass, J.M.; Adams, K.M.; Fitzgerald, H.E.; Zucker, R.A. Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. J. Am. Acad. Child. Adolesc. Psychiatry 2016, 45, 468–475. [Google Scholar] [CrossRef]
- Pentz, M.A.; Shin, H.S.; Riggs, N.; Unger, J.B.; Collison, K.L.; Chou, C.P. Parent, peer, and executive function relationships to early adolescent e-cigarette use: A substance use pathway? Addict. Behav. 2015, 42, 73–78. [Google Scholar] [CrossRef]
- Wilens, T.E.; Carrellas, N.W.; Martelon, M.; Yule, A.M.; Fried, R.; Anselmo, R.; McCabe, S.E. Neuropsychological functioning in college students who misuse prescription stimulants. Am. J. Addict. 2017, 26, 379–387. [Google Scholar] [CrossRef]
- Garland, E.L.; Bryan, C.J.; Nakamura, Y.; Froeliger, B.; Howard, M.O. Deficits in autonomic indices of emotion regulation and reward processing associated with prescription opioid use and misuse. Psychopharmacology 2017, 234, 621–629. [Google Scholar] [CrossRef]
- Sadeghi, S.; Ekhtiari, H.; Bahrami, B.; Ahmadabadi, M.N. Metacognitive deficiency in a perceptual but not a memory task in methadone maintenance patients. Sci. Rep. 2017, 7, 7052. [Google Scholar] [CrossRef]
- Castle, I.J.; Dong, C.; Haughwout, S.P.; White, A.M. Emergency department visits for adverse drug reactions involving alcohol: United States, 2005 to 2011. Alcohol Clin. Exp. Res. 2016, 40, 1913–1925. [Google Scholar] [CrossRef]
- Grigsby, T.J.; Howard, J.T. Prescription opioid misuse and comorbid substance use: Past 30-day prevalence, correlates, and co-occurring behavioral indicators in the 2016 National Survey on Drug Use and Health. Am. J. Addict. 2019, 28, 111–118. [Google Scholar] [CrossRef]
- Nechuta, S.J.; Tyndall, B.D.; Mukhopadhyay, S.; McPheeters, M.L. Sociodemographic factors, prescription history and opioid overdose deaths: A statewide analysis using linked PDMP and mortality data. Drug Alcohol Depend. 2018, 190, 62–71. [Google Scholar] [CrossRef]
- Park, T.W.; Saitz, R.; Ganoczy, D.; Ilgen, M.A.; Bohnert, A.S.B. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: Case-cohort study. BMJ 2015, 350, 2698. [Google Scholar] [CrossRef]
- Arria, A.M.; Caldeira, K.M.; Vincent, K.B.; Winick, E.R.; Baron, R.A.; O’Grady, K.E. Discontinuous college enrollment: Associations with substance use and mental health. Psychiatr. Serv. 2013, 64, 165–172. [Google Scholar] [CrossRef]
- Shell, D.F.; Newman, I.M. Effects of a web-based pre-enrollment alcohol brief motivational intervention on college student retention and alcohol-related violations. J. Am. Coll. Heath 2018, 17, 1–2. [Google Scholar] [CrossRef]
- Hulme, S.; Bright, D.; Nielsen, S. The source and diversion of pharmaceutical drugs for non-medical use: A systematic review and meta-analysis. Drug Alcohol Depend. 2018, 186, 242–256. [Google Scholar] [CrossRef]
- Lord, S.; Brevard, J.; Budman, S. Connecting to young adults: An online social network survey of beliefs and attitudes associated with prescription opioid misuse among college students. Subst. Use Misuse 2011, 46, 66–76. [Google Scholar] [CrossRef]
- Clinton, H.A.; Hunter, A.A.; Logan, S.B.; Lapidus, G.D. Evaluating opioid overdose using the National Violent Death Reporting System, 2016. Drug Alcohol Depend. 2019, 194, 371–376. [Google Scholar] [CrossRef]
- Borsuk, C.S.; Juhnke, G.A. Gender Differences among College Students Who Misuse Prescription Opioids. VISTA 2015. Available online: https://www.counseling.org/docs/default-source/vistas/gender-differences-among-college-students.pdf?sfvrsn=ecdb432c_6 (accessed on 20 February 2021).
- Martins, S.S.; Kim, J.H.; Chen, L.Y.; Levin, D.; Keyes, K.M.; Cerdá, M.; Storr, C.L. Nonmedical prescription drug use among US young adults by educational attainment. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 713–724. [Google Scholar] [CrossRef]
- McCabe, S.E.; West, B.T.; Teter, C.J.; Boyd, C.J. Trends in medical use, diversion, and nonmedical use of prescription medications among college students from 2003 to 2013: Connecting the dots. Addict. Behav. 2014, 39, 1176–1182. [Google Scholar] [CrossRef] [PubMed]
- Rozenbroek, K.; Rothstein, W.G. Medical and nonmedical users of prescription drugs among college students. J. Am. Coll. Health 2011, 59, 358–363. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Aguilar-Gaxiola, S.; Berglund, P.A.; Carraveo-Anduaga, J.J.; DeWit, D.J.; Greenfield, S.F.; Kolody, B.; Olfson, M.; Vega, W.A. Patterns and predictors of treatment seeking after onset of a substance use disorder. JAMA Psychiatry 2001, 58, 1065–1071. [Google Scholar] [CrossRef] [PubMed]
- Panther, S.G.; Bray, B.S.; White, J.R. The implementation of a naloxone rescue program in university students. J. Am. Pharm. Assoc. 2017, 57, S107–S112.e2. [Google Scholar] [CrossRef]
- Veliz, P.; Epstein-Ngo, Q.; Austic, E.; Boyd, C.; McCabe, S.E. Opioid use among interscholastic sports participants: An exploratory study from a sample of college students. Res. Q. Exerc. Sport 2015, 86, 205–211. [Google Scholar] [CrossRef]
- Johnson, N.L.; Johnson, D.M. Factors influencing the relationship between sexual trauma and risky sexual behavior in college students. J. Interpers Violence 2013, 28, 2315–2331. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Jones, R.E.; Spradlin, A.; Robinson, R.J.; Tragesser, S.L. Development and validation of the Opioid Prescription Medication Motives Questionnaire: A four-factor model of reasons for use. Psychol. Addict. Behav. 2014, 28, 1290–1296. [Google Scholar] [CrossRef]
- Mateu-Gelabert, P.; Guarino, H.; Jessell, L.; Teper, A. Injection and sexual HIV/HCV risk behaviors associated with nonmedical use of prescription opioids among young adults in New York City. J. Subst. Abuse Treat. 2015, 48, 13–20. [Google Scholar] [CrossRef]
- Roth, R.M.; Lance, C.E.; Isquith, P.K.; Fischer, A.S.; Giancola, P.R. Confirmatory factor analysis of the Behavior Rating Inventory of Executive Function-Adult version in healthy adults and application to attention-deficit/hyperactivity disorder. Arch. Clin. Neuropsychol 2013, 28, 425–434. [Google Scholar] [CrossRef]
- Ciszewski, S.; Francis, K.; Mendella, P.; Bissada, H.; Tasca, G.A. Validity and reliability of the behavior rating inventory of executive function—Adult version in a clinical sample with eating disorders. Eat. Behav. 2014, 5, 175–181. [Google Scholar] [CrossRef]
- Turchik, J.A.; Garske, J.P. Measurement of sexual risk taking among college students. Arch. Sex. Behav. 2009, 38, 936–948. [Google Scholar] [CrossRef]
- Mościcki, E.K.; Clarke, D.E.; Kuramoto, S.J.; Kraemer, H.C.; Narrow, W.E.; Kupfer, D.J.; Regier, D.A. Testing DSM-5 in routine clinical practice settings: Feasibility and clinical utility. Psychiatr. Serv. 2013, 64, 952–960. [Google Scholar] [CrossRef]
- Cella, D.; Riley, W.; Stone, A.; Rothrock, N.; Reeve, B.; Yount, S.; Amtmann, D.; Bode, R.; Buysse, D.; Choi, S.; et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J. Clin. Epidemiol. 2010, 63, 1179–1194. [Google Scholar] [CrossRef]
- Cook, K.F.; Jensen, S.E.; Schalet, B.D.; Beaumont, J.L.; Amtmann, D.; Czajkowski, S.; DeWalt, D.A.; Fries, J.F.; Pilkonis, P.A.; Reeve, B.B.; et al. PROMIS measures of pain, fatigue, negative affect, physical function, and social function demonstrated clinical validity across a range of chronic conditions. J. Clin. Epidemiol 2016, 73, 89–102. [Google Scholar] [CrossRef]
- Hays, R.D.; Bjorner, J.B.; Revicki, D.A.; Spritzer, K.L.; Cella, D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual. Life Res. 2009, 18, 873–880. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- Muthén, B.; Satorra, A. Complex sample data in structural equation modeling. Sociol. Methodol. 1995, 25, 267–316. [Google Scholar] [CrossRef]
- Sullivan, M.D. Depression effects on long-term prescription opioid use, abuse, and addiction. Clin. J. Pain 2018, 34, 878–884. [Google Scholar] [CrossRef]
- Jacobson, M.L.; Wulf, H.A.; Browne, C.A.; Luci, I. Opioid modulation of cognitive impairment in depression. Prog. Brain Res. 2018, 39, 1–48. [Google Scholar]
- Hopkins, R.E.; Bui, T.; Magliano, D.; Arnold, C.; Dooley, M. Prescriber education interventions to optimize opioid prescribing in acute care: A systematic review. Pain Physician 2019, 22, 551–562. [Google Scholar] [CrossRef]
- Burden, M.; Keniston, A.; Wallace, M.A.; Busse, J.W.; Casademont, J.; Chadaga, S.R.; Chandrasekaran, S.; Cicardi, M.; Cunningham, J.M.; Filella, D.; et al. Opioid utilization and perception of pain control in hospitalized patients: A cross-sectional study of 11 sites in 8 countries. J. Hosp. Med. 2019, 14, 737–745. [Google Scholar] [CrossRef]
- Tyson, D.M.; Chavez, M.N.; Lake, P.; Gutierrez, A.; Sherry, P.; Rigg, K.K.; Marshall, V.K.; Henderson, H.; di Ciccone, B.L.; Rajasekhara, S.; et al. Perceptions of prescription opioid medication within the context of cancer survivorship and the opioid epidemic. J. Cancer Surviv. 2021. [Google Scholar] [CrossRef]
- Elliott, K.R.; Jones, E. The association between frequency of opioid misuse and opioid use disorder among youth and adults in the United States. Drug. Alcohol. Depend. 2019, 197, 73–77. [Google Scholar] [CrossRef]
- Green, K.M.; Musci, R.J.; Matson, P.A.; Johnson, R.M.; Reboussin, B.A.; Ialongo, N.S. Developmental patterns of adolescent marijuana and alcohol use and their joint association with sexual risk behavior and outcomes in young adulthood. J. Urban Health 2017, 94, 115–124. [Google Scholar] [CrossRef]
- Clayton, H.B.; Bohm, M.K.; Lowry, R.; Ashley, C.; Ethier, K.A. Prescription opioid misuse associated with risk behaviors among adolescents. Am. J. Prev. 2019, 57, 533–539. [Google Scholar] [CrossRef]
- Lorvick, J.; Browne, E.N.; Lambdin, B.H.; Comfort, M. Polydrug use patterns, risk behavior and unmet healthcare need in a community-based sample of women who use cocaine, heroin or methamphetamine. Addict. Behav. 2018, 85, 94–99. [Google Scholar] [CrossRef]
- Stein, M.D.; Kanabar, M.; Anderson, B.J.; Lembke, A.; Bailey, G.L. Reasons for benzodiazepine use among persons seeking opioid detoxification. J. Subst. Abuse Treat. 2016, 68, 57–61. [Google Scholar] [CrossRef]
- Saddleson, M.L.; Kozlowski, L.T.; Giovino, G.A.; Hawk, L.W.; Murphy, J.M.; MacLean, M.G.; Goniewicz, M.L.; Homish, G.G.; Wrotniak, B.H.; Mahoney, M.C. Risky behaviors, e-cigarette use and susceptibility of use among college students. Drug Alcohol. Depend. 2015, 149, 25–30. [Google Scholar] [CrossRef]
- Cohn, A.; Villanti, A.; Richardson, A.; Rath, J.M.; Williams, V.; Stanton, C.; Mermelstein, R. The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addict. Behav. 2015, 48, 79–88. [Google Scholar] [CrossRef]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; McHale, P.; Bennett, A.; Ireland, R.; Pike, K. Associations between e-cigarette access and smoking and drinking behaviours in teenagers. BMC Public Health 2015, 15, 244. [Google Scholar] [CrossRef]
- Sun, T.; Buchanan, A.L.; Bratberg, J.P.; Patry, E.; Matson, K.L. Rx for addiction and medication safety (RAMS-PEER): Evaluation of an education and peer program on opioid misuse. Prev. Chronic Dis. 2020, 17, E37. [Google Scholar] [CrossRef]
| College in Southeast | College in Northeast | Total | |
|---|---|---|---|
| Variable | n (Percent) | n (Percent) | n (Percent) |
| Sex assigned at birth * | |||
| Female | 246 (75.9) | 357 (68.3) | 603 (71.2) |
| Male | 78 (24.1) | 166 (31.7) | 244 (28.8) |
| Race ** | |||
| American Indian or Native Alaskan | 0 (0.0) | 1 (0.2) | 1 (0.1) |
| Asian * | 41 (12.7) | 19 (3.6) | 60 (7.1) |
| Black or African American | 22 (6.8) | 23 (4.4) | 45 (5.3) |
| Native Hawaiian or Other Pacific Islander | 1 (0.3) | 2 (0.4) | 3 (0.4) |
| White * | 231 (74.4) | 463 (88.5) | 704 (83.2) |
| Other * | 18 (5.6) | 15 (2.9) | 33 (3.9) |
| Ethnicity | |||
| Hispanic or Latinx | 26 (8.0) | 33 (6.3) | 59 (7.0) |
| Not Hispanic or Latinx | 277 (88.4) | 444 (84.9) | 730 (86.2) |
| Year in College * | |||
| Freshman | 58 (17.9) | 114 (21.8) | 172 (20.3) |
| Sophomore * | 91 (28.1) | 98 (18.7) | 189 (22.3) |
| Junior | 88 (27.2) | 143 (27.3) | 231 (27.3) |
| Senior | 80 (24.7) | 152 (29.1) | 232 (27.4) |
| Greek Status | |||
| Yes | 74 (22.8) | 153 (29.3) | 227 (26.8) |
| No | 249 (76.9) | 367 (70.2) | 616 (72.7) |
| Lifetime Prescription for Opioids | |||
| Yes | 104 (32.1) | 174 (33.3) | 278 (32.8) |
| No | 214 (66.0) | 334 (63.9) | 548 (64.7) |
| Lifetime Nonmedical Prescription Opioid Use * | |||
| Yes | 25 (7.7) | 67 (12.8) | 92 (10.9) |
| No | 284 (87.74) | 420 (80.3) | 704 (83.1) |
| Past Month Nonmedical Prescription Opioid Use | |||
| Yes | 3 (0.9) | 4 (0.8) | 7 (0.8) |
| No | 265 (81.8) | 427 (81.6) | 692 (81.7) |
| M (SD): range | M (SD): range | M (SD): range | |
| Age * (total n = 847) | 20.09 (1.28): 18–24 | 20.28 (1.42): 18–24 | 20.21 (1.37): 18–24 |
| GPA * (total n = 799) | 3.38 (0.46): 0.92–4.0 | 3.1 (0.45): 1.43–4.0 | 3.33 (0.46): 0.92–4.0 |
| College in Southeast | College in Northeast | Total | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Lifetime Nonmedical Prescription Opioid Use * | 25 | 7.7 | 67 | 12.8 | 92 | 10.9 |
| Past Month Nonmedical Prescription Opioid Use | 3 | 0.9 | 4 | 0.8 | 7 | 0.8 |
| Lifetime Prescription for Opioid Medication | 104 | 32.1 | 174 | 33.3 | 278 | 32.8 |
| Current Prescription for Opioid Medication | 3 | 0.9 | 12 | 2.2 | 15 | 1.7 |
| Lifetime History of Regularly Drinking Alcohol ** | 131 | 43.1 | 252 | 52.7 | 383 | 49.0 |
| Lifetime Marijuana Use ** | 142 | 43.2 | 321 | 62.1 | 463 | 54.7 |
| Lifetime Nonmedical Use of Benzodiazapine ** | 18 | 5.5 | 61 | 11.8 | 79 | 9.3 |
| Lifetime Nonmedical Use of Prescription Stimulants ** | 42 | 12.8 | 118 | 22.8 | 160 | 18.9 |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | ||||||||||||||||||||
| 0.071 * | 1 | |||||||||||||||||||
| 0.006 | −0.052 | 1 | ||||||||||||||||||
| −0.004 | −0.045 | −0.123 ** | 1 | |||||||||||||||||
| −0.026 | −0.002 | 0.000 | 0.027 | 1 | ||||||||||||||||
| 0.002 | −0.019 | −0.085 * | 0.070 | −0.039 | 1 | |||||||||||||||
| 0.012 | 0.041 | −0.090 * | 0.018 | 0.106 ** | −0.116 ** | 1 | ||||||||||||||
| −0.033 | 0.015 | −0.083 * | 0.043 | 0.081 * | −0.056 | 0.097 ** | 1 | |||||||||||||
| −0.071 * | 0.027 | −0.104 ** | 0.045 | 0.274 ** | −0.137 ** | 0.216 ** | 0.239 ** | 1 | ||||||||||||
| −0.031 | 0.022 | −0.144 ** | 0.023 | 0.149 ** | −0.122 ** | 0.172 ** | 0.132 ** | 0.426 ** | 1 | |||||||||||
| −0.041 | 0.056 | −0.104 ** | −0.012 | 0.129 ** | −0.183 ** | 0.354 ** | 0.129 ** | 0.300 ** | 0.379 ** | 1 | ||||||||||
| −0.034 | 0.022 | −0.122 ** | −0.027 | 0.095 ** | −0.089 * | 0.419 ** | 0.043 | 0.224 ** | 0.259 ** | 0.468 ** | 1 | |||||||||
| 0.014 | 0.061 | −0.053 | −0.065 | 0.089 | −0.001 | 0.167 ** | −0.023 | 0.082 | 0.105 * | 0.145 ** | 0.126 ** | 1 | ||||||||
| 0.006 | 0.160 ** | −0.082 | −0.053 | 0.108 * | −0.009 | 0.081 | −0.015 | 0.042 | 0.128 ** | 0.117 * | 0.126 ** | 0.698 ** | 1 | |||||||
| 0.027 | 0.049 | −0.094 * | 0.097 * | 0.074 | 0.029 | 0.096 * | 0.014 | 0.088 * | 0.121 ** | 0.122 ** | 0.139 ** | 0.220 ** | 0.232 ** | 1 | ||||||
| −0.010 | 0.103 ** | −0.069 | 0.003 | 0.046 | −0.098 * | 0.122 ** | 0.024 | 0.085 * | 0.156 ** | 0.227 ** | 0.162 ** | 0.426 ** | 0.517 ** | 0.283 ** | 1 | |||||
| −0.030 | 0.054 | −0.043 | 0.008 | 0.018 | −0.170 ** | 0.108 ** | −0.011 | 0.071 | 0.157 ** | 0.215 ** | 0.162 ** | 0.406 ** | 0.413 ** | 0.225 ** | 0.818 ** | 1 | ||||
| 0.138 ** | 0.048 | 0.004 | −0.042 | 0.057 | 0.013 | 0.071 | 0.056 | 0.022 | 0.034 | 0.035 | 0.086 | 0.037 | −0.004 | 0.006 | 0.015 | 0.057 | 1 | |||
| 0.136 ** | −0.012 | 0.087 | −0.043 | −0.035 | 0.029 | −0.013 | −0.010 | −0.044 | −0.007 | −0.071 | −0.016 | 0.041 | −0.013 | −0.050 | 0.023 | 0.014 | 0.570 ** | 1 | ||
| 0.043 | 0.111 ** | −0.005 | −0.082 | 0.046 | 0.037 | 0.033 | 0.019 | 0.002 | 0.014 | 0.005 | 0.047 | 0.068 | 0.034 | −0.034 | −0.013 | −0.006 | 0.685 ** | 0.428 ** | 1 | |
| 0.078 | 0.150 ** | −0.039 | −0.061 | 0.025 | 0.006 | 0.080 | 0.020 | 0.007 | 0.031 | 0.053 | 0.056 | 0.007 | 0.017 | −0.024 | −0.039 | −0.056 | 0.608 ** | 0.329 ** | 0.760 ** | 1 |
| Sources | College in Southeast (n = 25) | College in Northeast (n = 67) | All Colleges (n = 92) |
|---|---|---|---|
| Friends | 10 (40.0%) | 18 (26.9%) | 28 (30.4%) |
| Dentist | 3 (12.0%) | 14 (20.9%) | 17 (18.5%) |
| Primary Care MD | 3 (12.0%) | 11 (16.4%) | 14 (15.2%) |
| Bought Illegally | 5 (20.0%) | 9 (13.4%) | 14 (15.2%) |
| Parents | 5 (20.0%) | 8 (11.9%) | 13 (14.1%) |
| Urgent Care | 3 (12.0%) | 6 (9.0%) | 9 (9.8%) |
| Stole | 4 (16.0%) | 3 (4.5%) | 7 (7.6%) |
| Emergency Room | 1 (4.0%) | 5 (7.5%) | 6 (6.5%) |
| Orthopedic MD | 1 (4.0%) | 5 (7.5%) | 6 (6.5%) |
| Other | 1 (4.0%) | 2 (3.0%) | 3 (3.3%) |
| Specialist (Other) | 1 (4.0%) | 1 (1.5%) | 2 (2.2%) |
| Pain Management Specialist | 0 (0.0%) | 1 (1.5%) | 1 (1.1%) |
| Most Common Prescription Opioids Used Nonmedically | |||
| Hydrocodone (e.g., Vicodin, Lorcet) | 9 (36.0%) | 16 (23.9%) | 25 (27.2%) |
| Immediate Release Oxycodone (e.g., Roxicet, Roxicodone, Percocet) | 8 (32.0%) | 16 (23.9%) | 24 (26.1%) |
| Codeine (e.g., Tylenol 3 and 4) | 5 (20.0%) | 17 (25.4%) | 22 (23.9%) |
| Extended-Release Oxycodone (e.g., Oxycontin) | 3 (12.0%) | 10 (14.9%) | 13 (14.1%) |
| Tramadol (Ultram, Tramal) | 2 (8.0%) | 5 (7.5%) | 7 (7.6%) |
| Morphine (e.g., MS Contin, Oramorph) | 0 (0.0%) | 3 (4.5%) | 3 (3.3%) |
| Hydromorphine (e.g., Dilaudid) | 0 (0.0%) | 3 (4.5%) | 3 (3.3%) |
| Fentanyl (e.g., Duragesic, Actiq) | 0 (0.0%) | 3 (4.5%) | 3 (3.3%) |
| Buprenorphine (e.g., Suboxone, Subutex) | 0 (0.0%) | 3 (4.5%) | 3 (3.3%) |
| Methadone | 0 (0.0%) | 3 (4.5%) | 2 (2.2%) |
| Oxymorphone (e.g., Opana, Numorphan) | 1 (4.0%) | 1 (1.5%) | 2 (2.2%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Weyandt, L.L.; Gudmundsdottir, B.G.; Shepard, E.; Brick, L.; Buchanan, A.; Clarkin, C.; Francis, A.; Marraccini, M. Nonmedical Prescription Opioid Use among a Sample of College Students: Prevalence and Predictors. Pharmacy 2021, 9, 106. https://doi.org/10.3390/pharmacy9020106
Weyandt LL, Gudmundsdottir BG, Shepard E, Brick L, Buchanan A, Clarkin C, Francis A, Marraccini M. Nonmedical Prescription Opioid Use among a Sample of College Students: Prevalence and Predictors. Pharmacy. 2021; 9(2):106. https://doi.org/10.3390/pharmacy9020106
Chicago/Turabian StyleWeyandt, Lisa L., Bergljót Gyda Gudmundsdottir, Emily Shepard, Leslie Brick, Ashley Buchanan, Christine Clarkin, Alyssa Francis, and Marisa Marraccini. 2021. "Nonmedical Prescription Opioid Use among a Sample of College Students: Prevalence and Predictors" Pharmacy 9, no. 2: 106. https://doi.org/10.3390/pharmacy9020106
APA StyleWeyandt, L. L., Gudmundsdottir, B. G., Shepard, E., Brick, L., Buchanan, A., Clarkin, C., Francis, A., & Marraccini, M. (2021). Nonmedical Prescription Opioid Use among a Sample of College Students: Prevalence and Predictors. Pharmacy, 9(2), 106. https://doi.org/10.3390/pharmacy9020106






