A De Novo Pharmacist-Family Physician Collaboration Model in a Family Medicine Clinic in Alberta, Canada
Abstract
1. Introduction
2. Materials and Methods
3. Results
- Monitored blood pressure and adjusted antihypertensives as appropriate;
- Tapered or titrated antidepressants or requested a referral to mental health counselling;
- Monitored thyroid function tests and adjusted medications as appropriate;
- Recommended or prescribed appropriate antibiotics for community infections such as otitis media, urinary tract infection or cellulitis;
- Adjusted dosage or discontinued medication due to organ dysfunction or failure such as renal insufficiency;
- Tapered or titrated opiates;
- Tapered benzodiazepines;
- Deprescribed proton pump inhibitors;
- Adjusted dosage of medications for diabetes.
4. Discussion
4.1. Strength
4.2. Limitation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Framework for Action on Interprofessional Education and Collaborative Practice; World Health Organization: Geneva, Switzerland, 2010; Available online: https://apps.who.int/iris/bitstream/handle/10665/70185/WHO_HRH_HPN_10.3_eng.pdf?sequence=1 (accessed on 17 August 2020).
- Zwarenstein, M.; Goldman, J.; Reeves, S. Interprofessional collaboration: Effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst. Rev. 2009, CD000072. [Google Scholar] [CrossRef]
- Tannenbaum, D.; Kerr, J.; Konkin, J.; Organek, A.; Parsons, E.; Saucier, D.; Shaw, L.; Walsh, A. Triple C Competency-Based Curriculum. Report of the Working Group on Postgraduate Curriculum Review—Part 1; College of Family Physicians of Canada: Mississauga, ON, Canada, 2011; Available online: www.cfpc.ca/uploadedFiles/Education/_PDFs/WGCR_TripleC_Report_English_Final_18Mar11.pdf (accessed on 17 August 2020).
- Frank, J.R. (Ed.) The CanMEDS 2005 Physician Competency Framework. Better Standards. Better Physicians. Better Care; Royal College of Physicians and Surgeons of Canada: Ottawa, ON, Canada, 2005; Available online: http://www.ub.edu/medicina_unitateducaciomedica/documentos/CanMeds.pdf (accessed on 17 August 2020).
- Association of Faculties of Medicine of Canada. The Future of Medical Education in Canada (FMEC): A Collective Vision for MD Education; Association of Faculties of Medicine of Canada: Ottawa, ON, Canada, 2010; Available online: https://afmc.ca/sites/default/files/pdf/2010-FMEC-MD_EN.pdf (accessed on 17 August 2020).
- Accreditation Standards for Canadian First Professional Degree in Pharmacy Programs. 2018. Available online: https://ccapp-accredit.ca/wp-content/uploads/2016/01/Accreditation-Standards-for-Canadian-First-Professional-Degree-in-Pharmacy-Programs.pdf (accessed on 17 August 2020).
- Centers for Disease Control and Prevention. Collaborative Practice Agreements and Pharmacists’ Patient Care Services; US Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2012. [Google Scholar]
- Rodis, J.L.; Sevin, A.; Awad, M.H.; Porter, B.; Glasgow, K.; Fox, C.H.; Pryor, B. Improving chronic disease outcomes through medication therapy management in federally qualified health centers. J. Prim. Care Community Health 2017. [Google Scholar] [CrossRef] [PubMed]
- Haag, J.D.; Stratton, T.P. Patient care services in rural Minnesota community pharmacies. J. Am. Pharm. Assoc. 2010, 50, 508–516. [Google Scholar] [CrossRef]
- McDonough, R.P.; Harthan, A.A.; McLeese, K.E.; Doucette, W.R. Retrospective financial analysis of medication therapy management services from the pharmacy’s perspective. J. Am. Pharm. Assoc. 2010, 50, 62–66. [Google Scholar] [CrossRef]
- Canadian Pharmacists Association. Pharmacists’ Expanded Scope of Practice. Available online: https://www.pharmacists.ca/cpha-ca/assets/File/newsevents/ExpandedScopeChart_June2015_EN.pdf (accessed on 17 August 2020).
- Alberta College of Pharmacy. The Health Professional’s Guide to Pharmacists Prescribing. Available online: https://abpharmacy.ca/sites/default/files/HPGuidePrescribing.pdf (accessed on 17 August 2020).
- Bryant, L.J.; Coster, G.; Gamble, G.D.; McCormick, R.N. General practitioners’ and pharmacists’ perceptions of the role of community pharmacists in delivering clinical services. Res. Soc. Adm. Pharm. 2009, 5, 347–362. [Google Scholar] [CrossRef]
- Laubscher, T.; Evans, C.; Blackburn, D.; Taylor, J.; Mckay, S. Collaboration between family physicians and community pharmacists to enhance adherence to chronic medications. Opinions of Saskatchewan family physicians. Can. Fam. Physician 2009, 55, e69–e75. [Google Scholar]
- LaLonde, L.; Hudon, É.; Goudreau, J.; Bélanger, D.; Villeneuve, J.; Perreault, S.; Blais, L.; Lamarre, D. Physician-pharmacist collaborative care in dyslipidemia management: The perception of clinicians and patients. Res. Soc. Adm. Pharm. 2011, 7, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Howard, M.; Trim, K.; Woodward, C.; Dolovich, L.; Sellors, C.; Kaczorowski, J.; Sellors, J. Collaboration between community pharmacists and family physicians: Lessons learned from the seniors medication assessment research trial. J. Am. Pharm. Assoc. 2003, 43, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, J.E.; Graber, G.; Saltiel, E.; Wallace, J.; Ryu, S.; Jackson, A.; Deutsch, S.; Weingarten, S.R. Physician-pharmacist co-management of hypertension: A randomized, comparative trial. Pharmacotherapy 2003, 23, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Hunt, J.S.; Siemienczuk, J.; Pape, G.; Rozenfeld, Y.; MacKay, J.; LeBlanc, B.H.; Touchette, D. A randomized controlled trial of team-based care: Impact of physician-pharmacist collaboration on uncontrolled hypertension. J. Gen. Intern. Med. 2008, 23, 1966–1972. [Google Scholar] [CrossRef]
- Carter, B.L.; Bergus, G.R.; Dawson, J.D.; Farris, K.B.; Doucette, W.R.; Chrischilles, E.A.; Hartz, A.J. A cluster randomized trial to evaluate physician/pharmacist collaboration to improve blood pressure control. J. Clin. Hypertens. 2008, 10, 260–271. [Google Scholar] [CrossRef]
- Carter, B.L.; Ardery, G.; Dawson, J.D.; James, P.A.; Bergus, G.R.; Doucette, W.R.; Chrischilles, E.A.; Franciscus, C.L.; Xu, Y. Physician and pharmacist collaboration to improve blood pressure control. Arch. Intern. Med. 2009, 169, 1996–2002. [Google Scholar] [CrossRef]
- Weber, C.A.; Ernst, M.E.; Sezate, G.S.; Zheng, S.; Carter, B.L. Pharmacist-physician co-management of hypertension and reduction in 24-h ambulatory blood pressures. Arch. Intern. Med. 2010, 170, 1634–1639. [Google Scholar] [CrossRef]
- Hirsch, J.D.; Steers, N.; Adler, D.S.; Kuo, G.M.; Morello, C.M.; Lang, M.; Singh, R.F.; Wood, Y.; Kaplan, R.M.; Mangione, C.M. Primary care-based, pharmacist-physician collaborative medication-therapy management of hypertension: A randomized, pragmatic trial. Clin. Ther. 2014, 36, 1244–1254. [Google Scholar] [CrossRef]
- Carter, B.L.; Coffey, C.S.; Ardery, G.; Uribe, L.; Ecklund, D.; James, P.; Egan, B.; Weg, M.V.; Chrischilles, E.; Vaughn, T. Cluster-randomized trial of a physician/pharmacist collaborative model to improve blood pressure control. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 235–243. [Google Scholar] [CrossRef]
- Sisson, E.M.; Dixon, D.L.; Kildow, D.C.; Van Tassell, B.W.; Carl, D.E.; Varghese, D.; Electricwala, B.; Carroll, N.V. Effectiveness of a pharmacist-physician team-based collaboration to improve long term blood pressure control at an inner-city safety-net clinic. Pharmacotherapy 2016, 36, 342–347. [Google Scholar] [CrossRef]
- Kiel, P.J.; McCord, A.D. Pharmacist impact on clinical outcomes in a diabetes disease management program via collaborative practice. Ann. Pharmacother. 2005, 39, 1828–1832. [Google Scholar] [CrossRef] [PubMed]
- Farland, M.Z.; Byrd, D.C.; McFarland, M.S.; Thomas, J.; Franks, A.S.; George, C.M.; Gross, B.N.; Guirguis, A.B.; Suda, K.J. Pharmacist-physician collaboration for diabetes care: The diabetes initiative program. Ann. Pharmacother. 2013, 47, 781–789. [Google Scholar] [CrossRef]
- Howard-Thompson, A.; Farland, M.Z.; Byrd, D.C.; Airee, A.; Thomas, J.; Campbell, J.; Cassidy, R.; Morgan, T.; Suda, K.J. Pharmacist physician collaboration for diabetes care: Cardiovascular outcomes. Ann. Pharmacother. 2013, 47, 1471–1477. [Google Scholar] [CrossRef]
- Hou, K.; Yang, H.; Ye, Z.; Wang, Y.; Liu, L.; Cui, X. Effectiveness of pharmacist-led anticoagulation management on clinical outcomes: A systematic review and meta-analysis. J. Pharm. Pharm. Sci. 2017, 20, 378–396. [Google Scholar] [CrossRef]
- Griffith, R.J.; Alsweiler, J.; Moore, A.E.; Brown, S.; Middleton, P.; Shepherd, E.; Crowther, C. Interventions to prevent women from developing gestational diabetes mellitus: An overview of Cochrane Reviews. Cochrane Database Syst. Rev. 2020, 6, CD012394. [Google Scholar] [CrossRef]
- De Barra, M.; Scott, C.; Scott, N.W.; Johnston, M.; De Bruin, M.; Nkansah, N.; Bond, C.M.; Matheson, C.; Rackow, P.; Williams, A.J.; et al. Pharmacist services for non-hospitalised patients. Cochrane Database Syst. Rev. 2018, 9, CD013102. [Google Scholar] [CrossRef]
- Canadian Medical Association. Family Medicine Profile. Available online: https://www.cma.ca/sites/default/files/family-e.pdf (accessed on 13 May 2021).
- Brown, D.C. Family practice—What’s the difference? Can. Fam. Phyisician 1979, 25, 1484–1487. [Google Scholar]
- Tan, E.C.; Stewart, K.; Elliott, R.A.; George, J. Pharmacist consultations in general practice clinics: The pharmacists in practice study (PIPS). Res. Soc. Adm. Pharm. 2014, 10, 623–632. [Google Scholar] [CrossRef]
- Khaira, M.; Mathers, A.; Gerard, N.B.; Dolovich, L. The evolving role and impact of integrating pharmacists into primary care teams: Experience from Ontario, Canada. Pharmacy 2020, 8, 234. [Google Scholar] [CrossRef] [PubMed]
- Hwang, A.Y.; Gums, T.H.; Gums, J.G. The benefits of physicians-pharmacist collaboration. J. Fam. Pract. 2017, 66, E1–E8. [Google Scholar]
- Hughes, C.M.; McCann, S. Perceived interprofessional barriers between community pharmacists and general practitioners: A qualitative assessment. Br. J. Gen. Pract. 2003, 53, 600–606. [Google Scholar] [PubMed]
- Donovan, A.L.; Aldrich, J.M.; Gross, A.K.; Barchas, D.M.; Thornton, K.C.; Schell-Chaple, H.M.; Gropper, M.A.; Lipshutz, A.K. Interprofessional care and teamwork in the ICU. Crit. Care Med. 2018, 46, 980–990. [Google Scholar] [CrossRef]
- Lee, H.; Ryu, K.; Sohn, Y.; Kim, J.; Suh, G.Y.; Kim, E.Y. Impact on patient outcomes of pharmacist participation in multidisciplinary critical care teams: A systematic review and meta-analysis. Crit. Care Med. 2019, 47, 1243–1250. [Google Scholar] [CrossRef] [PubMed]
- Rudis, M.I.; Brandl, K.M. Position paper on critical care pharmacy services. Society of Critical Care medicine and American College of Clinical Pharmacy Task Force on Critical Care of Pharmacy Services. Crit. Care Med. 2000, 28, 3746–3750. [Google Scholar] [CrossRef] [PubMed]
- Shiyanbola, O.O.; Farris, K.B. Concerns and beliefs about medicines and inappropriate medications: An internet-based surbey on risk factors for self-reported adverse drug events among the older adults. Am. J. Geriatr. Pharmacother. 2010, 8, 245–257. [Google Scholar] [CrossRef]
- Weber, C.A.; Leloux, M.R.; Carter, B.L.; Farris, K.B.; Xu, Y. Reduction in adverse symptoms as blood pressure becomes controlled. Pharmacotherapy 2008, 28, 1104–1114. [Google Scholar] [CrossRef]
- Neafsey, P.J.; M’lan, C.E.; Ge, M.; Walsh, S.J.; Lin, C.A.; Anderson, E. Reducing adverse self-medication behaviors in older adults with hypertension: Results of an e-health clinical efficacy trial. Ageing Int. 2011, 36, 159–191. [Google Scholar] [CrossRef]
- Bungard, T.J.; Gardner, L.; Archer, S.L.; Hamilton, P.; Ritchie, B.; Tymchak, W.; Tsuyuki, R.T. Evaluation of a pharmacist-managed anticoagulation clinic: Improving patient care. Open Med. 2009, 3, e18–e21. [Google Scholar]
- Ingram, S.J.; Kirkdale, C.L.; Williams, S.; Hartley, E.; Wintle, S.; Sefton, V.; Thornley, T. Moving anticoagulation initiation and monitoring services into the community: Evaluation of the Brighton and Hove community pharmacy service. BMC Health Serv. Res. 2018, 18, 91. [Google Scholar] [CrossRef]
- Schilling, J.; Kaatz, S.; Hudson, M.; Krol, G.D.; Szandzik, E.G.; Kalus, J. Clinical and safety impact of an inpatient pharmacist-directed anticoagulation service. J. Hosp. Med. 2011, 6, 322–328. [Google Scholar] [CrossRef]
- Milosavljevic, A.; Aspden, T.; Harrison, J. Community pharmacist-led interventions and their impact on patients’ medication adherence and other health outcomes: A systematic review. Int. J. Pharm. Pract. 2018, 26, 387–397. [Google Scholar] [CrossRef]
- McAlister, F.A.; Majumdar, S.R.; Padwal, R.S.; Fradette, M.; Thompson, A.; Buck, B.; Dean, N.; Bakal, J.A.; Tsuyuki, R.; Grover, S.; et al. Case management for blood pressure and lipid level control after minor stroke: PREVENTION randomized controlled trial. CMAJ 2014, 186, 577–584. [Google Scholar] [CrossRef]
| Family Physician | Primary Care Physician |
|---|---|
| 1. Continuous relationship with the patients | 1. Practice is limited to selected medical condition |
| 2.First contact physician for patients with any medical problems | 2. Refer patients to other specialists who have medical condition outside of their scope of practice. |
| 3. The family is a unit of care | 3. Fragmented patient care |
| 4. Coordinating with other specialists | 4. Do not take the holistic approach |
| 5. Screening and prevent diseases such as cancer | 5. Greater risk of polypharmacy and drug interactions |
| 6. Continuity of care | |
| 7. Established long-term patient/physician relationship with the patient and family | |
| 8. Use holistic approach | |
| 9. Large volume of patients | |
| 10. Diverse practice |
| Demographics | |
|---|---|
| Patients | 159 |
| Age range | 19–94 |
| Average age | 62 |
| Male | 76 |
| Female | 83 |
| Past Medical History | |
| HTN | 57 |
| Mental Health | 32 |
| DM | 22 |
| Chronic pain | 22 |
| Hypothyroidism | 17 |
| Dyslipidemia | 14 |
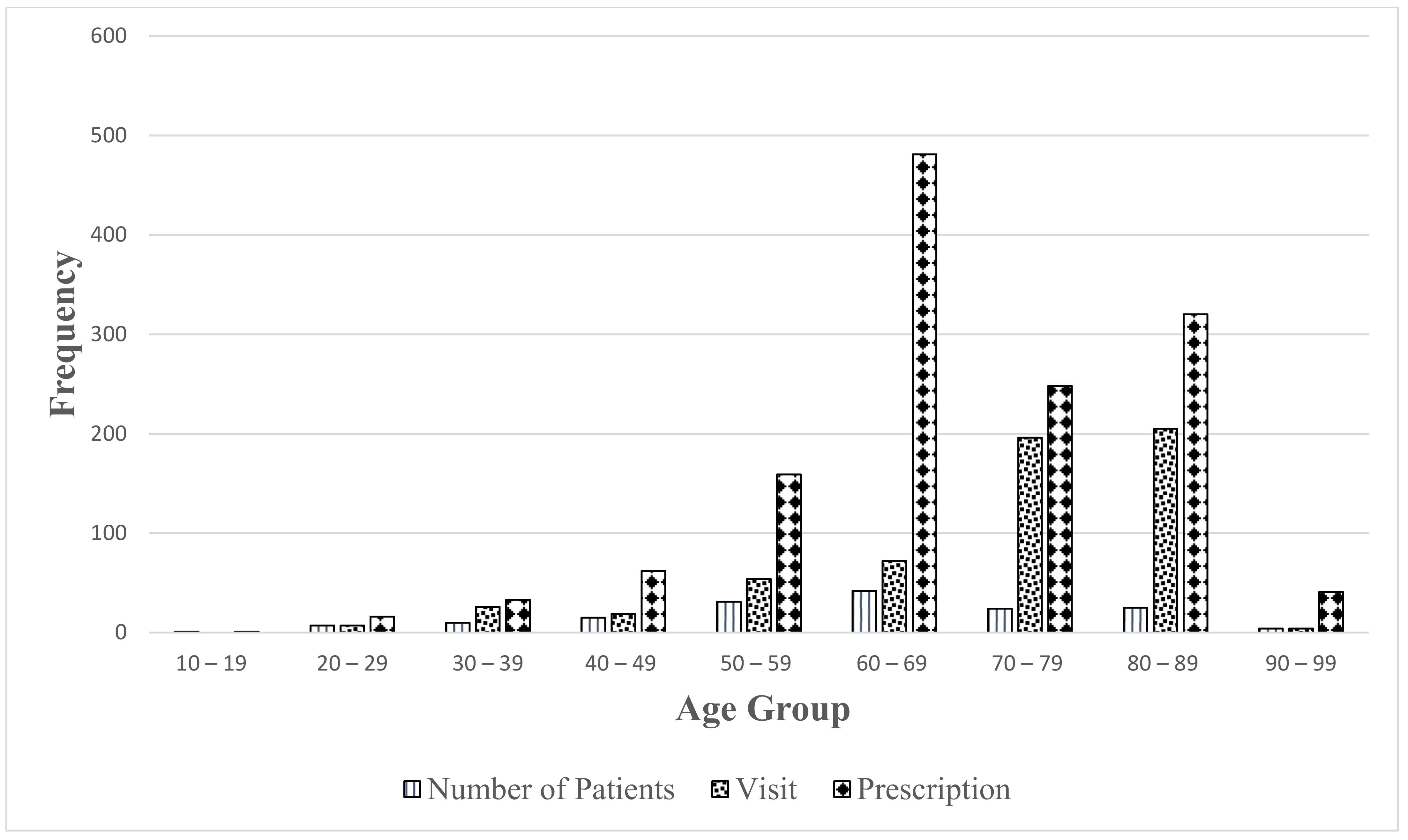
| Visit | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | Total |
|---|---|---|---|---|---|---|---|---|
| Independent (%) | 41(61) | 21(21) | 15(25) | 20(25) | 31 (30) | 74(51) | 18(69) | 220(38) |
| Total visits | 67 | 101 | 61 | 80 | 105 | 143 | 26 | 583 |
| Prescriptions | 97 | 121 | 162 | 207 | 282 | 353 | 139 | 1361 |
| Prescription/visit | 1.4 | 1.2 | 2.7 | 2.6 | 2.7 | 2.5 | 5.3 | 2.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banh, H.L.; Cave, A.J. A De Novo Pharmacist-Family Physician Collaboration Model in a Family Medicine Clinic in Alberta, Canada. Pharmacy 2021, 9, 107. https://doi.org/10.3390/pharmacy9020107
Banh HL, Cave AJ. A De Novo Pharmacist-Family Physician Collaboration Model in a Family Medicine Clinic in Alberta, Canada. Pharmacy. 2021; 9(2):107. https://doi.org/10.3390/pharmacy9020107
Chicago/Turabian StyleBanh, Hoan Linh, and Andrew J. Cave. 2021. "A De Novo Pharmacist-Family Physician Collaboration Model in a Family Medicine Clinic in Alberta, Canada" Pharmacy 9, no. 2: 107. https://doi.org/10.3390/pharmacy9020107
APA StyleBanh, H. L., & Cave, A. J. (2021). A De Novo Pharmacist-Family Physician Collaboration Model in a Family Medicine Clinic in Alberta, Canada. Pharmacy, 9(2), 107. https://doi.org/10.3390/pharmacy9020107





