Pharmaceutical Discharge Management: Implementation in Swiss Hospitals Compared to International Guidelines
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
2.2. Data Analysis
3. Results
3.1. Survey
3.1.1. Interventions Conducted by Healthcare Professionals to Support Patients at Hospital Discharge
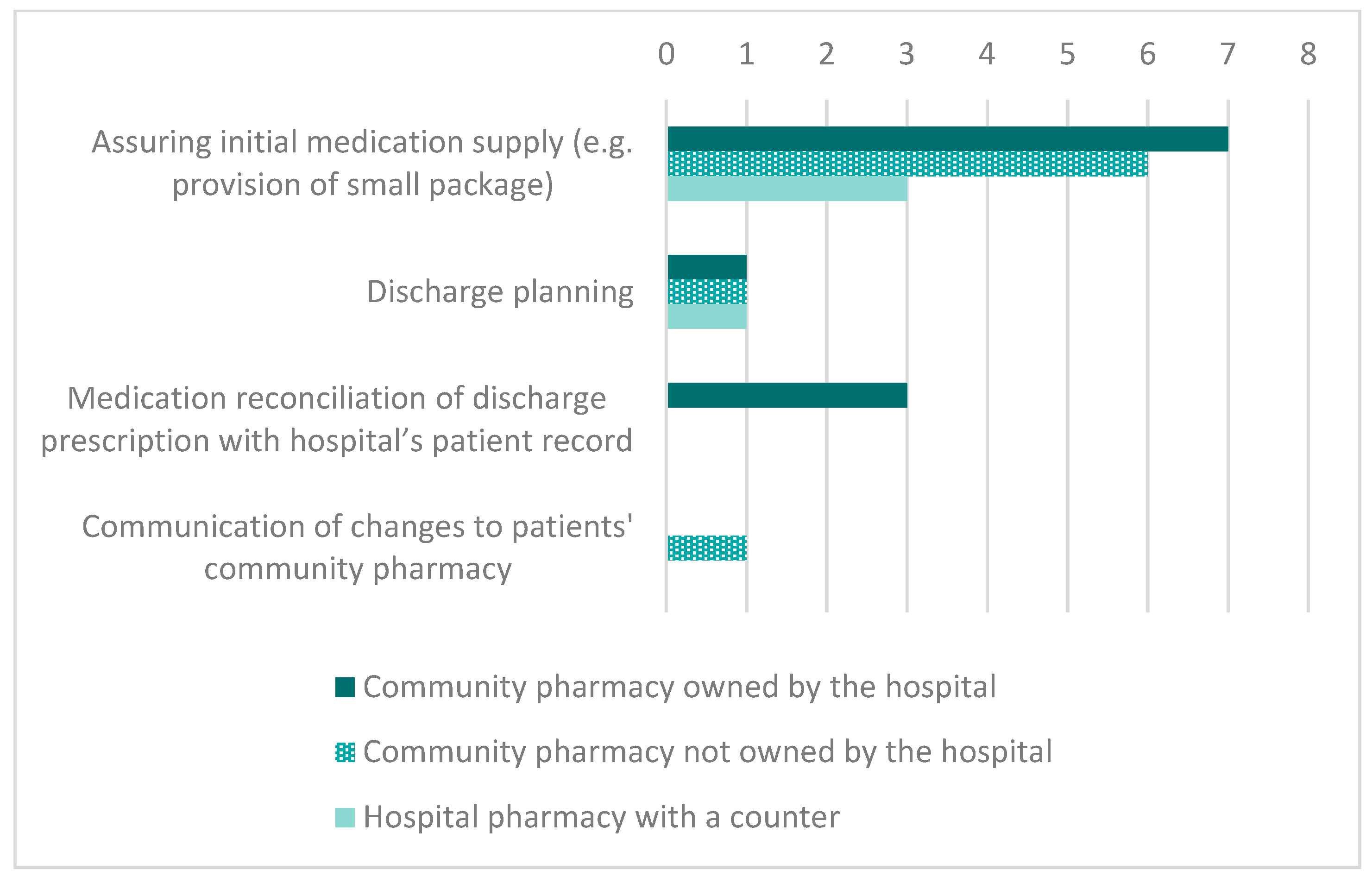
3.1.2. Collaboration with a Community Pharmacy
3.2. Interviews
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Cochrane Search
Appendix B. Guideline Search
- -
- Clinical guideline and hospital discharge and *
- -
- Guideline * continuity OR aftercare OR handoff OR transfer OR handover OR “transitional OR care” OR “seamless OR care” OR transition OR “hospital discharge” -covid-19
References
- Berry, J.G.; Gay, J.C.; Maddox, K.J.; Coleman, E.A.; Bucholz, E.M.; O’Neill, M.R.; Blaine, K.; Hall, M. Age trends in 30 day hospital readmissions: US national retrospective analysis. BMJ 2018, 360, k497. [Google Scholar] [CrossRef]
- El Morabet, N.; Uitvlugt, E.B.; van den Bemt, B.J.; van den Bemt, P.M.; Janssen, M.J.; Karapinar-Çarkit, F. Prevalence and Preventability of Drug-Related Hospital Readmissions: A Systematic Review. J. Am. Geriatr. Soc. 2018, 66, 602–608. [Google Scholar] [CrossRef]
- Hawes, E.M.; Pinelli, N.R.; Sanders, K.A.; Lipshutz, A.M.; Tong, G.; Sievers, L.S.; Chao, S.; Gwynne, M. Post-Hospital Discharge Care: A Retrospective Cohort Study Exploring the Value of Pharmacist-Enhanced Care and Describing Medication-Related Problems. North Carol. Med. J. 2018, 79, 4–13. [Google Scholar] [CrossRef][Green Version]
- Kripalani, S.; Roumie, C.L.; Dalal, A.K.; Cawthon, C.; Businger, A.; Eden, S.K.; Shintani, A.; Sponsler, K.C.; Harris, L.J.; Theobald, C.N.; et al. Effect of a Pharmacist Intervention on Clinically Important Medication Errors After Hospital Discharge. Ann. Intern. Med. 2012, 157, 1–10. [Google Scholar] [CrossRef]
- De Oliveira, G.S.; Castro-Alves, L.J.; Kendall, M.C.; McCarthy, R. Effectiveness of Pharmacist Intervention to Reduce Medication Errors and Health-Care Resources Utilization After Transitions of Care. J. Patient Saf. 2017, 10. [Google Scholar] [CrossRef]
- Mekonnen, A.B.; McLachlan, A.J.; Brien, J.-a.E. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: A systematic review and meta-analysis. BMJ Open 2016, 6, e010003. [Google Scholar] [CrossRef]
- Daliri, S.; Hugtenburg, J.G.; Ter Riet, G.; van den Bemt, B.J.F.; Buurman, B.M.; Reimer, W.J.M.S.O.; Van Buul-Gast, M.-C.; Karapinar-Çarkit, F. The effect of a pharmacy-led transitional care program on medication-related problems post-discharge: A before—After prospective study. PLoS ONE 2019, 14, e0213593. [Google Scholar] [CrossRef] [PubMed]
- Bonetti, A.F.; Reis, W.C.; Lombardi, N.F.; Mendes, A.M.; Netto, H.P.; Rotta, I.; Fernandez-Llimos, F.; Pontarolo, R. Pharmacist-led discharge medication counselling: A scoping review. J. Eval. Clin. Pract. 2018, 24, 570–579. [Google Scholar] [CrossRef]
- Capiau, A.; Foubert, K.; Van Der Linden, L.; Walgraeve, K.; Hias, J.; Spinewine, A.; Sennesael, A.-L.; Petrovic, M.; Somers, A.; Belgian Society for Gerontology and Geriatrics (BSGG). Medication Counselling in Older Patients Prior to Hospital Discharge: A Systematic Review. Drugs Aging 2020, 37, 635–655. [Google Scholar] [CrossRef]
- Tomlinson, J.; Cheong, V.-L.; Fylan, B.; Silcock, J.; Smith, H.; Karban, K.; Blenkinsopp, A. Successful care transitions for older people: A systematic review and meta-analysis of the effects of interventions that support medication continuity. Age Ageing 2020, 49, 558–569. [Google Scholar] [CrossRef]
- Leppin, A.L.; Gionfriddo, M.R.; Kessler, M.; Brito, J.P.; Mair, F.S.; Gallacher, K.; Wang, Z.; Erwin, P.J.; Sylvester, T.; Boehmer, K.; et al. Preventing 30-day hospital readmissions: A systematic review and meta-analysis of randomized trials. JAMA Intern. Med. 2014, 174, 1095–1107. [Google Scholar] [CrossRef]
- Studer, H.; Boeni, F.; Messerli, M.; Hersberger, K.E.; Lampert, M.L. Clinical pharmacy activities in Swiss hospitals: How have they evolved from 2013 to 2017? Pharmacy 2020, 8, 19. [Google Scholar] [CrossRef]
- Bundesgesetz über Arzneimittel und Medizinprodukte. Available online: https://www.admin.ch/ch/d/sr/8/812.21.de.pdf (accessed on 10 January 2021).
- Swiss Association of Public Health Administration and Hospital Pharmacists. Berufsbild des Spitalapothekers und Leitbild für Seine Weiterbildung. Available online: https://www.gsasa.ch/deliver.cfm?f=0CD89DA59212A7CBAEDB92D04866B8AB822D41B39CAE138ABE7A989FD2DB9A692B80BC5080BEBBCC6E97CABFB3488583E3A496F8AB8ED38C9B9F47BFBA04939D4D0AA14FBA9BB7ABAD1792ABEA5CCF75ED56AEBF87BB575C4E939F8DFE5E26BD5BDB7205173B05ACDFCBF495A8FC&type=.pdf (accessed on 9 January 2021).
- pharmaSuisse. Weiterbildungsprogramm zum Fähigkeitsausweis FPH in klinischer Pharmazie. Available online: https://www.gsasa.ch/de/bildung-de/fph-klinische-pharmazie/weiterbildungsprogramm/?oid=10149&lang=de (accessed on 9 January 2021).
- Bruhwiler, L.D.; Beeler, P.E.; Boni, F.; Giger, R.; Wiedemeier, P.G.; Hersberger, K.E.; Lutters, M. A RCT evaluating a pragmatic in-hospital service to increase the quality of discharge prescriptions. Int. J. Qual. Health Care 2019. [Google Scholar] [CrossRef]
- Hansen, L.O.; Young, R.S.; Hinami, K.; Leung, A.; Williams, M.V. Interventions to reduce 30-day rehospitalization: A systematic review. Ann. Intern. Med. 2011, 155, 520–528. [Google Scholar] [CrossRef]
- Coleman, E.A.; Parry, C.; Chalmers, S.; Min, S.J. The care transitions intervention: Results of a randomized controlled trial. Arch. Intern. Med. 2006, 166, 1822–1828. [Google Scholar] [CrossRef]
- Bobay, K.; Bahr, S.J.; Weiss, M.E.; Hughes, R.; Costa, L. Models of discharge care in Magnet(R) hospitals. J. Nurs. Adm. 2015, 45, 485–491. [Google Scholar] [CrossRef]
- Pedersen, C.A.; Schneider, P.J.; Scheckelhoff, D.J. ASHP national survey of pharmacy practice in hospital settings: Dispensing and administration--2014. Am. J. Health-Syst. Pharm. 2015, 72, 1119–1137. [Google Scholar] [CrossRef] [PubMed]
- Cawthon, C.; Walia, S.; Osborn, C.Y.; Niesner, K.J.; Schnipper, J.L.; Kripalani, S. Improving care transitions: The patient perspective. J. Health Commun. 2012, 17 (Suppl. S3), 312–324. [Google Scholar] [CrossRef]
- Pedersen, C.A.; Schneider, P.J.; Scheckelhoff, D.J. ASHP national survey of pharmacy practice in hospital settings: Monitoring and patient education--2012. Am. J. Health-Syst. Pharm. 2013, 70, 787–803. [Google Scholar] [CrossRef]
- Johnson, A.; Sandford, J.; Tyndall, J. Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home. Cochrane Database Syst. Rev. 2003, 2003, CD003716. [Google Scholar] [CrossRef]
- Goncalves-Bradley, D.C.; Lannin, N.A.; Clemson, L.M.; Cameron, I.D.; Shepperd, S. Discharge planning from hospital. Cochrane Database Syst. Rev. 2016, 1, CD000313. [Google Scholar] [CrossRef]
- Mistiaen, P.; Poot, E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst. Rev. 2006, CD004510. [Google Scholar] [CrossRef]
- National Institute for Health and Care Exellence. Transition between Inpatient Hospital Settings and Community or Care Home Settings for Adults with Social Care Needs. Available online: https://www.nice.org.uk/guidance/ng27/evidence/full-guideline-pdf-2185185565 (accessed on 17 September 2020).
- Royal Pharmaceutical Society. Keeping Patients Safe When They Transfer between Care Providers—Getting the Medicines Right. Available online: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Publications/Keeping%20patients%20safe%20transfer%20of%20care%20report.pdf (accessed on 17 September 2020).
- Alper, E.; O’Malley, T.A.; Greenwald, J. UptoDate: Hospital Discharge and Readmission. Available online: https://www.uptodate.com/contents/hospital-discharge-and-readmission#H19 (accessed on 17 September 2020).
- Head of Clinical Services–Community Hospitals and Transitional Care, Lincolnshire Community Health Services. Admission, Discharge and Transfer Policy for Community Hospitals. Available online: https://www.lincolnshirecommunityhealthservices.nhs.uk/application/files/7115/4221/1756/P_CS_06_Admission_Discharge_and_Transfer_Policy.pdf (accessed on 17 September 2020).
- Health Service Executive National Integrated Care Advisory Group. Integrated Care Guidance: A Practical Guide to Discharge and Transfer from Hospital. Available online: https://www.hse.ie/eng/about/who/qid/resourcespublications/nationalintegratedcareguidance.pdf (accessed on 17 September 2020).
- Aneurin Bevan University Health Board. Discharge Policy. Available online: http://www.wales.nhs.uk/sitesplus/documents/866/FOI%2017076%20Enclosure.pdf (accessed on 17 September 2020).
- Head of Capacity & Corporate Nursing. Policy & Procedure for Discharge Practices. Available online: https://hgs.uhb.nhs.uk/wp-content/uploads/Discharge-Practices-Policy.pdf (accessed on 17 September 2020).
- Change Agent Team, National Leadership and Innovation Agency for Healthcare. Passing the Baton: A Practical Guide to Effective Discharge Planning. Available online: https://www.adss.cymru/en/blog/post/passing-the-baton-a-practical-guide-to-effective-discharge-planning (accessed on 17 September 2020).
- Agency for Healthcare Research and Quality. Care Transitions from Hospital to Home: IDEAL Discharge Planning. Available online: https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/engagingfamilies/strategy4/Strat4_Implement_Hndbook_508_v2.pdf (accessed on 17 September 2020).
- Registered Nurses’ Association of Ontario. Care Transitions—Clinical Best Practice Guidelines. Available online: https://rnao.ca/sites/rnao-ca/files/Care_Transitions_BPG.pdf (accessed on 17 September 2020).
- Health Quality Ontario. Adopting a Common Approach to Transitional Care Planning: Helping Health Links Improve Transitions and Coordination of Care. Available online: http://www.hqontario.ca/Portals/0/documents/qi/health-links/bp-improve-package-traditional-care-planning-en.pdf (accessed on 17 September 2020).
- The Society of Hospital Pharmacists of Australia. Compiled Quick Guides SHPA. Available online: https://www.shpa.org.au/sites/default/files/uploaded-content/website-content/SOP/quick_guides_e-book_2013.pdf (accessed on 17 September 2020).
- The Society of Hospital Pharmacists of Australia. Chapter 6: Facilitating Continuity of Medication Management on Transition between Care Settings. Available online: https://www.shpa.org.au/sites/default/files/uploaded-content/website-content/SOP/sop_clinical_pharmacy_s26-s28_chapter6.pdf (accessed on 17 September 2020).
- New Zealand HealthCare Pharmacists’ Association. Clinical Pharmacy Guidelines. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwiFvaujlvDrAhVKDuwKHbs1Dmc4ChAWMAV6BAgGEAE&url=http%3A%2F%2Fwww.nzhpa.org.nz%2Fmedia%2F1379%2Fclinguide_07.pdf&usg=AOvVaw33_bwFGOQJ9MR5NxKT_JW6 (accessed on 17 September 2020).
- Health & Social Care Joint Unit and Change Agents Team. Discharge from Hospital: Pathway, Process and Practice. Available online: http://www.wales.nhs.uk/sitesplus/documents/829/DoH%20-%20Discharge%20Pathway%202003.PDF (accessed on 17 September 2020).
- Department of Health, Government of South Australia. Continuity in Medication Management—A Handbook for South Australian Hospitals. Available online: https://www.sahealth.sa.gov.au/wps/wcm/connect/e055bd8044fd8fc2aff7efcfa5ded0ab/Pharmaceutical+Reform+Handbook+V7_Print+version.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-e055bd8044fd8fc2aff7efcfa5ded0ab-n5iXGmp (accessed on 17 September 2020).
- Pedersen, C.A.; Schneider, P.J.; Ganio, M.C.; Scheckelhoff, D.J. ASHP national survey of pharmacy practice in hospital settings: Monitoring and patient education—2018. Am. J. Health-Syst. Pharm. 2019, 76, 1038–1058. [Google Scholar] [CrossRef] [PubMed]
- Ravn-Nielsen, L.V.; Duckert, M.L.; Lund, M.L.; Henriksen, J.P.; Nielsen, M.L.; Eriksen, C.S.; Buck, T.C.; Pottegard, A.; Hansen, M.R.; Hallas, J. Effect of an in-hospital multifaceted clinical pharmacist intervention on the risk of readmission: A randomized clinical trial. JAMA Intern. Med. 2018, 178, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Bonetti, A.; Bagatim, B.; Mendes, A.; Rotta, I.; Reis, R.; Fávero, M.; Fernandez-Llimós, F.; Pontarolo, R. Impact of discharge medication counseling in the cardiology unit of a tertiary hospital in Brazil: A randomized controlled trial. Clinics 2018, 73. [Google Scholar] [CrossRef]
- Gillespie, U.; Alassaad, A.; Henrohn, D.; Garmo, H.; Hammarlund-Udenaes, M.; Toss, H.; Kettis-Lindblad, A.; Melhus, H.; Morlin, C. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: A randomized controlled trial. Arch Intern. Med. 2009, 169, 894–900. [Google Scholar] [CrossRef] [PubMed]
- Horák, P.; Gibbons, N.; Sýkora, J.; Batista, A.; Underhill, J. EAHP statements survey 2016: Sections 1, 3 and 4 of the European Statements of Hospital Pharmacy. Eur. J. Hosp. Pharm. 2017, 24, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Ooi, C.E.; Rofe, O.; Vienet, M.; Elliott, R.A. Improving communication of medication changes using a pharmacist-prepared discharge medication management summary. Int. J. Clin. Pharm. 2017, 39, 394–402. [Google Scholar] [CrossRef]
- McCarthy, L.M.; Li, S.; Fernandes, O.; Cameron, K.; Lui, P.; Wong, G.; Pariser, P.; Farrell, J.; Luke, M.J.; Guilcher, S.J.T. Enhanced communication between inpatient and community pharmacists to optimize medication management during transitions of care. J. Am. Pharm. Assoc. 2019, 59, 79–86.e1. [Google Scholar] [CrossRef]
- Vincent, C.; Staines, A. Enhancing the Quality and Safety of Swiss Healthcare. Available online: https://www.bag.admin.ch/bag/en/home/versicherungen/krankenversicherung/krankenversicherung-qualitaetssicherung.html (accessed on 30 January 2020).
- Mekonnen, A.B.; McLachlan, A.J.; Brien, J.A. Pharmacy-led medication reconciliation programmes at hospital transitions: A systematic review and meta-analysis. J. Clin. Pharm. Ther. 2016, 41, 128–144. [Google Scholar] [CrossRef]
- Vanwesemael, T.; Boussery, K.; Dilles, T. Self-administration of medication in hospital: A literature review. Nurs. Sci. Q. 2020, 33, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.; Muir, P.; Allardice, J.-A.; Clark, K.; Groves, J.; Molenaar, M.; Robson, G. SHPA guidelines for self-administration of medication in hospitals and residential care facilities. J. Pharm. Pract. Res. 2002, 32, 324–325. [Google Scholar] [CrossRef]
- Stampfli, D.; Boeni, F.; Gerber, A.; Battig, V.A.D.; Weidmann, R.; Hersberger, K.E.; Lampert, M.L. Assessing the ability of the Drug-Associated Risk Tool (DART) questionnaire to stratify hospitalised older patients according to their risk of drug-related problems: A cross-sectional validation study. BMJ Open 2018, 8, e021284. [Google Scholar] [CrossRef] [PubMed]
| Intervention | Description |
|---|---|
| Patient education | Patient counselling on their medication (e.g., therapy duration/dosing) In-depth patient counselling on their medication (e.g., effect/benefit, therapy goal/side effects) Patient instructions (e.g., for inhalation devices/prefilled syringe) Patient counselling on red flags (symptoms that indicate a worsening of condition/medication intolerance) Patient counselling on medication prescribed before hospital admission |
| Discharge planning | Organization of medicines (e.g., contact with patients’ community pharmacies/pill dispensers/reimbursement) Organization of rehabilitation/home care |
| Appointment scheduled before discharge | Assuring follow-up care (e.g., a follow-up appointment with the treating physician) |
| Timely follow-up | Follow-up care by a case manager |
| Communication to PCP | Medication changes are communicated to at least one healthcare professional (e.g., practitioner, community pharmacy) or institution (e.g., home care, nursing home) |
| Follow-up telephone call | Follow-up telephone call with discharged patients |
| Patient hotline | Hospital or hospital community pharmacy 1 offers a patient hotline for medication related questions |
| Intervention | Activities in Swiss Hospitals | Frequency, n | Evidence in Cochrane Reviews | Guidelines | |
|---|---|---|---|---|---|
| Pre-discharge | Patient education | Patient counselling on their medication (e.g., therapy duration/dosing) | 40 | + [23] | + [26,27,28,29,30,31,33,34,35,36,37,38,39,40,41] |
| In-depth patient counselling on their medication (e.g., effect/benefit, therapy goal/side effects) | 32 | ||||
| Patient instructions (e.g., for inhalation devices/prefilled syringe) | 33 | ||||
| Patient counselling on red flags (symptoms that indicate a worsening of condition/medication intolerance) | 26 | ||||
| Patient counselling on medication prescribed before hospital admission | 19 | ||||
| Discharge planning | Organization of medicines (e.g., contact with patients’ community pharmacies/pill dispensers/reimbursement) | 9 * | +/0 [24] | + [26,28,29,30,31,32,33,34,35,36,37,38,39,40] | |
| Organization of rehabilitation/home care | 20 * | ||||
| Appointment scheduled before discharge | Assuring follow-up care (e.g., a follow-up appointment with the treating physician) | 15 * | ? | + [28,32,33,35,36,38] | |
| Post-discharge | Timely follow-up | Follow-up care by a case manager | 7 * | ? | + [28,30,34,35,39,40,42,43] |
| Communication to PCP | Medication changes are communicated to at least one healthcare professional (e.g., practitioner, community pharmacy) or institution (e.g., home care, nursing home) | 34 | ? | + [26,27,28,29,30,31,33,35,37,38,39,41] | |
| Follow-up telephone call | Follow-up telephone call with discharged patients | 2 | +/0 [25] | + [28,30,37,38] | |
| Patient hotline | Hospital or hospital community pharmacy offers a patient hotline for medication related questions | 10 | ? | + [32,35,36,38,40] |
| Hospital | Hospital Admission | Hospital Stay | Hospital Discharge | Follow-Up |
|---|---|---|---|---|
| Interventions at Admission | Interventions during Hospital Stay | Pre-Discharge Interventions | Post-Discharge Interventions | |
| Hospital 1 | - Medication reconciliation - Medication review | - Interprofessional ward rounds (medical ward) | Hospital community pharmacy *#: - Medication reconciliation - Medication review - Patient education | Hospital community pharmacy *#: - Patient hotline |
| Hospital 2 | None | - Medication self-management training program # - Group training for patients on different topics (e.g., bowel management) | Hospital community pharmacy *#: - Medication reconciliation - Patient education | Hospital community pharmacy *#: - Patient hotline |
| Hospital 3 | None | - Interprofessional ward rounds (oncology ward) - Medication review (oncology and palliative ward) | None | None |
| Hospital 4 | None | None | Hospital community pharmacy *#: - Medication reconciliation - Patient education | Hospital community pharmacy *#: - Patient hotline |
| Hospital 5 | None | - Medication review (medical ward) | Hospital pharmacy#: - Medication reconciliation - Medication review | None |
| Hospital 6 | None | - Interprofessional ward round (medical ward) | Hospital community pharmacy *#: - Patient education | Hospital community pharmacy *#: - Patient hotline |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Studer, H.; Boeni, F.; Hersberger, K.E.; Lampert, M.L. Pharmaceutical Discharge Management: Implementation in Swiss Hospitals Compared to International Guidelines. Pharmacy 2021, 9, 33. https://doi.org/10.3390/pharmacy9010033
Studer H, Boeni F, Hersberger KE, Lampert ML. Pharmaceutical Discharge Management: Implementation in Swiss Hospitals Compared to International Guidelines. Pharmacy. 2021; 9(1):33. https://doi.org/10.3390/pharmacy9010033
Chicago/Turabian StyleStuder, Helene, Fabienne Boeni, Kurt E. Hersberger, and Markus L. Lampert. 2021. "Pharmaceutical Discharge Management: Implementation in Swiss Hospitals Compared to International Guidelines" Pharmacy 9, no. 1: 33. https://doi.org/10.3390/pharmacy9010033
APA StyleStuder, H., Boeni, F., Hersberger, K. E., & Lampert, M. L. (2021). Pharmaceutical Discharge Management: Implementation in Swiss Hospitals Compared to International Guidelines. Pharmacy, 9(1), 33. https://doi.org/10.3390/pharmacy9010033






