A Role for Primary Care Pharmacists in the Management of Inflammatory Bowel Disease? Lessons from Chronic Disease: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Study Eligibility
2.2. Quality Assessment
2.3. Data Extraction
3. Results
3.1. Study Selection
3.2. Assessment of Quality
3.3. Description of Studies
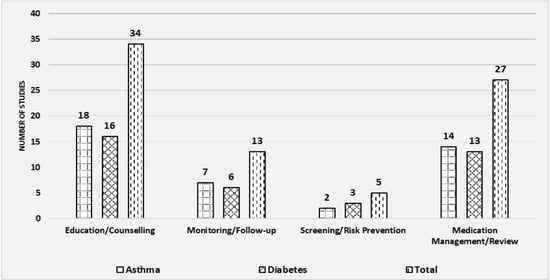
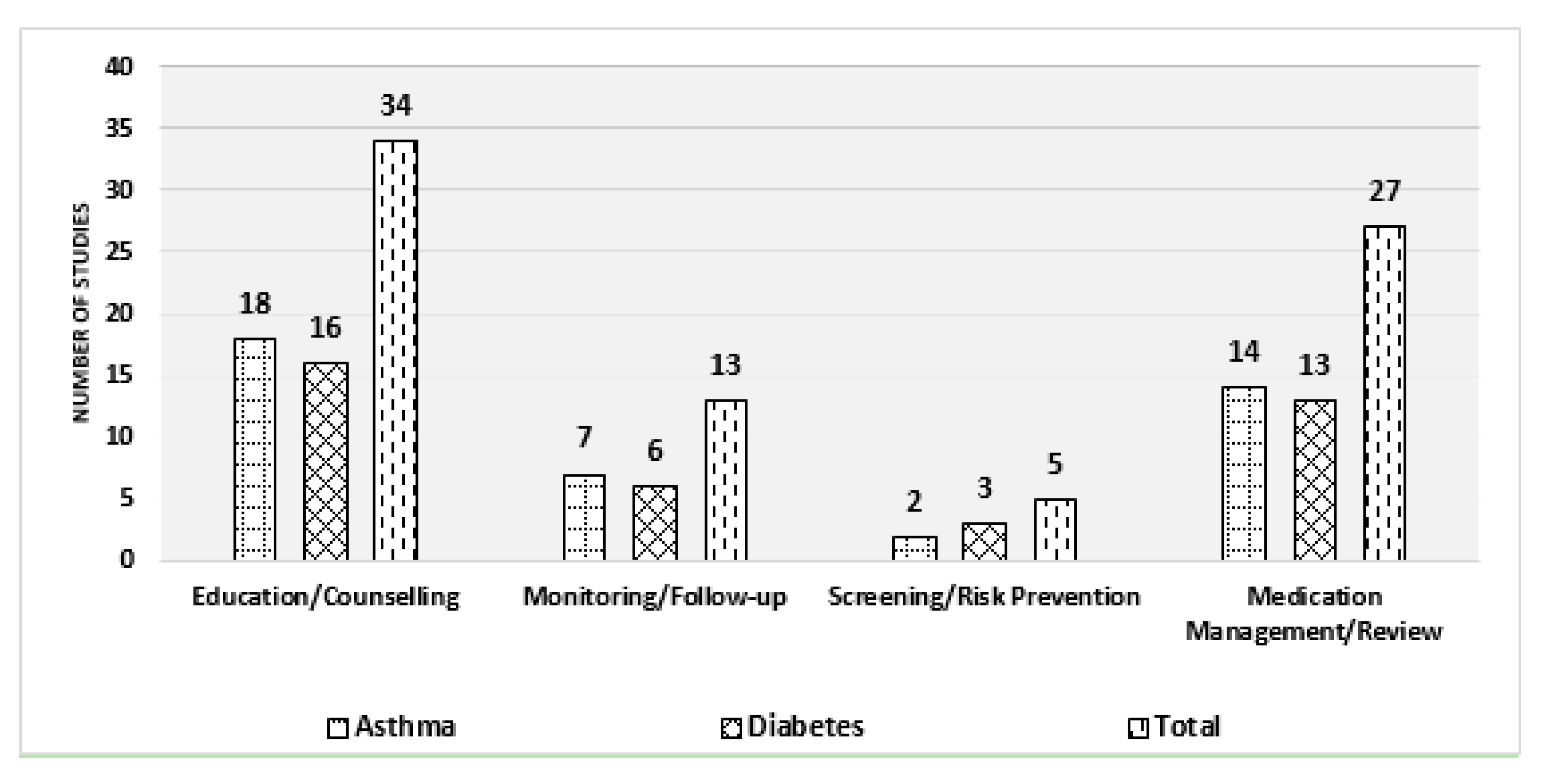
3.4. Types of Intervention by Pharmacists
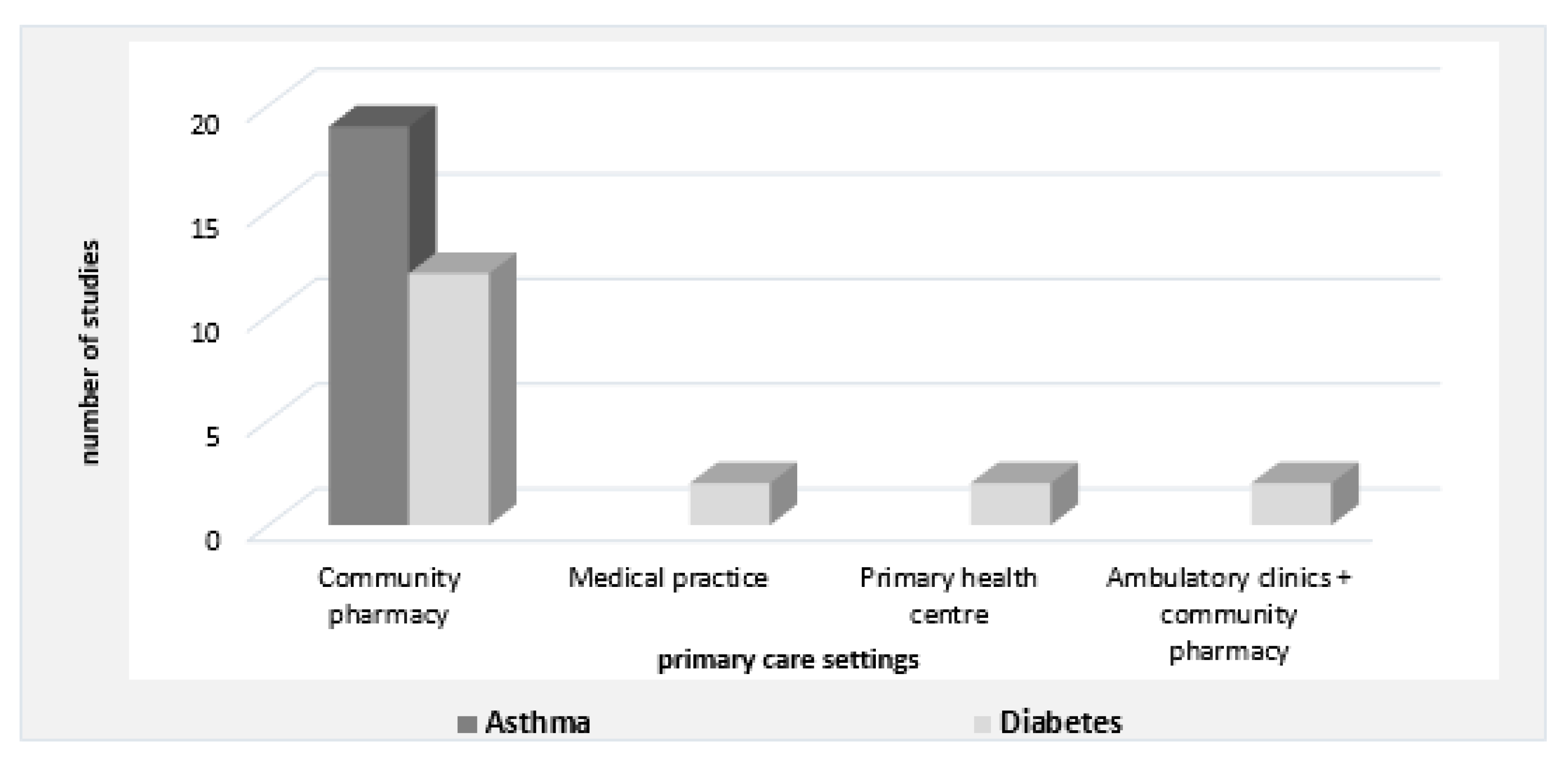
3.5. Measurable Outcomes of Pharmacist Interventions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Disclaimer
Abbreviations
References
- International Pharmaceutical Federation (FIP). Beating Non-Communicable Diseases in the Community—The Contributions of Pharmacists. 2019. Available online: https://www.fip.org/files/fip/publications/NCDs/beating-ncds-in-the-community-the-contribution-of-pharmacists.pdf (accessed on 4 June 2019).
- World Health Organization (WHO). Preventing Chronic Disease: A Vital Investiment. WHO Global Report. Available online: http://who.int/chp/chronic_disease_report/en (accessed on 4 June 2019).
- Swerissen, H.; Duckett, S. Mapping Primary Care in Australia. Available online: https://grattan.edu.au/report/mapping-primary-care-in-australia/ (accessed on 2 February 2020).
- The Department of Health. Primary Health Care in Australia. National Primary Health Care Strategic Framework. 2013. Available online: https://www1.health.gov.au/internet/publications/publishing.nsf/Content/NPHC-Strategic-Framework~phc-australia (accessed on 21 December 2019).
- Mowat, C.; Cole, A.; Windsor, A.; Ahmad, T.; Arnott, I.; Driscoll, R.; Mitton, S.; Orchard, T.; Rutter, M.; Younge, L.; et al. Guidelines for the management of inflammatory bowel disease in adults. Gut 2011, 60, 571–607. [Google Scholar] [CrossRef] [PubMed]
- PricewaterhouseCoopers (PwC) Australia. Improving Inflammatory Bowel Disease Care across Australia. Crohn’s Colitis Australia [Report]. 2013, p. 53. Available online: https://www.crohnsandcolitis.com.au/site/wp-content/uploads/PwC-report-2013.pdf (accessed on 9 May 2019).
- Massuger, W.; Moore, G.T.C.; Andrews, J.M.; Kilkenny, M.F.; Reyneke, M.; Knowles, S.; Purcell, L.; Alex, G.; Buckton, S.; Page, A.T.; et al. Crohn’s & Colitis Australia inflammatory bowel disease audit: Measuring the quality of care in Australia. Intern. Med. J. 2019, 49, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Prasad, S.S.; Potter, M.; Keely, S.; Talley, N.J.; Walker, M.M.; Kairuz, T. Roles of healthcare professionals in the management of chronic gastrointestinal diseases with a focus on primary care: A systematic review. JGH Open 2020, 4, 221–229. [Google Scholar] [CrossRef]
- Morabia, A.; Abel, T. The WHO report “Preventing chronic diseases: A vital investment” and us. Soz Prav. 2006, 51, 74. [Google Scholar] [CrossRef]
- Hughes, C.A.; Breault, R.R.; Hicks, D.; Schindel, T.J. Positioning pharmacists’ roles in primary health care: A discourse analysis of the compensation plan in Alberta, Canada. BMC Health Serv. Res. 2017, 17, 770. [Google Scholar] [CrossRef] [PubMed]
- Houle, S.K.; Grindrod, K.A.; Chatterley, T.; Tsuyuki, R.T. Paying pharmacists for patient care: A systematic review of remunerated pharmacy clinical care services. Can. Pharm. J. 2014, 147, 209–232. [Google Scholar] [CrossRef] [PubMed]
- Koltun, W.A. Better together: Improved care of the IBD patient using the multi-disciplinary IBD center. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 491–493. [Google Scholar] [CrossRef]
- Lee, C.K.; Melmed, G.Y. Multidisciplinary Team-Based Approaches to IBD Management: How Might “One-Stop Shopping” Work for Complex IBD Care? Am. J. Gastroenterol. 2017, 112, 825–827. [Google Scholar] [CrossRef] [PubMed]
- Fiorino, G.; Allocca, M.; Chaparro, M.; Coenen, S.; Fidalgo, C.; Younge, L.; Gisbert, J.P. ‘Quality of Care’ Standards in Inflammatory Bowel Disease: A Systematic Review. J. Crohns Colitis 2019, 13, 127–137. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 151, W65–W94. [Google Scholar] [CrossRef] [PubMed]
- Kozma, C.M.; Reeder, C.E.; Schulz, R.M. Economic, clinical, and humanistic outcomes: A planning model for pharmacoeconomic research. Clin. Ther. 1993, 15, 1121–1132, discussion 1120. [Google Scholar] [PubMed]
- The Joanna Briggs Institution. Critical Appraisal Checklist for Randomized Controlled Trials. Available online: https://joannabriggs.org/sites/default/files/2019-05/JBI_RCTs_Appraisal_tool2017_0.pdf (accessed on 20 June 2019).
- The Joanna Briggs Institution. Critical Appraisal Checklist for Quasi-Experimental Studies. Available online: https://joannabriggs.org/sites/default/files/2019-05/JBI_Quasi-Experimental_Appraisal_Tool2017_0.pdf (accessed on 20 June 2019).
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Qureshi, R.; Mattis, P.; Lisy, K.; et al. Chapter 7: Systematic reviews of etiology and risk. In Joanna Briggs Institute Reviewer’s Manual; Aromataris, E., Munnn, Z., Eds.; The Joanna Briggs Institute: Adelaide, Australia, 2017; Available online: https://wiki.joannabriggs.org/display/MANUAL/Appendix+7.1++Critical+appraisal+checklist+for+cohort+studies (accessed on 20 June 2019).
- Mayer, H.; Nonn, C.; Osterbrink, J.; Evers, G.C. Quality criteria of assessment scales—Cohen’s kappa as measure of interrator reliability (1). Pflege 2004, 17, 36–46. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Al Hamarneh, Y.N.; Hemmelgarn, B.R.; Hassan, I.; Jones, C.A.; Tsuyuki, R.T. The Effectiveness of Pharmacist Interventions on Cardiovascular Risk in Adult Patients with Type 2 Diabetes: The Multicentre Randomized Controlled RxEACH Trial. Can. J. Diabetes 2017, 41, 580–586. [Google Scholar] [CrossRef]
- Armour, C.; Bosnic-Anticevich, S.; Brillant, M.; Burton, D.; Emmerton, L.; Krass, I.; Saini, B.; Smith, L.; Stewart, K. Pharmacy Asthma Care Program (PACP) improves outcomes for patients in the community. Thorax 2007, 62, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.P.; Hassali, M.A.; Saleem, F.; Aljadhey, H. Effects of pharmacist-led patient education on diabetes-related knowledge and medication adherence: A home-based study. Health Educ. J. 2015, 75, 421–433. [Google Scholar] [CrossRef]
- Cordina, M.; McElnay, J.C. Assessment of a community pharmacy-based program for patients with asthma. Pharmacotherapy 2001, 21, 1196–1203. [Google Scholar] [CrossRef]
- Doucette, W.R.; Witry, M.J.; Farris, K.B.; McDonough, R.P. Community pharmacist-provided extended diabetes care. Ann. Pharmacother. 2009, 43, 882–889. [Google Scholar] [CrossRef]
- Mehuys, E.; Van Bortel, L.; De Bolle, L.; Van Tongelen, I.; Annemans, L.; Remon, J.P.; Brusselle, G. Effectiveness of pharmacist intervention for asthma control improvement. Eur. Respir. J. 2008, 31, 790–799. [Google Scholar] [CrossRef]
- Mehuys, E.; Van Bortel, L.; De Bolle, L.; Van Tongelen, I.; Annemans, L.; Remon, J.P.; Giri, M. Effectiveness of a community pharmacist intervention in diabetes care: A randomized controlled trial. J. Clin. Pharm. Ther. 2011, 36, 602–613. [Google Scholar] [CrossRef]
- Al Hamarneh, Y.N.; Charrois, T.; Lewanczuk, R.; Tsuyuki, R.T. Pharmacist intervention for glycaemic control in the community (the RxING study). BMJ Open 2013, 3, e003154. [Google Scholar] [CrossRef] [PubMed]
- Bereznicki, B.J.; Peterson, G.; Jackson, S.; Walters, E.H.; George, J.; Stewart, K.; March, G.J. Uptake and effectiveness of a community pharmacy intervention programme to improve asthma management. J. Clin. Pharm. Ther. 2013, 38, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Bliss, E.; Codack, H.; Boothe, J. Diabetes care—An evaluation of a community pharmacy based HbA1c testing service. Pharm. J. 2001, 267, 264–266. [Google Scholar]
- Correr, C.J.; Melchiors, A.C.; Fernandez-Llimos, F.; Pontarolo, R. Effects of a pharmacotherapy follow-up in community pharmacies on type 2 diabetes patients in Brazil. Int. J. Clin. Pharm. 2011, 33, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Hendrie, D.; Miller, T.R.; Woodman, R.J.; Hoti, K.; Hughes, J. Cost-effectiveness of reducing glycaemic episodes through community pharmacy management of patients with type 2 diabetes mellitus. J. Prim. Prev. 2014, 35, 439–449. [Google Scholar] [CrossRef]
- Kovacevic, M.; Culafic, M.; Jovanovic, M.; Vucicevic, K.; Kovacevic, S.V.; Miljkovic, B. Impact of community pharmacists’ interventions on asthma self-management care. Res. Soc. Adm. Pharm. 2018, 14, 603–611. [Google Scholar] [CrossRef]
- Krass, I.; Armour, C.L.; Mitchell, B.; Brillant, M.; Dienaar, R.; Hughes, J.; Lau, P.; Peterson, G.; Stewart, K.; Taylor, S.; et al. The Pharmacy Diabetes Care Program: Assessment of a community pharmacy diabetes service model in Australia. Diabet. Med. 2007, 24, 677–683. [Google Scholar] [CrossRef]
- Krass, I.; Taylor, S.J.; D McInman, A.; Armour, C.L. The pharmacist’s role in continuity of care in type 2 diabetes: An evaluation of a model. J. Pharm. Technol. 2006, 22, 3–8. [Google Scholar] [CrossRef]
- Krass, I.; Taylor, S.J.; Smith, C.; Armour, C.L. Impact on medication use and adherence of Australian pharmacists’ diabetes care services. J. Am. Pharm. Assoc. 2005, 45, 33–40. [Google Scholar] [CrossRef]
- Kritikos, V.; Armour, C.L.; Bosnic-Anticevich, S.Z. Interactive small-group asthma education in the community pharmacy setting: A pilot study. J. Asthma 2007, 44, 57–64. [Google Scholar] [CrossRef]
- Schulz, M.; Verheyen, F.; Mühlig, S.; Müller, J.M.; Mühlbauer, K.; Knop-Schneickert, E.; Petermann, F.; Bergmann, K.C. Pharmaceutical care services for asthma patients: A controlled intervention study. J. Clin. Pharmacol. 2001, 41, 668–676. [Google Scholar] [CrossRef] [PubMed]
- Benedict, A.W.; Spence, M.M.; Sie, J.L.; Chin, H.A.; Ngo, C.D.; Salmingo, J.F.; Vidaurreta, A.T.; Rashid, N. Evaluation of a pharmacist-managed diabetes program in a primary care setting within an integrated health care system. J. Manag. Care Spec. Pharm. 2018, 24, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.; Schifano, F.; Robinson, P.; Phillips, G.; Doherty, L.; Melnick, P.; Laming, L.; Sinclair, A.; Dhillon, S. Impact of community pharmacy diabetes monitoring and education programme on diabetes management: A randomized controlled study. Diabet. Med. 2012, 29, e326–e333. [Google Scholar] [CrossRef]
- Barbanel, D.; Eldridge, S.; Griffiths, C. Can a self-management programme delivered by a community pharmacist improve asthma control? A randomised trial. Thorax 2003, 58, 851–854. [Google Scholar] [CrossRef] [PubMed]
- Basheti, I.A.; Armour, C.L.; Bosnic-Anticevich, S.Z.; Reddel, H.K. Evaluation of a novel educational strategy, including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Educ. Couns. 2008, 72, 26–33. [Google Scholar] [CrossRef]
- Garcia-Cardenas, V.; Sabater-Hernandez, D.; Kenny, P.; Martinez-Martinez, F.; Faus, M.J.; Benrimoj, S.I. Effect of a pharmacist intervention on asthma control. A cluster randomised trial. Respir. Med. 2013, 107, 1346–1355. [Google Scholar] [CrossRef]
- Klassing, H.M.; Ruisinger, J.F.; Prohaska, E.S.; Melton, B.L. Evaluation of Pharmacist-Initiated Interventions on Vaccination Rates in Patients with Asthma or COPD. J. Community Health 2018, 43, 297–303. [Google Scholar] [CrossRef]
- McLean, W.; Gillis, J.; Waller, R. The BC Community Pharmacy Asthma Study: A study of clinical, economic and holistic outcomes influenced by an asthma care protocol provided by specially trained community pharmacists in British Columbia. Can. Respir. J. 2003, 10, 195–202. [Google Scholar] [CrossRef]
- Saini, B.; Krass, I.; Armour, C. Development, implementation, and evaluation of a community pharmacy-based asthma care model. Ann. Pharmacother. 2004, 38, 1954–1960. [Google Scholar] [CrossRef]
- Bello, S.I.; Ganiyu, K.A.; Dakop, Y.O.; Erah, P.O. Pharmacist’s intervention in the control of blood sugar levels in randomised diabetes patients at a primary health care setting in Benin City. Niger. Q. J. Hosp. Med. 2012, 22, 245–248. [Google Scholar]
- Diamond, S.A.; Chapman, K.R. The impact of a nationally coordinated pharmacy-based asthma education intervention. Can. Respir. J. 2001, 8, 261–265. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Emmerton, L.; Shaw, J.; Kheir, N. Asthma management by New Zealand pharmacists: A pharmaceutical care demonstration project. J. Clin. Pharm. Ther. 2003, 28, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Hammerlein, A.; Muller, U.; Schulz, M. Pharmacist-led intervention study to improve inhalation technique in asthma and COPD patients. J. Eval. Clin. Pract. 2011, 17, 61–70. [Google Scholar] [CrossRef]
- Lemay, K.S.; Saini, B.; Bosnic-Anticevich, S.; Smith, L.; Stewart, K.; Emmerton, L.; Burton, D.L.; Krass, I.; Armour, C.L. An exploration of clinical interventions provided by pharmacists within a complex asthma service. Pharm. Pract. 2015, 13, 529. [Google Scholar] [CrossRef] [PubMed]
- Nkansah, N.T.; Brewer, J.M.; Connors, R.; Shermock, K.M. Clinical outcomes of patients with diabetes mellitus receiving medication management by pharmacists in an urban private physician practice. Am. J. Health-Syst. Pharm. 2008, 65, 145–149. [Google Scholar] [CrossRef]
- Saini, B.; LeMay, K.; Emmerton, L.; Krass, I.; Smith, L.; Bosnic-Anticevich, S.; Stewart, K.; Burton, D.; Armour, C. Asthma disease management-Australian pharmacists’ interventions improve patients’ asthma knowledge and this is sustained. Patient Educ. Couns. 2011, 83, 295–302. [Google Scholar] [CrossRef]
- Wermeille, J.; Bennie, M.; Brown, I.; McKnight, J. Pharmaceutical care model for patients with type 2 diabetes: Integration of the community pharmacist into the diabetes team—A pilot study. Pharm. World Sci. 2004, 26, 18–25. [Google Scholar] [CrossRef]
- Cranor, C.W.; Bunting, B.A.; Christensen, D.B. The Asheville Project: Long-term clinical and economic outcomes of a community pharmacy diabetes care program. J. Am. Pharm. Assoc. 2003, 43, 173–184. [Google Scholar] [CrossRef]
- Ottenbros, S.; Teichert, M.; de Groot, R.; Griens, F.; Sodihardjo, F.; Wensing, M.; de Gier, J.J. Pharmacist-led intervention study to improve drug therapy in asthma and COPD patients. Int. J. Clin. Pharm. 2014, 36, 336–344. [Google Scholar] [CrossRef]
- Oyetayo, O.O.; James, C.; Martinez, A.; Roberson, K.; Talbert, R.L. The Hispanic Diabetes Management Program: Impact of community pharmacists on clinical outcomes. J. Am. Pharm. Assoc. JAPhA 2011, 51, 623–626. [Google Scholar] [CrossRef]
- Santschi, V.; Chiolero, A.; Paradis, G.; Colosimo, A.L.; Burnand, B. Pharmacist interventions to improve cardiovascular disease risk factors in diabetes: A systematic review and meta-analysis of randomized controlled trials. Diabetes Care 2012, 35, 2706–2717. [Google Scholar] [CrossRef]
- Roebuck, M.C.; Liberman, J.N.; Gemmill-Toyama, M.; Brennan, T.A. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff. 2011, 30, 91–99. [Google Scholar] [CrossRef]
- Abegunde, A.T.; Muhammad, B.H.; Ali, T. Preventive health measures in inflammatory bowel disease. World J. Gastroenterol. 2016, 22, 7625–7644. [Google Scholar] [CrossRef]
- Farraye, F.A.; Melmed, G.Y.; Lichtenstein, G.R.; Kane, S.V. ACG Clinical Guideline: Preventive Care in Inflammatory Bowel Disease. Am. J. Gastroenterol. 2017, 112, 241–258. [Google Scholar] [CrossRef] [PubMed]
- Torres, J.; Burisch, J.; Riddle, M.; Dubinsky, M.; Colombel, J.F. Preclinical disease and preventive strategies in IBD: Perspectives, challenges and opportunities. Gut 2016, 65, 1061–1069. [Google Scholar] [CrossRef]
- Australian Government Department of Health. Inflammtory Bowel Disease National Action Plan 2019. Available online: https://www.crohnsandcolitis.com.au/ibdqoc/ibd-national-action-plan/ (accessed on 17 January 2020).
- International Pharmaceutical Federation (FIP). An Overview of Current Pharmacy Impact on Immunisation—A Global Report. Available online: https://www.fip.org/files/fip/publications/FIP_report_on_Immunisation.pdf (accessed on 29 February 2020).
- WHO. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. Available online: https://apps.who.int/iris/bitstream/handle/10665/94384/9789241506236_eng.pdf?sequence=1 (accessed on 3 August 2019).
- Paterick, T.E.; Patel, N.; Tajik, A.J.; Chandrasekaran, K. Improving health outcomes through patient education and partnerships with patients. Proceedings (Bayl. Univ. Med. Cent.) 2017, 30, 112–113. [Google Scholar] [CrossRef]
- McDermott, E.; Healy, G.; Mullen, G.; Keegan, D.; Byrne, K.; Guerandel, A.; Forry, M.; Moloney, J.; Doherty, G.; Cullen, G.; et al. Patient Education in Inflammatory Bowel Disease: A Patient-Centred, Mixed Methodology Study. J. Crohns Colitis 2018, 12, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.; Chen, A.; Tiao, D.; Selinger, C.; Leong, R. Medication adherence in inflammatory bowel disease. Intest. Res. 2017, 15, 434–445. [Google Scholar] [CrossRef]
- Tiao, D.K.; Chan, W.; Jeganathan, J.; Chan, J.T.; Perry, J.; Selinger, C.P.; Leong, R.W. Inflammatory Bowel Disease Pharmacist Adherence Counseling Improves Medication Adherence in Crohn’s Disease and Ulcerative Colitis. Inflamm. Bowel. Dis. 2017, 23, 1257–1261. [Google Scholar] [CrossRef] [PubMed]
- Prasad, S.S.; Keely, S.; Talley, N.J.; Kairuz, T.; Walker, M.M. Pharmacists’ Confidence in Managing Patients with Inflammatory Bowel Disease. Pharmacy 2020, 8, 68. [Google Scholar] [CrossRef] [PubMed]
- Burr, N.E.; Smith, C.; West, R.; Hull, M.A.; Subramanian, V. Increasing Prescription of Opiates and Mortality in Patients With Inflammatory Bowel Diseases in England. Clin. Gastroenterol. Hepatol. 2018, 16, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Foy, R.; Leaman, B.; McCrorie, C.; Petty, D.; House, A.; Bennett, M.; Carder, P.; Faulkner, S.; Glidewell, L.; West, R. Prescribed opioids in primary care: Cross-sectional and longitudinal analyses of influence of patient and practice characteristics. BMJ Open 2016, 6, e010276. [Google Scholar] [CrossRef]
- Zielinska, A.; Salaga, M.; Wlodarczyk, M.; Fichna, J. Focus on current and future management possibilities in inflammatory bowel disease-related chronic pain. Int. J. Colorectal. Dis. 2019, 34, 217–227. [Google Scholar] [CrossRef] [PubMed]


| Disease | Clinical | Humanistic | Economic | Clinical + Humanistic | Clinical + Economic | Clinical + Humanistic + Economic |
|---|---|---|---|---|---|---|
| Diabetes | 10 | 0 | 0 | 5 | 2 | 1 |
| Asthma | 10 | 1 | 0 | 5 | 0 | 3 |
| Total | 20 | 1 | 0 | 10 | 2 | 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prasad, S.S.; Duncanson, K.; Keely, S.; Talley, N.J.; Kairuz, T.; Holtmann, G.J.; Shah, A.; Walker, M.M. A Role for Primary Care Pharmacists in the Management of Inflammatory Bowel Disease? Lessons from Chronic Disease: A Systematic Review. Pharmacy 2020, 8, 204. https://doi.org/10.3390/pharmacy8040204
Prasad SS, Duncanson K, Keely S, Talley NJ, Kairuz T, Holtmann GJ, Shah A, Walker MM. A Role for Primary Care Pharmacists in the Management of Inflammatory Bowel Disease? Lessons from Chronic Disease: A Systematic Review. Pharmacy. 2020; 8(4):204. https://doi.org/10.3390/pharmacy8040204
Chicago/Turabian StylePrasad, Sharmila S., Kerith Duncanson, Simon Keely, Nicholas J. Talley, Therése Kairuz, Gerald J. Holtmann, Ayesha Shah, and Marjorie M. Walker. 2020. "A Role for Primary Care Pharmacists in the Management of Inflammatory Bowel Disease? Lessons from Chronic Disease: A Systematic Review" Pharmacy 8, no. 4: 204. https://doi.org/10.3390/pharmacy8040204
APA StylePrasad, S. S., Duncanson, K., Keely, S., Talley, N. J., Kairuz, T., Holtmann, G. J., Shah, A., & Walker, M. M. (2020). A Role for Primary Care Pharmacists in the Management of Inflammatory Bowel Disease? Lessons from Chronic Disease: A Systematic Review. Pharmacy, 8(4), 204. https://doi.org/10.3390/pharmacy8040204