Evaluation of a Pharmacist–Dietician-Led Patient-Centered Approach to Managing CKD-MBD: A Mixed-Method Study
Abstract
1. Introduction
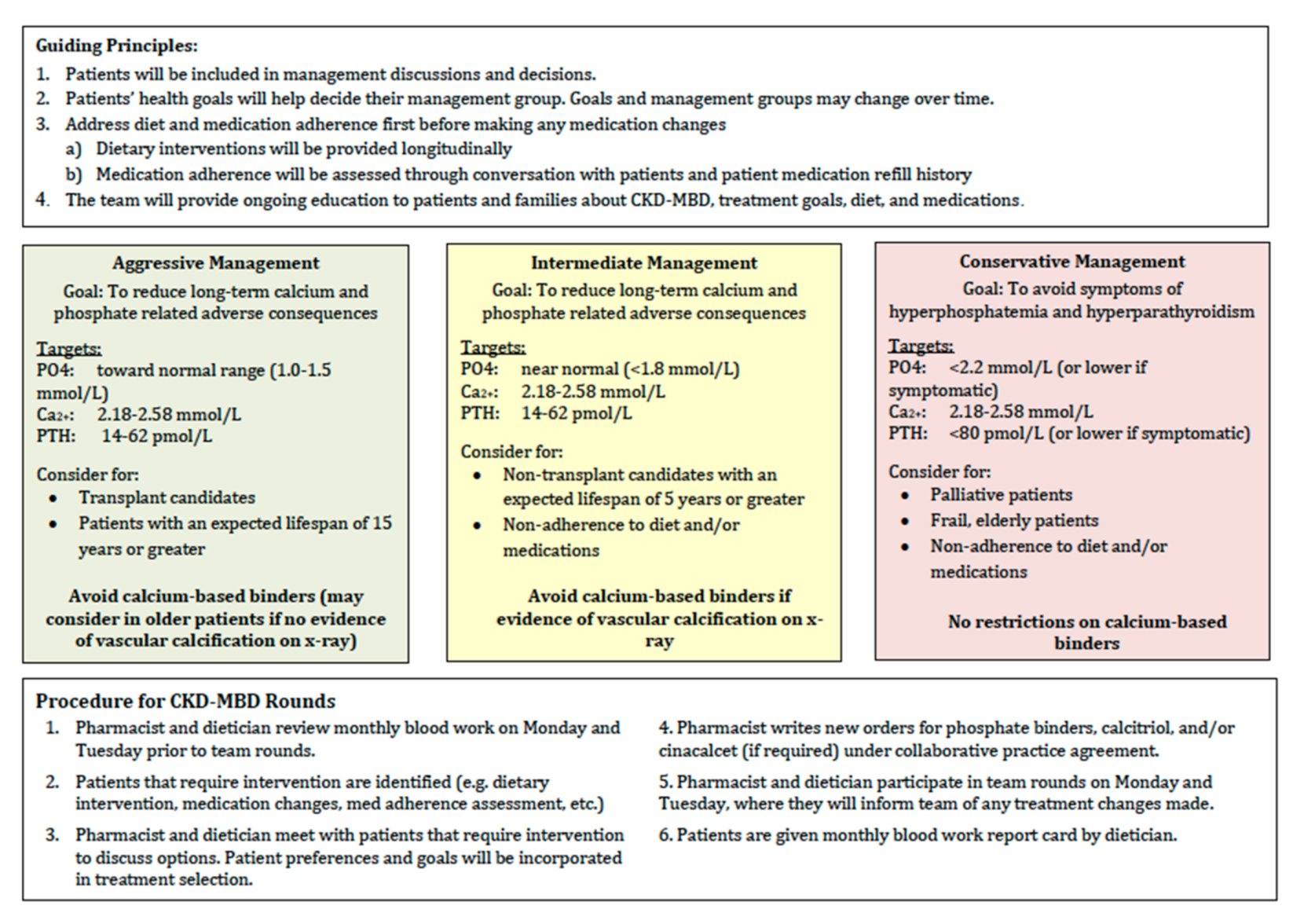
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection
2.3.1. Quantitative
2.3.2. Qualitative
2.4. Data Analysis
2.4.1. Quantitative Analysis
2.4.2. Qualitative Analysis
3. Results
3.1. Quantitative Results
3.2. Qualitative Results
3.2.1. Major Themes
Lack of Privacy
Knowledge and Perception of Bloodwork Rounds
Issues with Taking Phosphate Binders
Areas for Increased Patient Education
3.2.2. Minor Themes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
| 1. How satisfied are you with the effect of your {treatment/care}? | |
| □ Very satisfied | 0 |
| □ Satisfied | 1 |
| □ Neither satisfied nor dissatisfied | 2 |
| □ Dissatisfied | 3 |
| □ Very dissatisfied | 4 |
| 2. How satisfied are you with the explanations the {doctor/other health professional} has given you about the results of your {treatment/care}? | |
| □ Very dissatisfied | 0 |
| □ Dissatisfied | 1 |
| □ Neither satisfied nor dissatisfied | 2 |
| □ Satisfied | 3 |
| □ Very satisfied | 4 |
| 3. The {doctor/other health professional} was very careful to check everything when examining you. | |
| □ Strongly agree | 0 |
| □ Agree | 1 |
| □ Not sure | 2 |
| □ Disagree | 3 |
| □ Strongly disagree | 4 |
| 4. How satisfied were you with the choices you had in decisions affecting your health care? | |
| □ Very satisfied | 4 |
| □ Satisfied | 3 |
| □ Neither satisfied nor dissatisfied | 2 |
| □ Dissatisfied | 1 |
| □ Very disssatisfied | 0 |
| □ Very dissatisfied | 0 |
| □ Dissatisfied | 1 |
| □ Neither satisfied nor dissatisfied | 2 |
| □ Satisfied | 3 |
| □ Very satisfied | 4 |
| 5. How much of the time did you feel respected by the {doctor/other health professional}? | |
| □ All of the time | 0 |
| □ Most of the time | 1 |
| □ About half of the time | 2 |
| □ Some of the time | 3 |
| □ None of the time | 4 |
| 6. The time you had with the {doctor/other health professional} was too short. | |
| □ Strongly agree | 0 |
| □ Agree | 1 |
| □ Not sure | 2 |
| □ Disagree | 3 |
| □ Strongly disagree | 4 |
| 7. Are you satisfied with the care you received in the {hospital/clinic}? | |
| □ Very satisfied | 0 |
| □ Satisfied | 1 |
| □ Neither satisfied nor dissatisfied | 2 |
| □ Dissatisfied | 3 |
| □ Very dissatisfied | 4 |
- Reverse the scores for items #1, #3, #5, #7.
- Sum all scores. The score range is from 0 (extremely dissatisfied) to 28 (extremely satisfied).
Appendix C
- What do you know about the process of monthly blood work rounds?
- Tell me about your experiences with the healthcare team during monthly bloodwork rounds (explain the process of monthly bloodwork rounds to ensure participants know what portion of their healthcare interactions you are referring to)
- Tell me about your level of involvement in the decision-making process when changes are made to your medications?
- ○
- How would you like to be included?
- ○
- What would that look like for you?
- Tell me about a time you had concerns about your treatment or medications
- ○
- Were you given the opportunity to/did you feel you could ask about them?
- What do you think about privacy/confidentiality on the unit?
- Tell me about your experience with taking phosphate binders (these medications include TUMS, calcium, renagel)
- ○
- Do you find it difficult to remember taking phosphate binding medication?
- ○
- Tell me about any reasons or barriers that stop you from taking your medications.
- Have you noticed a change in your experience in your care?
- Have you felt more involved?
References
- Moe, S.M.; Drüeke, T.B. Improving global outcomes in mineral and bone disorders. Clin. J. Am. Soc. Nephrol. 2008, 3 (Suppl. 3), S127–S130. [Google Scholar] [CrossRef] [PubMed]
- Adeney, K.L.; Siscovick, D.S.; Ix, J.H.; Seliger, S.L.; Shlipak, M.G.; Jenny, N.S.; Kestenbaum, B.R. Association of serum phosphate with vascular and valvular calcification in moderate CKD. J. Am. Soc. Nephrol. 2009, 20, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Kestenbaum, B.; Sampson, J.N.; Rudser, K.D.; Patterson, D.J.; Seliger, S.L.; Young, B.; Sherrard, N.J.; Andress, D.L. Serum phosphate levels and mortality risk among people with chronic kidney disease. J. Am. Soc. Nephrol. 2005, 16, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Block, G.A.; Klassen, P.S.; Lazarus, J.M.; Ofsthun, N.; Lowrie, E.G.; Chertow, G.M. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J. Am. Soc. Nephrol. 2004, 15, 2208–2218. [Google Scholar] [CrossRef] [PubMed]
- Shaman, A.M.; Kowalski, S.R. Hyperphosphatemia management in patients with chronic kidney disease. Saudi Pharm. J. 2016, 24, 494–505. [Google Scholar] [CrossRef] [PubMed]
- Kuhlmann, M.K. Management of hyperphosphatemia. Hemodial. Int. 2006, 10, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Reid, C.; Seymour, J.; Jones, C. A thematic synthesis of the experiences of adults living with hemodialysis. Clin. J. Am. Soc. Nephrol. 2016, 11, 1206–1218. [Google Scholar] [CrossRef] [PubMed]
- Orsino, A.; Cameron, J.I.; Seidl, M.; Mendelssohn, D.; Stewart, D.E. Medical decision-making and information needs in end-stage renal disease patients. Gen. Hosp. Psychiatry 2003, 25, 324–331. [Google Scholar] [CrossRef]
- Hibbard, J.H.; Greene, J. What the evidence shows about patient activation: Better health outcomes and care experiences; fewer data on costs. Health Aff. 2013, 32, 207–214. [Google Scholar] [CrossRef] [PubMed]
- O’Hare, A.M.; Rodriguez, R.A.; Bowling, C.B. Caring for patients with kidney disease: Shifting the paradigm from evidence-based medicine to patient-centered care. Nephrol. Dial. Transpl. 2016, 31, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Kidney disease: Improving global outcomes (KDIGO) CKD-MBD update work group. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD-MBD). Kidney Int. Suppl. 2017, 7, 1–59. [Google Scholar] [CrossRef] [PubMed]
- Kidney disease: Improving global outcomes (KDIGO) CKD-MBD work group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int. Suppl. 2009, 113, S1–S130. [Google Scholar] [CrossRef]
- Hawthorne, G.; Sansoni, J.; Hayes, L.; Marosszeky, N.; Sansoni, E. Measuring patient satisfaction with health care treatment using the short assessment of patient satisfaction measure delivered superior and robust satisfaction estimates. J. Clin. Epidemiol. 2014, 67, 527–537. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analyses for the Social Sciences; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Yokum, D.; Glass, G.; Cheung, C.F.; Cunningham, J.; Fan, S.; Madden, A.M. Evaluation of a phosphate management protocol to achieve optimum serum phosphate levels in hemodialysis patients. J. Ren. Nutr. 2008, 18, 521–529. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | n = 74 |
|---|---|
| Age—yr (mean, SD) | 67 ± 14.4 |
| Sex—n (%) | |
| Male | 44 (59.5) |
| Female | 30 (40.5) |
| Length of time on dialysis—yr (mean, SD) | 4.8 ± 3.2 |
| Transplant status—n (%) | |
| Not a candidate | 53 (71.6) |
| Active | 6 (8.1) |
| Work up | 10 (13.5) |
| On hold | 5 (6.8) |
| Evidence of calcification—n (%) | 51 (68.9) |
| n = 74 | Pre Intervention | Post Intervention | p-Value | ηp2 * |
|---|---|---|---|---|
| Calcium—mmol/L (mean, SD) ** | 2.21 ± 0.17 | 2.21 ± 0.22 | 0.983 | 0.000 |
| Phosphate—mmol/L (mean, SD) | 1.73 ± 0.51 | 1.68 ± 0.69 | 0.408 | 0.009 |
| Parathyroid hormone—pmol/L (mean, SD) *** | 57.8 ± 33.2 | 59.1 ± 31.2 | 0.784 | 0.001 |
| n = 45 | Pre Intervention | Post Intervention | p-Value | ηp2 * |
|---|---|---|---|---|
| Number of medications | 2.28 ± 1.17 | 2.23 ± 1.098 | 0.375 | 0.143 |
| Number of monthly medication changes | 0.32 ± 0.58 | 0.23 ± 0.484 | 0.146 | 0.245 |
| Milligrams/day | ||||
| Calcium | 2191.11 ±1158.1 | 2018.9 ± 1125.1 | 0.054 | 0.082 |
| Sevelamer | 4512 ± 2115.1 | 4576 ± 2221.4 | 0.784 | 0.003 |
| Lanthanum | 1687.5 ± 1028.2 | 1562.5 ± 1161.4 | 0.391 | 0.250 |
| Cinacalcet | 59.5 ± 29.1 | 58.6 ± 32.0 | 0.861 | 0.001 |
| Cacitriol—oral | 0.0004 ± 0.001 | 0.0003 ± 0.0005 | 0.400 | 0.024 |
| Tablets/day | ||||
| Calcium | 4.16 ± 2.4 | 3.87 ± 2.3 | 0.074 | 0.071 |
| Sevelamer | 5.80 ± 2.53 | 5.88 ± 2.66 | 0.784 | 0.003 |
| Lanthanum | 2.5 ± 0.577 | 2.25 ± 0.957 | 0.391 | 0.250 |
| Cinacalcet | 1.66 ± 0.8 | 1.68 ± 1.03 | 0.902 | 0.001 |
| Cacitriol—oral | 0.96 ± 2.17 | 0.74 ± 1.02 | 0.319 | 0.033 |
| n = 48 * | Very Satisfied | Satisfied | Neither | Dissatisfied | Very Dissatisfied |
|---|---|---|---|---|---|
| Overall Survey Result (n = 48) | (8) | (79) | N/A | (13) | N/A |
| How satisfied are you with the effect of your treatment/care? (n = 52) | 37 (71.2) | 13 (25.0) | 1 (1.9) | 1 (1.9) | 0 (0) |
| How satisfied are you with the explanations the doctor/other healthcare professional has given you about the results of your treatment/care? (n = 52) | 14 (26.9) | 15 (28.8) | 3 (5.8) | 4 (7.7) | 16 (30.8) |
| How satisfied were you with the choices you had in decisions affecting your healthcare? (n = 52) | 20 (38.5) | 30 (57.7) | 2 (3.8) | 0 (0) | 0 (0) |
| Are you satisfied with the care you received in the hospital/clinic? (n = 48) | 29 (59.2) | 19 (38.8) | 1 (2.0) | 0 (0) | 0 (0) |
| All of the Time | Most of the Time | Not Sure | Some of the Time | Never | |
| How much of the time did you feel respected by the doctor/other healthcare professional? (n = 52) | 38 (73.1) | 12 (26.9) | 0 (0) | 0 (0) | 0 (0) |
| Strongly Agree | Agree | Not Sure | Disagree | Strongly Disagree | |
| The time you had with the doctor/other healthcare professional was too short (n = 48) | 9 (18.8) | 23 (47.9) | 6 (12.5) | 10 (20.8) | 0 (0) |
| The doctor/other healthcare professional was very careful to check everything when examining you (n = 52) | 16 (30.8) | 31 (59.6) | 5 (9.6) | 0 (0) | 0 (0) |
| Major Themes (+ sub Themes) | Quotations |
|---|---|
Lack of privacy
| “It’s not confidential between doctor and patient because nine times out of ten you’re in a room with somebody else” “No, so you can’t pose a question you might find embarrassing or questionable to somebody else, and you know basically you don’t want anyone knowing your business” “When they’re giving your test results they should be more private” |
Knowledge and perceptions of bloodwork rounds
| “You can’t really take the time. Nothing against the doctors but they’re like bang bang bang—you don’t have time to say anything. They’re in, they’re out” “Everything is hey how ya doing, looks good, okay bye” |
Issues with taking phosphate binders
| “It’s alright for them to say too much phosphorus, you’re gonna have hardening of your arteries…when? You know 5 years, 2 years, 20 years? If it’s 20 years, why am I getting too excited about it? “The TUMS were too chalky. They weren’t for me” “Well, you’re taking so many pills!” |
Areas for increased patient education
| “If you wanna take a binder and keep these papers, you can... at home, you know, scoot back through it and see what’s been up and what’s been down and, you know, almost scrutinize yourself in some of these things. That’s great. But it should be maybe on a monthly basis” |
| Major Themes (+ sub Themes) | Quotations |
|---|---|
Living with chronic illness
| “Well it goes to show really, we’re all in a very delicate situation.” “If you’re getting feedback from the doctor and the results, and you know your potassium levels are high…then maybe you can make some efforts to minimize you intake- you know it’s up to everybody to make sure they’re as health as they want to be.” |
Satisfaction with care
| “Personally I feel fairly well monitored… and you know looked after” “It’s actually a very good process” |
Individualized care
| “But I think they gotta start treating people not by the book” “And my point is, we are not a number—we are all individuals” |
Fluid and dry weight
| “You come in, and they go by your weight, and they deduct the dry weight they set for you… and you turn around and—I’ve seen me come in, go home, and I’m cramping from my toes right up my body because there’s just no fluid in there” |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baker, T.; Naylor, H.; MacNeil, B.; MacKinnon, M. Evaluation of a Pharmacist–Dietician-Led Patient-Centered Approach to Managing CKD-MBD: A Mixed-Method Study. Pharmacy 2020, 8, 171. https://doi.org/10.3390/pharmacy8030171
Baker T, Naylor H, MacNeil B, MacKinnon M. Evaluation of a Pharmacist–Dietician-Led Patient-Centered Approach to Managing CKD-MBD: A Mixed-Method Study. Pharmacy. 2020; 8(3):171. https://doi.org/10.3390/pharmacy8030171
Chicago/Turabian StyleBaker, Tamara, Heather Naylor, Bryanne MacNeil, and Martin MacKinnon. 2020. "Evaluation of a Pharmacist–Dietician-Led Patient-Centered Approach to Managing CKD-MBD: A Mixed-Method Study" Pharmacy 8, no. 3: 171. https://doi.org/10.3390/pharmacy8030171
APA StyleBaker, T., Naylor, H., MacNeil, B., & MacKinnon, M. (2020). Evaluation of a Pharmacist–Dietician-Led Patient-Centered Approach to Managing CKD-MBD: A Mixed-Method Study. Pharmacy, 8(3), 171. https://doi.org/10.3390/pharmacy8030171




