A Student Pharmacist Quality Engagement Team to Support Initial Implementation of Comprehensive Medication Management within Independent Community Pharmacies
Abstract
1. Introduction
1.1. Background
1.2. Objective
2. Innovation
2.1. Formation and Structure of the QET
2.2. QET Activities
2.3. Utility of the QET
3. Implementation
3.1. Applying an Implementation Framework to the QET Project
3.2. Implementation Strategies Utilized by the QET
4. Outcomes
4.1. QET Project Outcomes
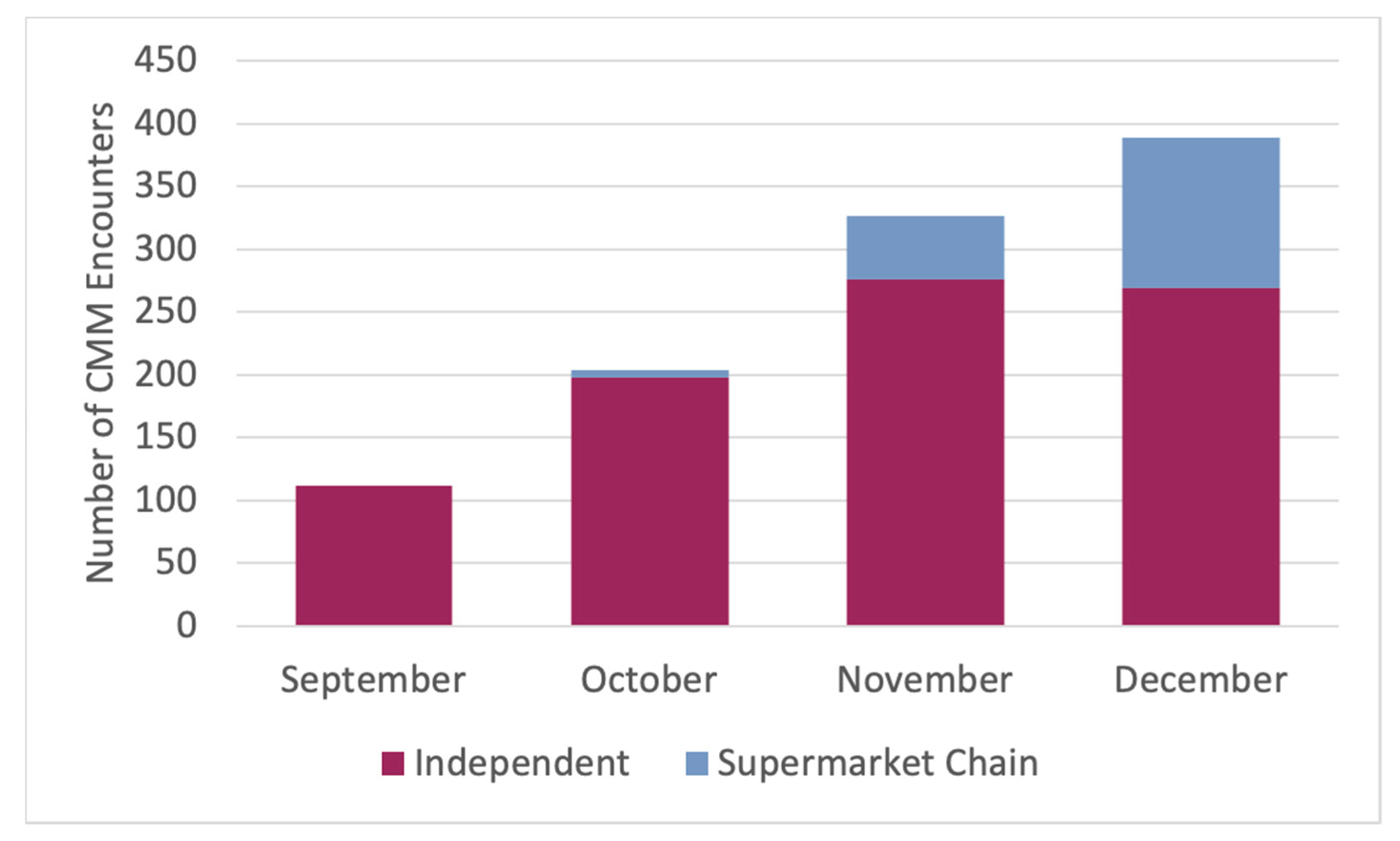
4.2. Adoption of CMM at Participating Pharmacies
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Community Pharmacy Enhanced Services Network (CPESN). Available online: https://cpesn.com (accessed on 9 June 2020).
- McGivney, M.S.; Pope, D.D.; Trygstad, T. Unrealized potential and unrecognized value: Community-based pharmacy practice is reinventing itself—Join the movement. J. Am. Coll. Clin. Pharm. 2019, 2, 330–334. [Google Scholar] [CrossRef]
- Community Care of North Carolina. Community care of North Carolina clinical program analysis. 2015. Available online: https://www.communitycarenc.org/sites/default/files/2017-11/roi-document-may-2015.pdf (accessed on 25 June 2020).
- Farley, J.F.; Ferreri, S.P.; Easter, J.C.; McClurg, M.R. The North Carolina Experiment: Active research in the development and assessment of new practice models. N. C. Med. J. 2017, 78, 186–190. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Strilesky, M. The 7 Components of a Clinical Integration Network. Becker’s Hospital Review. Available online: https://www.beckershospitalreview.com/hospital-physician-relationships/the-7-components-of-a-clinical-integration-network.html (accessed on 1 July 2020).
- Clinically Integrated Networks: Business and Legal Considerations. DHG Healthcare. Available online: https://ohiohospitals.org/getattachment/Member-Services/Personal-Membership-Groups/OSHRM/Turcotte-Yanci-Presentation.pdf.aspx (accessed on 1 July 2020).
- Pennsylvania Pharmacists Association. Available online: https://www.papharmacists.com/general/custom.asp?page=PPCN_Information (accessed on 9 June 2020).
- Pennsylvania Pharmacists Care Network (PPCN). Available online: http://papharmacists.network.com (accessed on 9 June 2020).
- STRAND is now OmniSYS. Available online: https://strandrx.com/ (accessed on 9 June 2020).
- Pharmacist eCare Plan Initiative. Available online: https://www.ecareplaninitiative.com/ (accessed on 9 June 2020).
- OmniSYS. Available online: https://www.omnisys.com/our-solutions/clinical-services/pharmacy-ehr/ (accessed on 9 June 2020).
- The Patient-Centered Medical Home: Integrating Comprehensive Medication Management to Optimize Patient Outcomes Resource Guide. Patient-Centered Primary Care Collaborative. 2012. Available online: https://www.pcpcc.org/sites/default/files/media/medmanagement.pdf (accessed on 9 June 2020).
- Comprehensive Medication Management in Team-Based Care. ACCP. Available online: https://www.accp.com/docs/positions/misc/CMM%20Brief.pdf (accessed on 9 June 2020).
- Community Leadership and Innovation in Practice Center. Available online: https://clip.pharmacy.pitt.edu (accessed on 9 June 2020).
- Blanchard, C.; Livet, M.; Ward, C.; Sorge, L.; Sorensen, T.D.; McClurg, M.R. The Active Implementation Frameworks: A roadmap for advancing implementation of Comprehensive Medication Management in Primary care. Res. Social Adm. Pharm. 2017, 13, 922–929. [Google Scholar] [CrossRef] [PubMed]
- National Implementation Research Network (NIRN). (2013). Active implementation frameworks. Chapel Hill, NC. Available online: https://nirn.fpg.unc.edu/ai-hub (accessed on 25 June 2020).
- Deming, E. The New Economics for Industry, Government, and Education; The MIT Press: Cambridge, MA, USA, 2000. [Google Scholar]
- Powell, B.J.; Waltz, T.J.; Chinman, M.J.; Damschroder, L.J.; Smith, J.L.; Matthieu, M.M.; Proctor, E.K.; Kirchner, J.E. A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015, 10, 21. [Google Scholar] [CrossRef] [PubMed]
- Doong, K.; Berenbrok, L.A.; Coley, K.C.; Carroll, J.C.; Richardson, R.; Antinopoulos, B.C.; Patel, A.; McGivney, M.S. Implementation of comprehensive medication management at supermarket pharmacies in a pharmacy network. J. Am. Pharm. Assoc. 2019, 59, S25–S31. [Google Scholar] [CrossRef] [PubMed]
- Urick, B.Y.; Bhosle, M.; Farley, J.F. Patient medication adherence among pharmacies participating in a North Carolina enhanced services network. J. Manag. Care Spec. Pharm. 2020, 26, 718–722. [Google Scholar] [CrossRef] [PubMed]
- Bacci, J.L.; Bigham, K.A.; Dillon-Sumner, L.; Ferreri, S.; Frail, C.K.; Hamada, C.Y.; Lantaff, W.; McGivney, M.S.; Renner, H.; Snyder, M.E.; et al. Community pharmacist patient care services: A systematic review of approaches used for implementation and evaluation. J. Am. Coll. Clin. Pharm. 2019, 2, 423–432. [Google Scholar] [CrossRef]
- Turner, K.; Weinberger, M.; Renfro, C.; Powell, B.J.; Ferreri, S.; Trodgon, J.G.; Mark, N.; Trygstad, T.; Shea, C.M. Stages of change: Moving community pharmacies from a drug dispensing to population health management model. Med. Care. Res. Rev. 2019. [Google Scholar] [CrossRef] [PubMed]
- Turner, K.; Weinberger, M.; Renfro, C.; Ferreri, S.; Trygstad, T.; Trogdon, J.; Shea, C.M. The role of network ties to support implementation of a community pharmacy enhanced services network. Res. Social Adm. Pharm. 2019, 15, 1118–1125. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.G.; Ferreri, S.P.; Brown, P.; Wines, K.; Shea, C.M.; Pfeiffenberger, T.M. Implementing an integrated care management program in community pharmacies: A focus on medication management services. J. Am. Pharm. Assoc. 2017, 57, 229–235.e1. [Google Scholar] [CrossRef] [PubMed]
- Renfro, C.P.; Turner, K.; Desai, R.; Counts, J.; Shea, C.M.; Ferreri, S.P. Implementation process for comprehensive medication review in the community pharmacy setting. J. Am. Pharm. Assoc. 2019, 59, 836–841.e2. [Google Scholar] [CrossRef] [PubMed]
- Clifton, C.L.; Branham, A.R.; Hayes, H.H., Jr.; Moose, J.S.; Rhodes, L.A.; Marciniak, M.W. Financial impact of patients enrolled in a medication adherence program at an independent community pharmacy. J. Am. Pharm. Assoc. 2018, 58, S109–S113. [Google Scholar] [CrossRef] [PubMed]
- Pestka, D.L.; Frail, C.K.; Palombi, L.C.; Von Hoff, B.A.; Conway, J.M.; Sorensen, T.D. Strategies and steps fostering the success of medication management services in community pharmacies. J. Am. Pharm. Assoc. 2016, 56, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Hall, P.D.; Fish, H.; McBane, S.; Mercer, J.; Moreau, C.; Owen, J.; Policastri, A.; Rattinger, G.B.; Baxi Srivastava, S.; Thomas, M.C.; et al. The Report of the 2018–2019 Professional Affairs Standing Committee: The Role of Educators in Pharmacy Practice Transformation. Am. J. Pharm. Educ. 2019, 83, 7596. [Google Scholar] [CrossRef] [PubMed]
- Somma, M.A.; Meyer, S.M. “Community of Learning” in Experiential Education. Am. J. Pharm. Educ. 2007, 71, 19. [Google Scholar] [CrossRef]
- Draugalis, J.R.; Johnson, E.J.; Urice, D.R. Challenges and lessons amid the COVID-19 pandemic at one college of pharmacy. Am. J. Pharm. Educ. 2020, 84, 8157. [Google Scholar] [CrossRef] [PubMed]
- Academia-CPESN Transformation (ACT) Pharmacy Collaborative. Available online: https://www.actforpharmacy.com/ (accessed on 6 July 2020).
| Category | Sample Questions |
|---|---|
| Comprehensive Medication Management (CMM) Workflow |
|
| Team Involvement in CMM |
|
| Patient Engagement |
|
| Successful Strategies and Implementation Support |
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herbert, S.M.C.; Carroll, J.C.; Coley, K.C.; McGrath, S.H.; McGivney, M.S. A Student Pharmacist Quality Engagement Team to Support Initial Implementation of Comprehensive Medication Management within Independent Community Pharmacies. Pharmacy 2020, 8, 141. https://doi.org/10.3390/pharmacy8030141
Herbert SMC, Carroll JC, Coley KC, McGrath SH, McGivney MS. A Student Pharmacist Quality Engagement Team to Support Initial Implementation of Comprehensive Medication Management within Independent Community Pharmacies. Pharmacy. 2020; 8(3):141. https://doi.org/10.3390/pharmacy8030141
Chicago/Turabian StyleHerbert, Sophia M. C., Joni C. Carroll, Kim C. Coley, Stephanie Harriman McGrath, and Melissa Somma McGivney. 2020. "A Student Pharmacist Quality Engagement Team to Support Initial Implementation of Comprehensive Medication Management within Independent Community Pharmacies" Pharmacy 8, no. 3: 141. https://doi.org/10.3390/pharmacy8030141
APA StyleHerbert, S. M. C., Carroll, J. C., Coley, K. C., McGrath, S. H., & McGivney, M. S. (2020). A Student Pharmacist Quality Engagement Team to Support Initial Implementation of Comprehensive Medication Management within Independent Community Pharmacies. Pharmacy, 8(3), 141. https://doi.org/10.3390/pharmacy8030141







