Trends in Clinical Pharmacist Integration in Family Medicine Residency Programs in North America
Abstract
1. Introduction
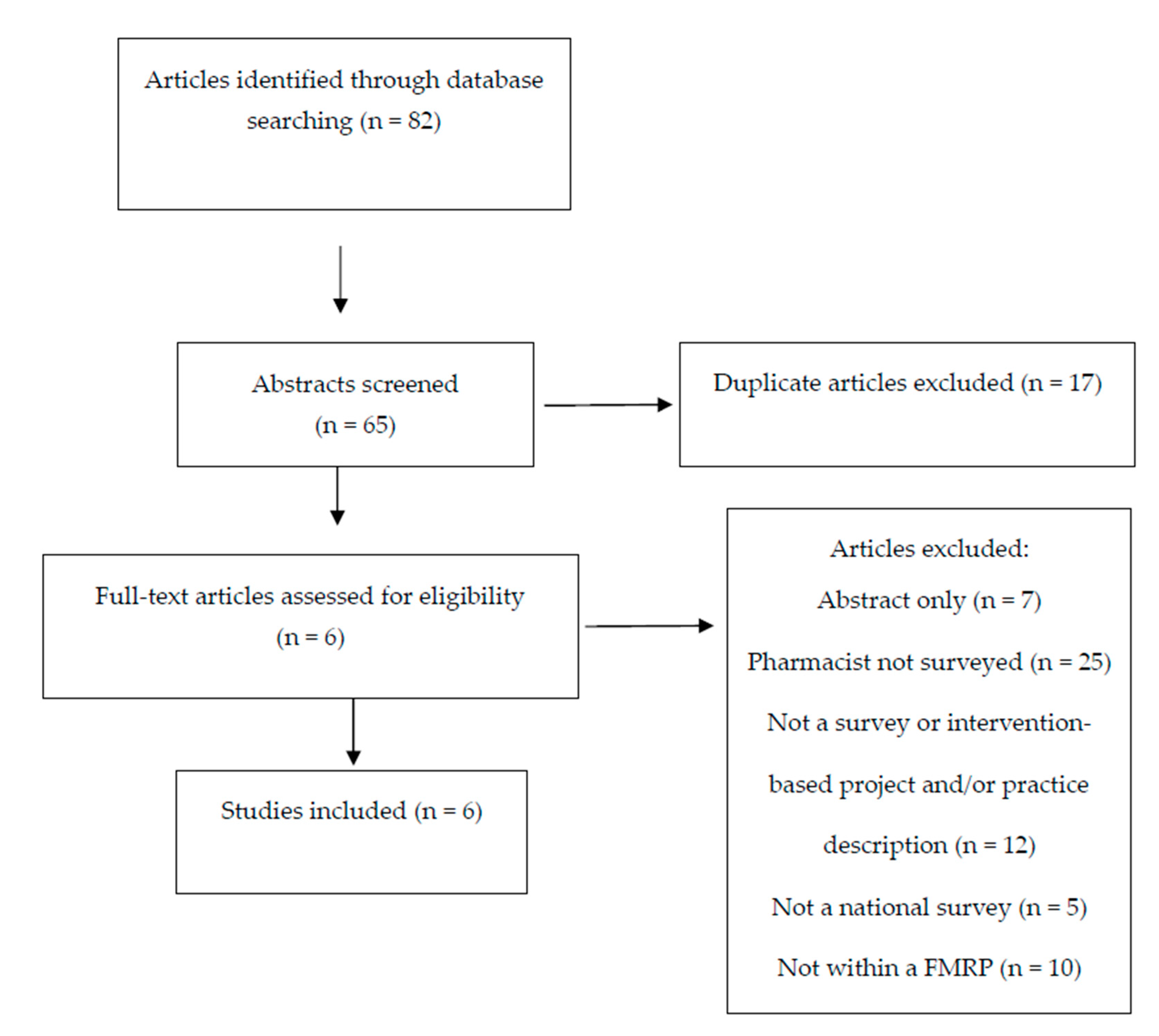
2. Materials and Methods
3. Results
3.1. Prevalence
3.2. Clinical and Educational Scope
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- American College of Clinical Pharmacy. Standards of Practice for Clinical Pharmacists. Pharm. J. Hum. Pharmacol. Drug Ther. 2014, 34, 794–797. [Google Scholar] [CrossRef] [PubMed]
- Joint Comission of Pharmacy Practitioners. Pharmacists’ Patient Care Process. Published Online 29 May 2014. Available online: https://jcpp.net/wp-content/uploads/2016/03/PatientCareProcess-with-supporting-organizations.pdf (accessed on 8 July 2020).
- Branch, W.T.; Kroenke, K.; Levinson, W. The clinician-educator--present and future roles. J. Gen. Intern. Med. 1997, 12 (Suppl. 2), S1–S4. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Moore, T. Pharmacist faculty member in a family medicine residency program. Am. J. Hosp. Pharm. 1977, 34, 973–975. [Google Scholar] [CrossRef] [PubMed]
- Love, D.; Hodge, N.; Foley, W. The clinical pharmacist in a family practice residency program. J. Fam. Pract. 1980, 10, 67–72. [Google Scholar] [PubMed]
- Johnston, T.; Heffron, W. Clinical pharmacy in the family practice residency programs. J. Fam. Pract. 1981, 13, 91–94. [Google Scholar] [PubMed]
- Haxby, D.; Weart, C.; Goodman, B. Family practice physicians’ perceptions of the usefulness of drug therapy recommendations from clinical pharmacists. Am. J. Hosp. Pharm. 1988, 45, 824–827. [Google Scholar] [CrossRef]
- Pottie, K.; Farrell, B.; Haydt, S.; Dolovich, L.; Sellors, C.; Kennie, N.; Hogg, W.; Martin, C.M. Integrating pharmacists into family practice teams: physicians’ perspectives on collaborative care. Can. Fam. Physician 2008, 54, 1714–1717. [Google Scholar]
- Jarrett, J.B.; Lounsbery, J.L.; D’Amico, F.; Dickerson, L.M.; Franko, J.; Nagle, J.; Seehusen, D.; Wilson, S.A. Clinical Pharmacists as Educators in Family Medicine Residency Programs: A CERA Study of Program Directors. Fam. Med. 2016, 48, 180–186. [Google Scholar]
- Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree (Standards 2016). Published Online 2015. Available online: https://www.acpe-accredit.org/pdf/CS_PoliciesandProcedures.pdf (accessed on 2 May 2020).
- Greiner, A.; Knebel, E. (Eds.) Institute of Medicine (US) Committee on The Health Professions Education Summit. Chapter 3, The Core Competencies Needed for Health Care Professionals. In Professions Education: A Bridge. to Quality; National Academies Press (US): Washington, DC, USA, 2003. Available online: https://www.ncbi.nlm.nih.gov/books/NBK221519/ (accessed on 7 April 2017).
- Canadian Council for the Accreditation of Pharmacy Programs (CCAPP). Accreditation Standards for Canadian First Professional Degree in Pharmacy Programs. Published Online January 2018. Available online: http://ccapp-accredit.ca/wp-content/uploads/2016/01/Accreditation-Standards-for-Canadian-First-Professional-Degree-in-Pharmacy-Programs.pdf (accessed on 7 April 2017).
- Canadian Hospital Pharmacy Residency Board. Accreditation Standards. Published Online January 2010. Available online: https://static1.squarespace.com/static/51b156fee4b0d15df77a6385/t/5329d58ae4b0e8b344d59962/1395250570379/CHPRB+Standards+FINAL+2010.pdf (accessed on 19 May 2020).
- American Society of Health-System Pharmacists. ASHP Accreditation Standard for Postgraduate Year One (PGY1) Pharmacy Residency Programs. Published Online September 2016. Available online: https://www.ashp.org/-/media/assets/professional-development/residencies/docs/pgy1-accreditation-standard-2016.ashx?la=en&hash=82D0575273AD83E720B114D62B7926FD35792AFD (accessed on 7 April 2017).
- Saseen, J.J.; Ripley, T.L.; Bondi, D.; Burke, J.M.; Cohen, L.J.; McBane, S.; McConnell, K.J.; Sackey, B.; Sanoski, C.; Simonyan, A.; et al. ACCP Clinical Pharmacist Competencies. Pharm. J. Hum. Pharmacol. Drug Ther. 2017, 37, 630–636. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Kiger, M.E.; Varpio, L. Thematic analysis of qualitative data: AMEE Guide No. 131. Med. Teach. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bendayan, R.; Robinson, J.D.; Stewart, R.B. Pharmaceutical services in family practice medical residency training programs. Am. J. Hosp. Pharm. 1983, 40, 274–277. [Google Scholar] [CrossRef] [PubMed]
- Shaughnessy, A.F.; Hume, A.L. Clinical pharmacists in family practice residency programs. J. Fam. Pract. 1990, 31, 305–309. [Google Scholar] [PubMed]
- Whelan, A.M.; Burge, F.; Munroe, K. Pharmacy services in family medicine residencies. Survey of clinics associated with Canadian residency programs. Can. Fam. Physician 1994, 40, 468–471. [Google Scholar]
- Dickerson, L.M.; Denham, A.M.; Lynch, T. The state of clinical pharmacy practice in family practice residency programs. Fam. Med. 2002, 34, 653–657. [Google Scholar]
- Jorgenson, D.; Muller, A.; Whelan, A.M.; Buxton, K. Pharmacists teaching in family medicine residency programs: National survey. Can. Fam. Physician 2011, 57, e341–e346. [Google Scholar]
- Lounsbery, J.L.; Jarrett, J.B.; Dickerson, L.M.; Wilson, S.A. Integration of Clinical Pharmacists in Family Medicine Residency Programs. Fam. Med. 2017, 49, 430–436. [Google Scholar]
- Johnson, T.J. Pharmacist work force in 2020: Implications of requiring residency training for practice. Am. J. Health-Syst. Pharm. 2008, 65, 166–170. [Google Scholar] [CrossRef][Green Version]
- National Matching Services Inc. ASHP Match Statistics (Updated 2020). 2020. Available online: https://natmatch.com/ashprmp/stats.html (accessed on 20 May 2020).
- Strang, A.F.; Baia, P. An Investigation of Teaching and Learning Programs in Pharmacy Education. Am. J. Pharm. Educ. 2016, 80, 59. [Google Scholar] [CrossRef]
- Havrda, D.E.; Engle, J.P.; Anderson, K.C.; Ray, S.M.; Haines, S.L.; Kane-Gill, S.L.; Ballard, S.L.; Crannage, A.J.; Rochester, C.D.; Parman, M.G.; et al. Guidelines for resident teaching experiences. Pharmacotherapy. 2013, 33, e147–e161. [Google Scholar] [CrossRef]
- Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements (2017 Update). Available online: https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRs_2017-07-01.pdf (accessed on 5 August 2018).
- Hwang, A.Y.; Gums, T.H.; Gums, J.G. The benefits of physician-pharmacist collaboration. J. Fam. Pract. 2017, 66, E1–E8. [Google Scholar] [PubMed]
- Patterson, B.J.; Solimeo, S.L.; Stewart, K.R.; Rosenthal, G.E.; Kaboli, P.J.; Lund, B.C. Perceptions of pharmacists’ integration into patient-centered medical home teams. Res. Soc. Adm. Pharm. 2015, 11, 85–95. [Google Scholar] [CrossRef] [PubMed]
- Bodenheimer, T.; Sinsky, C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann. Fam. Med. 2014, 12, 573–576. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, M.; Kahwati, L.C.; Golin, C.E.; Blalock, S.J.; Coker-Schwimmer, E.; Posey, R.; Lohr, K.N. Medication therapy management interventions in outpatient settings: A systematic review and meta-analysis. JAMA Intern. Med. 2015, 175, 76–87. [Google Scholar] [CrossRef] [PubMed]
| Survey Year (Country) | Total Number of Programs, n | Programs with Responses Obtained, n | Programs with Clinical Pharmacists, n | Programs with Pharmacists out of Programs with Responses, % | Pharmacist Survey Response Rate, % |
|---|---|---|---|---|---|
| 2015 [23] (U.S.) | 480 | 396 | 208 | 52.5 (208/396) | 56.1 (142/253) |
| 2009 [22] (Canada) | 158 | 86 | 40 | 46.5 (40/86) | 80.0 (32/40) |
| 2000 [21] (U.S.) | 579 | 555* | 155 | 27.9 (155/555) | 74.7 (130/174) |
| 1994 [20] (Canada) | 82 | 58 | 8 | 13.8 (8/58) | 100.0 (9/9) |
| 1990 [19] (U.S.) | 381 | 325 | 79 | 24.3 (79/325) | NR |
| 1983 [18] (U.S.) | 386 | NR | 68 | NR | 72.1 (49/68) |
| Characteristic | 1983 [18] (US), n = 49 | 1990 [19] (US), n = 80 | 1994 [20] (Canada), n = 9 | 2000 [21] (US), n = 130 | 2009 [22] (Canada), n = 32 | 2015 [23] (US), n = 142 |
|---|---|---|---|---|---|---|
| Age, years | 13 (27%) <30 | 34.6 (range 24–51) | “Most” were 30–40 | 36.5 ± 8.2 (range 25–59) | 78% <45 | 38.5 ± 9.6 (range 26–67) |
| 29 (59%) 30–40 | ||||||
| 4 (8%) 41–50 | ||||||
| 3 (6%) 51–60 | ||||||
| 0 (0%) >60 | ||||||
| Gender | ||||||
| Male | 37 (76%) | 68% | 1 (11%) | 46% | 36% | 43 (30%) |
| Female | 12 (24%) | 32% | 8 (89%) | 54% | 65% | 99 (70%) |
| Degree | ||||||
| PharmD | 67% | 85% | 1 (11%) | 89% | 76% | 138 (97%) |
| Residency | 53% | 68% | 5 (56%) | 69% | NR | 104 (86%) |
| Academic appointment | ||||||
| C/SOP | 28 (57%) | 61 (76%) | NR | 80% | NR | 105 (74%) |
| C/SOM | 19 (39%) | 29 (36%) | NR | 52% | NR | 69 (49%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jarrett, J.B.; Lounsbery, J.L. Trends in Clinical Pharmacist Integration in Family Medicine Residency Programs in North America. Pharmacy 2020, 8, 126. https://doi.org/10.3390/pharmacy8030126
Jarrett JB, Lounsbery JL. Trends in Clinical Pharmacist Integration in Family Medicine Residency Programs in North America. Pharmacy. 2020; 8(3):126. https://doi.org/10.3390/pharmacy8030126
Chicago/Turabian StyleJarrett, Jennie B., and Jody L. Lounsbery. 2020. "Trends in Clinical Pharmacist Integration in Family Medicine Residency Programs in North America" Pharmacy 8, no. 3: 126. https://doi.org/10.3390/pharmacy8030126
APA StyleJarrett, J. B., & Lounsbery, J. L. (2020). Trends in Clinical Pharmacist Integration in Family Medicine Residency Programs in North America. Pharmacy, 8(3), 126. https://doi.org/10.3390/pharmacy8030126





