Tracking Australian Hajj Pilgrims’ Health Behavior before, during and after Hajj, and the Effective Use of Preventive Measures in Reducing Hajj-Related Illness: A Cohort Study
Abstract
1. Introduction
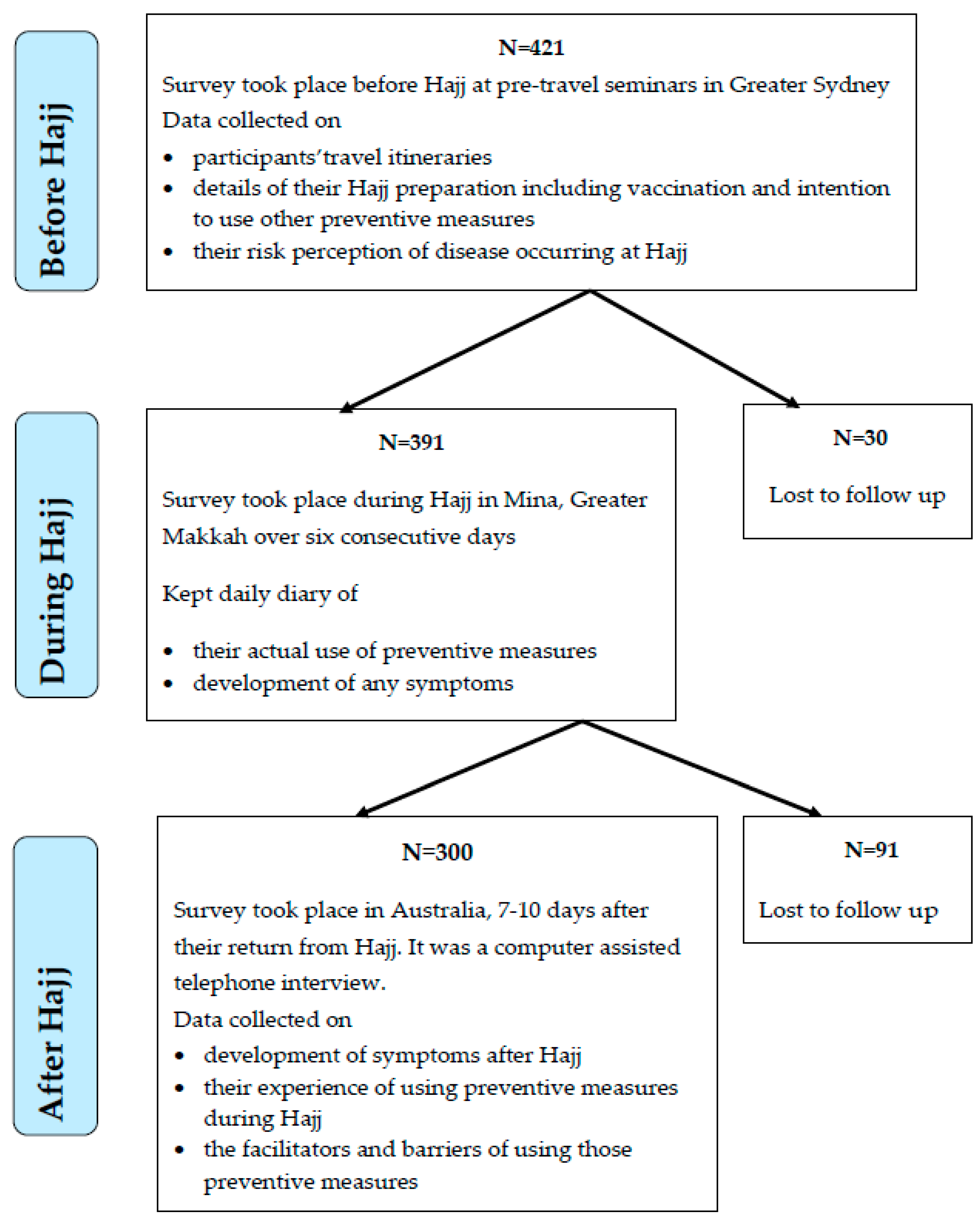
2. Materials and Methods
2.1. Study Population
2.2. Recruitment Methods
2.3. Data Collection
2.3.1. Pre-Hajj Survey
2.3.2. ‘During Hajj’ Survey
2.3.3. Post-Hajj Survey
2.4. Sample Size
2.5. Data Analysis
3. Results
3.1. Demographics
3.2. Vaccine Uptake
3.3. Influenza and Pneumococcal Vaccination Rate Among ‘at Risk’ Individuals
3.4. Barriers, Facilitators and Associated Factors of Vaccine Uptake
3.5. Risk Perception about Diseases
3.6. Non-Pharmacological Preventive Measures
3.6.1. Intention to Use Non-Pharmacological Measures (before Hajj)
3.6.2. Actual Use of Non-Pharmacological Measures during Hajj
3.6.3. Barriers and Facilitators to the Use of Facemasks and Hand Hygiene during Hajj
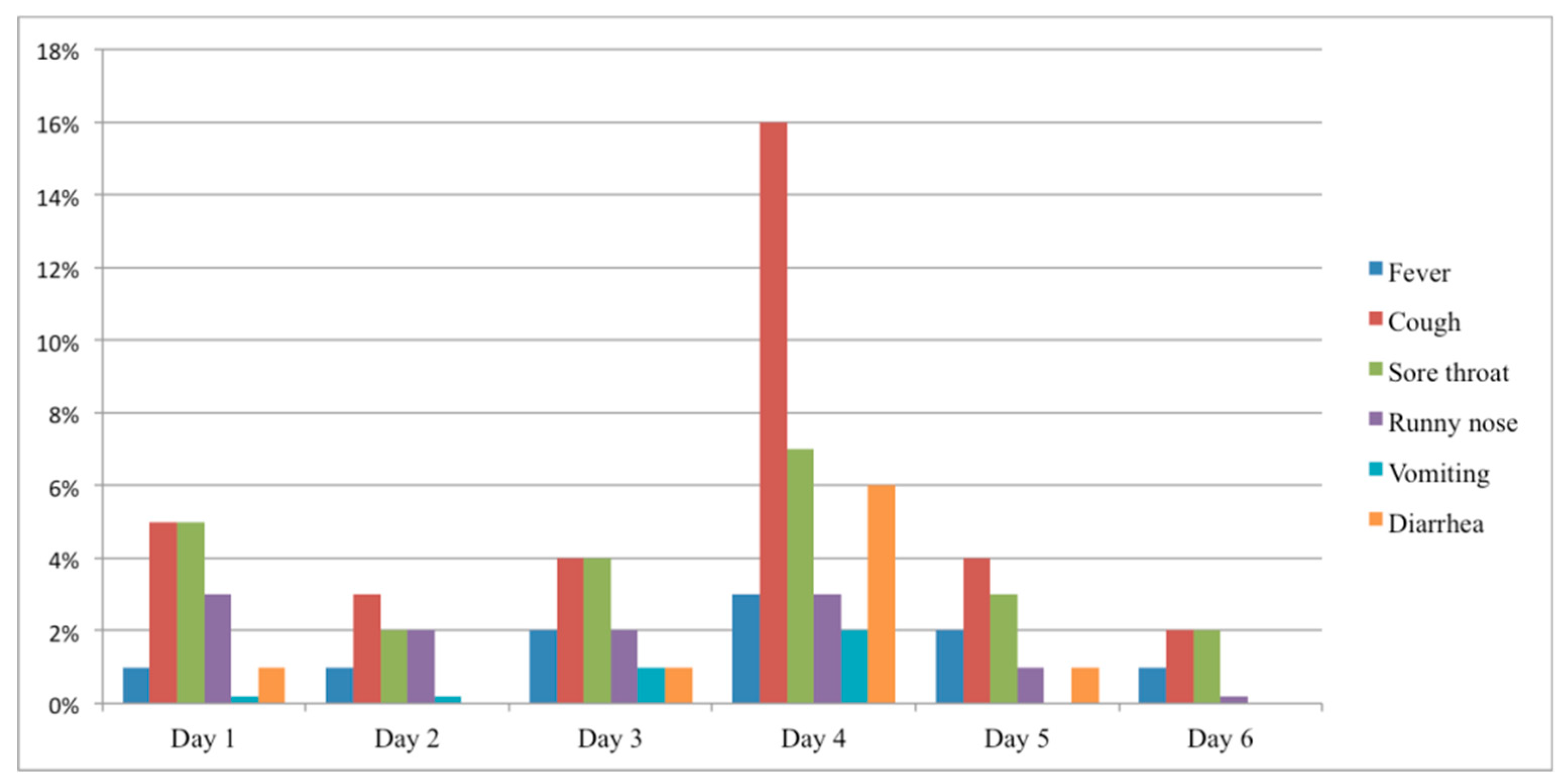
3.7. Incidence of Hajj-Related Illnesses
3.7.1. During Hajj
3.7.2. After Hajj
3.7.3. Effectiveness of Preventive Measures in Reducing Hajj-Related Illnesses
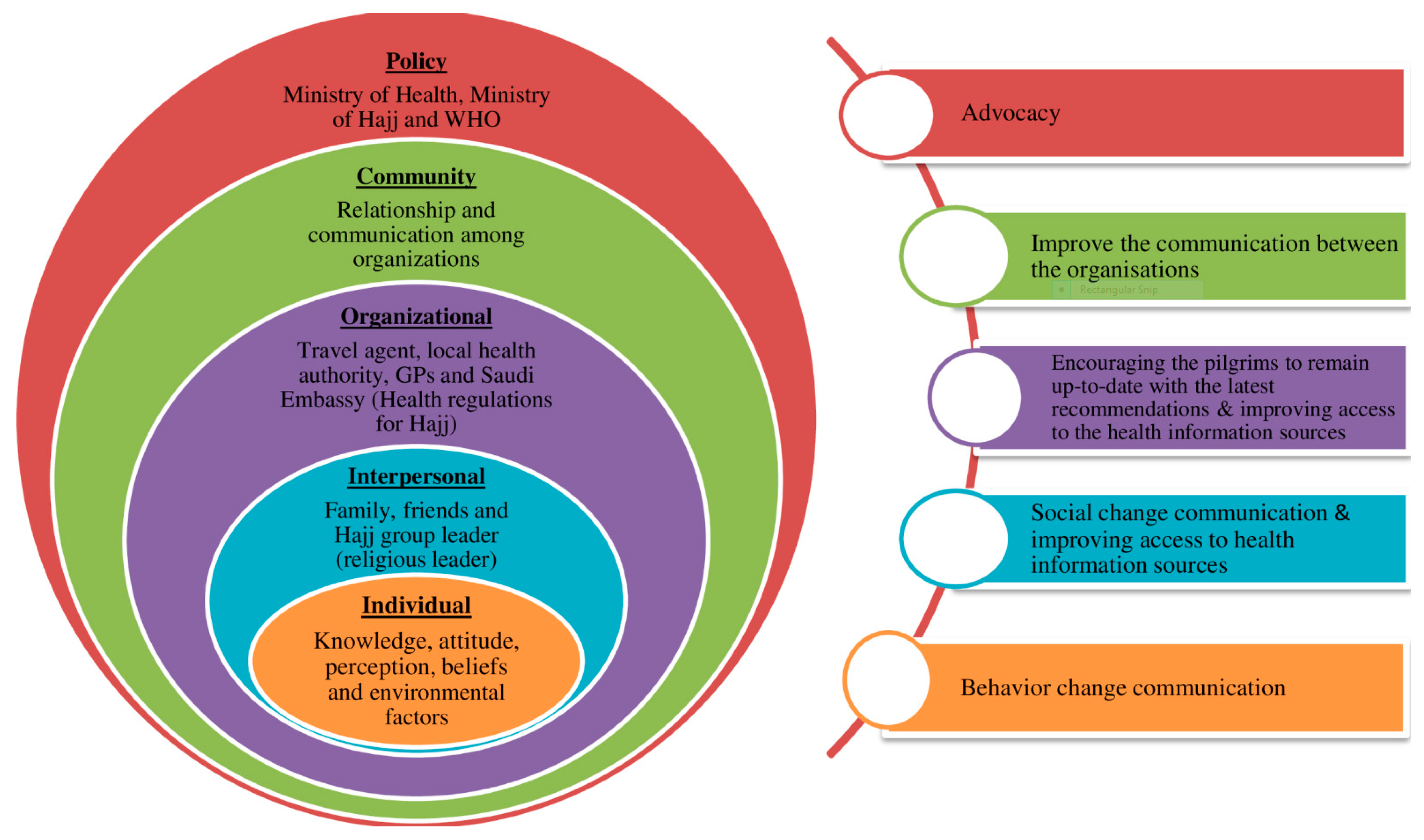
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Memish, Z.A. Health of the Hajj. Science 2018, 361, 533. [Google Scholar] [CrossRef]
- Petersen, E.; Memish, Z.A.; Zumla, A.; Maani, A.A. Transmission of respiratory tract infections at mass gathering events. Curr. Opin. Pulm. Med. 2020, 26, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, A.S.; Heywood, A.E.; Rashid, H. Preparing Australian pilgrims for the Hajj 2018. J. Travel Med. 2018, 25. [Google Scholar] [CrossRef] [PubMed]
- Algarni, H.; Memish, Z.A.; Assiri, A.M. Health conditions for travellers to Saudi Arabia for the pilgrimage to Mecca (Hajj)–2015. J. Epidemiol. Glob. Health 2016, 6, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, A.S.; Rasheed, H.; Heywood, A. Vaccinations against respiratory tract infections at Hajj. Clin. Microbiol. Infect. 2015, 21, 115–127. [Google Scholar] [CrossRef][Green Version]
- Salamati, P.; Razavi, S.M.; Saeednejad, M. Vaccination in Hajj: An overview of the recent findings. Int. J. Prev. Med. 2016, 7, 129. [Google Scholar] [CrossRef]
- Benkouiten, S.; Brouqui, P.; Gautret, P. Non-pharmaceutical interventions for the prevention of respiratory tract infections during Hajj pilgrimage. Travel Med. Infect. Dis. 2014, 12, 429–442. [Google Scholar] [CrossRef]
- Gautret, P.; Vu, H.V.; Sani, S.; Doutchi, M.; Parola, P.; Brouqui, P. Protective Measures Against Acute Respiratory Symptoms in French Pilgrims Participating in the Hajj of 2009: Table 1. J. Travel Med. 2011, 18, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Balaban, V.; Stauffer, W.M.; Hammad, A.; Afgarshe, M.; Abd-Alla, M.; Ahmed, Q.; Memish, Z.A.; Saba, J.; Harton, E.; Palumbo, G.; et al. Protective Practices and Respiratory Illness Among US Travelers to the 2009 Hajj. J. Travel Med. 2012, 19, 163–168. [Google Scholar] [CrossRef][Green Version]
- Balaban, V.; Stauffer, W.; Hammad, A.; Afgarshe, M.; Abd-Alla, M.; Ahmed, Q.; Memish, Z.; Saba, J.; Harton, E.; Palumbo, G.; et al. Predictors of protective behaviors among American travelers to the 2009 Hajj. J. Epidemiol. Glob. Health 2013, 3, 189–190. [Google Scholar] [CrossRef]
- Gautret, P.; Soula, G.; Parola, P.; Brouqui, P. Hajj Pilgrims’ Knowledge about Acute Respiratory Infections. Emerg. Infect. Dis. 2009, 15, 1861–1862. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, Q.A.; Arabi, Y.M.; Memish, Z. Health risks at the Hajj. Lancet 2006, 367, 1008–1015. [Google Scholar] [CrossRef]
- Alqahtani, A.S.; Tashani, M.; Heywood, A.; Booy, R.; Rashid, H.; Wiley, K.; Gautret, P.; Lami, F.; Khader, Y. Exploring Australian Hajj Tour Operators’ Knowledge and Practices Regarding Pilgrims’ Health Risks: A Qualitative Study. JMIR Public Health Surveill. 2019, 5, e10960. [Google Scholar] [CrossRef] [PubMed]
- Barasheed, O.; Rashid, H.; Heron, L.; Ridda, I.; Haworth, E.; Nguyen-Van-Tam, J.S.; Dwyer, D.E.; Booy, R.; Hajj Research Team. Influenza Vaccination Among Australian Hajj Pilgrims: Uptake, Attitudes, and Barriers. J. Travel Med. 2014, 21, 384–390. [Google Scholar] [CrossRef][Green Version]
- Tashani, M.; Barasheed, O.; Azeem, M.; Alfelali, M.; Badahdah, A.-M.; Bokhary, H.; Almasri, N.; AlShehri, J.; Matbouly, G.; Kalantan, N.; et al. Pneumococcal Vaccine Uptake Among Australian Hajj Pilgrims in 2011–2013. Infect. Disord. Drug Targets 2014, 14, 117–124. [Google Scholar] [CrossRef]
- Azeem, M.; Tashani, M.; Barasheed, O.; Heron, L.; Hill-Cawthorne, G.A.; Haworth, E.; Dwyer, D.; Rashid, H.; Booy, R. Knowledge, Attitude and Practice (KAP) Survey Concerning Antimicrobial Use among Australian Hajj Pilgrims. Infect. Disord. Drug Targets 2014, 14, 125–132. [Google Scholar] [CrossRef]
- Alqahtani, A.S.; Tashani, M.; Ridda, I.; Gamil, A.; Booy, R.; Rasheed, H. Burden of clinical infections due to S. pneumoniae during Hajj: A systematic review. Vaccine 2018, 36, 4440–4446. [Google Scholar] [CrossRef]
- Rashid, H.; Muttalif, A.R.A.; Dahlan, Z.B.M.; Djauzi, S.; Iqbal, Z.; Karim, H.M.; Naeem, S.M.; Tantawichien, T.; Zotomayor, R.; Patil, S.; et al. The potential for pneumococcal vaccination in Hajj pilgrims: Expert opinion. Travel Med. Infect. Dis. 2013, 11, 288–294. [Google Scholar] [CrossRef]
- Turkestani, A.; Balahmar, M.; Ibrahem, A.; Moqbel, E.; Memish, Z. Using health educators to improve knowledge of healthy behaviour among Hajj 1432 (2011) pilgrims. East. Mediterr. Health J. 2013, 19, 9–12. [Google Scholar] [CrossRef]
- Alqahtani, A.S.; Fakeerh, M.; Bondagji, D.; Park, S.; Heywood, A.E.; Wiley, K.E.; Booy, R.; Rashid, H. Hand hygiene compliance and effectiveness against respiratory infections among Hajj pilgrims: A systematic review. Infect. Disord. Drug Targets 2018, 18, 1. [Google Scholar] [CrossRef]
- Migault, C.; Kanagaratnam, L.; Hentzien, M.; Giltat, A.; Nguyen, Y.; Brunet, A.; Thibault, M.; LeGall, A.; Drame, M.; Bani-Sadr, F. Effectiveness of an education health programme about Middle East respiratory syndrome coronavirus tested during travel consultations. Public Health 2019, 173, 29–32. [Google Scholar] [CrossRef] [PubMed]
- Barasheed, O.; Alfelali, M.; Mushta, S.; Bokhary, H.; AlShehri, J.; Attar, A.A.; Booy, R.; Rashid, H. Uptake and effectiveness of facemask against respiratory infections at mass gatherings: A systematic review. Int. J. Infect. Dis. 2016, 47, 105–111. [Google Scholar] [CrossRef] [PubMed]
- McLeroy, K.; Bibeau, D.; Steckler, A.; Glanz, K. An Ecological Perspective on Health Promotion Programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, A.S.; BinDhim, N.F.; Tashani, M.; Willaby, H.; Wiley, K.; Heywood, A.E.; Booy, R.; Rashid, H. Pilot use of a novel smartphone application to track traveller health behaviour and collect infectious disease data during a mass gathering: Hajj pilgrimage 2014. J. Epidemiol. Glob. Health 2015, 6, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Moattari, A.; Emami, A.; Moghadami, M.; Honarvar, B. Influenza viral infections among the Iranian Hajj pilgrims returning to Shiraz, Fars province, Iran. Influ. Other Respir. Viruses 2012, 6, e77–e79. [Google Scholar] [CrossRef]
- Benkouiten, S.; Charrel, R.N.; Belhouchat, K.; Drali, T.; Salez, N.; Nougairède, A.; Zandotti, C.; Memish, Z.A.; Al Masri, M.; Gaillard, C.; et al. Circulation of Respiratory Viruses Among Pilgrims During the 2012 Hajj Pilgrimage. Clin. Infect. Dis. 2013, 57, 992–1000. [Google Scholar] [CrossRef]
- Deris, Z.Z.; Hasan, H.; Sulaiman, S.A.; Ab Wahab, M.S.; Naing, N.N.; Othman, N.H. The Prevalence of Acute Respiratory Symptoms and Role of Protective Measures Among Malaysian Hajj Pilgrims. J. Travel Med. 2010, 17, 82–88. [Google Scholar] [CrossRef][Green Version]
- Rashid, H.; Barasheed, O.; Booy, R. Acute febrile respiratory infection symptoms in Australian Hajjis at risk of exposure to Middle East respiratory syndrome coronavirus. Med. J. Aust. 2013, 199, 453. [Google Scholar] [CrossRef]
- Alfelali, M.; Rasheed, H. Prevalence of influenza at Hajj: Is it correlated with vaccine uptake? Infect. Disord. Drug Targets 2014, 14, 213–218. [Google Scholar] [CrossRef]
- Maslamani, Y.A.M.; Choudhry, A.J. Health related experiences among international pilgrims departing through King Abdul Aziz international airport, Jeddah, Saudi Arabia, Hajj 1431 H (201 0). Saudi Epidemiol. Bull. 2011, 18, 42–44. [Google Scholar]
- Hashim, S.; Ayub, Z.N.; Mohamed, Z.; Hasan, H.; Harun, A.; Ismail, N.; Rahman, Z.A.; Suraiya, S.; Naing, N.N.; Aziz, A.A. The prevalence and preventive measures of the respiratory illness among Malaysian pilgrims in 2013 hajj season. J. Travel Med. 2016, 23, 019. [Google Scholar] [CrossRef] [PubMed]
- Alfelali, M.; Barasheed, O.; Tashani, M.; Azeem, M.I.; El Bashir, H.; Memish, Z.A.; Heron, L.; Khandaker, G.; Booy, R.; Rashid, H. Changes in the prevalence of influenza-like illness and influenza vaccine uptake among Hajj pilgrims: A 10-year retrospective analysis of data. Vaccine 2015, 33, 2562–2569. [Google Scholar] [CrossRef]
- Alfelali, M.; Barasheed, O.; Koul, P.; Badahdah, A.-M.; Bokhary, H.; Tashani, M.; Bakarman, M.; Khandaker, G.; Booy, R.; Rashid, H. Influenza vaccine effectiveness among Hajj pilgrims: A test-negative case-control analysis of data from different Hajj years. Expert Rev. Vaccines 2019, 18, 1103–1114. [Google Scholar] [CrossRef] [PubMed]
- Barasheed, O.; Almasri, N.; Badahdah, A.-M.; Heron, L.; Taylor, J.; McPhee, K.; Ridda, I.; Haworth, E.; Dwyer, D.; Rashid, H.; et al. Pilot Randomised Controlled Trial to Test Effectiveness of Facemasks in Preventing Influenza-like Illness Transmission among Australian Hajj Pilgrims in 2011. Infect. Disord. Drug Targets 2014, 14, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Gautret, P.; Bauge, M.; Simon, F.; Benkouiten, S.; Parola, P.; Brouqui, P. Travel Reported by Pilgrims From Marseille, France Before and After the 2010 Hajj: Table 1. J. Travel Med. 2012, 19, 130–132. [Google Scholar] [CrossRef] [PubMed]
- Atique, S.; Itumalla, R. Hajj in the Time of COVID-19. Infect. Dis. Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Hoang, V.-T.; Ali-Salem, S.; Belhouchat, K.; Meftah, M.; Sow, D.; Dao, T.-L.; Ly, T.D.A.; Drali, T.; Ninove, L.; Yezli, S.; et al. Respiratory tract infections among French Hajj pilgrims from 2014 to 2017. Sci. Rep. 2019, 9, 17771–17778. [Google Scholar] [CrossRef]
- Dauda Goni, M.; Hasan, H.; Naing, N.N.; Wan-Arfah, N.; Zeiny Deris, Z.; Nor Arifin, W.; Abubakar Baaba, A. Assessment of Knowledge, Attitude and Practice towards Prevention of Respiratory Tract Infections among Hajj and Umrah Pilgrims from Malaysia in 2018. Int. J. Environ. Res. Public Health 2019, 16, 4569. [Google Scholar] [CrossRef]
- Goni, M.D.; Naing, N.N.; Hasan, H.; Wan-Arfah, N.; Deris, Z.Z.; Arifin, W.N.; Baaba, A.A. Uptake of Recommended Vaccines and Its Associated Factors Among Malaysian Pilgrims During Hajj and Umrah 2018. Front. Public Health 2019, 7, 268. [Google Scholar] [CrossRef]
- Ebrahim, S.H.; Memish, Z.A. Saudi Arabias measures to curb the COVID-19 outbreak: Temporary suspension of the Umrah pilgrimage. J. Travel Med. 2020. [Google Scholar] [CrossRef]
- Ahmed, Q.A.; Memish, Z.A. The cancellation of mass gatherings (MGs)? Decision making in the time of COVID-19. Travel Med. Infect. Dis. 2020, 101631. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | n (%) |
|---|---|
| Age groups | |
| Mean | 42.2 years |
| SD | ± 11.2 |
| Gender | |
| Male | 229 (54) |
| Female | 192 (46) |
| Education | |
| No formal education | 23(5) |
| School certificate (year 10 equivalent) | 75 (18) |
| High school certificate (year 12 equivalent) | 98 (23) |
| Certificate/diploma | 61(15) |
| University degree and higher degree | 164 (39) |
| Employments status | |
| No | 141(34) |
| Yes | 280 (66) |
| Self-employed | 79 (28) |
| Full time | 140 (50) |
| Casual | 25 (9) |
| Part-time | 35 (13) |
| Country of birth | |
| Australia | 128 (30) |
| Middle Eastern countries | 141 (33) |
| Indian sub-continent | 103 (24) |
| Southeast Asian countries | 34 (8) |
| Others | 15 (4) |
| Median years of stay in Australia * | 21.5 years |
| Chronic diseases | |
| No | 303 (72) |
| Yes | 118 (28) |
| Diabetes | 41(35) |
| Asthma | 33 (28) |
| High cholesterol | 30 (25) |
| Hypertension | 28 (24) |
| Heart diseases | 8 (7) |
| Cancer | 3 (3) |
| Other lung diseases | 2 (2) |
| Chronic kidney disease | 2 (2) |
| Immunosuppressive condition (e.g., HIV, long-term steroid use) | 1 (1) |
| Vaccine Name | n (%) |
|---|---|
| Seasonal influenza vaccine | 319 (76) |
| Pneumococcal vaccine | 107 (25) |
| Pertussis (whooping cough) vaccine | 88 (21) |
| Hepatitis A vaccine | 45 (11) |
| Hepatitis B vaccine | 46 (11) |
| MMR (measles, mumps, and rubella) vaccine | 33 (8) |
| dTP (diphtheria, tetanus, polio) | 33 (8) |
| Typhoid vaccine | 29 (7) |
| Polio vaccine | 9 (2) |
| Vaccinated Reasons * | |
| I don’t want to get sick | 212 (65) |
| The vaccine is effective in protecting me against diseases | 64 (20) |
| If I get sick my Hajj worship could be jeopardised | 63 (19) |
| By vaccinating, I can prevent passing diseases to others | 45 (14) |
| I am at risk because I’m at risk/low immunity | 20 (6) |
| Not Vaccinated Reason * | |
| I didn’t know about them | 45 (49) |
| I don’t think I will get a disease at Hajj, I’m under “ALLAH’s” protection | 21 (23) |
| I don’t need them because I’m not at risk | 20 (22) |
| I rely on my own body’s immunity (healthy lifestyle) | 10 (11) |
| The vaccines are too expensive, they should be free | 4 (4) |
| I was afraid of having vaccine side effects | 3 (3) |
| Preventive Measures Use | Frequently n (%) | Infrequently n (%) | Non-Compliant n (%) |
|---|---|---|---|
| Facemask | 76 (19) | 51 (13) | 264 (68) |
| Hand washing with antibacterial gel and soap | 270 (70) | 92 (23) | 28 (7) |
| Use of alcoholic hand rub | 61 (16) | 23 (6) | 306 (79) |
| Hand washing with plain water | 111 (29) | 81 (21) | 198 (51) |
| Hand washing after touching an ill person | 51 (13) | 12 (3) | 327 (84) |
| Use of disposable handkerchiefs | 139 (36) | 64 (16) | 187 (48) |
| Intention n (%) | Actual Use “Yes” n (% *) | p Value | |
|---|---|---|---|
| Facemask | |||
| No | 169 (40) | 40 (24) | 0.9 |
| Possibly | 91 (22) | 22 (24) | |
| Yes | 161 (38) | 34 (21) | |
| Hand washing with antibacterial gel and soap | |||
| No | 55 (13) | 41 (75) | 0.1 |
| Possibly | 60 (14) | 56 (93) | |
| Yes | 306 (73) | 243 (79) | |
| Hand washing with plain water | |||
| No | 92 (22) | 45 (49) | 0.06 |
| Possibly | 46 (11) | 18 (39) | |
| Yes | 283 (67) | 103 (36) | |
| Use of alcoholic hand rub | |||
| No | 196 (47) | 28 (14) | 0.6 |
| Possibly | 58 (14) | 9 (16) | |
| Yes | 167 (40) | 30 (18) | |
| Hand washing after touching an ill person | |||
| No | 87 (21) | 11 (13) | 0.5 |
| Possibly | 39 (9) | 4 (10) | |
| Yes | 295 (70) | 44 (15) | |
| Use of disposable handkerchiefs | |||
| No | 85 (20) | 25 (29) | 0.2 |
| Possibly | 34 (8) | 26 (76) | |
| Yes | 302 (72) | 120 (40) |
| Preventive Measures | Symptoms | Symptoms in Those Who Complied n (%) and Did not Comply with the Preventive Measure n (%) | aOR (95% CI) p |
|---|---|---|---|
| Hand washing with plain water | Fever | 16 (9.4); 28 (12.8) | 0.7 (0.4–1.4), 0.30 |
| Cough | 56 (32.9); 92 (42) | 0.7 (0. 5–1.0), 0.07 | |
| Sore throat | 68 (40); 103 (47) | 0.8 (0.5–1.1), 0.17 | |
| Runny nose | 33 (19.4); 70 (32) | 0.5 (0.3–0.1), 0.03 | |
| Vomiting | 6 (3.5); 8 (3.7) | 1.0 (0.3–2.8), 0.07 | |
| Hand washing with soap and antibacterial products | Fever | 39 (11.5); 5 (10) | 1.2 (0.4–3.1), 0.76 |
| Cough | 132 (38.8); 16 (32) | 1.4 (0.7–2.5), 0.36 | |
| Sore throat | 145 (42.6); 26 (52) | 0.7 (0.4–1.2), 0.22 | |
| Runny nose | 88 (25.9); 15 (30) | 0.8 (0.4–1.6), 0.62 | |
| Vomiting | 13 (3.8); 1 (2) | 2.0 (0.3–15.2), 0.64 | |
| Use of alcoholic hand rub | Fever | 7 (10.3); 37 (11.5) | 0.9 (0.4–2.1), 0.78 |
| Cough | 18 (26.5); 130 (40.4) | 0.4 (0.2–0.9), 0.02 | |
| Sore throat | 29 (42.6); 142 (44.1) | 0.9 (0.6–1.6), 0.83 | |
| Runny nose | 17 (25); 86 (26.7) | 0.9 (0.5–1.7), 0.77 | |
| Vomiting | 3 (4.4); 11 (3.4) | 1.3 (0.4–4.8), 0.40 | |
| Hand washing after touching an ill person | Fever | 7 (11.9); 37 (11.2) | 1.1 (0.5–2.5), 0.89 |
| Cough | 20 (33.9); 128 (38.7) | 0.8 (0.5–1.5), 0.49 | |
| Sore throat | 24 (40.7); 147 (44.4) | 0.9 (0.5–1.5), 0.59 | |
| Runny nose | 19 (32.2); 84 (25.4) | 1.4 (0.8–2.5), 0.27 | |
| Vomiting | 3 (5.1); 11 (3.3) | 1.6 (0.4–5.8), 0.51 | |
| Use of disposable handkerchiefs | Fever | 24 (13.9); 20 (9.3) | 1.6 (0.8–3.0), 0.16 |
| Cough | 68 (39.3); 80 (37) | 1.1 (0.7–1.7), 0.46 | |
| Sore throat | 80 (46.2); 91 (42.1) | 1.18 (0.8–1.8), 0.42 | |
| Runny nose | 52 (30.1); 51 (23.6) | 1.4 (0.9–2.2), 0.15 | |
| Vomiting | 10 (5.8); 4 (1.9) | 3.3 (1.0–10.6), < 0.05 | |
| Facemask | Fever | 13 (10.3); 31 (11.7) | 1.3 (0.7–2.7), 0.43 |
| Cough | 39 (31); 108 (40.9) | 1.2 (0.7–1.9), 0.51 | |
| Sore throat | 39 (31); 131 (49.6) | 0.9 (0.5–1.4), 0.48 | |
| Runny nose | 33 (26.2); 69 (26.1) | 2.1 (1.2–3.6), < 0.01 | |
| Vomiting | 5 (4); 9 (3.4) | 1.7 (0.6–5.3), 0.33 | |
| Influenza vaccine | Fever | 34 (10.7); 1 (10) | 1.2 (0.15–9.6), 0.88 |
| Cough | 105 (32.9); 7 (70) | 0.2 (0.1–0.9), 0.02 | |
| Sore throat | 133 (41.7); 5 (50) | 0.8 (0.2–2.9), 0.77 | |
| Runny nose | 73 (22.9); 5 (50) | 0.3 (0.1–1.2), 0.09 | |
| Vomiting | 10 (3.1); 1 (10) | 0.3 (0.04–2.8), 0.30 | |
| Pneumococcal vaccine | Fever | 10 (9.3); 25 (11.3) | 0.8 (0.4–1.7), 0.55 |
| Cough | 38 (35.5); 74 (33.3) | 1.10 (0.7–1.8), 0.79 | |
| Sore throat | 39 (36.4); 99 (44.6) | 0.7 (0.4–1.1), 0.11 | |
| Runny nose | 27 (25.2); 51 (23) | 1.1 (0.6–1.9), 0.73 | |
| Vomiting | 5 (4.7); 6 (2.7) | 1.7 (0.5–5.8), 0.38 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqahtani, A.S.; Tashani, M.; Heywood, A.E.; Almohammed, A.B.S.; Booy, R.; Wiley, K.E.; Rashid, H. Tracking Australian Hajj Pilgrims’ Health Behavior before, during and after Hajj, and the Effective Use of Preventive Measures in Reducing Hajj-Related Illness: A Cohort Study. Pharmacy 2020, 8, 78. https://doi.org/10.3390/pharmacy8020078
Alqahtani AS, Tashani M, Heywood AE, Almohammed ABS, Booy R, Wiley KE, Rashid H. Tracking Australian Hajj Pilgrims’ Health Behavior before, during and after Hajj, and the Effective Use of Preventive Measures in Reducing Hajj-Related Illness: A Cohort Study. Pharmacy. 2020; 8(2):78. https://doi.org/10.3390/pharmacy8020078
Chicago/Turabian StyleAlqahtani, Amani Salem, Mohamed Tashani, Anita Elizabeth Heywood, Abdulrahman Bader S. Almohammed, Robert Booy, Kerrie Elizabeth Wiley, and Harunor Rashid. 2020. "Tracking Australian Hajj Pilgrims’ Health Behavior before, during and after Hajj, and the Effective Use of Preventive Measures in Reducing Hajj-Related Illness: A Cohort Study" Pharmacy 8, no. 2: 78. https://doi.org/10.3390/pharmacy8020078
APA StyleAlqahtani, A. S., Tashani, M., Heywood, A. E., Almohammed, A. B. S., Booy, R., Wiley, K. E., & Rashid, H. (2020). Tracking Australian Hajj Pilgrims’ Health Behavior before, during and after Hajj, and the Effective Use of Preventive Measures in Reducing Hajj-Related Illness: A Cohort Study. Pharmacy, 8(2), 78. https://doi.org/10.3390/pharmacy8020078






