Pharmacist-Driven Culture and Sexually Transmitted Infection Testing Follow-Up Program in the Emergency Department
Abstract
1. Introduction
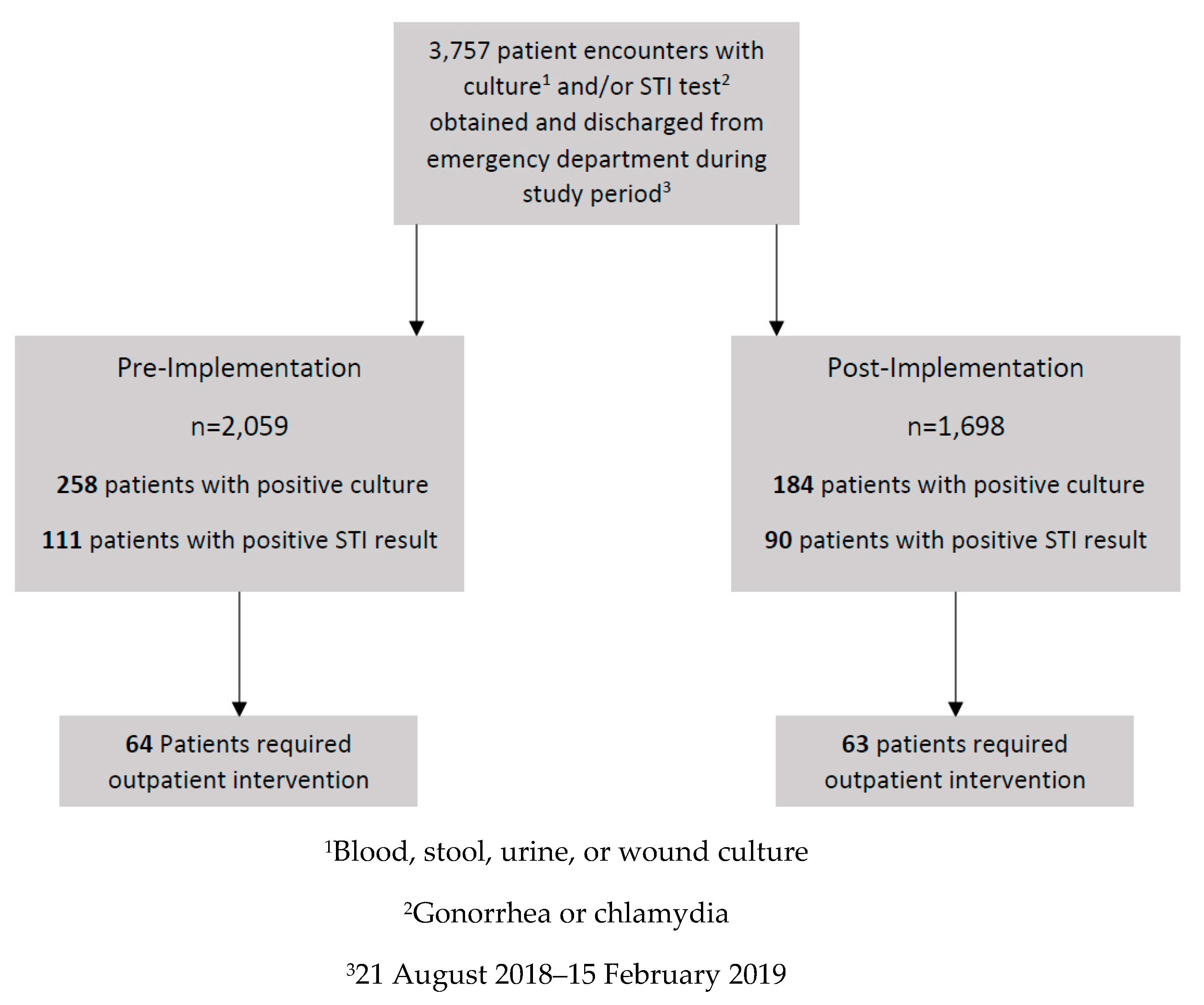
2. Materials and Methods
2.1. Study Setting
2.2. Study Design
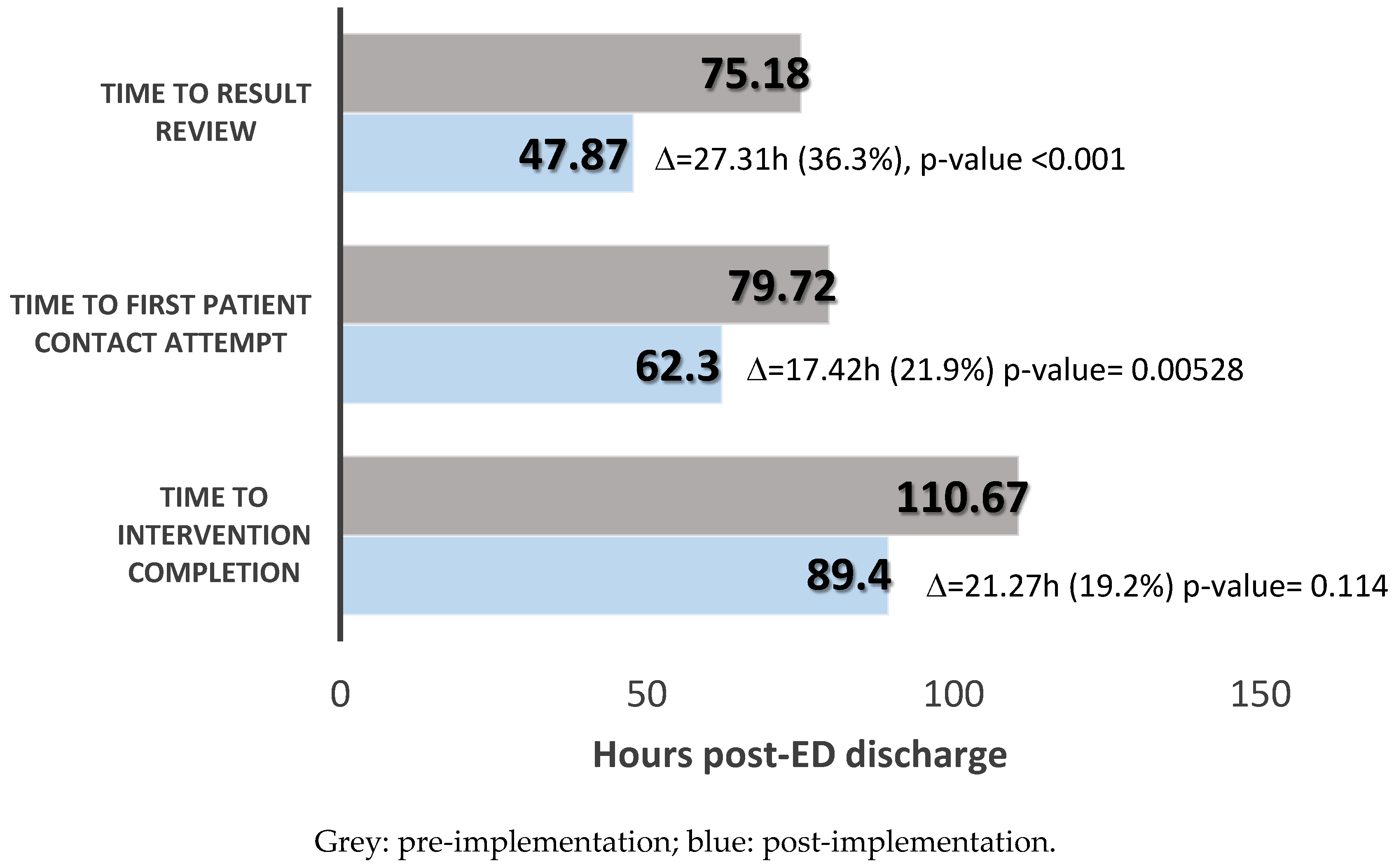
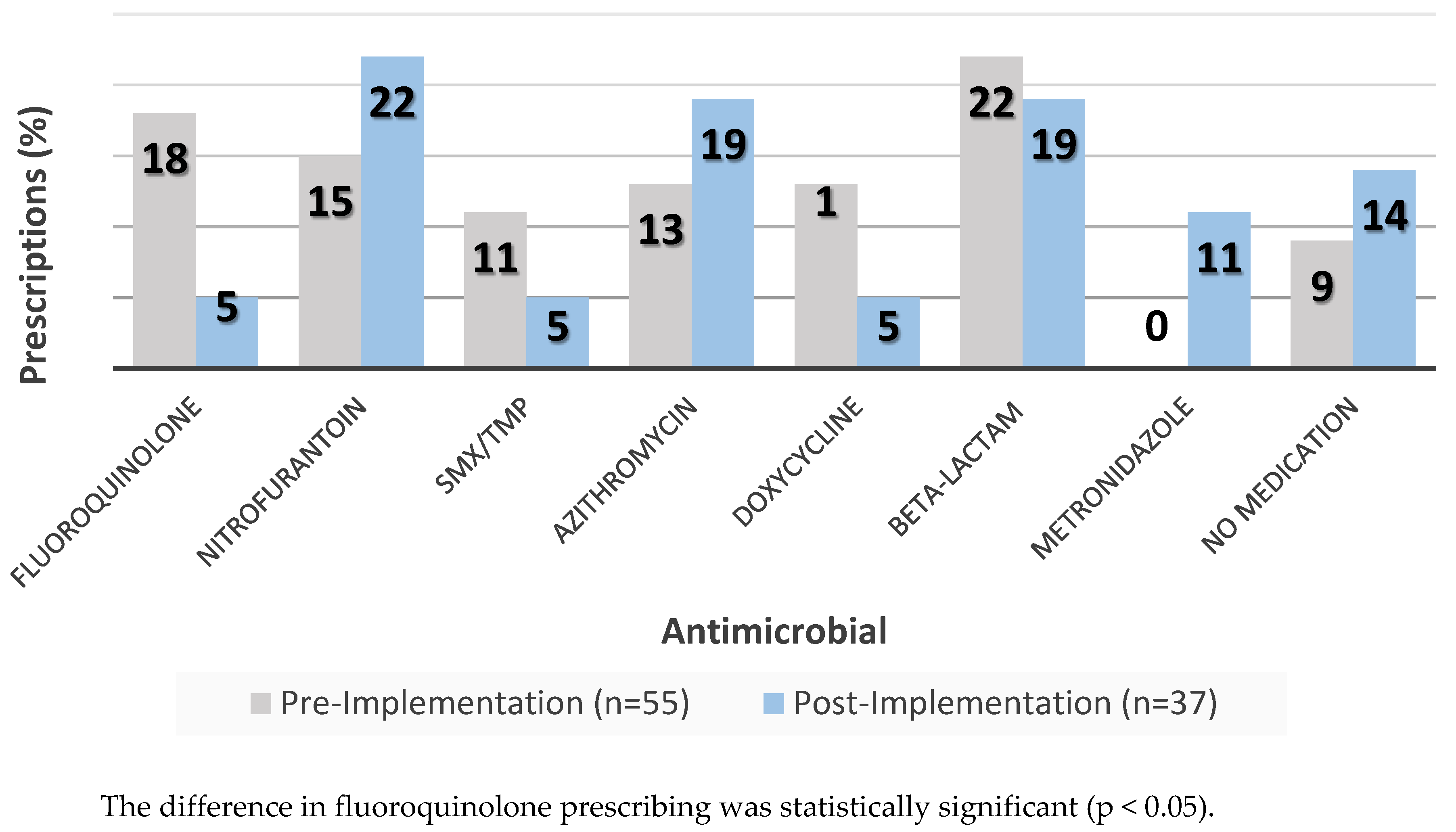
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A

References
- The Joint Commission Department of Standards and Survey Methods. Approved: New Antimicrobial Stewardship Standard. Jt. Comm. Perspect. 2016, 36, 1–8. [Google Scholar]
- Center for Disease Control and Prevention. Core Elements of Outpatient Antimicrobial Stewardship. Available online: www.cdc.gov/antibiotic-use/community/pdfs/16_268900-A_CoreElementsOutpatient_appendix_508.pdf (accessed on 1 August 2018).
- Drekonja, D.M.; Filice, G.A.; Greer, N.; Olson, A.; MacDonald, R.; Rutks, I.; Wilt, T.J. Antimicrobial stewardship in outpatient settings: A systematic review. Infect. Control Hosp. Epidemiol. 2015, 36, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control. Antibiotic Resistance Threats in the United States; CDC: Atlanta, GA, USA, 2013. Available online: www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf (accessed on 1 August 2018).
- Seddon, M.M.; Bookstaver, P.B.; Justo, J.A.; Kohn, J.; Rac, H.; Haggard, E.; Mediwala, K.N.; Dash, S.; Al-Hasan, M.N. Role of early de-escalation of antimicrobial therapy on risk of Clostridioides difficile infection following Enterobacteriaceae bloodstream infections. Clin. Infect. Dis. 2019, 69, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, S.C.; Yeung, S.L.; Zurayk, M.; Terry, J.; Dunn, M.; Nieberg, P.; Pallares, J.; Wong-Beringer, A. Leveraging Antimicrobial Stewardship in the ED to Improve the Quality of Urinary Tract Infection Management and Outcomes. Open Forum Infect. Dis. 2018, 5, ofy101. [Google Scholar] [CrossRef] [PubMed]
- Dumkow, L.E.; Kenney, R.M.; MacDonald, N.C.; Carreno, J.J.; Malhotra, M.K.; Davis, S.L. Impact of a Multidiscinplinary Culture Follow-up Program of Antimicrobial Therpay in the ED. Infect. Dis. Ther. 2014, 3, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Randolph, T.C.; Parker, A.; Meyer, L.; Zeina, R. Effect of a pharmacist-managed culture review process on antimicrobial therapy in an ED. Am. J. Health-Syst. Pharm. 2011, 68, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Baker, S.N.; Acquisto, N.M.; Ashley, E.D.; Fairbanks, R.J.; Beamish, S.E.; Haas, C.E. Pharmacist-managed antimicrobial stewardship program for patients discharged from the ED. J. Pharm. Pract. 2012, 25, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Olson, A.; Pegelow, E.; Cowell, J.; Feldman, R.; Stanton, M.; Ray, J.; Dang, C. Pharmacist-Initiated Culture Follow-Up in the ED Reduces Time to Treatment Optimization. Ann. Emerg. Med. 2017, 70, S61. [Google Scholar] [CrossRef][Green Version]
- May, L.; Tancredi, D.; Mooso, B.; Nguyen, M.; Ondak, S.; Anderson, C.; Briggs, J.; Luong, L.; Miller, L.G. An ED Antimicrobial Stewardship Intervention to Improve Antibiotic Selection and Duration for Skin and Soft-tissue infections in Adult and Pediatric Outpatients. Open Forum Infect. Dis. 2018, 5, S97–S98. [Google Scholar] [CrossRef]
- Bookstaver, P.B.; Jenkins, T.C.; Stenehjem, E.; Doron, S.; Brown, J.; Goldwater, S.H.; Lopes, C.; Haynes, A.; Udeze, C.; Mo, Y.; et al. Impact of Outpatient vs Inpatient ABSSSI Treatment on Outcomes: A Retrospective Observational Analysis of Medical Charts Across US EDs. Open Forum Infect. Dis. 2018, 5, ofy109. [Google Scholar] [CrossRef] [PubMed]
- Fay, L.N.; Wolf, L.M.; Brandt, K.L.; DeYoung, G.R.; Anderson, A.M.; Egwuatu, N.E.; Dumkow, L.E. Pharmacist-led antimicrobial stewardship program in an urgent care setting. Am. J. Health Syst. Pharm. 2019, 76, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.Y.S.; Tabrizi, S.N.; Law, M.; Vodstrcil, L.A.; Chen, M.; Fairley, C.K.; Guy, R.; Bradshaw, C.; Hocking, J.S. Azithromycin versus doxycycline for the treatment of genital chlamydia infection: A meta-analysis of randomized controlled trials. Clin. Infect. Dis. 2014, 59, 193–205. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention 2015 Sexually Transmitted Diseases Treatment Guidelines. Available online: www.cdc.gov/std/tg2015/gonorrhea.htm (accessed on 15 July 2019).
- Bahr, S.J.; Solverson, S.; Schlidt, A.; Hack, D.; Smith, J.L.; Ryan, P. Integrated Literature Review of Post discharge Telephone Calls. West J. Nurs. Res. 2014, 36, 84–104. [Google Scholar] [CrossRef] [PubMed]
- Dan, S.; Shah, A.; Justo, J.A.; Bookstaver, P.B.; Kohn, J.; Albrecht, H.; Al-Hasan, M.N. Prediction of Fluoroquinolone Resistance in Gram-Negative Bacteria Causing Bloodstream Infections. Antimicrob. Agents Chemother. 2016, 60, 2265–2272. [Google Scholar] [CrossRef] [PubMed]
- DeMarsh, M.; Bookstaver, P.B.; Gordon, C.; Lim, J.; Griffith, N.; Bookstaver, N.K.; Justo, J.A.; Kohn, J.; Al-Hasan, M.N. Prediction of Sulfamethoxazole/Trimethoprim Resistance in Community-Onset Urinary Tract Infections. J. Glob. Antimicrob. Resist. 2019. [Google Scholar] [CrossRef] [PubMed]
| Baseline Characteristic, n (%) | Pre-Implementation, n = 64 | Post-Implementation, n = 63 | p-Value |
|---|---|---|---|
| Mean age, years (standard deviation) | 50.67 (23.4) | 42.40 (24.0) | 0.028 |
| Female gender | 51 (79.69) | 51 (80.95) | 1 |
| Result type | 0.17 | ||
| Urine | 46 (71.9) | 36 (57.1) | |
| PCR/molecular testing 1 | 15 (23.4) | 24 (38.1) | |
| Blood cultures | 3 (4.7) | 3 (4.8) | |
| Antibiotic provided upon ED discharge | 0.35 2 | ||
| Nitrofurantoin | 4 (6.3) | 7 (11.1) | |
| Sulfamethoxazole/trimethoprim | 9 (14.1) | 3 (4.8) | |
| Clindamycin | 0 | 1 (1.6) | |
| Metronidazole | 9 (14.1) | 6 (9.5) | |
| No antibiotic | 38 (59.4) | 38 (60.3) | |
| Other | 1 (1.6) | 0 | |
| Beta-lactam | 1 (1.6) | 2 (3.2) | 0.62 |
| Fluoroquinolone | 2 (3.1) | 4 (6.4) | 0.44 |
| Type of Intervention, n (%) | Pre-Implementation, n = 64 | Post-Implementation, n = 63 | p-Value |
|---|---|---|---|
| Initiation of therapy | 25 (39) | 19 (30.2) | 0.39 |
| Modification of therapy | 24 (37.5) | 14 (22.2) | 0.09 |
| Contact primary care provider | 4 (6.3) | 8 (12.7) | 0.35 |
| Contact nursing home | 5 (7.8) | 7 (11.1) | 0.74 |
| No medication 1 | 5 (7.8) | 5 (7.9) | 1 |
| Letter sent | 3 (4.7) | 12 (19) | 0.026 |
| Outcome, n (%) | Pre-implementation, n = 64 | Post-implementation, n = 63 | p-Value |
|---|---|---|---|
| Patients with repeat ED encounter within 30 days | 10 (15.6) | 12 (19.1) | 0.783 |
| Patients with repeat ED encounter related to index case | 5 (7.3) | 0 | -- |
| Patients with hospital admissions within 30 days | 6 (9.4) | 5 (7.9) | 1 |
| Patients with unintended repeat hospital admission related to index case | 2 (2.9) | 1 (1.7) | -- |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shealy, S.C.; Alexander, C.; Hardison, T.G.; Magagnoli, J.; Justo, J.A.; Derrick, C.; Kohn, J.; Winders, H.R.; Privette, T.; Al-Hasan, M.N.; et al. Pharmacist-Driven Culture and Sexually Transmitted Infection Testing Follow-Up Program in the Emergency Department. Pharmacy 2020, 8, 72. https://doi.org/10.3390/pharmacy8020072
Shealy SC, Alexander C, Hardison TG, Magagnoli J, Justo JA, Derrick C, Kohn J, Winders HR, Privette T, Al-Hasan MN, et al. Pharmacist-Driven Culture and Sexually Transmitted Infection Testing Follow-Up Program in the Emergency Department. Pharmacy. 2020; 8(2):72. https://doi.org/10.3390/pharmacy8020072
Chicago/Turabian StyleShealy, Stephanie C., Christine Alexander, Tina Grof Hardison, Joseph Magagnoli, Julie Ann Justo, Caroline Derrick, Joseph Kohn, Hana Rac Winders, Troy Privette, Majdi N. Al-Hasan, and et al. 2020. "Pharmacist-Driven Culture and Sexually Transmitted Infection Testing Follow-Up Program in the Emergency Department" Pharmacy 8, no. 2: 72. https://doi.org/10.3390/pharmacy8020072
APA StyleShealy, S. C., Alexander, C., Hardison, T. G., Magagnoli, J., Justo, J. A., Derrick, C., Kohn, J., Winders, H. R., Privette, T., Al-Hasan, M. N., & Bookstaver, P. B. (2020). Pharmacist-Driven Culture and Sexually Transmitted Infection Testing Follow-Up Program in the Emergency Department. Pharmacy, 8(2), 72. https://doi.org/10.3390/pharmacy8020072







