Alignment of Community Pharmacy Foundation Grant Funding and the Evolution of Pharmacy Practice in the United States of America
Abstract
:1. Introduction
- The development, processing, and use of findings that affirm the value of community pharmacy practice in the healthcare delivery system.
- The measurement, publication, and dissemination of findings documenting the value of professional services delivered to patients by community pharmacists.
- Efforts that measure the impact of pharmacist interventions in achieving the targeted therapeutic goals set collaboratively by the patient, the pharmacist, and other members of the healthcare team.
- Efforts that evaluate patient-specific outcomes with regard to the quality of care delivered by community pharmacists.
2. Colonial America: The Roots of Pharmacy Practice in the United States
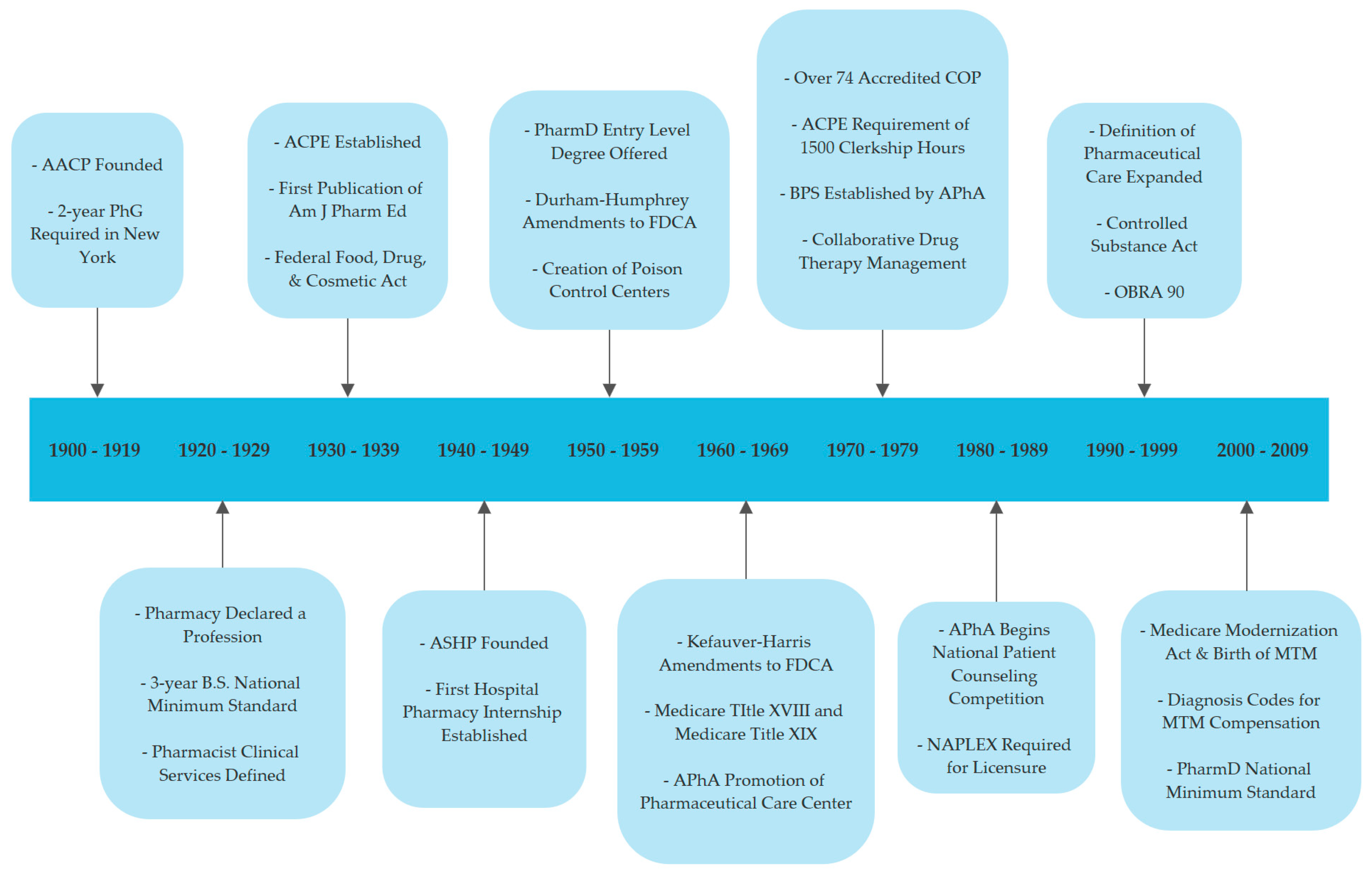
3. CPF Grant Funding Aligns with the Evolution of Pharmacy Practice in the United States
3.1. The Pharmaceutical Care Era
3.2. Relationship of Medication Therapy Management to the Practice of Pharmaceutical Care
3.3. The Value-Based Care Era
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Community Pharmacy Foundation. History & Origin. Community Pharmacy Foundation, 2019. Available online: https://communitypharmacyfoundation.org/about/default.asp (accessed on 24 April 2019).
- Isetts, B.J.; Olson, A.W.; Kondic, A.M.; Schommer, J. An Evaluation of the Distribution, Scope, and Impact of Community Pharmacy Foundation Grants Completed by Academic Principal Investigators between 2002 and 2014. Innov. Pharm. 2017, 8, 1–10. [Google Scholar] [CrossRef]
- Olson, W.A.; Isetts, B.J.; Kondic, A.M.; Schommer, J. Comparing the Research Contributions of Community Pharmacy Foundation Funding on Practice Innovation between Non-Academics and Academics. Innov. Pharm. 2017, 8, 1–8. [Google Scholar] [CrossRef]
- Baker, D.M.; Colbert, J.; Miller, S.; Nagel-Edwards, K.; Wensel, T.M.; Samuel, E.; Jusczak, P. AACP History Special Interest Group Model PowerPoint Presentations. American Institute of the History of Pharmacy, 2019. Available online: https://aihp.org/historical-resources/teaching/aacp-sig-model-presentations/ (accessed on 21 April 2019).
- Hogshire, J. Pills-a-Go-Go: The Fiendish Investigation into Pill Marketing, Art, History, and Consumption; Feral House: Los Angeles, CA, USA, 1999. [Google Scholar]
- McCarthy, R. Lecture One: Early Pharmacy in America. American Institute of the History of Pharmacy, 2019. Available online: https://aihp.org/historical-resources/teaching/ (accessed on 23 April 2019).
- Alpers, W.C. The history of the American Pharmaceutical Association. J. Am. Pharm. Assoc. 1912, 1, 972–992. [Google Scholar] [CrossRef] [Green Version]
- Drug Topics. From Apothecary to PharmD: 160 Years of Caring for Patients. Drug Topics, 2016. Available online: https://www.drugtopics.com/chains-business/apothecary-pharmd-160-years-caring-patients (accessed on 25 April 2019).
- Clark, T. Celebrating 50 years of advancement in pharmacy residency training. Am. J. Health Syst. Pharm. 2014, 71, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
- Stolpe, S.F.; Adams, A.J.; Bradley-Baker, L.R.; Burns, A.L.; Owen, J.A. Historical Development and Emerging Trends of Community Pharmacy Residencies. Am. J. Pharm. Educ. 2011, 75, 160. [Google Scholar] [CrossRef] [PubMed]
- Isetts, B.J. Systems of pharmaceutical care. In Managing Pharmacy Practice: Principles, Strategies, and Systems; Peterson, A.M., Ed.; CRC Press: New York, NY, USA, 2004; pp. 233–260. [Google Scholar]
- Mikeal, R.L.; Brown, T.P.; Lazarus, H.L.; Vinson, M.C. Quality of pharmaceutical care in hospitals. Am. J. Health Syst. Pharm. 1975, 32, 567–574. [Google Scholar] [CrossRef]
- Hepler, C.D.; Strand, L.M. Opportunities and responsibilities in pharmaceutical care. Am. J. Hosp. Pharm. 1990, 47, 533–543. [Google Scholar] [CrossRef]
- Zillich, A.J.; Sutherland, J.M.; Kumbera, P.A.; Carter, B.L. Hypertension Outcomes through Blood Pressure Monitoring and Evaluation by Pharmacists (HOME Study). J. Gen. Intern. Med. 2005, 20, 1091–1096. [Google Scholar] [CrossRef]
- Mott, D. Pharmacy Participation in and Nature of Claims Submitted to the Wisconsin Medicaid Pharmaceutical Care Program. Community Pharmacy Foundation, 2005. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_35597.pdf (accessed on 26 April 2019).
- Doucette, W.R. Extended Diabetes Care through Diabetes Center-Community Pharmacy Collaboration. Community Pharmacy Foundation, 2006. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_5689.pdf (accessed on 26 April 2019).
- Chui, M. Evaluation of online prospective DUR programs in community pharmacy practice. JMCP 2000, 6, 27–32. [Google Scholar] [CrossRef]
- Owen, J. Asthma Care Improvement Initiative Study. Community Pharmacy Foundation, 2005. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_93056.pdf (accessed on 26 April 2019).
- Wertheimer, A. Effect of Prior Authorization and Formulary Limitation on Community Pharmacy Practice and Profitability. Community Pharmacy Foundation, 2005. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_86425.pdf (accessed on 26 April 2019).
- Shepherd, M.D.; Richards, K.M.; Winegar, A.L. Time from Medicare Part D claim adjudication to community pharmacy payment. J. Am. Pharm. Assoc. 2007, 47, 695–701. [Google Scholar] [CrossRef]
- Harrington, C. Pharmacy Based Activity to Reverse and Manage Disease (PHARMD): The Hypertension Project The Community Pharmacy Foundation. 2004. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_74116.pdf (accessed on 26 April 2019).
- Isetts, B.J. The Global Perspective—United States. In Pharmaceutical Care Practice, 3rd ed.; Cipolle, R.J., Strand, L.M., Morley, P.C., Eds.; McGraw Hill: New York, NY, USA, 2012. [Google Scholar]
- Medicare Payment Advisory Commission HGC. Report to the Congress: Medicare Coverage of Nonphysician Practitioners; Medicare Payment Advisory Commission: Washington, DC, USA, 2002.
- Isetts, B.J.; Buffington, D.E. CPT code change proposal: National data on pharmacists medication therapy management services. J. Am. Pharm. Assoc. 2007, 47, 491–495. [Google Scholar] [CrossRef] [PubMed]
- American Medical Association. CPT Changes 2006: An Insider’s View; American Medical Association: Chicago, IL, USA, 2005; pp. 309–312. [Google Scholar]
- Westberg, S.M.; Pittenger, A.; Dickson, K.; Brummel, A.; Odell, L.; Johnson, J.K. Advancing Medication Therapy Management Services: Creating increased awareness and utilization of MTMS CPT billing codes Community Pharmacy Foundation. 2010. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_68855.pdf (accessed on 29 April 2019).
- Centers for Disease Control and Prevention. Community Pharmacists and Medication Therapy Management|CDC|DHDSP. Centers for Disease Control and Prevention, 2018. Available online: https://www.cdc.gov/dhdsp/pubs/guides/best-practices/pharmacist-mtm.htm (accessed on 24 April 2019).
- Isetts, B.J. Pharmaceutical care, MTM, & payment: The past, present, & future. Ann. Pharmacother. 2012, 46, S47–S56. [Google Scholar] [PubMed]
- American Pharmacists Association; National Association of Chain Drug Stores Foundation. Medication therapy management in pharmacy practice: core elements of an MTM service model (version 2.0). J. Am. Pharm. Assoc. 2008, 48, 341–353. [Google Scholar] [CrossRef] [PubMed]
- Temple, T.; Puentz, K.; Doucette, W.R. Implementation of the Pharmaceutical Case Management Model in a Private Sector Health Plan. Community Pharmacy Foundation, 2008. Available online: https://communitypharmacyfoundation.org/grants/grants_list_details.asp?grants_id=70378 (accessed on 27 April 2019).
- Doucette, W.R. An Initial Evaluation of Medication Therapy Management (MTM) Services in the Upper Midwest Region. Community Pharmacy Foundation, 2009. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_2886.pdf (accessed on 27 April 2019).
- Osborne, M.A.; Snyder, M.E.; Hall, D.L.; Coley, K.C.; McGivney, M.S. Evaluating Pennsylvania Pharmacists’ Provision of Community-based Patient Care Services. Innov. Pharm. 2011, 2, 1–9. [Google Scholar] [CrossRef]
- Trapskin, K.; Johnson, C.; Cory, P.; Sorum, S.; Decker, C. Forging a novel provider and payer partnership in Wisconsin to compensate pharmacists for quality-driven pharmacy and medication therapy management services. J. Am. Pharm. Assoc. 2009, 49, 642–651. [Google Scholar] [CrossRef]
- Rashed, S.M.; Goldstein, S.; Tolley, E.A.; Wilson-Relyea, B.J. Cost Outcomes of Diabetes Education in a specialized community pharmacy. Am. J. Pharm. Benefits 2010, 2, 421–428. [Google Scholar]
- Pudlo, A.; Abernathy, M.; Peek, J. Financial analysis of MTM Services Implemented in a Non-MTM Participating Pharmacy. Community Pharmacy Foundation, 2011. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_20787.pdf (accessed on 27 April 2019).
- McDonough, R.P.; Doucette, W.R.; Urmie, J.M.; Patterson, B.J. A Comprehensive Longitudinal Assessment of an Innovative Community Pharmacy Practice Community Pharmacy Foundation. 2012. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_54202.pdf (accessed on 29 April 2019).
- Garrelts MacLean, L.; Schwartz, C.; Sclar, D.A.; Wu, A.; Whitcomb Henry, H. Community Pharmacy Based Rapid Strep Testing with Prescriptive Authority. Community Pharmacy Foundation, 2009. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_12587.pdf (accessed on 29 April 2019).
- Bleske, B.E.; Dillman, N.O.; Cornelius, D.; Ward, J.K.; Burson, S.C.; Diez, H.L.; Pickworth, K.K.; Bennett, M.S.; Nicklas, J.M.; Dorsch, M.P. Heart failure assessment at the community pharmacy level: A feasibility pilot study. J. Am. Pharm. Assoc. 2014, 54, 634–641. [Google Scholar] [CrossRef]
- American Pharmacists Association Foundation. Incentive Grants. APhA Foundation. Available online: https://www.aphafoundation.org/incentive-grants (accessed on 2 June 2019).
- Schommer, J.C.; Bonnarens, J.K.; Brown, L.M.; Venable, J.; Good, K.R. Value of community pharmacy residency programs: College of pharmacy and practice site perspectives. J. Am. Pharm. Assoc. 2010, 50, e72–e88. [Google Scholar] [CrossRef]
- Owen, J.A. PGY1 Community Pharmacy Residency Implementation Guide. Community Pharmacy Foundation, 2014. Available online: https://communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_4805.pdf (accessed on 27 April 2019).
- Pharmacy Quality Alliance. Strategies to Expand Value-Based Pharmacist-Provided Care. Action Guide: For Community Pharmacists, Healthcare Prayers, and Other Stakeholders. 2019. Available online: https://www.pqaalliance.org/pharmacist-provided-care (accessed on 27 April 2019).
- Twigg, G.A.; Motsko, J.; Sherr, J.; El-Baff, S. Interprofessional Approach to Increase Billable Care-Events in a Rural Community. Innov. Pharm. 2017, 8, 1–8. [Google Scholar] [CrossRef]
- Mager, N.A.; Bright, D.R.; Markus, D.; Weis, L.; Hartzell, D.M.; Gartner, J. Use of targeted medication reviews to deliver preconception care: A demonstration project. J. Am. Pharm. Assoc. 2017, 57, 90–94. [Google Scholar] [CrossRef]
- Phillips, R.C.; Ferreri, S. Integrating Community Pharmacists into Team-Based Care Community Pharmacy Foundation. 2018. Available online: www.communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_52603.pdf (accessed on 27 April 2019).
- Engstrom, K.A. Pharmacist Based Medication Therapy Management is an Essential Part of Patient Centered Medical Home Community Pharmacy Foundation. 2013. Available online: https://www.communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_59132.pdf. Published 2013 (accessed on 29 April 2019).
- Heetderks, L.; Paluta, L. Demonstrating the Impact and Feasibility of a Business Model which includes a Community-Based Pharmacist in a Patient Centered Medical Home (PCMH) Practice. Community Pharmacy Foundation, 2014. Available online: https://www.communitypharmacyfoundation.org/resources/grant_docs/CPFGrantDoc_46853.pdf (accessed on 29 April 2019).
- Luder, H.R.; Shannon, P.; Kirby, J.; Frede, S.M. Community pharmacist collaboration with a patient-centered medical home: Establishment of a patient-centered medical neighborhood and payment model. J. Am. Pharm. Assoc. 2018, 58, 44–50. [Google Scholar] [CrossRef]
- Wilson, C.; Twigg, G.A. Pharmacist-led depression screening and intervention in an underserved, rural, and multi-ethnic diabetic population. J. Am. Pharm. Assoc. 2016, 58, 205–209. [Google Scholar] [CrossRef]
- Centers for Medicare and Medicaid Services. Accountable Care Organizations (ACOs): General Information Center for Medicare & Medicaid Innovation. Centers for Medicare and Medicaid Services, 2019. Available online: https://innovation.cms.gov/initiatives/aco/ (accessed on 27 April 2019).
- Isetts, B. Integrating Medication Therapy Management (MTM) Services Provided by Community Pharmacists into a Community-Based Accountable Care Organization (ACO). Pharmacy 2017, 5, 56. [Google Scholar] [CrossRef]
- Board of Pharmacy Specialties. History. Board of Pharmacy Specialties, 2019. Available online: https://www.bpsweb.org/about-bps/history/ (accessed on 27 April 2019).
- Skelton, J.B.; Owen, J.A. Developing a vision and strategic plan for future community-based residency training. J. Am. Pharm. Assoc. 2016, 56, 584–589. [Google Scholar] [CrossRef]
| AHRQ Level | AHRQ Level Description |
|---|---|
| 1 | Studies that add to the knowledge base only and do not represent direct change in policy or practice |
| 2 | Studies that may lead to a policy or program change as a direct result of the research |
| 3 | Studies that may cause a potential change in what clinicians or patients do, or result in a change in a care pattern |
| 4 | Studies that may change actual health outcomes (clinical, economic quality of life, and/or patient satisfaction), or profoundly change practice |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hoffmann-Eubanks, B.; Kondic, A.M.; Isetts, B.J. Alignment of Community Pharmacy Foundation Grant Funding and the Evolution of Pharmacy Practice in the United States of America. Pharmacy 2019, 7, 63. https://doi.org/10.3390/pharmacy7020063
Hoffmann-Eubanks B, Kondic AM, Isetts BJ. Alignment of Community Pharmacy Foundation Grant Funding and the Evolution of Pharmacy Practice in the United States of America. Pharmacy. 2019; 7(2):63. https://doi.org/10.3390/pharmacy7020063
Chicago/Turabian StyleHoffmann-Eubanks, Brittany, Anne Marie Kondic, and Brian J. Isetts. 2019. "Alignment of Community Pharmacy Foundation Grant Funding and the Evolution of Pharmacy Practice in the United States of America" Pharmacy 7, no. 2: 63. https://doi.org/10.3390/pharmacy7020063
APA StyleHoffmann-Eubanks, B., Kondic, A. M., & Isetts, B. J. (2019). Alignment of Community Pharmacy Foundation Grant Funding and the Evolution of Pharmacy Practice in the United States of America. Pharmacy, 7(2), 63. https://doi.org/10.3390/pharmacy7020063





