Patterns of Medication Dispensation for Multiple Comorbidities among Older Adults in Australia
Abstract
1. Background
2. Method
2.1. Study Design and Data Source
2.2. Study Population
2.3. Study Outcomes
2.4. Statistical Analyses
3. Results
3.1. Sample Characteristics
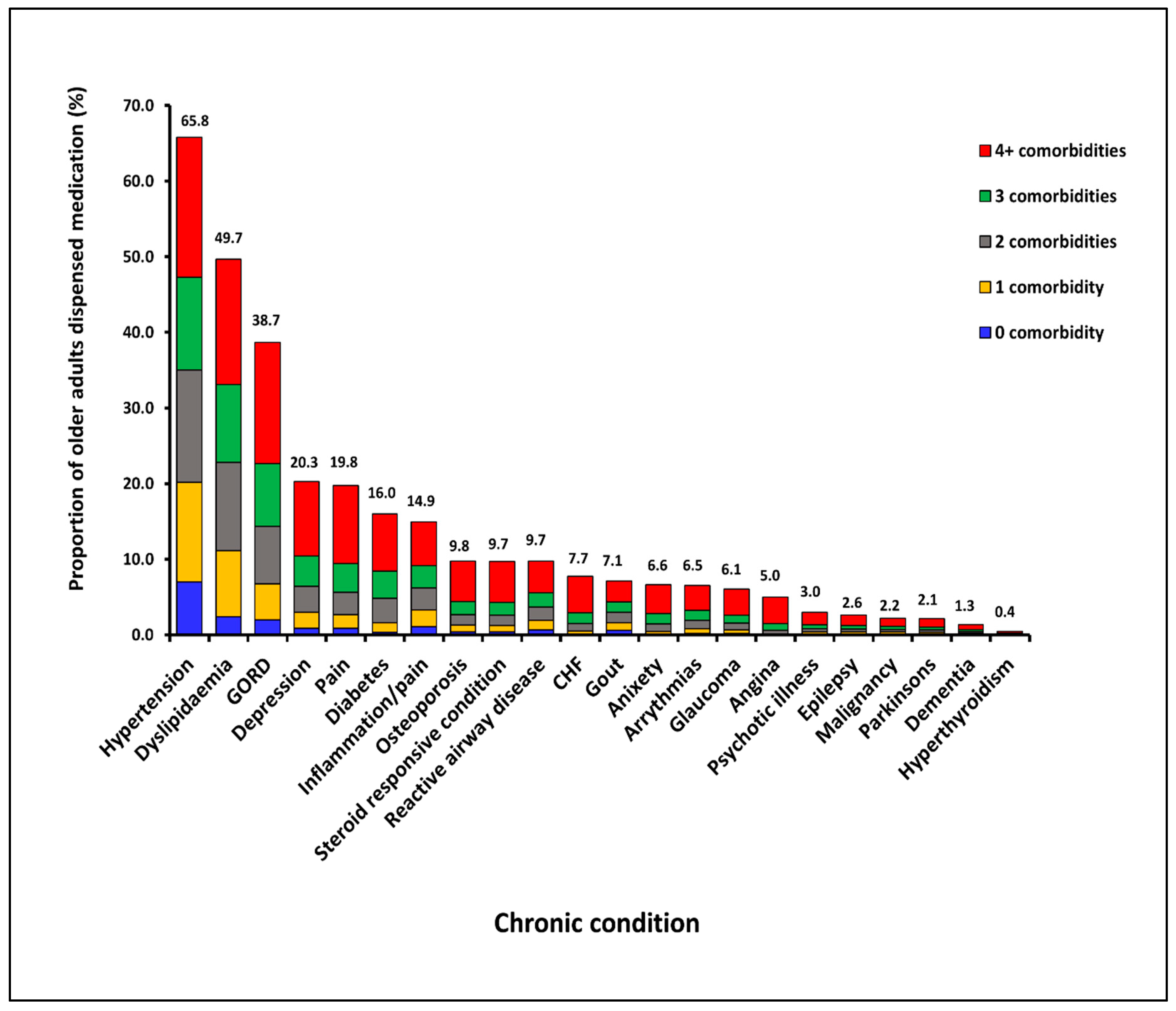
3.2. Patterns of Medication Dispensation for Individual CCs from 2013 to 2016
3.3. Dispensation of Medications for Multiple CCs
3.4. Patterns of Medication Dispensation for Multiple CCs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ofori-Asenso, R.; Zomer, E.; Curtis, A.; Zoungas, S.; Gambhir, M. Measures of Population Ageing in Australia from 1950 to 2050. J. Popul. Ageing 2017, 11, 1–19. [Google Scholar] [CrossRef]
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Meinow, B.; Fratiglioni, L. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 2011, 10, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Ofori-Asenso, R.; Chin, K.L.; Curtis, A.J.; Zomer, E.; Zoungas, S.; Liew, D. Recent Patterns of Multimorbidity Among Older Adults in High-Income Countries. Popul. Health Manag. 2018. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. 4364.0.55.001-National Health Survey: First Results, 2014-15. 2015. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/mf/4364.0.55.001 (accessed on 5 March 2018).
- Australian Bureau of Statistics. 4364.0.55.001-Australian Health Survey: First Results, 2011-12. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/4364.0.55.001main+features12011-12 (accessed on 5 March 2018).
- Kroll, M.; Phalkey, R.K.; Kraas, F. Challenges to the surveillance of non-communicable diseases—A review of selected approaches. BMC Public Health 2015, 15, 1243. [Google Scholar] [CrossRef] [PubMed]
- Australian Commission on Safety and Quality in Health Care. Framework for Australian Clinical Quality Registries; Australian Commission on Safety and Quality in Health Care: Sydney, Australian, 2014.
- Smeets, H.M.; de Wit, N.J.; Hoes, A.W. Routine health insurance data for scientific research: Potential and limitations of the Agis Health Database. J. Clin. Epidemiol. 2011, 64, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Maio, V.; Yuen, E.; Rabinowitz, C.; Louis, D.; Jimbo, M.; Donatini, A.; Mall, S.; Taroni, F. Using pharmacy data to identify those with chronic conditions in Emilia Romagna, Italy. J. Health Serv. Res. Policy 2005, 10, 232–238. [Google Scholar] [CrossRef]
- Huber, C.A.; Szucs, T.D.; Rapold, R.; Reich, O. Identifying patients with chronic conditions using pharmacy data in Switzerland: An updated mapping approach to the classification of medications. BMC Public Health 2013, 13, 1030. [Google Scholar] [CrossRef]
- Zellweger, U.; Bopp, M.; Holzer, B.M.; Djalali, S.; Kaplan, V. Prevalence of chronic medical conditions in Switzerland: Exploring estimates validity by comparing complementary data sources. BMC Public Health 2014, 14, 1157. [Google Scholar] [CrossRef]
- Chini, F.; Pezzotti, P.; Orzella, L.; Borgia, P.; Guasticchi, G. Can we use the pharmacy data to estimate the prevalence of chronic conditions? A comparison of multiple data sources. BMC Public Health 2011, 11, 688. [Google Scholar] [CrossRef]
- Gini, R.; Francesconi, P.; Mazzaglia, G.; Cricelli, I.; Pasqua, A.; Gallina, P.; Brugaletta, S.; Donato, D.; Donatini, A.; Marini, A.; et al. Chronic disease prevalence from Italian administrative databases in the VALORE project: A validation through comparison of population estimates with general practice databases and national survey. BMC Public Health 2013, 13, 15. [Google Scholar] [CrossRef]
- Naughton, C.; Bennett, K.; Feely, J. Prevalence of chronic disease in the elderly based on a national pharmacy claims database. Age Ageing 2006, 35, 633–636. [Google Scholar] [CrossRef] [PubMed]
- Cossman, R.E.; Cossman, J.S.; James, W.L.; Blanchard, T.; Thomas, R.K.; Pol, L.G.; Cosby, A.G.; Mirvis, D.M. Evaluating heart disease presciptions-filled as a proxy for heart disease prevalence rates. J. Health Hum. Serv. Adm. 2008, 30, 503–528. [Google Scholar] [PubMed]
- Cossman, R.E.; Cossman, J.S.; James, W.L.; Blanchard, T.; Thomas, R.; Pol, L.G.; Cosby, A.G. Correlating pharmaceutical data with a national health survey as a proxy for estimating rural population health. Popul. Health Met. 2010, 8, 25. [Google Scholar] [CrossRef] [PubMed]
- Caughey, G.E.; Roughead, E.E.; Shakib, S.; McDermott, R.A.; Vitry, A.I.; Gilbert, A.L. Comorbidity of chronic disease and potential treatment conflicts in older people dispensed antidepressants. Age Ageing 2010, 39, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Caughey, G.E.; Roughead, E.E.; Vitry, A.I.; McDermott, R.A.; Shakib, S.; Gilbert, A.L. Comorbidity in the elderly with diabetes: Identification of areas of potential treatment conflicts. Diabetes Res. Clin. Pract. 2010, 87, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Vitry, A.; Wong, S.A.; Roughead, E.E.; Ramsay, E.; Barratt, J. Validity of medication-based co-morbidity indices in the Australian elderly population. Aust. N. Z. J. Public Health 2009, 33, 126–130. [Google Scholar] [CrossRef] [PubMed]
- van Oostrom, S.H.; Picavet, H.S.J.; van Gelder, B.M.; Lemmens, L.C.; Hoeymans, N.; van Dijk, C.E.; Verheij, R.A.; Schellevis, F.G.; Baan, C.A. Multimorbidity and comorbidity in the Dutch population-data from general practices. BMC Public Health 2012, 12, 715. [Google Scholar] [CrossRef]
- Islam, M.M.; Valderas, J.M.; Yen, L.; Dawda, P.; Jowsey, T.; McRae, I.S. Multimorbidity and Comorbidity of Chronic Diseases among the Senior Australians: Prevalence and Patterns. PLoS ONE 2014, 9, e83783. [Google Scholar] [CrossRef]
- Mellish, L.; Karanges, E.A.; Litchfield, M.J.; Schaffer, A.L.; Blanch, B.; Daniels, B.J.; Segrave, A.; Pearson, S.A. The Australian Pharmaceutical Benefits Scheme data collection: A practical guide for researchers. BMC Res. Notes 2015, 8, 634. [Google Scholar] [CrossRef]
- Willcox, S. Chronic Diseases in Australia: The Case for Changing Course; Australian Health Policy Collaboration Issues paper No. 2014-02; Australian Health Policy Collaboration: Melbourne, Australian, 2014. [Google Scholar]
- Rasekaba, T.M.; Lim, W.K.; Hutchinson, A.F. Effect of a chronic disease management service for patients with diabetes on hospitalisation and acute care costs. Aust. Health Rev. 2012, 36, 205–212. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. Older Australia at a Glance. 2017. Available online: https://www.aihw.gov.au/reports/older-people/older-australia-at-a-glance/contents/health-functioning/causes-of-death (accessed on 5 March 2018).
- Harrison, C.; Henderson, J.; Miller, G.; Britt, H. The prevalence of complex multimorbidity in Australia. Aust. N. Z. J. Public Health 2016, 40, 239–244. [Google Scholar] [CrossRef]
- Pratt, N.L.; Kerr, M.; Barratt, J.D.; Kemp-Casey, A.; Ellett, L.M.K.; Ramsay, E.; Roughead, E.E. The validity of the Rx-Risk Comorbidity Index using medicines mapped to the Anatomical Therapeutic Chemical (ATC) Classification System. BMJ Open 2018, 8, e021122. [Google Scholar] [CrossRef] [PubMed]
- Lalic, S.; Gisev, N.; Simon Bell, J.; Korhonen, M.J.; Ilomaki, J. Predictors of persistent prescription opioid analgesic use among people without cancer in Australia. Br. J. Clin. Pharmacol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Fortin, M.; Stewart, M.; Poitras, M.E.; Almirall, J.; Maddocks, H. A Systematic Review of Prevalence Studies on Multimorbidity: Toward a More Uniform Methodology. Ann. Fam. Med. 2012, 10, 142–151. [Google Scholar] [CrossRef] [PubMed]
- Gnjidic, D.; Le Couteur, D.G.; Hilmer, S.N. Discontinuing drug treatments. Br. Med. J. 2014, 349. [Google Scholar] [CrossRef]
- Loza, E.; Jover, J.A.; Rodriguez-Rodriguez, L.; Carmona, L.; Group, E.S. Observed and expected frequency of comorbid chronic diseases in rheumatic patients. Ann. Rheum. Dis. 2008, 67, 418–421. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Australia’s Health 2016; Australia’s Health Series No. 15. Cat. No. AUS 199; Australian Institute of Health and Welfare: Canberra, Australian, 2016.
- McRae, I.; Yen, L.; Jeon, Y.H.; Herath, P.M.; Essue, B. Multimorbidity is associated with higher out-of-pocket spending: A study of older Australians with multiple chronic conditions. Aust. J. Prim. Health. 2013, 19, b144–b149. [Google Scholar] [CrossRef] [PubMed]
- Britt, H.C.; Harrison, C.M.; Miller, G.C.; Knox, S.A. Prevalence and patterns of multimorbidity in Australia. Med. J. Aust. 2008, 189, 72–77. [Google Scholar] [PubMed]
- Harrison, C.; Henderson, J.; Miller, G.; Britt, H. The prevalence of diagnosed chronic conditions and multimorbidity in Australia: A method for estimating population prevalence from general practice patient encounter data. PLoS ONE 2017, 12, e0172935. [Google Scholar] [CrossRef] [PubMed]
- Harrison, C.; Britt, H.; Miller, G.; Henderson, J. Examining different measures of multimorbidity, using a large prospective cross-sectional study in Australian general practice. BMJ Open 2014, 4, e004694. [Google Scholar] [CrossRef]
- Weycker, D.; Nichols, G.A.; O’Keeffe-Rosetti, M.; Edelsberg, J.; Khan, Z.M.; Kaura, S.; Oster, G. Risk-factor clustering and cardiovascular disease risk in hypertensive patients. Am. J. Hypertens. 2007, 20, 99–607. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Health Expenditure AUSTRALIA 2015–16; Health a Welfare Expenditure Series No. 58. Cat. No. HWE 68; Australian Institute of Health and Welfare: Canberra, Australian, 2017.
- Australian Institute of Health and Welfare. 25 Years of Health Expenditure in Australia 1989–90 to 2013–14; Health and Welfare Expenditure Series No. 56. Cat. No. HWE 66; Australian Institute of Health and Welfare: Canberra, Australian, 2016.
- Moodie, A.R.; Tolhurst, P.; Martin, J.E. Australia’s health: Being accountable for prevention. Med. J. Aust. 2016, 204, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Mangin, D.; Sweeney, K.; Heath, I. Preventive health care in elderly people needs rethinking. Br. Med. J. 2007, 335, 285–287. [Google Scholar] [CrossRef] [PubMed]
- Salive, M.E. Multimorbidity in older adults. Epidemiol. Rev. 2013, 35, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. Dementia in Australia; Cat. no. AGE 70; Australian Institute of Health and Welfare: Canberra, Australian, 2012.
- Rice, D.P.; Fillit, H.M.; Max, W.; Knopman, D.S.; Lloyd, J.R.; Duttagupta, S. Prevalence, costs, and treatment of Alzheimer’s disease and related dementia: A managed care perspective. Am. J. Manag. Care 2001, 7, 809–818. [Google Scholar] [PubMed]
| Year | Total No. of Persons | Mean Age (S.D), Years | Gender Distribution | |||||
|---|---|---|---|---|---|---|---|---|
| Men (n, %) | Women (n, %) | |||||||
| 65–74 | 75–84 | ≥85 | 65–74 | 75–84 | ≥85 | |||
| 2013 | 315,074 | 72.7 (7.5) | 84,356 (26.8) | 46,514 (14.8) | 13,877 (4.4) | 89,572 (28.4) | 55,104 (17.5) | 25,651 (8.1) |
| 2014 | 327,433 | 73.7 (7.5) | 87,557 (26.7) | 47,982 (14.7) | 15,342 (4.7) | 93,467 (28.5) | 56,286 (17.2) | 26,799 (8.2) |
| 2015 | 340,153 | 73.8 (7.5) | 91,060 (26.8) | 49,584 (14.6) | 16,586 (4.9) | 97,434 (28.6) | 57,510 (16.9) | 27,979 (8.2) |
| 2016 | 351,471 | 73.8 (7.5) | 93,880 (26.7) | 51,193 (14.6) | 17,640 (5.0) | 100,808 (28.7) | 59,188 (16.8) | 28,762 (8.2) |
| Chronic Condition | 2013 | 2014 | 2015 | 2016 |
|---|---|---|---|---|
| Hypertension | 66.5 | 66.2 | 65.8 | 65.7 |
| Dyslipidaemia | 50.9 | 50.3 | 50.0 | 50.0 |
| GORD | 41.0 | 41.4 | 41.3 | 41.4 |
| Pain | 25.7 | 26.5 | 26.9 | 26.6 |
| Depression | 21.4 | 21.4 | 21.6 | 21.8 |
| Inflammation/pain | 20.8 | 20.5 | 20.2 | 20.1 |
| Diabetes | 15.7 | 15.9 | 16.1 | 16.3 |
| Steroid responsive conditions | 12.3 | 12.7 | 13.1 | 13.3 |
| Reactive airway disease | 11.9 | 12.1 | 12.1 | 12.0 |
| Osteoporosis | 10.5 | 10.4 | 10.5 | 10.8 |
| CHF | 9.0 | 8.9 | 8.8 | 8.8 |
| Anxiety | 8.7 | 8.4 | 8.0 | 7.9 |
| Glaucoma | 7.6 | 7.5 | 7.4 | 7.3 |
| Gout | 7.4 | 7.4 | 7.5 | 7.5 |
| Angina | 7.3 | 6.9 | 6.5 | 6.3 |
| Arrythmias | 6.6 | 6.6 | 6.8 | 7.1 |
| Psychotic illness | 3.7 | 3.6 | 3.6 | 3.5 |
| Epilepsy | 3.1 | 3.0 | 3.0 | 2.9 |
| Malignancy | 2.3 | 2.4 | 2.5 | 2.6 |
| Parkinson’s disease | 2.2 | 2.3 | 2.3 | 2.3 |
| Dementia | 1.3 | 1.4 | 1.4 | 1.5 |
| Hyperthyroidism | 0.5 | 0.5 | 0.5 | 0.5 |
| No. of CCs | Percentage of Older Adults Dispensed Medications for No. of CCs in Respective Years | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2013 | 2014 | 2015 | 2016 | |||||||||||||||||||||
| All | M | W | 65–74 | 75–84 | 85+ | All | M | W | 65–74 | 75–84 | 85+ | All | M | W | 65–74 | 75–84 | 85+ | All | M | W | 65–74 | 75–84 | 85+ | |
| 0 | 5.7 | 5.9 | 5.6 | 7.6 | 3.4 | 3.3 | 5.8 | 6.0 | 5.7 | 7.8 | 3.5 | 3.2 | 5.9 | 5.9 | 5.8 | 7.9 | 3.4 | 3.1 | 5.8 | 5.9 | 5.7 | 7.8 | 3.4 | 3.2 |
| 1 | 14.6 | 15.2 | 14.0 | 17.9 | 10.7 | 9.6 | 14.7 | 15.3 | 14.2 | 18.1 | 10.8 | 9.3 | 14.7 | 15.2 | 14.3 | 18.1 | 11.0 | 9.3 | 14.7 | 15.2 | 14.2 | 18.1 | 10.9 | 9.3 |
| 2 | 18.5 | 19.1 | 18.0 | 20.5 | 16.5 | 14.8 | 18.2 | 18.9 | 17.7 | 20.2 | 16.3 | 14.4 | 18.2 | 18.7 | 17.8 | 20.2 | 16.4 | 14.3 | 18.3 | 18.8 | 17.7 | 20.2 | 16.4 | 14.4 |
| 3 | 18.6 | 19.0 | 18.2 | 18.8 | 18.6 | 17.7 | 18.5 | 18.9 | 18.2 | 18.6 | 18.7 | 17.8 | 18.5 | 18.9 | 18.1 | 18.4 | 18.8 | 17.8 | 18.5 | 19.0 | 18.2 | 18.6 | 18.8 | 17.9 |
| 4 | 15.5 | 15.4 | 15.6 | 14.1 | 17.2 | 17.4 | 15.5 | 15.5 | 15.6 | 14.1 | 17.0 | 17.8 | 15.5 | 15.5 | 15.5 | 14.1 | 17.0 | 17.7 | 15.5 | 15.5 | 15.6 | 14.1 | 17.1 | 17.7 |
| 5 | 11.3 | 10.8 | 11.7 | 9.4 | 13.3 | 14.4 | 11.3 | 10.9 | 11.8 | 9.5 | 13.3 | 14.4 | 11.4 | 11.0 | 11.7 | 9.5 | 13.2 | 14.8 | 11.4 | 11.0 | 11.7 | 9.5 | 13.3 | 14.6 |
| 6 | 7.4 | 6.9 | 7.8 | 5.7 | 9.2 | 10.4 | 7.4 | 7.0 | 7.8 | 5.6 | 9.3 | 10.5 | 7.4 | 7.0 | 7.8 | 5.8 | 9.2 | 10.2 | 7.4 | 7.0 | 7.8 | 5.7 | 9.2 | 10.4 |
| 7 | 4.4 | 4.0 | 4.7 | 3.2 | 5.5 | 6.4 | 4.4 | 4.0 | 4.7 | 3.2 | 5.6 | 6.6 | 4.4 | 4.0 | 4.7 | 3.2 | 5.6 | 6.7 | 4.4 | 4.0 | 4.7 | 3.2 | 5.6 | 6.5 |
| 8 | 2.3 | 2.1 | 2.5 | 1.6 | 3.1 | 3.5 | 2.3 | 2.0 | 2.5 | 1.6 | 3.0 | 3.4 | 2.3 | 2.1 | 2.5 | 1.6 | 3.0 | 3.5 | 2.3 | 2.1 | 2.5 | 1.6 | 3.0 | 3.4 |
| 9 | 1.1 | 1.0 | 1.2 | 0.7 | 1.6 | 1.6 | 1.1 | 1.0 | 1.2 | 0.8 | 1.5 | 1.5 | 1.1 | 1.0 | 1.2 | 0.8 | 1.4 | 1.7 | 1.1 | 1.0 | 1.2 | 0.8 | 1.5 | 1.6 |
| ≥10 | 0.7 | 0.7 | 0.7 | 0.5 | 1.0 | 1.0 | 0.7 | 0.7 | 0.7 | 0.5 | 1.0 | 1.0 | 0.7 | 0.7 | 0.7 | 0.5 | 1.0 | 0.9 | 0.7 | 0.7 | 0.7 | 0.5 | 1.0 | 1.0 |
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 5.8 | 5.9 | 5.7 | 7.8 | 3.4 | 3.2 |
| Mean no. of CCs (S.D) | 3.4 (2.1) | 3.3 (2.1) | 3.4 (2.1) | 3.0 (2.0) | 3.8 (2.1) | 3.9 (2.2) | 3.4 (2.1) | 3.3 (2.1) | 3.4 (2.1) | 3.0 (2.0) | 3.8 (2.1) | 4.0 (2.1) | 3.4 (2.1) | 3.3 (2.1) | 3.4 (2.1) | 3.0 (2.0) | 3.8 (2.1) | 4.0 (2.1) | 3.4 (2.1) | 3.3 (2.1) | 3.0 (2.0) | 3.1 (2.1) | 3.8 (2.1) | 4.0 (2.1) |
| % ≥2 CC | 79.8 | 79.0 | 80.4 | 74.5 | 85.9 | 87.1 | 79.5 | 78.8 | 80.1 | 74.1 | 85.7 | 87.4 | 79.4 | 78.9 | 79.9 | 74.0 | 85.6 | 87.6 | 79.5 | 78.9 | 80.1 | 74.1 | 85.7 | 87.6 |
| Ranking * | CC Dyad | Prevalence (%) | O/E Ratio | p-Value † | |
|---|---|---|---|---|---|
| Expected (E) | Observed (O) | ||||
| 1. | Dyslipidaemia + hypertension | 29.8 | 36.0 | 1.21 | <0.001 |
| 2. | Gastric acid disorder + hypertension | 24.7 | 27.1 | 1.10 | <0.001 |
| 3. | Dyslipidaemia + gastric acid disorder | 20.8 | 23.9 | 1.15 | <0.001 |
| 4. | Pain + hypertension | 15.9 | 16.7 | 1.05 | <0.001 |
| 5. | Gastric acid disorder + pain | 11.0 | 14.8 | 1.35 | <0.001 |
| 6. | Dyslipidaemia + pain | 13.3 | 13.8 | 1.04 | <0.001 |
| 7. | Depression + hypertension | 12.9 | 13.5 | 1.05 | <0.001 |
| 8. | Diabetes + dyslipidaemia | 8.2 | 12.8 | 1.56 | <0.001 |
| 9. | Diabetes + hypertension | 9.7 | 12.5 | 1.29 | <0.001 |
| 10. | Depression + gastric acid disorder | 9.0 | 12.4 | 1.38 | <0.001 |
| 11. | Depression + dyslipidaemia | 10.9 | 11.9 | 1.09 | <0.001 |
| 12. | Inflammatory disorder + hypertension | 12.0 | 11.5 | 0.96 | <0.001 |
| 13. | Dyslipidaemia + Inflammation/pain | 10.1 | 9.9 | 0.98 | 0.0059 |
| 14. | Gastric acid disorder + inflammation/pain | 8.3 | 9.9 | 1.19 | <0.001 |
| 15. | Depression + pain | 5.8 | 8.9 | 1.53 | <0.001 |
| Ranking * | CC Triad | Prevalence (%) | O/E Ratio | p-Value † | |
|---|---|---|---|---|---|
| Expected (E) | Observed (O) | ||||
| 1. | Dyslipidaemia + GORD + hypertension | 12.7 | 18.7 | 1.47 | <0.001 |
| 2. | Diabetes + dyslipidaemia + hypertension | 5.2 | 10.8 | 2.08 | <0.001 |
| 3. | Dyslipidaemia + pain + hypertension | 6.5 | 10.8 | 1.66 | <0.001 |
| 4. | GORD + pain + hypertension | 5.0 | 10.6 | 2.12 | <0.001 |
| 5. | Dyslipidaemia + GORD + pain | 3.8 | 9.1 | 2.39 | <0.001 |
| 6. | Depression + dyslipidaemia + hypertension | 6.6 | 9.0 | 1.36 | <0.001 |
| 7. | Depression + GORD + hypertension | 5.2 | 8.7 | 1.67 | <0.001 |
| 8. | Depression + dyslipidaemia + GORD | 3.9 | 7.8 | 2.00 | <0.001 |
| 9. | Dyslipidaemia + inflammation + hypertension | 4.9 | 7.3 | 1.49 | <0.001 |
| 10. | Diabetes + dyslipidaemia + GORD | 3.1 | 6.7 | 2.16 | <0.001 |
| 11. | GORD + inflammation + hypertension | 3.8 | 6.6 | 1.74 | <0.001 |
| 12. | Diabetes + GORD + hypertension | 4.1 | 6.5 | 1.59 | <0.001 |
| 13. | Depression + GORD + pain | 1.6 | 6.3 | 3.94 | <0.001 |
| 14. | Depression + pain + hypertension | 2.6 | 6.1 | 2.35 | <0.001 |
| 15. | Dyslipidaemia + GORD + inflammation/pain | 2.9 | 5.9 | 2.03 | <0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ofori-Asenso, R.; Ilomaki, J.; Curtis, A.J.; Zomer, E.; Zoungas, S.; Liew, D. Patterns of Medication Dispensation for Multiple Comorbidities among Older Adults in Australia. Pharmacy 2018, 6, 134. https://doi.org/10.3390/pharmacy6040134
Ofori-Asenso R, Ilomaki J, Curtis AJ, Zomer E, Zoungas S, Liew D. Patterns of Medication Dispensation for Multiple Comorbidities among Older Adults in Australia. Pharmacy. 2018; 6(4):134. https://doi.org/10.3390/pharmacy6040134
Chicago/Turabian StyleOfori-Asenso, Richard, Jenni Ilomaki, Andrea J. Curtis, Ella Zomer, Sophia Zoungas, and Danny Liew. 2018. "Patterns of Medication Dispensation for Multiple Comorbidities among Older Adults in Australia" Pharmacy 6, no. 4: 134. https://doi.org/10.3390/pharmacy6040134
APA StyleOfori-Asenso, R., Ilomaki, J., Curtis, A. J., Zomer, E., Zoungas, S., & Liew, D. (2018). Patterns of Medication Dispensation for Multiple Comorbidities among Older Adults in Australia. Pharmacy, 6(4), 134. https://doi.org/10.3390/pharmacy6040134




