Development of a Theory-Based Intervention to Enhance Information Exchange during Over-The-Counter Consultations in Community Pharmacy
Abstract
1. Introduction
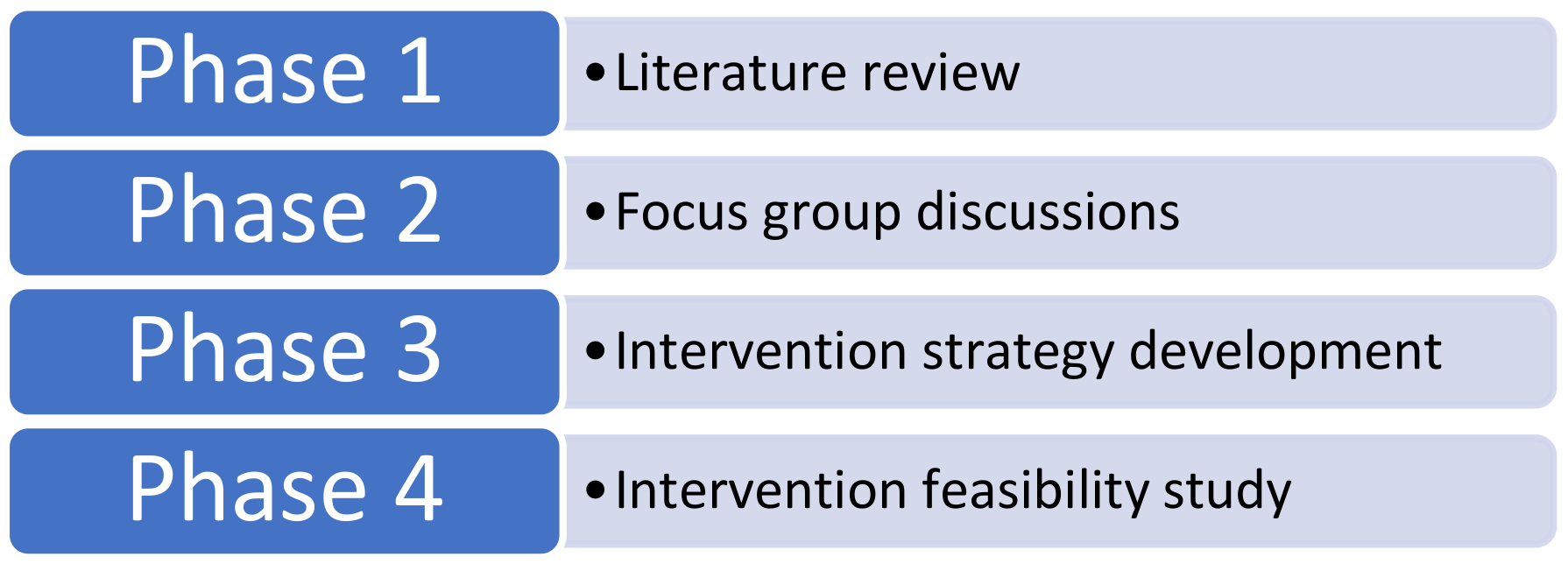
2. Materials and Methods
Underpinning Theory
3. Results
3.1. Stage 1: Behavioural Analysis
3.2. Stage 2: Identify Intervention Options, Content and Implementation Options
3.3. Intervention Strategy
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Collins, J.C.; Schneider, C.R.; Faraj, R.; Wilson, F.; De Almeida Neto, A.C.; Moles, R.J. Management of common ailments requiring referral in the pharmacy: A mystery shopping intervention study. Int. J. Clin. Pharm. 2017, 39, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Blenkinsopp, A.; Paxton, P.; Blenkinsopp, J. Symptoms in the Pharmacy: A Guide to the Management of Common Illness, 6th ed.; Blackwell Publishing Ltd.: Oxford, UK, 2009; ISBN 978-1-118-59844-3. [Google Scholar]
- Boardman, H.; Lewis, M.; Croft, P.; Trinder, P.; Rajaratnam, G. Use of community pharmacies: A population-based survey. J. Public Health 2005, 27, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Benrimoj, S.I.; Frommer, M.S. Community pharmacy in Australia. Aust. Health Rev. 2004, 28, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Hibbert, D.; Bissell, P.; Ward, P.R. Consumerism and professional work in the community pharmacy. Sociol. Health Illn. 2002, 24, 46–65. [Google Scholar] [CrossRef]
- Hughes, C.M.; McElnay, J.C.; Fleming, G.F. Benefits and risks of self medication. Drug Saf. 2001, 24, 1027–1037. [Google Scholar] [CrossRef] [PubMed]
- Therapeutic Goods Administration Reasons for Scheduling Delegate’s Final Decisions, June 2017. Available online: https://www.tga.gov.au/scheduling-decision-final/scheduling-delegates-final-decisions-june-2017 (accessed on 29 August 2017).
- Association of the European Self-Medication Industry. Available online: http://www.aesgp.eu/facts-figures/otc-ingredients/#undefined (accessed on 24 October 2017).
- US Food and Drug Administration. What Are Over-the-Counter (OTC) Drugs and How Are They Approved? Available online: https://www.fda.gov/aboutfda/transparency/basics/ucm194951.htm (accessed on 23 October 2017).
- Khdour, M.R.; Hallak, H.O. Societal perspectives on community pharmacy services in West Bank—Palestine. Pharm Pract. 2012, 10, 17–24. [Google Scholar] [CrossRef]
- Todd, A.; Copeland, A.; Husband, A.; Kasim, A.; Bambra, C. Access all areas? An area-level analysis of accessibility to general practice and community pharmacy services in England by urbanity and social deprivation. BMJ Open 2015, 5. [Google Scholar] [CrossRef] [PubMed]
- Paola, S. “Convenience and Accessibility” An Evaluation of the First Pharmacist-Administered Vaccinations in WA Has Shown Positive Results for Patient and Practitioner. Available online: https://ajp.com.au/news/providing-convenience-accessibility/ (accessed on 24 October 2018).
- Lam, B. How to Increase the Accessibility of Pharmacists When the Pharmacy Is Open. Available online: http://www.pharmaceutical-journal.com/news-and-analysis/event/how-to-increase-the-accessibility-of-pharmacists-when-the-pharmacy-is-open/20066487.article (accessed on 8 December 2017).
- Bennadi, D. Self-medication: A current challenge. J. Basic Clin. Pharm. 2014, 5, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Fielding, S.; Slovic, P.; Johnston, M.; Lee Amanda, J.; Bond Christine, M.; Watson Margaret, C. Public risk perception of non-prescription medicines and information disclosure during consultations: A suitable target for intervention? Int. J. Pharm. Pract. 2018. [Google Scholar] [CrossRef] [PubMed]
- Roumie, C.; Griffin, M.R. Over-the-counter analgesics in older adults—A call for improved labelling and consumer education. Drugs Aging 2004, 21, 485–498. [Google Scholar] [CrossRef] [PubMed]
- Calamusa, A.; Di Marzio, A.; Cristofani, R.; Arrighetti, P.; Santaniello, V.; Alfani, S.; Carducci, A. Factors that influence Italian consumers’ understanding of over-the-counter medicines and risk perception. Patient Educ. Couns. 2012, 87, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Stosic, R.; Dunagan, F.; Palmer, H.; Fowler, T.; Adams, I. Responsible self-medication: Perceived risks and benefits of over-the-counter analgesic use. Int. J. Pharm. Pract. 2011, 19, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Mullan, J.; Weston Kathryn, M.; Bonney, A.; Burns, P.; Mullan, J.; Rudd, R. Consumer knowledge about over-the-counter NSAIDs: They don’t know what they don’t know. Aust. N. Z. J. Public Health 2017, 41, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Pharmaceutical Society of Australia. Professional Practice Standards—Version 5—2017; Pharmaceutical Society of Australia: Deakin West, Australia, 2017; ISBN 978-0-908185-05-4. [Google Scholar]
- Pharmaceutical Society of Australia. National Competency Standards Framework for Pharmacists in Australia 2016; Pharmaceutical Society of Australia: Deakin West, Australia, 2016; ISBN 978-0-908185-03-0. [Google Scholar]
- Bell, J.; Dziekan, G.; Pollack, C.; Mahachai, V. Self-Care in the twenty first century: A vital role for the pharmacist. Adv. Ther. 2016, 33, 1691–1703. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. The Role of the Pharmacist in Self-Care and Self-Medication. 4th WHO Consultative Group on the Role of the Pharmacist, Ed. 1998. Available online: http://apps.who.int/medicinedocs/en/d/Jwhozip32e/#Jwhozip32e (accessed on 14 September 2017).
- Watson, M.C.; Johnston, M.; Entwistle, V.; Lee, A.J.; Bond, C.M.; Fielding, S. Using the theory of planned behaviour to develop targets for interventions to enhance patient communication during pharmacy consultations for non-prescription medicines. Int. J. Pharm. Pract. 2014, 22, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.C.; Cleland, J.A.; Bond, C.M. Simulated patient visits with immediate feedback to improve the supply of over-the-counter medicines: A feasibility study. Fam. Pract. 2009, 26, 532–542. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.; Bond, C.; Grimshaw, J.; Johnston, M. Factors predicting the guideline compliant supply (or non-supply) of non-prescription medicines in the community pharmacy setting. Qual. Saf. Health Care 2006, 15, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Berger, K.; Eickhoff, C.; Schulz, M. Counselling quality in community pharmacies: Implementation of the pseudo customer methodology in Germany. J. Clin. Pharm. Ther. 2005, 30, 45–57. [Google Scholar] [CrossRef] [PubMed]
- Rutter, P.M.; Horsley, E.; Brown, D.T. Evaluation of community pharmacists’ recommendations to standardized patient scenarios. Ann. Pharmacother. 2004, 38, 1080–1085. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.C.; Hart, J.; Johnston, M.; Bond, C.M. Exploring the supply of non-prescription medicines from community pharmacies in Scotland. Pharm. World Sci. 2008, 30, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, H.S.; Schaefer, M. Evaluation of the impact of pharmacist’s advice giving on the outcomes of self-medication in patients suffering from dyspepsia. Pharm. World Sci. 2000, 22, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.R.; Everett, A.W.; Geelhoed, E.; Kendall, P.A.; Murray, K.; Garnett, P.; Salama, M.; Clifford, R.M. Provision of primary care to patients with chronic cough in the community pharmacy setting. Ann. Pharmacother. 2011, 45, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.R.; Everett, A.W.; Geelhoed, E.; Padgett, C.; Ripley, S.; Murray, K.; Kendall, P.A.; Clifford, R.M. Intern pharmacists as change agents to improve the practice of nonprescription medication supply: Provision of salbutamol to patients with asthma. Ann. Pharmacother. 2010, 44, 1319–1326. [Google Scholar] [CrossRef] [PubMed]
- Queddeng, K.; Chaar, B.; Williams, K. Emergency contraception in Australian community pharmacies: A simulated patient study. Contraception 2011, 83, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Kippist, C.; Wong, K.; Bartlett, D.; Bandana, S. How do pharmacists respond to complaints of acute insomnia? A simulated patient study. Int. J. Clin. Pharm. 2011, 33, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Kelly, F.S.; Williams, K.A.; Benrimoj, S.I. Does advice from pharmacy staff vary according to the nonprescription medicine requested? Ann. Pharmacother. 2009, 43, 1877–1886. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.C.; Bond, C.M.; Grimshaw, J.M.; Mollison, J.; Ludbrook, A.; Walker, A.E. Educational strategies to promote evidence-based community pharmacy practice: A cluster randomized controlled trial. Fam. Pract. 2002, 19, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.C.; Bond, C.M. The evidence-based supply of non-prescription medicines: Barriers and beliefs. Int. J. Pharm. Pract. 2004, 12, 65–72. [Google Scholar] [CrossRef]
- Kaae, S.; Saleem, S.; Kristiansen, M. How do Danish community pharmacies vary in engaging customers in medicine dialogues at the counter—An observational study. Pharm Pract. (Granada) 2014, 12, 422. [Google Scholar] [CrossRef] [PubMed]
- Seubert, L.J.; Whitelaw, K.; Boeni, F.; Hattingh, L.; Watson, M.C.; Clifford, R.M. Barriers and facilitators for information exchange during over-the-counter consultations in community pharmacy: A focus group study. Pharmacy 2017, 5, 65. [Google Scholar] [CrossRef] [PubMed]
- Hanna, L.-A.; Hughes, C. ‘First, do no harm’: Factors that influence pharmacists making decisions about over-the-counter medication. Drug Saf. 2010, 33, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Watson, M.C.; Bond, C.M.; Johnston, M.; Mearns, K. Using human error theory to explore the supply of nonprescription medicines from community pharmacies. Qual. Saf. Health Care 2006, 15, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.R.; Everett, A.W.; Geelhoed, E.; Kendall, P.A.; Clifford, R.M. Measuring the assessment and counselling provided with the supply of non-prescription asthma reliever medication: A simulated patient study. Ann. Pharmacother. 2009, 43, 1512–1518. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.R.; Emery, L.; Brostek, R.; Clifford, R.M. Evaluation of the supply of antifungal medication for the treatment of vaginal thrush in the community pharmacy setting: A randomized controlled trial. Pharm. Pract. (Granada) 2013, 11, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Benrimoj, S.I.; Werner, J.B.; Raffaele, C.; Roberts, A.S.; Costa, F.A. Monitoring quality standards in the provision of non-prescription medicines from Australian Community Pharmacies: Results of a national programme. Qual. Saf. Health Care 2007, 16, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.R.; Gudka, S.; Fleischer, L.; Clifford, R.M. The use of a written assessment checklist for the provision of emergency contraception via community pharmacies: A simulated patient study. Pharm. Pract. 2013, 11, 127–131. [Google Scholar] [CrossRef]
- Watson, M.C.; Cleland, J.; Inch, J.; Bond, C.M.; Francis, J. Theory-based communication skills training for medicine counter assistants to improve consultations for non-prescription medicines. Med. Educ. 2007, 41, 450–459. [Google Scholar] [CrossRef] [PubMed]
- Seubert, L.J.; Whitelaw, K.; Hattingh, L.; Watson, M.C.; Clifford, R.M. Interventions to enhance effective communication during over-the-counter consultations in the community pharmacy setting: A systematic review. Res. Soc. Adm. Pharm. 2017. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Atkins, L.; West, R. The Behaviour Change Wheel. A Guide to Designing Interventions, 1st ed.; Silverback Publishing: Great Britain, UK, 2014; ISBN 978-1-291-84605-8. [Google Scholar]
- Atkins, L.; Francis, J.; Islam, R.; O’Connor, D.; Patey, A.; Ivers, N.; Foy, R.; Duncan, E.M.; Colquhoun, H.; Grimshaw, J.M.; et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement. Sci. 2017, 12, 77. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Johnston, M. Behavior Change Techniques. In Encyclopedia of Behavioral Medicine; Gellman, M.D., Turner, J.R., Eds.; Springer: New York, NY, USA, 2013; pp. 182–187. ISBN 978-1-4419-1005-9. [Google Scholar]
- Michie, S.; van Stralen, M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6. [Google Scholar] [CrossRef] [PubMed]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7. [Google Scholar] [CrossRef] [PubMed]
| COM-B Source Behaviour | TDF Domain |
|---|---|
| CAPABILITY | Skills (Cognitive and interpersonal; Physical) |
| Knowledge | |
| Memory, attention and decision processes | |
| Behavioural regulation | |
| OPPORTUNITY | Social influences |
| Environmental context and resources | |
| MOTIVATION | Social and professional role and identity |
| Belief about capabilities | |
| Optimism | |
| Belief about consequences | |
| Intentions | |
| Goals | |
| Reinforcement | |
| Emotion |
| Target Behaviour: Consumer Engaging in Information Exchange. | |||
|---|---|---|---|
| COM-B and TDF * | Barrier | Is There a Need for Change? | Intervention Function |
| PSYCHOLOGICAL CAPABILITY | |||
| Knowledge (An awareness of the existence of something) [52] | Consumers did not understand the role and responsibilities of pharmacists. | √ | Education |
| Consumers did not understand the qualifications of pharmacists. | √ | ||
| Consumers did not understand the risks of medicine use. | √ Consumers do not perceive risks with OTC medicines. Consumers believe medicines available without prescription are safe. | ||
| Cognitive and interpersonal skills (An ability or proficiency acquired through practice) [52] | Pharmacy personnel consultation & communication skills | Improving these skills may improve interactions. | Training |
| PHYSICAL OPPORTUNITY | |||
| Environmental context and resources (Any circumstance of a person’s situation or environment that discourages or encourages the development of skills and abilities, independence, social competence, and adaptive behaviour) [52] | Privacy is required for conversations. | √ Discussing health can be a sensitive issue. | Training Restriction Environmental restructuring Enablement |
| Pharmacy personnel should have time to engage in interactions | √ | ||
| Pharmacists were not always identifiable | √ | ||
| Appropriate remuneration for pharmacist consultations is required | √ | ||
| The environment should look like a professional/healthcare setting | Potentially yes. Some community pharmacies are very retail/warehouse/discount oriented. | ||
| The OTC consultation area is not always clearly identifiable | √ | ||
| REFLECTIVE MOTIVATION | |||
| Social and professional role and identity (A coherent set of behaviours and displayed personal qualities of an individual in a social or work setting) [52] | Consumers did not trust the person asking questions | √ Consumers do not know the role of the pharmacist | Education Persuasion Modelling |
| Service between pharmacies and personnel is not consistent so consumers did not know what to expect | √ | ||
| Belief about capabilities (Acceptance of the truth, reality, or validity about an ability, talent, or facility that a person can put to constructive use) [52] | Consumers believed they are able to appropriately self-asses their condition before consultation | √ | Education Persuasion Modelling Enablement |
| Consumers did not believe pharmacy personnel were able to help with OTC enquiries | √ | ||
| Belief about consequences (Acceptance of the truth, reality, or validity regarding outcomes of a behaviour in a given situation) [52] | Consumers did not understand the risks of medicine use | √ Consumers engage in information exchange if they ask about a symptom but not if they ask for a specific product | Education Persuasion Modelling |
| Consumers did not know that being asked questions is for their benefit | √ | ||
| Consumers did not know that their consultation information will be kept confidential | √ Consumers do not know that pharmacy personnel are bound by privacy laws | ||
| Intentions (A conscious decision to perform a behaviour or a resolve to act in a certain way) [52] | Consumers expected to purchase an OTC product without exchanging information | √ | Education Persuasion Incentivisation Coercion Modelling |
| Consumers expected to answer questions if asking about a symptom | √ | ||
| Consumers resisted information exchange if repeatedly requesting the same product | √ | ||
| AUTOMATIC MOTIVATION | |||
| Reinforcement (Increasing the probability of a response by arranging a dependent relationship, or contingency, between the response and a given stimulus) [52] | Consumers did not feel it necessary to be asked questions (not from focus group but an observation of the research group) | √ If consumers exchange information and have a positive outcome as a result, this will subconsciously encourage information exchange behaviours in future consultations. | Training Incentivisation Coercion Environmental restructuring |
| Behavioural diagnosis of the relevant COM-B components | Psychological capability, physical opportunity, reflective and automatic motivation need to change in order for the target behaviour “consumer engaging in information exchange” to occur. | ||
| Intervention Function | BCTs Identified to Enable Delivery of the Intervention Function | BCT Examples |
|---|---|---|
| Education |
| Explain the role and responsibilities of the pharmacist. Explain the qualifications of the pharmacist. Explain the risks of OTC medicine use. Explain the confidentiality of personal information. |
| Persuasion |
| Inform consumers about positive health consequences from information exchange. |
| Environmental restructuring |
| Pharmacy personnel to wear badges identifying their role. Provide cues/prompts for engaging in information exchange. |
| Modelling |
| Demonstrate the type of questions that might be asked. |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seubert, L.J.; Whitelaw, K.; Hattingh, L.; Watson, M.C.; Clifford, R.M. Development of a Theory-Based Intervention to Enhance Information Exchange during Over-The-Counter Consultations in Community Pharmacy. Pharmacy 2018, 6, 117. https://doi.org/10.3390/pharmacy6040117
Seubert LJ, Whitelaw K, Hattingh L, Watson MC, Clifford RM. Development of a Theory-Based Intervention to Enhance Information Exchange during Over-The-Counter Consultations in Community Pharmacy. Pharmacy. 2018; 6(4):117. https://doi.org/10.3390/pharmacy6040117
Chicago/Turabian StyleSeubert, Liza J., Kerry Whitelaw, Laetitia Hattingh, Margaret C. Watson, and Rhonda M. Clifford. 2018. "Development of a Theory-Based Intervention to Enhance Information Exchange during Over-The-Counter Consultations in Community Pharmacy" Pharmacy 6, no. 4: 117. https://doi.org/10.3390/pharmacy6040117
APA StyleSeubert, L. J., Whitelaw, K., Hattingh, L., Watson, M. C., & Clifford, R. M. (2018). Development of a Theory-Based Intervention to Enhance Information Exchange during Over-The-Counter Consultations in Community Pharmacy. Pharmacy, 6(4), 117. https://doi.org/10.3390/pharmacy6040117






