Using Theory to Explore the Determinants of Medication Adherence; Moving Away from a One-Size-Fits-All Approach
Abstract
1. Introduction
2. Medication Adherence: Current Understanding and Interventions
3. Medication Adherence from a Theoretical Perspective: Identifying Barriers to Change
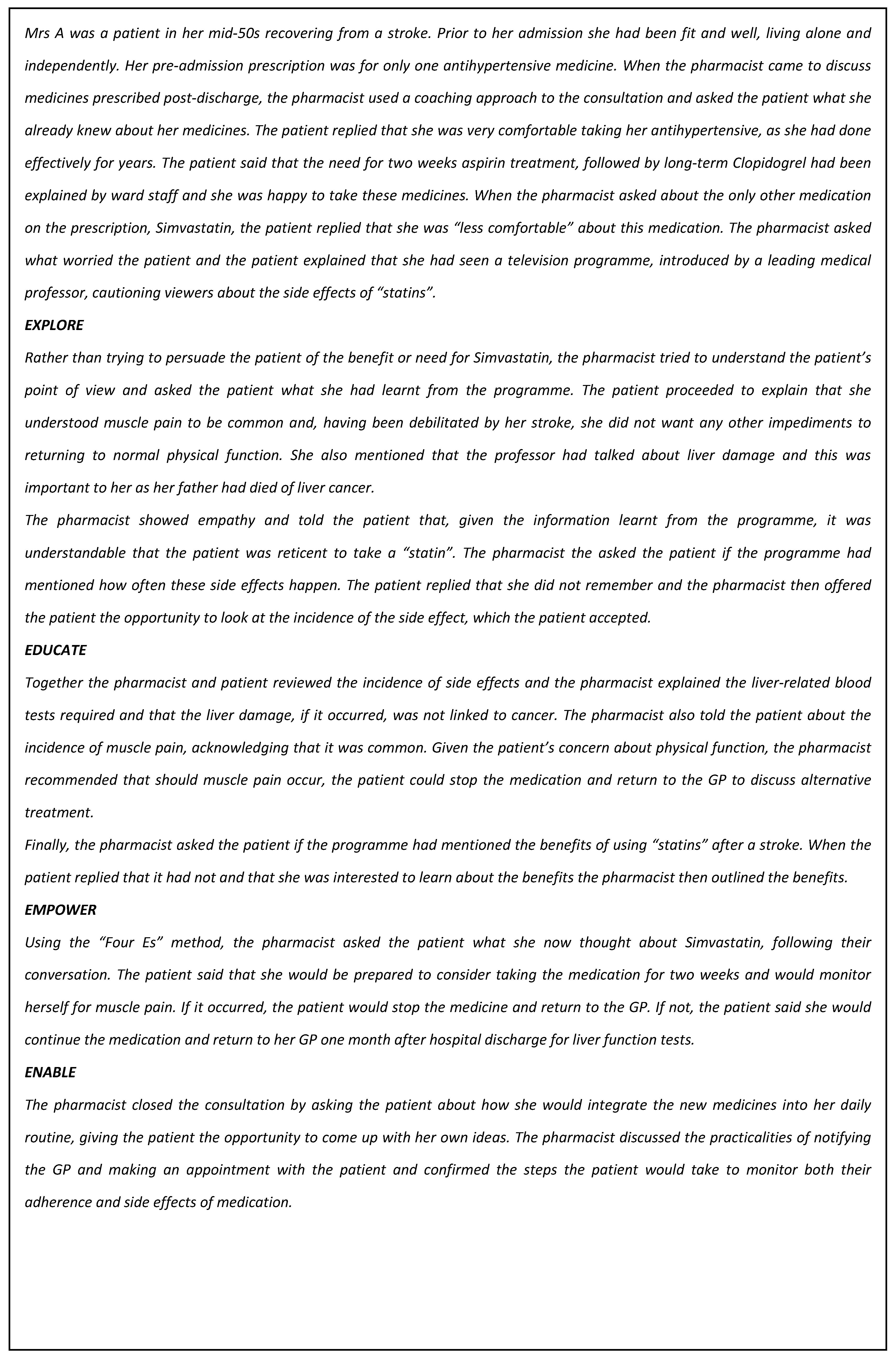
4. Using Health Coaching to Support Adherence through Person-Centred Care: Examples from Practice
5. Conclusions
Acknowledgements
Conflicts of Interest
References
- World Health Organization. Adherence to Long Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Horne, R.; Weinman, J.; Barber, N.; Elliott, R.; Morgan, M.; Cribb, A.; Kellar, I. Concordance, Adherence and Compliance in Medicine Taking; NCCSDO: London, UK, 2005. [Google Scholar]
- Simpson, S.H.; Eurich, D.T.; Majumdar, S.R.; Padwal, R.S.; Tsuyuki, R.T.; Varney, J.; Johnson, J.A. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006, 333, 15. [Google Scholar] [CrossRef] [PubMed]
- Ingersoll, K.S.; Cohen, J. The impact of medication regimen factors on adherence to chronic treatment: A review of literature. J. Behav. Med. 2008, 31, 213–224. [Google Scholar] [CrossRef] [PubMed]
- Rosen, O.Z.; Fridman, R.; Rosen, B.T.; Shane, R.; Pevnick, J.M. Medication adherence as a predictor of 30-day hospital readmissions. Patient Preference Adherence 2017, 11, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Nieuwlaat, R.; Wilczynski, N.; Navarro, T.; Hobson, N.; Jeffery, R.; Keepanasseril, A.; Agoritsas, T.; Mistry, N.; Iorio, A.; Jack, S.; et al. Interventions for enhancing medication adherence. Cochrane Database Syst. Rev. 2014, 11. [Google Scholar] [CrossRef]
- Kardas, P.; Lewekm, P.; Matyjaszczyk, M. Determinants of patient adherence: A review of systematic reviews. Front. Pharmacol. 2013, 4, 91. [Google Scholar] [CrossRef] [PubMed]
- Vermeire, E.; Hearnshaw, H.; Van Royen, P.; Denekens, J. Patient adherence to treatment: Three decades of research. A comprehensive review. J. Clin. Pharm. Ther. 2001, 26, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Weinman, J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J. Psychosom. Res. 1999, 47, 555–567. [Google Scholar] [CrossRef]
- Horne, R.; Chapman, S.C.; Parham, R.; Freemantle, N.; Forbes, A.; Cooper, V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: A meta-analytic review of the Necessity-Concerns Framework. PLoS ONE 2013, 8, e80633. [Google Scholar] [CrossRef] [PubMed]
- Royal Pharmaceutical Society. Improving Patient Outcomes: The Better Use of Multi-Compartment Compliance Aids; Royal Pharmaceutical Society: London, UK, 2013. [Google Scholar]
- Easthall, C.; Song, F.; Bhattacharya, D. A meta-analysis of cognitive-based behaviour change techniques as interventions to improve medication adherence. BMJ Open 2013, 3, e002749. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.R.; Rollnick, S.R. Motivational Interviewing: Preparing People for Change; Guilford Press: New York, NY, USA, 1991. [Google Scholar]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change intervention. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- DiMatteo, M.R. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychol. 2004, 23, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Rintamaki, L.S.; Davis, T.C.; Skripkauskas, S.; Bennett, C.L.; Wolf, M.S. Social stigma concerns and HIV medication adherence. AIDS Patient Care STDs 2006, 20, 359–368. [Google Scholar] [CrossRef] [PubMed]
- Taddeo, D.; Egedy, M.; Frappier, J.Y. Adherence to treatment in adolescents. Paediatr. Child Health 2008, 13, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.J.; Twigg, M.; Taylor, N.; Easthall, C.; Hartt, J.; Budd, T.; Zhicheng, L.; Dima, A.; Bhattacharya, D. Final Report for the IMAB-Q Study: Validation and Feasibility Testing of a Novel Questionnaire to Identify Barriers to Medication Adherence; Pharmacy Research UK: London, UK, 2017; Available online: http://pharmacyresearchuk.org/wp-content/uploads/2017/01/IMAB-Q-validation-and-feasibility-testing-full-report.pdf (accessed on 1 August 2017).
- Michie, S.; Johnston, M.; Abraham, C.; Lawton, R.; Parker, D.; Walker, A. Making psychological theory useful for implementing evidence based practice: A consensus approach. Qual. Saf. Health Care 2005, 14, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef] [PubMed]
- Easthall, C.; Taylor, N.J.; Wright, D.J.; Bhattacharya, D. Developing the ‘Identification of Medication Adherence Barriers (IMAB) Instrument: A Novel Application of Behavior Change Theoretical Frameworks. In Proceedings of the UK Society for Behavioural Medicine (UKSBM) 8th Annual Scientific Meeting, Manchester, UK, 10–11 December 2012. [Google Scholar]
- Presseau, J.; Schwalm, J.D.; Grimshaw, J.M.; Witteman, H.O.; Natarajan, M.K.; Linklater, S.; Sullivan, K.; Ivers, N.M. Identifying determinants of medication adherence following myocardial infarction using the Theoretical Domains Framework and the Health Action Process Approach. Psychol. Health 2016, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Crayton, E.; Fahey, M.; Ashworth, M.; Besser, S.J.; Weinman, J.; Wright, A.J. Psychological determinants of medication adherence in stroke survivors: A systematic review of observational studies. Ann. Behav. Med. 2016, 31, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Voshaar, M.; Vriezekolk, J.; van Dulmen, S.; van den Bemt, B.; van de Laar, M. Barriers and facilitators to disease-modifying antirheumatic drug use in patients with inflammatory rheumatic diseases: A qualitative theory-based study. BMC Musculoskeletal Disord. 2016, 17, 442. [Google Scholar] [CrossRef] [PubMed]
- McCullough, A.R.; Ryan, C.; O’Neill, B.; Bradley, J.M.; Elborn, J.S.; Hughes, C.M. Defining the content and delivery of an intervention to Change AdhereNce to treatment in BonchiEctasis (CAN-BE): A qualitative approach incorporating the Theoretical Domains Framework, behavioural change techniques and stakeholder expert panels. BMC Health Serv. Res. 2015, 15, 342. [Google Scholar] [CrossRef] [PubMed]
- Jackson, C.; Eliasson, L.; Barber, N.; Weinman, J. Applying COM-B to medication adherence. A suggested framework for research and interventions. Eur. Health Psychol. 2014, 16, 7–17. [Google Scholar]
- Patton, D.E.; Hughes, C.M.; Cadogan, C.A.; Ryan, C.A. Theory-based interventions to improve medication adherence in older adults prescribed polypharmacy: As systematic review. Drugs Aging 2017, 34, 97–113. [Google Scholar] [CrossRef] [PubMed]
- Munro, S.; Lewin, S.; Swart, T.; Volmink, T. A review of health behaviour theories: How useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS? BMC Public Health 2007, 7, 104. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Wolever, R.Q.; Dreusicke, M.H. Integrative health coaching: A behavior skills approach that improves HbA1c and pharmacy claims-derived medication adherence. BMJ Open Diabetes Res. Care 2016, 4, e000201. [Google Scholar] [CrossRef] [PubMed]
- Carter, A.; Tamkin, P.; Wilson, S.; Miller, L. The Case for Health Coaching: Lessons Learned from Implementing a Training and Development Intervention for Clinicians across the East of England; Report Commissioned for NHS Health Education East of England; Institute for Employment Studies: Brighton, UK, 2015. [Google Scholar]
- Kivelä, K.; Elo, S.; Kyngäs, H.; Kääriäinen, M. The effects of health coaching on adult patients with chronic diseases: A systematic review. Patient Educ. Couns. 2014, 97, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Delaney, G.; Newlyn, N.; Pamplona, E.; Hocking, S.L.; Glastras, S.J.; McGrath, R.T.; Fulcher, G.R. Identification of Patients with Diabetes Who Benefit Most From a Health Coaching Program in Chronic Disease Management, Sydney, Australia, 2013. Prev. Chronic Dis. 2017, 14, E21. [Google Scholar] [CrossRef] [PubMed]
- Sherman, R.P.; Ganguli, I. Primary Care—Based Health Coaching for the Management of Prediabetes. Am. J. Lifestyle Med. 2017. [Google Scholar] [CrossRef]
- Duff, A.; Latchford, G. Using motivational interviewing to improve medicines adherence. Pharm. J. 2016, 296, 7899. [Google Scholar] [CrossRef]
- Stanton, L.; Lyon, R. Using Adherence Therapy and Motivational Intervieiwing to Address Patients’ Concerns about Their Experiences with Medication. In Measuring and Improving Patients’ Experience of Care; Picton, C., Ed.; Royal Pharmaceutical Society: London, UK, 2015; pp. 7–8. [Google Scholar]
- White, D. A service evaluation of acceptability and patient experience of pharmacy consultations conducted within a CBT framework. Eur. J. Hosp. Pharm. 2014, 21, 170–174. [Google Scholar] [CrossRef]
- Barnett, N.L.; Flora, K. Patient-centred consultations in a dispensary setting: A learning journey. Eur. J. Hosp. Pharm. 2017, 24, 107–109. [Google Scholar] [CrossRef]
- Nielsen, N. (OSCA coaching). Personal Communication, January 2017.
- Nina Barnett London North West Healthcare NHS Trust. Unpublished data. July 2017.
- Barnett, N.; Dave, K.; Athwal, D.; Parmar, P.; Kaher, S.; Ward, C. Impact of an integrated medicines management service on preventable medicines-related readmission to hospital: A descriptive study. Eur. J. Hosp. Pharm. 2016. [Google Scholar] [CrossRef]
- Barnett, N. The new medicine service and beyond—Taking concordance to the next level. Pharm. J. 2011, 287, 653. [Google Scholar]
- Whitmore, J. Coaching for Performance: Growing Human Potential and Purpose: The Principles and Practice of Coaching and Leadership; Nicholas Brealey: Boston, MA, USA, 2002. [Google Scholar]
- Centre for Pharmacy Postgraduate Education. Consultation Skills for Pharmacy Practice: Taking a Patient-Centred Approach. 2014. Available online: http://www.consultationskillsforpharmacy.com/docs/docb.pdf (accessed on 19 February 2017).
- Barnett, N.L. Medication adherence: Where are we now? A UK perspective. Eur. J. Hosp. Pharm. 2014, 21, 181–184. [Google Scholar] [CrossRef]
- Centre for Pharmacy Postgraduate Education. Polypharmacy Medial Wall. 2017. Available online: https://www.cppe.ac.uk/therapeutics/polypharmacy (accessed on 26 June 2017).
- Barnett, N.; Jubraj, B. What Would Be Helpful to You Right Now? Making the Difference in a Short Consultation. 2014. Available online: https://vimeo.com/150664602 (accessed on 6 March 2017).
- Barnett, N.; Jubraj, B. What Would Be Helpful to You Right Now? Making the Difference in a Short Consultation. Debrief. 2014. Available online: https://vimeo.com/150664603 (accessed on 6 March 2017).
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Easthall, C.; Barnett, N. Using Theory to Explore the Determinants of Medication Adherence; Moving Away from a One-Size-Fits-All Approach. Pharmacy 2017, 5, 50. https://doi.org/10.3390/pharmacy5030050
Easthall C, Barnett N. Using Theory to Explore the Determinants of Medication Adherence; Moving Away from a One-Size-Fits-All Approach. Pharmacy. 2017; 5(3):50. https://doi.org/10.3390/pharmacy5030050
Chicago/Turabian StyleEasthall, Claire, and Nina Barnett. 2017. "Using Theory to Explore the Determinants of Medication Adherence; Moving Away from a One-Size-Fits-All Approach" Pharmacy 5, no. 3: 50. https://doi.org/10.3390/pharmacy5030050
APA StyleEasthall, C., & Barnett, N. (2017). Using Theory to Explore the Determinants of Medication Adherence; Moving Away from a One-Size-Fits-All Approach. Pharmacy, 5(3), 50. https://doi.org/10.3390/pharmacy5030050




