The PHAR-QA Project: Competency Framework for Pharmacy Practice—First Steps, the Results of the European Network Delphi Round 1
Abstract
:1. Introduction
2. Methodology
- (1)
- (2)
- Evaluation by the consortial expert panel (the authors)—the round 1 questionnaire was modified in three Delphi rounds, the panel providing rankings and comments on what was unclear, missing, or in duplicate, etc., so producing the fourth version. Nine out of thirteen of the panel (authors) are practicing pharmacists in addition to being academics. Several have more than 20 years of experience as practicing pharmacists. Twelve out of thirteen have a long experience of university teaching of pharmacy, in most cases of 25 years or more. One is an expert in medical education. Once terminology issues were resolved there was widespread consensus on the different visions of pharmacy practice.
- (3)
- The fourth version of the questionnaire consisting of 68 propositions for competences for pharmacy practice in 13 clusters was submitted to a large expert panel (academics, students, and pharmacists from all areas of the profession (n = 1245).
- (4)
- The analysis of ranking data and comments on the fourth version, gathered using a surveymonkey questionnaire [34], will lead to the production of the fifth version. The ranking data and comments on the fourth version are presented in this article. The surveymonkey questionnaire (Figure 1) was available online from 14 February 2014 through 1 November 2015 i.e., 8.5 months. Such a long period was required in order to achieve (a modicum of) balance in the distribution of respondents (by occupation, country, age…).
- (5)
- A future second evaluation by the large European wide expert panel will lead to the production of the final QA framework.
- (1)
- Age
- (2)
- Country of residence
- (3)
- Current occupation: community, hospital or industrial pharmacist, pharmacist working on other area, student, academic
- (4)
- If you are a student, what is your year of enrolment?
- (5)
- If you are a professional (licensed practitioner, academic staff...), how long have you been practicing?
- (6)
- Job title
- (1)
- Learning and knowledge.
- (2)
- Values.
- (3)
- Communication and organizational skills.
- (4)
- Knowledge of different areas of the science of medicines.
- (5)
- Understanding of industrial pharmacy.
- (6)
- Patient consultation and assessment.
- (7)
- Need for drug treatment.
- (8)
- Drug interactions.
- (9)
- Provision of drug product.
- (10)
- Patient education.
- (11)
- Provision of information and service.
- (12)
- Monitoring of drug therapy.
- (13)
- Evaluation of outcomes.
- (1)
- Not important = Can be ignored.
- (2)
- Quite important =Valuable but not obligatory.
- (3)
- Very important = Obligatory with exceptions depending upon field of pharmacy practice.
- (4)
- Essential = Obligatory.
| Rank | Frequency | |
|---|---|---|
| 1 | 3 | |
| 2 | 121 | |
| 3 | 480 | |
| 4 | 622 | |
| Total = 1226 | f 3 + f 4 = 1102 | Score = (1102/1226) × 100 = 90% |
3. Statistical Analysis
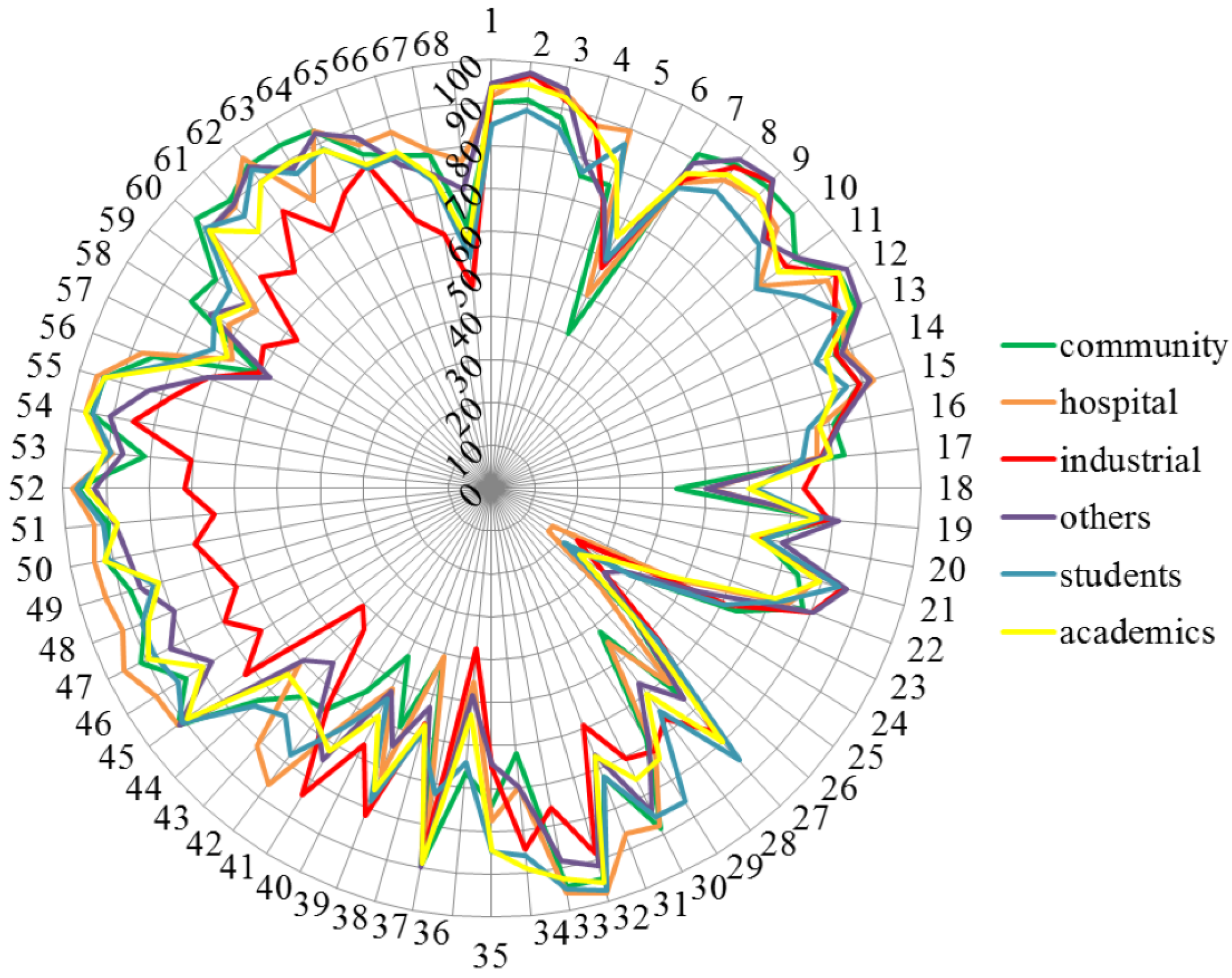
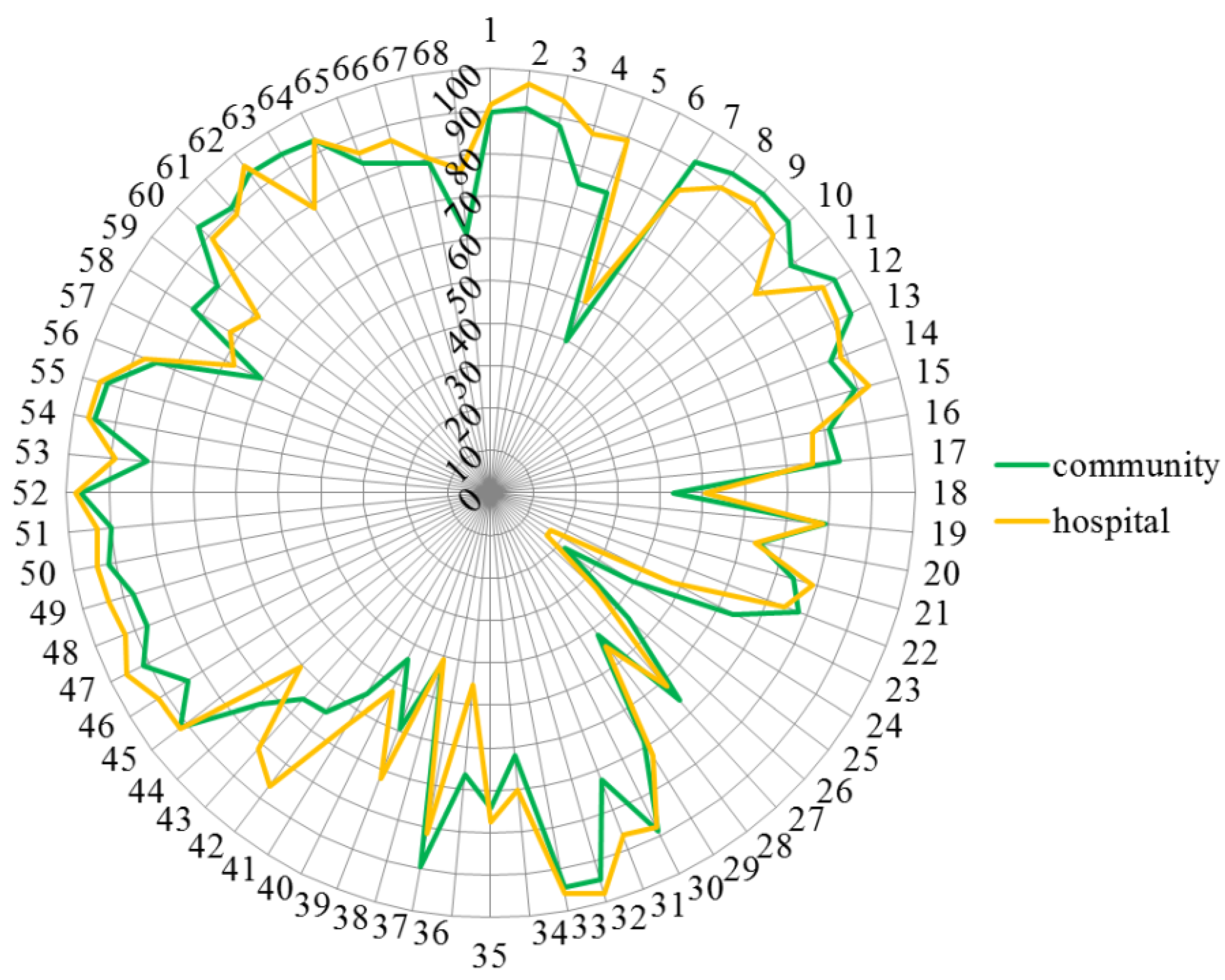
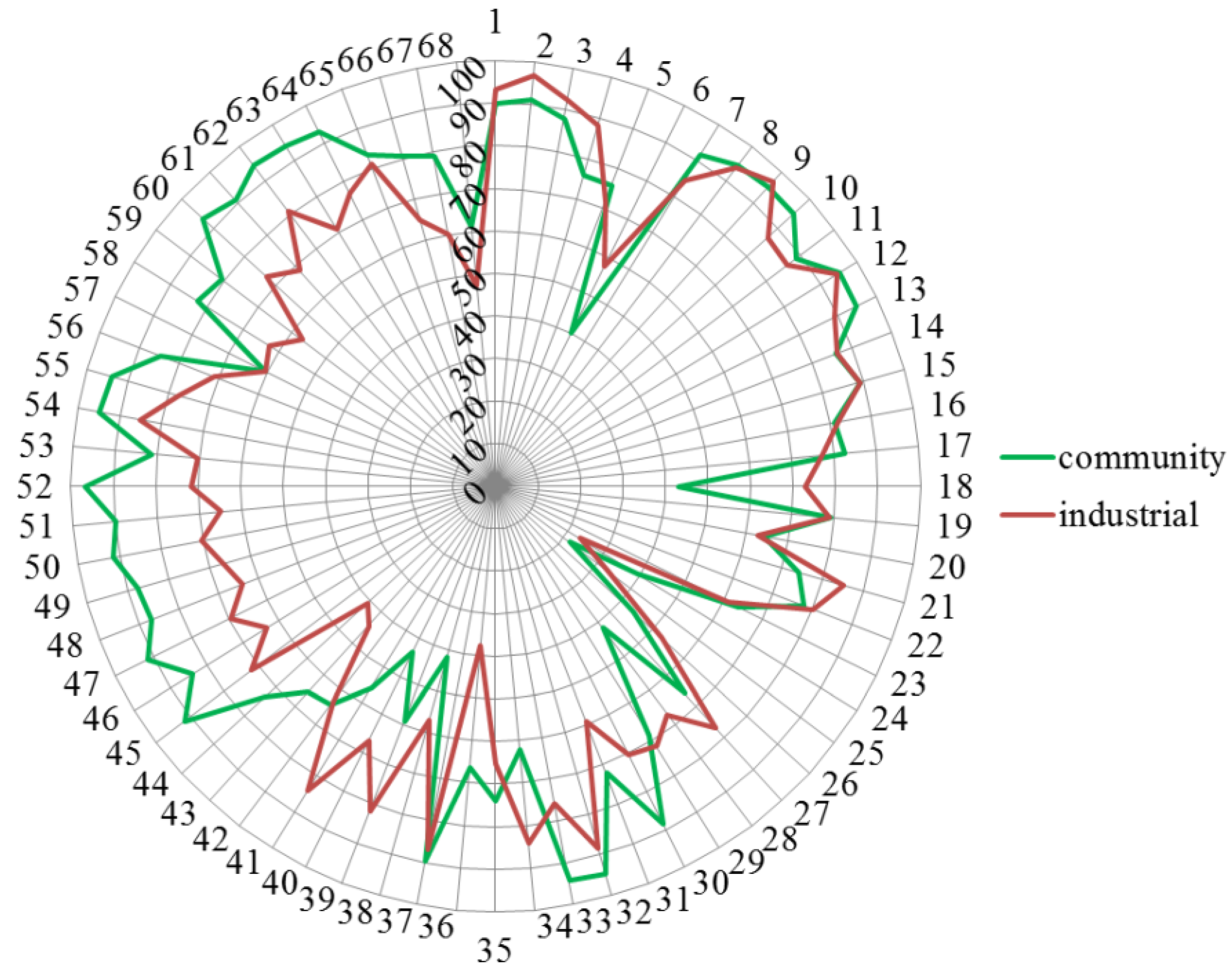
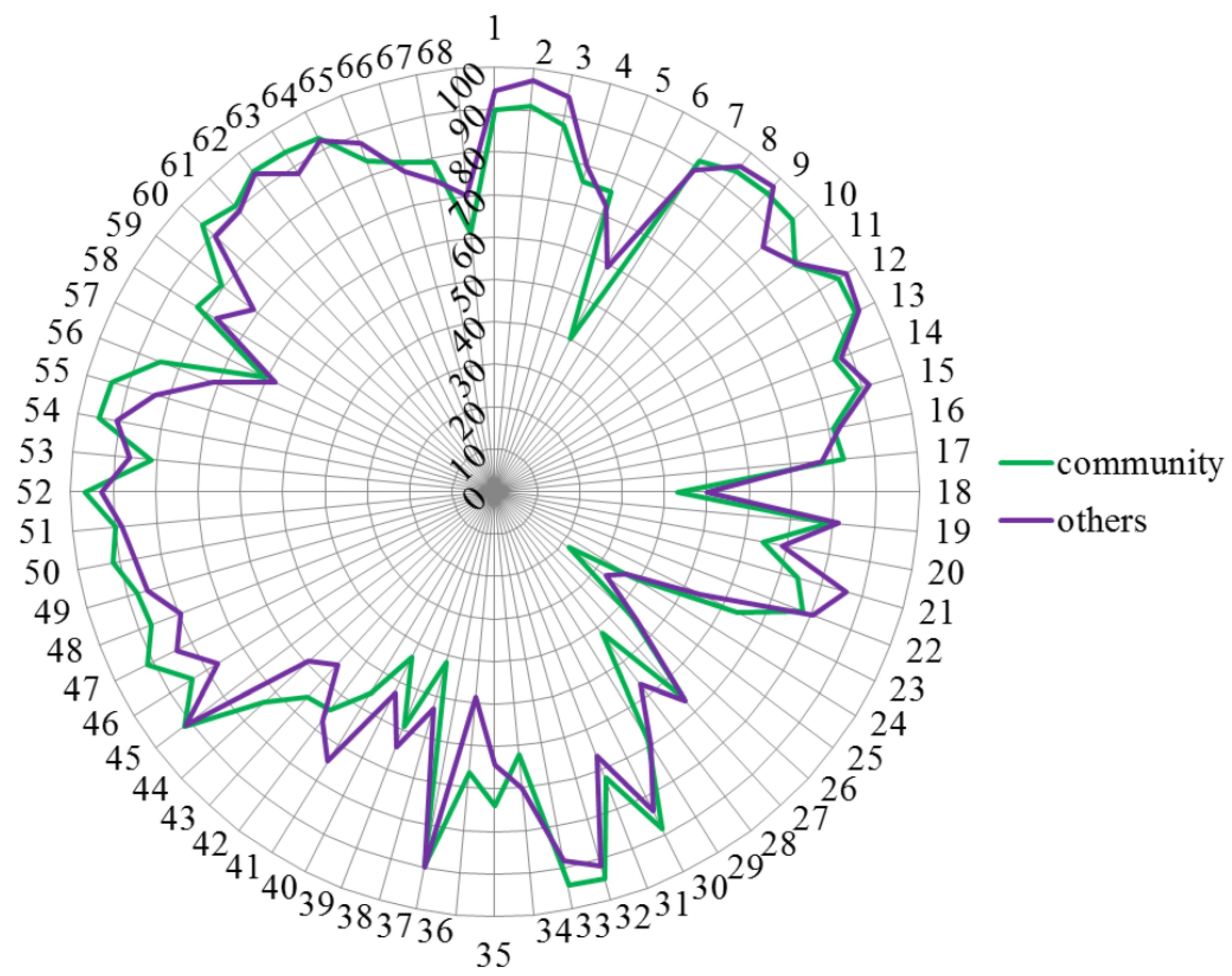
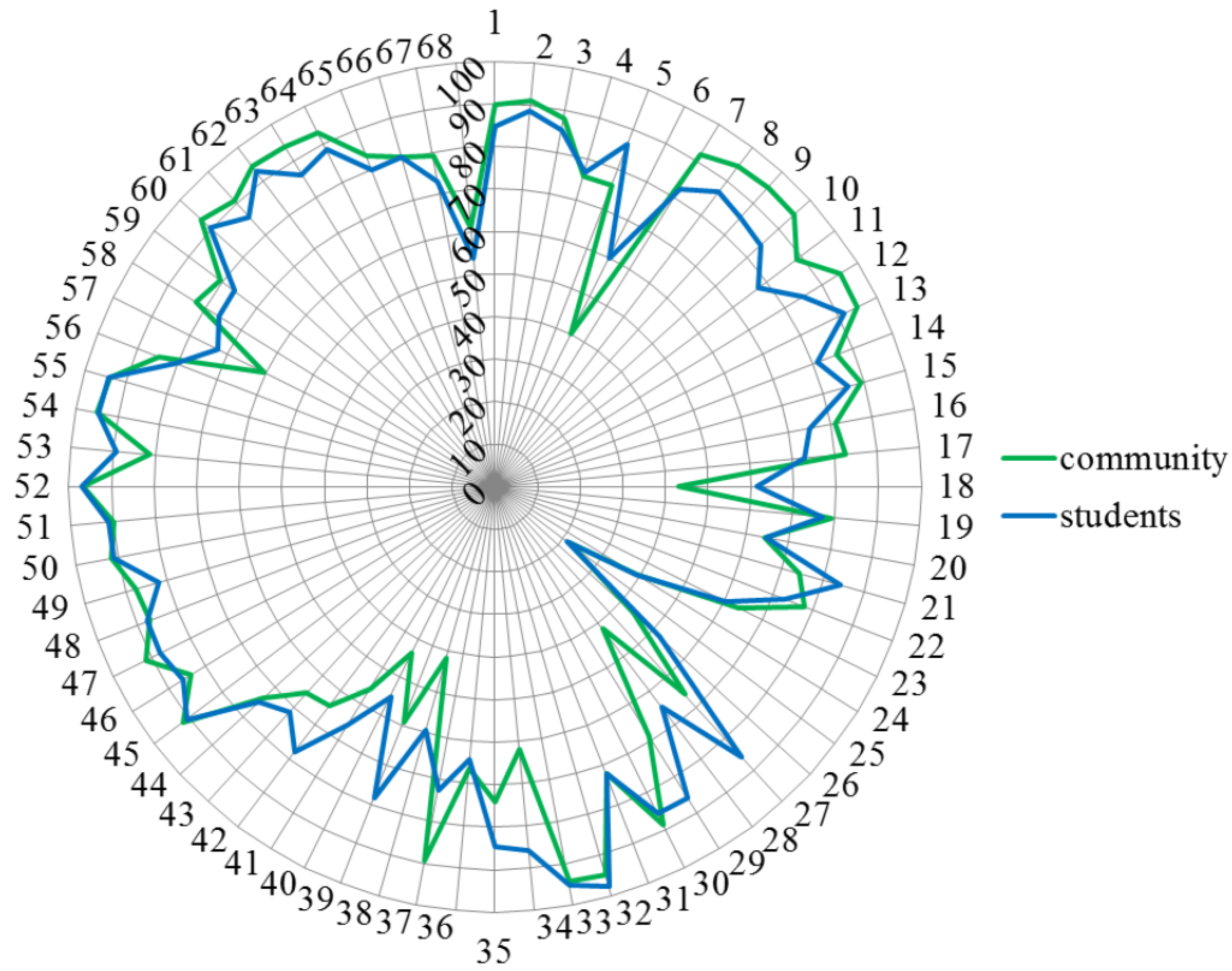
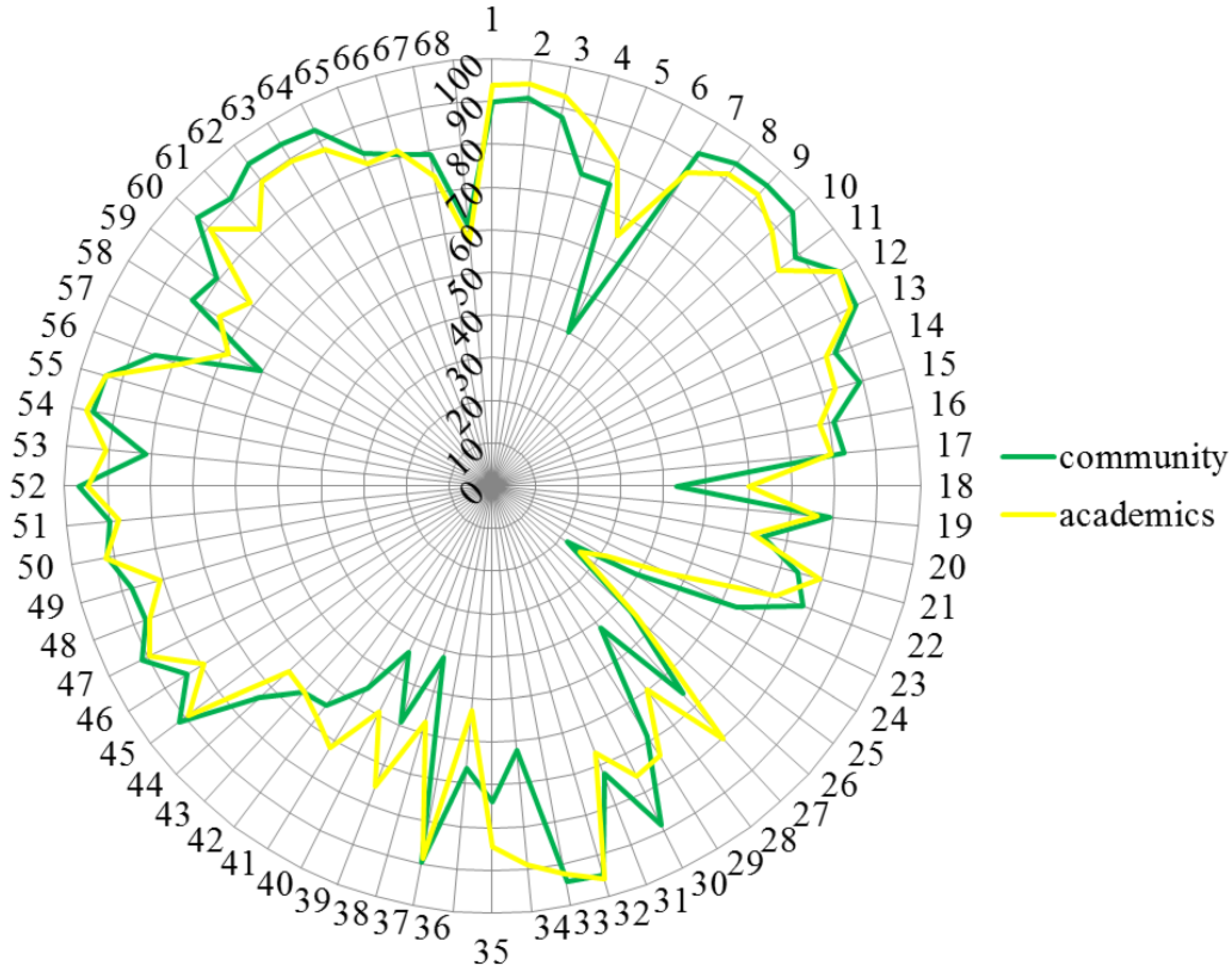
- Overall rankings by six groups of respondents. These are given as means and scores. Although the parametric use of means was probably robust enough under the circumstances, means are given as an indication only and differences were determined using non-parametric methods (see below).
- Comparisons of ranking by community pharmacists with that of the 5 other professional groups of respondents
4. Results
| Professional Groups | Number of Respondents | % | Estimated EUROPEAN POPULATION (× 1000) | Calculated Minimal Sample Size (95% Confidence Level, 10% Error) |
|---|---|---|---|---|
| Community pharmacists | 258 | 20.7 | 400 (PGEU) | 97 |
| Hospital pharmacists | 152 | 12.2 | 12 (EAHP) | 96 |
| Industrial pharmacists | 135 | 10.8 | 10 (EIPG) | 96 |
| Others | 77 | 6.2 | ? | ? |
| Breakdown of “others” | ||||
| Regulatory affairs, government | 27 | - | ? | ? |
| Consultancy | 10 | - | ? | ? |
| Wholesale, marketing, distribution | 10 | - | ? | ? |
| Lobbyist, NGO | 6 | - | ? | ? |
| Pharmacy chamber, society, association | 5 | - | ? | ? |
| Healthcare insurance agency | 1 | - | ? | ? |
| Not specified | 18 | - | - | - |
| Students | 382 | 30.7 | 200 (PHARMINE) | 96 |
| Academics | 241 | 19.4 | 10 (PHARMINE) | 96 |
| Total | 1245 | 100 | 400 + 12 + 10 + 200 + 10 = 632 | 97 |
| Rank | Number | % |
|---|---|---|
| 1 | 2470 | 2.9 |
| 2 | 14,933 | 17.6 |
| 3 | 30,132 | 35.6 |
| 4 | 29,194 | 34.1 |
| Cannot rank | 1764 | 2.1 |
| Blank | 6167 | 7.3 |
| Theoretical total | = 68 × 1245 = 84,660 | 100% |
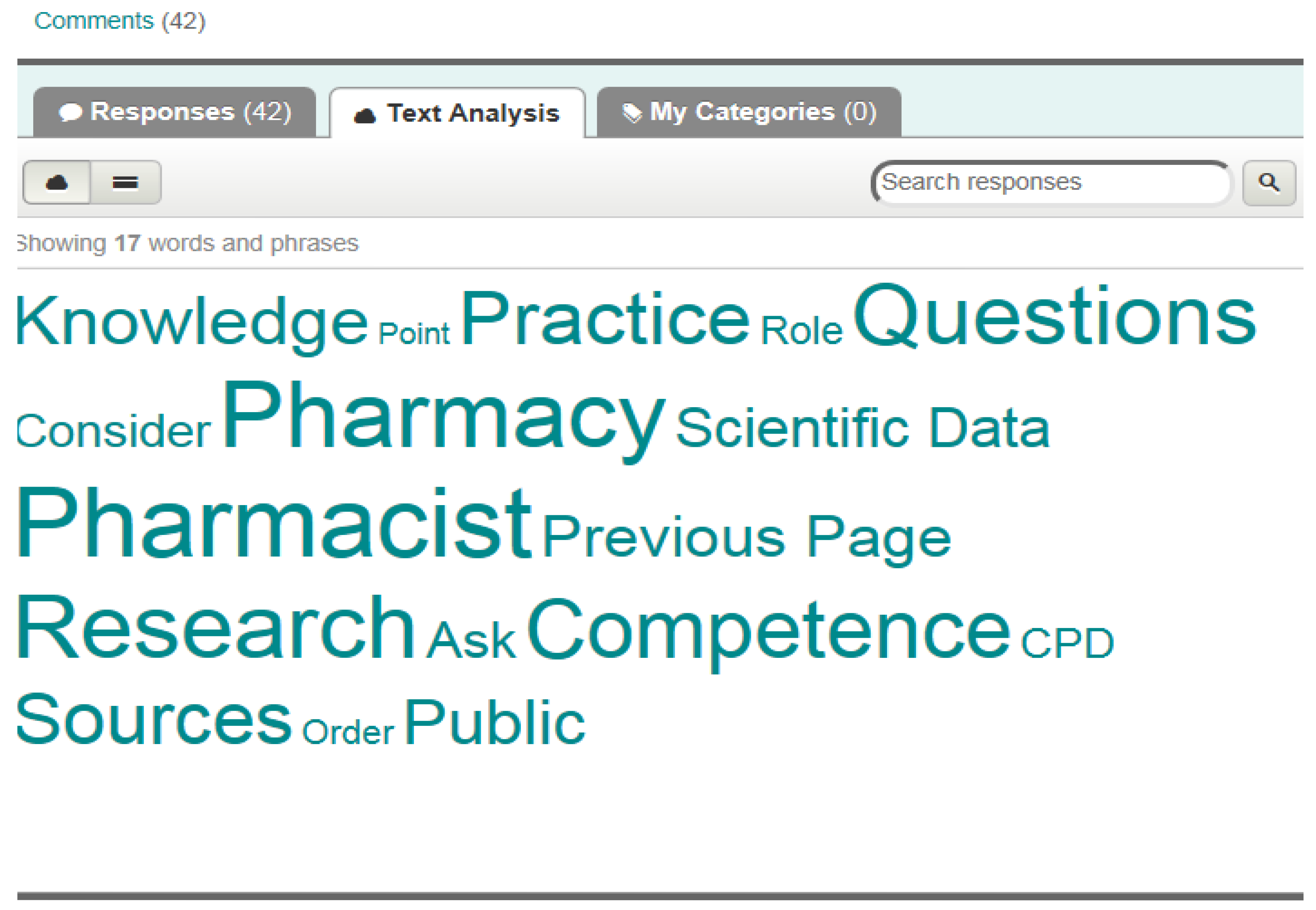
- Target audience
- ○
- “…refer to daily work in a community pharmacy”
- ○
- “focus on practicing pharmacists”
- ○
- “for specialists”
- ○
- “Not really the role of primary care, but important for some knowledge and awareness.”
- ○
- “Things that every pharmacist should be familiar with and even more in patient care fields, as in hospital or community pharmacy.”
- ○
- “For community pharmacists the above are essential, but for other pharmacists less.”
- ○
- “Can imagine it to be important in hospitals...”
- ○
- “For clinical and hospital pharmacists.”
- University level
- ○
- “Competences recorded as ‘very important’ cannot be fully obtained on pre-graduate level and also postgraduate training is needed.”
- ○
- “Competence 66 cannot be fully achieved during the pre-graduate training and requires also postgraduate education.”
- Difficulties in application
- ○
- “Are subject areas professional competences?”
- ○
- “If not commercially available I would contend that we should change what we are prescribing. I do not believe in ‘specials’ which in the UK are abused and contribute hugely and inappropriately to our drugs bill.”
- ○
- “There are always people who need some special drug which is not commercially available.”
- ○
- “Not sure how most pharmacists would be able to manufacture?”
- ○
- “General information on diet or exercise is important but the specific recommendations for the patient should be made by the experts in those areas (e.g. dietician or physiotherapist).”
- ○
- “Information should be basically provided by doctors, before pharmacists.”
- ○
- “I am not sure that pharmacists know current clinical guidelines. If medicine is prescribed we give it to patient.”
- Suggestions for further inclusions, etc.
- ○
- “Acquire other competencies for new services like vaccinations in the pharmacy, screening tests (colon cancer, heart disease, COPD, etc.) Public Health services in general, NCD (non-communicable diseases)”
- ○
- “Services like vaccinations, screenings (colon cancer, kidney, COPD, Heart disease, etc.) and others should become essential in the curriculum in order to be able to perform the services in the future.”
- ○
- “Pharmacist should also provide information about medical devices and other items available in the pharmacy.”
- ○
- “The knowledge on drug therapies and reactions on failing therapies are core fields for pharmacists.”
- ○
- “Radio-pharmacy”
- Technical difficulties with the survey
- ○
- “In my browser section 6 appears blank”
- ○
- “Never ask 2 things in the same question…”
- ○
- “No possibility of open-ended questions…”
- Language difficulties
- ○
- “Too complicated for my simple English…”
- ○
- “I cannot rank this competence for I do not fully understand the meaning of the competence.”
5. Discussion
6. Conclusions
7. Perspectives
- The ranking of the fourth version of the framework presented in this paper
- The comments of the respondents, namely
- ○
- Need for simplified construction of questions
- ○
- Attention given to use of easy to understand English
- The question “did we miss anything?” with suggestions for competences to be included (open-ended question)
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix
| Number of Competence | Mean Ranking | Median Ranking | Score 3% + 4% | |
|---|---|---|---|---|
| 7. Personal competences: learning and knowledge. | ||||
| 1. Ability to identify learning needs and to learn independently (including continuous professional development (CPD)). | 1 | 3.4 | 4 | 89.89 |
| 2. Analysis: ability to apply logic to problem solving, evaluating pros and cons and following up on the solution found. | 2 | 3.5 | 4 | 92.70 |
| 3. Synthesis: capacity to gather and critically appraise relevant knowledge and to summarize the key points. | 3 | 3.4 | 4 | 89.70 |
| 4. Capacity to evaluate scientific data in line with current scientific and technological knowledge. | 4 | 3.2 | 3 | 81.38 |
| 5. Ability to interpret preclinical and clinical evidence-based medical science and apply the knowledge to pharmaceutical practice. | 5 | 3.2 | 3 | 81.02 |
| 6. Ability to design and conduct research using appropriate methodology. | 6 | 2.7 | 3 | 55.47 |
| 7. Ability to maintain current knowledge of relevant legislation and codes of pharmacy practice. | 7 | 3.3 | 3 | 85.96 |
| 8. Personal competences: values. | ||||
| 1. Demonstrate a professional approach to tasks and human relations. | 8 | 3.4 | 4 | 91.09 |
| 2. Demonstrate the ability to maintain confidentiality. | 9 | 3.5 | 4 | 91.74 |
| 3. Take full personal responsibility for patient care and other aspects of one’s practice. | 10 | 3.4 | 4 | 88.43 |
| 4. Inspire the confidence of others in one's actions and advice. | 11 | 3.2 | 3 | 82.84 |
| 5. Demonstrate high ethical standards. | 12 | 3.6 | 4 | 91.88 |
| 9. Personal competences: communication and organizational skills. | ||||
| 1. Effective communication skills (both orally and written). | 13 | 3.4 | 4 | 92.60 |
| 2. Effective use of information technology. | 14 | 3.1 | 3 | 84.63 |
| 3. Ability to work effectively as part of a team. | 15 | 3.3 | 3 | 87.76 |
| 4. Ability to identify and implement legal and professional requirements relating to employment (e.g., for pharmacy technicians) and to safety in the workplace. | 16 | 3.1 | 3 | 78.43 |
| 5. Ability to contribute to the learning and training of staff. | 17 | 3.0 | 3 | 77.46 |
| 6. Ability to design and manage the development processes in the production of medicines. | 18 | 2.7 | 3 | 56.59 |
| 7. Ability to identify and manage risk and quality of service issues. | 19 | 3.1 | 3 | 77.99 |
| 8. Ability to identify the need for new services. | 20 | 2.8 | 3 | 64.00 |
| 9. Ability to communicate in English and/or locally relevant languages. | 21 | 3.2 | 3 | 80.67 |
| 10. Ability to evaluate issues related to quality of service. | 22 | 2.9 | 3 | 75.07 |
| 11. Ability to negotiate, understand a business environment and develop entrepreneurship. | 23 | 2.7 | 3 | 56.62 |
| 10. Personal competences: knowledge of different areas of the science of medicines. | ||||
| 1. Plant and animal biology. | 24 | 2.2 | 2 | 32.87 |
| 2. Physics. | 25 | 2.0 | 2 | 23.65 |
| 3. General and inorganic chemistry. | 26 | 2.5 | 2 | 46.50 |
| 4. Organic and medicinal/pharmaceutical chemistry. | 27 | 3.1 | 3 | 75.26 |
| 5. Analytical chemistry. | 28 | 2.7 | 3 | 56.29 |
| 6. General and applied biochemistry (medicinal and clinical). | 29 | 3.0 | 3 | 75.74 |
| 7. Anatomy and physiology; medical terminology. | 30 | 3.2 | 3 | 82.86 |
| 8. Microbiology. | 31 | 2.9 | 3 | 71.21 |
| 9. Pharmacology including pharmacokinetics. | 32 | 3.7 | 4 | 95.21 |
| 10. Pharmacotherapy and pharmaco-epidemiology. | 33 | 3.6 | 4 | 91.98 |
| 11. Pharmaceutical technology including analyses of medicinal products. | 34 | 3.2 | 3 | 78.24 |
| 12. Toxicology. | 35 | 3.1 | 3 | 77.92 |
| 13. Pharmacognosy. | 36 | 2.7 | 3 | 56.07 |
| 14. Legislation and professional ethics. | 37 | 3.3 | 3 | 83.13 |
| 11. Personal competences: understanding of industrial pharmacy. | ||||
| 1. Current knowledge of design, synthesis, isolation, characterization and biological evaluation of active substances. | 38 | 2.6 | 3 | 52.39 |
| 2. Current knowledge of good manufacturing practice (GMP) and of good laboratory practice (GLP). | 39 | 3.0 | 3 | 72.60 |
| 3. Current knowledge of European directives on qualified persons (QPs). | 40 | 2.6 | 3 | 54.44 |
| 4. Current knowledge of drug registration, licensing and marketing. | 41 | 2.9 | 3 | 67.36 |
| 5. Current knowledge of good clinical practice (GCP). | 42 | 3.0 | 3 | 71.96 |
| 12. Patient care competences: patient consultation and assessment. | ||||
| 1. Ability to perform and interpret medical laboratory tests. | 43 | 2.9 | 3 | 66.46 |
| 2. Ability to perform appropriate diagnostic or physiological tests to inform clinical decision making e.g., measurement of blood pressure. | 44 | 2.8 | 3 | 66.27 |
| 3. Ability to recognize when referral to another member of the healthcare team is needed because a potential clinical problem is identified (pharmaceutical, medical, psychological or social). | 45 | 3.4 | 4 | 88.86 |
| 13. Patient care competences: need for drug treatment. | ||||
| 1. Retrieval and interpretation of relevant information on the patient's clinical background. | 46 | 3.2 | 3 | 82.23 |
| 2. Retrieval and interpretation of an accurate and comprehensive drug history if and when required. | 47 | 3.4 | 4 | 87.83 |
| 3. Identification of non-adherence and implementation of appropriate patient intervention. | 48 | 3.3 | 3 | 84.80 |
| 4. Ability to advise to physicians and—in some cases—prescribe medication. | 49 | 3.2 | 3 | 83.10 |
| 14. Patient care competences: drug interactions. | ||||
| 1. Identification, understanding and prioritization of drug-drug interactions at a molecular level (e.g., use of codeine with paracetamol). | 50 | 3.5 | 4 | 89.35 |
| 2. Identification, understanding, and prioritization of drug-patient interactions, including those that preclude or require the use of a specific drug (e.g., trastuzumab for treatment of breast cancer in women with HER2 overexpression). | 51 | 3.4 | 4 | 87.51 |
| 3. Identification, understanding, and prioritization of drug-disease interactions (e.g., NSAIDs in heart failure). | 52 | 3.6 | 4 | 93.61 |
| 15. Patient care competences: provision of drug product. | ||||
| 1. Familiarity with the bio-pharmaceutical, pharmacodynamic and pharmacokinetic activity of a substance in the body. | 53 | 3.3 | 3 | 85.62 |
| 2. Supply of appropriate medicines taking into account dose, correct formulation, concentration, administration route and timing. | 54 | 3.6 | 4 | 94.03 |
| 3. Critical evaluation of the prescription to ensure that it is clinically appropriate and legal. | 55 | 3.5 | 4 | 91.87 |
| 4. Familiarity with the supply chain of medicines and the ability to ensure timely flow of drug products to the patient. | 56 | 3.1 | 3 | 80.26 |
| 5. Ability to manufacture medicinal products that are not commercially available. | 57 | 2.9 | 3 | 66.57 |
| 16. Patient care competences: patient education. | ||||
| 1. Promotion of public health in collaboration with other actors in the healthcare system. | 58 | 3.1 | 3 | 75.53 |
| 2. Provision of appropriate lifestyle advice on smoking, obesity, etc. | 59 | 3.0 | 3 | 73.07 |
| 3. Provision of appropriate advice on resistance to antibiotics and similar public health issues. | 60 | 3.3 | 3 | 88.66 |
| 17. Patient care competences: provision of information and service. | ||||
| 1. Ability to use effective consultations to identify the patient's need for information. | 61 | 3.2 | 3 | 84.84 |
| 2. Provision of accurate and appropriate information on prescription medicines. | 62 | 3.5 | 4 | 91.81 |
| 3. Provision of informed support for patients in selection and use of non-prescription medicines for minor ailments (e.g., cough remedies...). | 63 | 3.4 | 4 | 86.09 |
| 18. Patient care competences: monitoring of drug therapy. | ||||
| 1. Identification and prioritization of problems in the management of medicines in a timely manner and with sufficient efficacy to ensure patient safety. | 64 | 3.3 | 3 | 89.01 |
| 2. Ability to monitor and report to all concerned in a timely manner, and in accordance with current regulatory guidelines on Good Pharmacovigilance Practices (GVPs), Adverse Drug Events and Reactions (ADEs and ADRs). | 65 | 3.2 | 3 | 82.35 |
| 3. Undertaking of a critical evaluation of prescribed medicines to confirm that current clinical guidelines are appropriately applied. | 66 | 3.1 | 3 | 79.88 |
| 19. Patient care competences: evaluation of outcomes. | ||||
| 1. Assessment of outcomes on the monitoring of patient care and follow-up interventions. | 67 | 3.0 | 3 | 74.14 |
| 2. Evaluation of cost effectiveness of treatment. | 68 | 2.7 | 3 | 59.60 |
References
- The PHAR-QA Project: Quality Assurance in European Pharmacy Education and Training. Available online: http://www.phar-qa.eu (accessed on 12 November 2015).
- The European Commission. The EU Directive 2013/55/EU on the Recognition of Professional Qualifications. Available online: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2005:255:0022:0142:EN:PDF (accessed on 18 March 2014).
- Atkinson, J.; Rombaut, B. The PHARMINE paradigm—matching the supply of pharmacy education and training to demands. Eur. Ind. Pharm. 2010, 6, 4–7. [Google Scholar]
- Atkinson, J.; Rombaut, B. The PHARMINE study on the impact of the European Union directive on sectoral professions and of the Bologna declaration on pharmacy education in Europe. Pharm. Pract. 2011, 9, 169–187. [Google Scholar] [CrossRef]
- Atkinson, J.; Rombaut, B.; Sánchez Pozo, A.; Rekkas, D.; Veski, P.; Hirvonen, J.; Bozic, B.; Skowron, A.; Mircioiu, C.; Marcincal, A.; et al. Systems for Quality Assurance in Pharmacy Education and Training in the European Union. Pharmacy 2014, 2, 17–26. [Google Scholar] [CrossRef]
- International Pharmaceutical Federation. FIP Education Initiative. In Quality Assurance of Pharmacy Education: The FIP Global Framework, 2nd ed.; 2014; Available online: https://www.fip.org/files/fip/PharmacyEducation/Quality_Assurance/QA_Framework_2nd_Edition_online_version.pdf (accessed on 12 November 2015).
- Bruno, A.; Bates, I.; Brock, T.; Anderson, C. Towards a global competency framework. Am. J. Pharm. Educ. 2010, 74, 56. [Google Scholar] [CrossRef] [PubMed]
- Govaerts, M.J. Educational competencies or education for professional competence? Med. Educ. 2008, 42, 234–236. [Google Scholar] [CrossRef] [PubMed]
- Mestrovic, A.; Stanicic, Z.; Ortner-Hadziabdic, M.; Mucalo, I.; Bates, I.; Duggan, C.; Carter, S.; Bruno, A.; Košiček, M. Individualized education and competency development of Croatian community pharmacists using the General Level Framework. Am. J. Pharm. Educ. 2012, 76, 23. [Google Scholar] [CrossRef] [PubMed]
- Dorman, T.; Miller, B.M. Continuing medical education: The link between physician learning and health care outcomes. Acad. Med. 2011, 86, 1339. [Google Scholar] [CrossRef] [PubMed]
- Svetlana1, S.; Ivana, T.; Tatjana, C.; Duskana, K.; Bates, I. Evaluation of Competences at the Community Pharmacy Settings. Ind. J. Pharm. Edu. Res. 2014, 48, 22–30. [Google Scholar] [CrossRef]
- The Association of Lithuanian Serials. Center of Competence of Healthcare and Pharmacy Specialists. Available online: http://serials.lt/news/ (accessed on 12 November 2015).
- The Pharmaceutical Society of Ireland. Core Competency Framework. Available online: http://www.thepsi.ie/gns/pharmacy-practice/core-competency-framework.aspx (accessed on 12 November 2015).
- The Competency Development and Evaluation Group (CoDEG). The CoDEG General Level Framework (GLF). Available online: http://www.codeg.org/frameworks/general-level-practice/ (accessed on 12 November 2015).
- European Association of Faculties of Pharmacy (EAFP). Available online: http://www.eafponline.eu/ (accessed on 12 November 2015).
- The TUNING Network. Competences: Medical Doctors. Available online: http://www.unideusto.org/tuningeu/subject-areas/medicine.html (accessed on 12 November 2015).
- Oxford English Dictionary. Definition of “Competence”. Available online: http://www.oed.com/view/Entry/37567?redirectedFrom=competence#eid (accessed on 12 November 2015).
- Merriam-Webster’s Dictionary. Definition of “Competence”. Available online: http://www.merriam-webster.com/dictionary/competence (accessed on 12 November 2015).
- The Council on Credentialing in Pharmacy. Credentialing in Pharmacy. Am. J. Health Syst. Pharm. 2001, 58, 69–76. [Google Scholar]
- PGEU—Pharmaceutical Group of the European Union. Available online: http://www.pgeu.eu/ (accessed on 12 November 2015).
- EPSA—European Pharmaceutical Students Association online. Available online: http://www.epsa-online.org/ (accessed on 12 November 2015).
- EAHP—European Association of Hospital Pharmacists. Available online: http://www.eahp.eu/ (accessed on 12 November 2015).
- EIPG—European Industrial Pharmacists Group. Available online: http://www.eipg.eu/ (accessed on 12 November 2015).
- ACPE—Accreditation Council for Pharmacy Education. Available online: https://www.acpe-accredit.org/ (accessed on 12 November 2015).
- Stupans, I.; McAllister, S.; Clifford, R.; Hughes, J.; Krass, I.; March, G.; Owen, S.; Woulfe, J. Nationwide collaborative development of learning outcomes and exemplar standards for Australian pharmacy programmes. Int. J. Pharm. Pract. 2014. Available online: http://onlinelibrary.wiley.com/doi/10.1111/ijpp.12163/pdf (accessed on 12 November 2015). [Google Scholar]
- Hsu, C.C.; Sandford, B.A. The Delphi Technique: Making Sense of Consensus. Pract. Assess. Res. Eval. 2007, 12, 1–8. [Google Scholar]
- A Competency Framework for Pharmacy Practitioners General Level (CoDEG): General Level Framework, September, 2010. Available online: http://www.codeg.org/frameworks/general-level-practice/ (accessed on 12 November 2015).
- World Federation for Medical Education (WFME) Global Standards for Quality Improvement in Basic Medical Education BME in English. Available online: http://wfme.org/standards/bme (accessed on 12 November 2015).
- PHARMINE WP3 Final Report Identifying and Defining Competences for Pharmacists. Available online: http://www.pharmine.org/wp-content/uploads/2014/05/PHARMINE-WP3-Final-ReportDEF_LO.pdf (accessed on 12 November 2015).
- Medical Education in Europe (MEDINE). Available online: http://medine2.com/archive/medine1/ (accessed on 12 November 2015).
- International Medical School IMS2020 Report 2011. Available online: http://www.ims-2020.eu/ (accessed on 12 November 2015).
- Association for Dental Education in Europe ADEE 2009. Available online: http://www.adee.org/ (accessed on 12 November 2015).
- Eurohealth 2012 Volume 18/2. Available online: http://www.euro.who.int/en/about-us/partners/observatory/publications/eurohealth/gender-and-health (accessed on 12 November 2015).
- SurveyMonkey (Online Survey Development Cloud). Available online: https://www.surveymonkey.com/ (accessed on 12 November 2015).
- Goodman, C. The Delphi technique: A critique. J. Adv. Nurs. 1987, 12, 729–734. [Google Scholar] [CrossRef] [PubMed]
- Marz, R.; Dekker, F.W.; van Schravendijk, C.; O’Flynn, S.; Ross, M.T. Tuning research competences for Bologna three cycles in medicine: Report of a MEDINE2 European consensus survey. Perp. Med. Educ. 2013, 2, 181–195. [Google Scholar] [CrossRef] [PubMed]
- Survey Software—The Survey System. Available online: http://www.surveysystem.com/sscalc.htm (accessed on 12 November 2015).
- Bourlioux, P. Erasmus subject evaluations. Studies in pharmacy in Europe. Available online: http://www.phar-qa.eu/wp-content/uploads/2015/04/P_Bourlioux_Erasmus-subject-evaluations-1995.pdf (accessed on 12 November 2015).
- EUA Briefing Note on Directive 2013/55/EU, Containing the Amendments to Directive 2005/36/EC on the Recognition of Professional Qualifications. Available online: http://www.eua.be/Libraries/Higher_Education/EUA_briefing_note_on_amended_Directive_January_2014.sflb.ashx (accessed on 12 November 2015).
- The consortium evaluation of the PHAR-QA framework of competences for pharmacists—revised version. Available online: https://www.surveymonkey.com/r/pharqa2 (accessed on 12 November 2015).
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Atkinson, J.; De Paepe, K.; Pozo, A.S.; Rekkas, D.; Volmer, D.; Hirvonen, J.; Bozic, B.; Skowron, A.; Mircioiu, C.; Marcincal, A.; et al. The PHAR-QA Project: Competency Framework for Pharmacy Practice—First Steps, the Results of the European Network Delphi Round 1. Pharmacy 2015, 3, 307-329. https://doi.org/10.3390/pharmacy3040307
Atkinson J, De Paepe K, Pozo AS, Rekkas D, Volmer D, Hirvonen J, Bozic B, Skowron A, Mircioiu C, Marcincal A, et al. The PHAR-QA Project: Competency Framework for Pharmacy Practice—First Steps, the Results of the European Network Delphi Round 1. Pharmacy. 2015; 3(4):307-329. https://doi.org/10.3390/pharmacy3040307
Chicago/Turabian StyleAtkinson, Jeffrey, Kristien De Paepe, Antonio Sánchez Pozo, Dimitrios Rekkas, Daisy Volmer, Jouni Hirvonen, Borut Bozic, Agnieska Skowron, Constantin Mircioiu, Annie Marcincal, and et al. 2015. "The PHAR-QA Project: Competency Framework for Pharmacy Practice—First Steps, the Results of the European Network Delphi Round 1" Pharmacy 3, no. 4: 307-329. https://doi.org/10.3390/pharmacy3040307
APA StyleAtkinson, J., De Paepe, K., Pozo, A. S., Rekkas, D., Volmer, D., Hirvonen, J., Bozic, B., Skowron, A., Mircioiu, C., Marcincal, A., Koster, A., Wilson, K., & Van Schravendijk, C. (2015). The PHAR-QA Project: Competency Framework for Pharmacy Practice—First Steps, the Results of the European Network Delphi Round 1. Pharmacy, 3(4), 307-329. https://doi.org/10.3390/pharmacy3040307













