Medication Use by Older Adults with Frailty: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Identifying the Research Question
- To analyze medication use in older adults with frailty by examining the prevalence of PIMs, polypharmacy, capacity for medication management, adherence to prescribed regimens, medication errors, and associated health outcomes.
- To provide recommendations for addressing medication-related issues in this population by detailing available tools (such as medication review instruments) and processes (including deprescribing strategies) that can aid in identifying and managing these problems.
2.2. Identifying the Relevant Studies
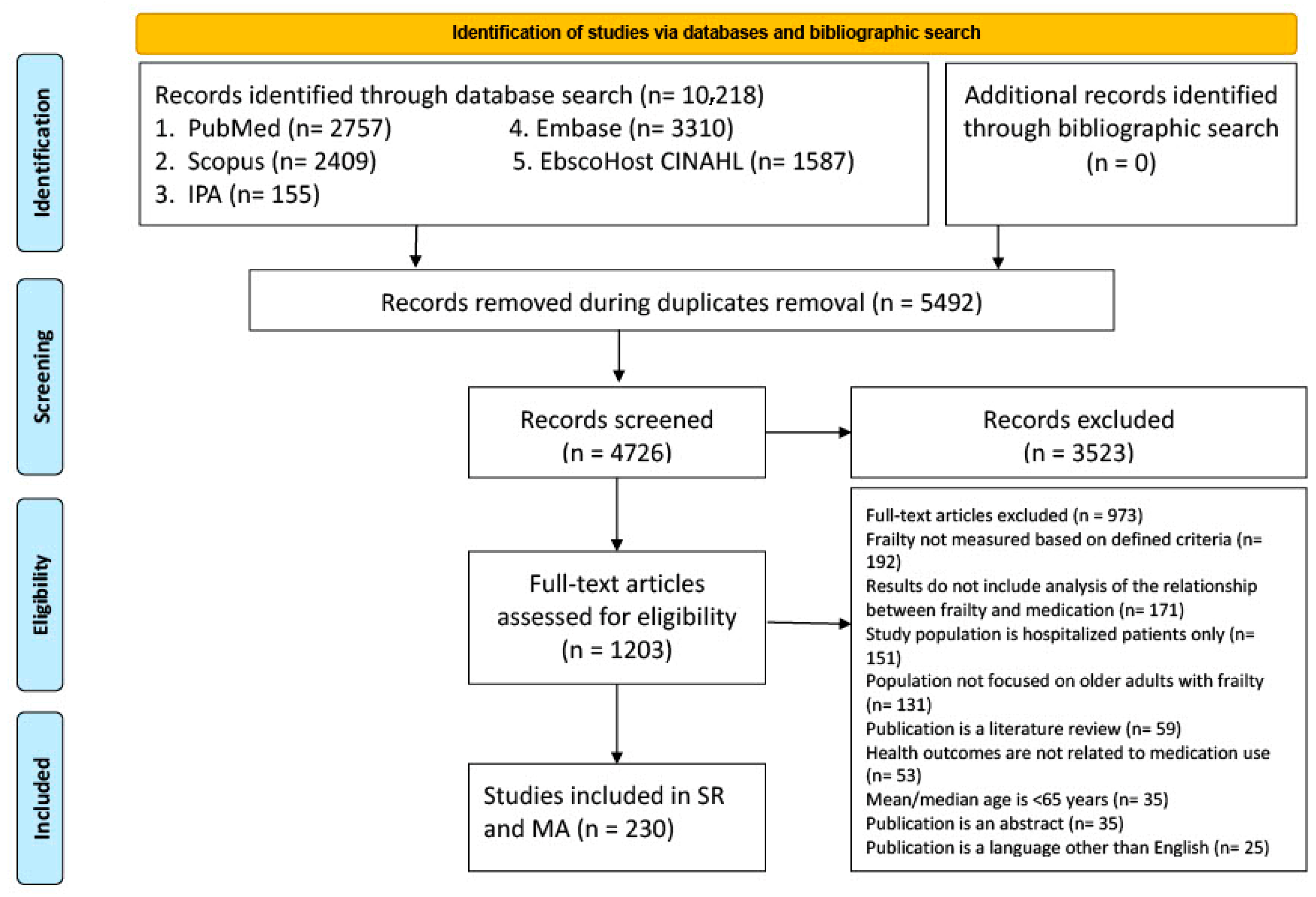
2.3. Study Selection
2.4. Data Charting
2.5. Collating, Summarizing, and Reporting the Results
3. Results
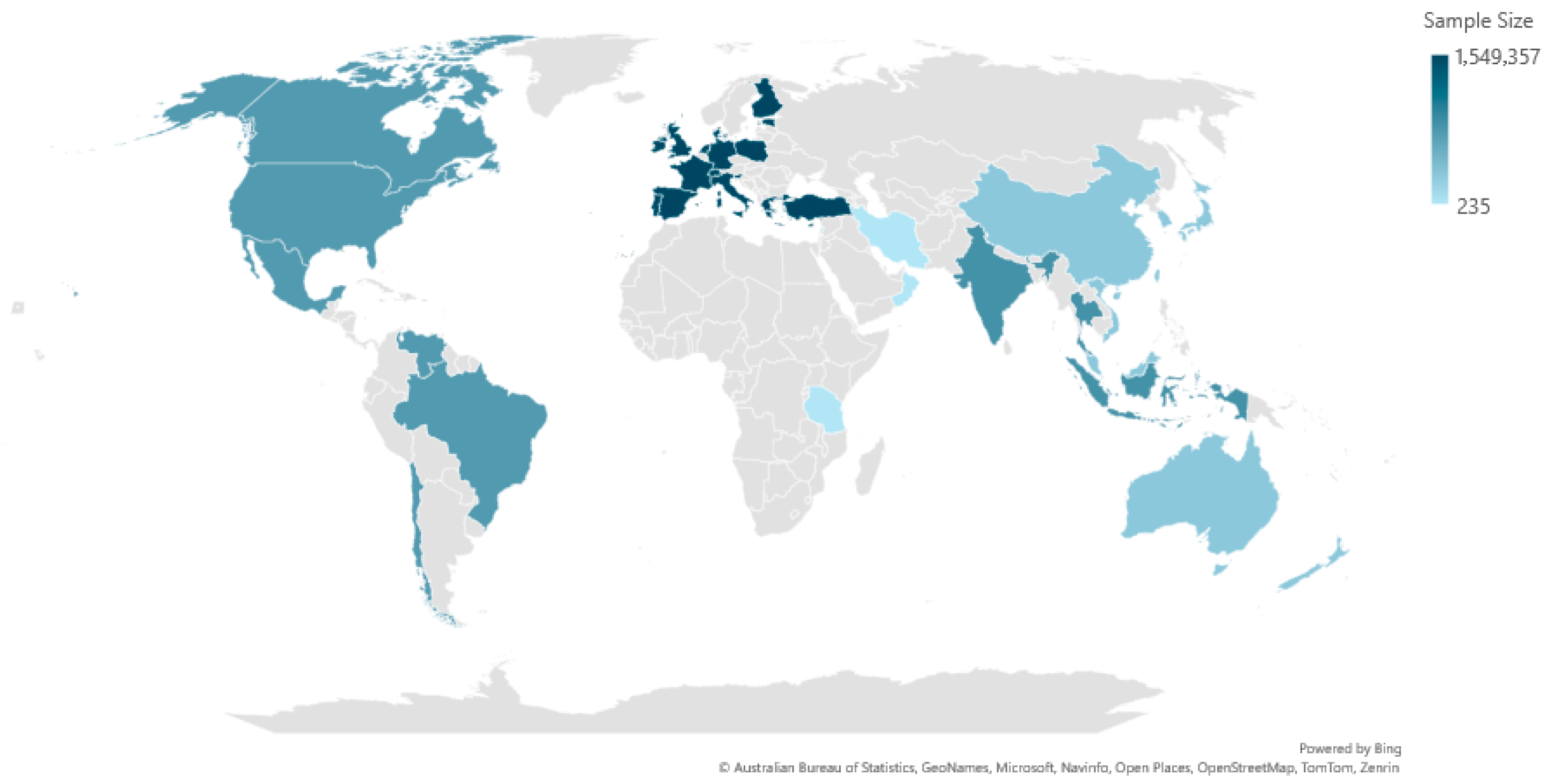
3.1. Characteristics of Included Studies
3.2. Prevalence of Frailty
3.3. Medication Use in Frailty
3.4. Prevalence of Polypharmacy and Hyper-Polypharmacy
3.5. Prevalence of PIMs in Older Adults Based on Frailty
3.6. Drug-Related Problems in Older Adults with Frailty
3.7. Impact of Medication Review on Polypharmacy Across Different Frailty Levels
3.8. Association Between Polypharmacy, Hyper-Polypharmacy, Medication Use, PIMs, and Frailty
3.8.1. Association Between Polypharmacy and Frailty
3.8.2. Association Between Hyper-Polypharmacy and Frailty
3.8.3. Association Between Medication Use and Frailty
3.8.4. Association Between PIMs and Frailty
3.9. Recommendations for Addressing Drug-Related Problems (DRPs) in Older Adults with Frailty
3.9.1. Comprehensive Medication Review and Deprescribing
3.9.2. Pharmacist-Led Deprescribing Reviews
3.9.3. Interdisciplinary Team Approaches
3.9.4. Deprescribing Tools and Criteria
3.9.5. Multifactorial Interventions
4. Discussion
4.1. Variability in Frailty Prevalence
4.2. Medication Use and Frailty
4.3. Potentially Inappropriate Medications (PIMs)
4.4. Association Between Medication Use, Polypharmacy, and DRPs with Frailty and Its Implications
4.5. Recommendations for Addressing DRPs
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 15 July 2024).
- Government of Canada, Statistics Canada. A Portrait of Canada’s Growing Population Aged 85 and Older from the 2021 Census. 27 April 2022. Available online: https://www12.statcan.gc.ca/census-recensement/2021/as-sa/98-200-X/2021004/98-200-X2021004-eng.cfm (accessed on 15 July 2024).
- Fillenbaum, G.G.; Pieper, C.F.; Cohen, H.J.; Cornoni-Huntley, J.C.; Guralnik, J.M. Comorbidity of five chronic health conditions in elderly community residents: Determinants and impact on mortality. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2000, 55, M84–M89. [Google Scholar] [CrossRef]
- Roberts, K.C.; Rao, D.P.; Bennett, T.L.; Loukine, L.; Jayaraman, G.C. Prevalence and patterns of chronic disease multimorbidity and associated determinants in Canada. Health promotion and chronic disease prevention in Canada: Research, policy and practice. Health Promot. Chronic Dis. Prev. Can. 2015, 35, 87–94. [Google Scholar] [CrossRef]
- Tam, T. Aging and Chronic Diseases: A Profile of Canadian Seniors; Government of Canada: Ottawa, ON, Canada, 2020. [Google Scholar]
- Levers, M.; Estabrooks, C.A.; Kerr, J.C.R. Factors contributing to frailty: Literature review. J. Adv. Nurs. 2006, 56, 282–291. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. Ser. A 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Feng, Z.; Lugtenberg, M.; Franse, C.; Fang, X.; Hu, S.; Jin, C.; Raat, H. Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: A systematic review of longitudinal studies. PLoS ONE 2017, 12, e0178383. [Google Scholar] [CrossRef]
- Gobbens, R.J.J.; Luijkx, K.G.; Wijnen-Sponselee, M.T.; Schols, J.M.G.A. Towards an integral conceptual model of frailty. J. Nutr. Health Aging 2010, 14, 175–181. [Google Scholar] [CrossRef]
- Kaufman, S.R. The social construction of frailty: An anthropological perspective. J. Aging Stud. 1994, 8, 45–58. [Google Scholar] [CrossRef]
- Sciacchitano, S.; Carola, V.; Nicolais, G.; Sciacchitano, S.; Napoli, C.; Mancini, R.; Rocco, M.; Coluzzi, F. To be frail or not to be frail: This is the question—A critical narrative review of frailty. J. Clin. Med. 2024, 13, 721. [Google Scholar] [CrossRef]
- Fulop, T.; Larbi, A.; Witkowski, J.M.; McElhaney, J.; Loeb, M.; Mitnitski, A.; Pawelec, G. Aging, frailty and age-related diseases. Biogerontology 2010, 11, 547–563. [Google Scholar] [CrossRef]
- Schulz, R.; Sherwood, P.R. Physical and mental health effects of family caregiving. J. Soc. Work. Educ. 2008, 44 (Suppl. S3), 105–113. [Google Scholar] [CrossRef]
- O’caoimh, R.; McGauran, J.; O’donovan, M.R.; Gillman, C.; O’hea, A.; Hayes, M.; O’connor, K.; Moloney, E.; Alcock, M. Frailty screening in the emergency department: Comparing the variable indicative of placement risk, clinical frailty scale and PRISMA-7. Int. J. Environ. Res. Public Health 2022, 20, 290. [Google Scholar] [CrossRef]
- Lunenfeld, B.; Stratton, P. The clinical consequences of an ageing world and preventive strategies. Best. Pract. Res. Clin. Obstet. Gynaecol. 2013, 27, 643–659. [Google Scholar] [CrossRef]
- Canadian Frailty Network. AVOID Frailty. Available online: https://www.cfn-nce.ca/frailty-matters/avoid-frailty/#:~:text=Over%201.6%20million%20older%20Canadians,older%20adults%20living%20with%20frailty (accessed on 15 July 2024).
- Matos, A.D.; Barbosa, F.; Cunha, C.; Voss, G.; Correia, F. Social isolation, physical inactivity and inadequate diet among European middle-aged and older adults. BMC Public Health 2021, 21, 924. [Google Scholar] [CrossRef] [PubMed]
- Ofori-Asenso, R.; Chin, K.L.; Mazidi, M.; Zomer, E.; Ilomaki, J.; Zullo, A.R.; Gasevic, D.; Ademi, Z.; Korhonen, M.J.; LoGiudice, D.; et al. Global incidence of frailty and prefrailty among community-dwelling older adults: A systematic review and meta-analysis. JAMA Netw. Open 2019, 2, e198398. [Google Scholar] [CrossRef]
- Toh, J.J.Y.; Zhang, H.; Soh, Y.Y.; Zhang, Z.; Wu, X.V. Prevalence and health outcomes of polypharmacy and hyperpolypharmacy in older adults with frailty: A systematic review and meta-analysis. Ageing Res. Rev. 2023, 83, 101811. [Google Scholar] [CrossRef]
- Hubbard, R.E.; O’mahony, M.S.; Woodhouse, K.W. Medication prescribing in frail older people. Eur. J. Clin. Pharmacol. 2013, 69, 319–326. [Google Scholar] [CrossRef]
- Akkawi, M.E.; Aziz, H.H.A.; Nahas, A.R.F. The impact of potentially inappropriate medications and polypharmacy on 3-month hospital readmission among older patients: A retrospective cohort study from Malaysia. Geriatrics 2023, 8, 49. [Google Scholar] [CrossRef]
- Beckman, A.; Bernsten, C.; Parker, M.G.; Thorslund, M.; Fastbom, J. The difficulty of opening medicine containers in old age: A population-based study. Pharm. World Sci. 2005, 27, 393–398. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Aprahamian, I.; Biella, M.M.; De Almeida, G.V.A.; Pegoraro, F.; Pedrini, A.V.A.; Cestari, B.; Bignotto, L.H.; De Melo, B.A.R.; Martinelli, J.E. Polypharmacy but not potential inappropriate prescription was associated with frailty in older adults from a middle-income country outpatient clinic. J. Frailty Aging 2018, 7, 108–112. [Google Scholar] [CrossRef]
- Ye, L.; Yang-Huang, J.; Franse, C.B.; Rukavina, T.; Vasiljev, V.; Mattace-Raso, F.; Verma, A.; Borrás, T.A.; Rentoumis, T.; Raat, H. Factors associated with polypharmacy and the high risk of medication-related problems among older community-dwelling adults in European countries: A longitudinal study. BMC Geriatr. 2022, 22, 841. [Google Scholar] [CrossRef]
- Derhem, B.; Özsari, S. Frailty and Polypharmacy in Primary Care. Biol. Res. Nurs. 2023, 25, 658–663. [Google Scholar] [CrossRef]
- Pala, F.; Yalçin Gürsoy, M. Prevalence of Frailty and Related Factors Among Community-Dwelling Older Adults: A Cross-Sectional Study from Western Türkiye. Turk. Klin. J. Nurs. Sci. 2023, 15, 660–667. [Google Scholar] [CrossRef]
- Tchalla, A.; Laubarie-Mouret, C.; Cardinaud, N.; Gayot, C.; Rebiere, M.; Dumoitier, N.; Rudelle, K.; Druet-Cabanac, M.; Laroche, M.-L.; Boyer, S. Risk factors of frailty and functional disability in community-dwelling older adults: A cross-sectional analysis of the FREEDOM-LNA cohort study. BMC Geriatr. 2022, 22, 762. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Zúñiga, R.; Davis, J.R.; Ruddy, K.; De Looze, C.; Carey, D.; Meaney, J.; Kenny, R.A.; Knight, S.P.; Romero-Ortuno, R. Structural brain signatures of frailty, defined as accumulation of self-reported health deficits in older adults. Front. Aging Neurosci. 2023, 15, 1065191. [Google Scholar] [CrossRef]
- Santos, P.H.S.; dos Santos, L.; Fernandes, M.H.; Brito, T.A.; Munaro, H.L.R.; Carneiro, J.A.O. Factors associated with frailty syndrome in older adults with three-and four-criteria clustering. Geriatr. Nurs. 2023, 51, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Chaitoff, A.; Haff, N.; Lauffenburger, J.C.; Choudhry, N.K. Medication de-escalation opportunities among frail older adults with strictly-controlled cardiometabolic disease. J. Am. Geriatr. Soc. 2023, 71, 2655–2657. [Google Scholar] [CrossRef]
- Cox, N.; Ilyas, I.; Roberts, H.C.; Ibrahim, K. Exploring the prevalence and types of fall-risk-increasing drugs among older people with upper limb fractures. Int. J. Pharm. Pract. 2023, 31, 106–112. [Google Scholar] [CrossRef]
- Sobhani, A.; Sharifi, F.; Fadayevatan, R.; Kamrani, A.A.A.; Moodi, M.; Khorashadizadeh, M.; Kazemi, T.; Khodabakhshi, H.; Fakhrzadeh, H.; Arzaghi, M.; et al. Low physical activity is the strongest factor associated with frailty phenotype and frailty index: Data from baseline phase of Birjand Longitudinal Aging Study (BLAS). BMC Geriatr. 2022, 22, 498. [Google Scholar] [CrossRef]
- Mortsiefer, A.; Löscher, S.; Pashutina, Y.; Santos, S.; Altiner, A.; Drewelow, E.; Ritzke, M.; Wollny, A.; Thürmann, P.; Bencheva, V.; et al. Family conferences to facilitate deprescribing in older outpatients with Frailty and with polypharmacy: The COFRAIL Cluster Randomized trial. JAMA Netw. Open 2022, 6, e234723. [Google Scholar] [CrossRef]
- Kume, Y.; Kodama, A.; Takahashi, T.; Lee, S.; Makizako, H.; Ono, T.; Shimada, H.; Ota, H. Social frailty is independently associated with geriatric depression among older adults living in northern Japan: A cross-sectional study of ORANGE registry. Geriatr. Gerontol. Int. 2022, 22, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Kurnat-Thoma, E.L.; Murray, M.T.; Juneau, P. Frailty and determinants of health among older adults in the United States 2011–2016. J. Aging Health 2022, 34, 233–244. [Google Scholar] [CrossRef]
- de Sousa, C.R.; Coutinho, J.F.V.; Neto, J.B.F.; Barbosa, R.G.B.; Marques, M.B.; Diniz, J.L. Factors associated with vulnerability and fragility in the elderly: A cross-sectional study. Rev. Bras. Enferm. 2021, 75, e20200399. [Google Scholar] [CrossRef]
- Österdahl, M.F.; Sinnott, S.-J.; Douglas, I.; Clegg, A.; Tomlinson, L.; Wong, A. Frailty and rate of fractures in patients initiating antihypertensive medications: A cohort study in primary care. Drugs Ther. Perspect. 2022, 38, 41–50. [Google Scholar] [CrossRef]
- Thiruchelvam, K.; Byles, J.; Hasan, S.S.; Egan, N.; Kairuz, T. Prevalence and association of continuous polypharmacy and frailty among older women: A longitudinal analysis over 15 years. Maturitas 2021, 146, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Rhalimi, M.; Housieaux, E.; Mary, A.; Detuncq, C.; Muller, A.; Georgin, F.; Comby, F.; Wehrlé, C.; Davoust, N.; Brazier, M. Role of the community pharmacist in detecting frailty and spatio-temporal disorientation among community-dwelling older people in France. Aging Clin. Exp. Res. 2021, 33, 1645–1650. [Google Scholar] [CrossRef]
- Chen, M.Z.; Wong, M.W.K.; Lim, J.Y.; Merchant, R.A. Frailty and quality of life in older adults with metabolic syndrome—Findings from the healthy older people everyday (HOPE) study. J. Nutr. Health Aging 2021, 25, 637–644. [Google Scholar] [CrossRef]
- McKechnie, D.G.J.; Papacosta, A.O.; Lennon, L.T.; Ramsay, S.E.; Whincup, P.H.; Wannamethee, S.G. Associations between inflammation, cardiovascular biomarkers and incident frailty: The British Regional Heart Study. Age Ageing 2021, 50, 1979–1987. [Google Scholar] [CrossRef]
- Bonfiglio, V.; Umegaki, H.; Kuzuya, M. Potentially inappropriate medications and polypharmacy: A study of older people with mild cognitive impairment and mild dementia. J. Alzheimer’s Dis. 2019, 71, 889–897. [Google Scholar] [CrossRef]
- Bolina, A.F.; Gomes, N.C.; Marchiori, G.F.; Pegorari, M.S.; Tavares, D.M.d.S. Potentially inappropriate medication use and frailty phenotype among community-dwelling older adults: A population-based study. J. Clin. Nurs. 2019, 28, 3914–3922. [Google Scholar] [CrossRef]
- Moon, J.H.; Huh, J.S.; Won, C.W.; Kim, H.J. Is polypharmacy associated with cognitive frailty in the elderly? Results from the Korean frailty and aging cohort study. J. Nutr. Health Aging 2019, 23, 958–965. [Google Scholar] [CrossRef]
- Saum, K.; Schöttker, B.; Meid, A.D.; Holleczek, B.; Haefeli, W.E.; Hauer, K.; Brenner, H. Is polypharmacy associated with frailty in older people? Results from the ESTHER cohort study. J. Am. Geriatr. Soc. 2017, 65, e27–e32. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.; Nieboer, D.; Yang-Huang, J.; Borrás, T.A.; Garcés-Ferrer, J.; Verma, A.; van Grieken, A.; Raat, H. The association between frailty and the risk of medication-related problems among community-dwelling older adults in Europe. J. Am. Geriatr. Soc. 2023, 71, 2485–2494. [Google Scholar] [CrossRef]
- Thiruchelvam, K.; Byles, J.; Hasan, S.S.; Egan, N.; Kairuz, T. Frailty and potentially inappropriate medications using the 2019 Beers Criteria: Findings from the Australian Longitudinal Study on Women’s Health (ALSWH). Aging Clin. Exp. Res. 2021, 33, 2499–2509. [Google Scholar] [CrossRef] [PubMed]
- Callahan, K.E.; Lenoir, K.M.; Usoh, C.O.; Williamson, J.D.; Brown, L.Y.; Moses, A.W.; Hinely, M.; Neuwirth, Z.; Pajewski, N.M. Using an Electronic Health Record and Deficit Accumulation to Pragmatically Identify Candidates for Optimal Prescribing in Patients With Type 2 Diabetes. Diabetes Spectr. 2022, 35, 344–350. [Google Scholar] [CrossRef]
- Muhlack, D.C.; Hoppe, L.K.; Saum, K.-U.; Haefeli, W.E.; Brenner, H.; Schöttker, B. Investigation of a possible association of potentially inappropriate medication for older adults and frailty in a prospective cohort study from Germany. Age Ageing 2020, 49, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Muhlack, D.C.; Hoppe, L.K.; Stock, C.; Haefeli, W.E.; Brenner, H.; Schöttker, B. The associations of geriatric syndromes and other patient characteristics with the current and future use of potentially inappropriate medications in a large cohort study. Eur. J. Clin. Pharmacol. 2018, 74, 1633–1644. [Google Scholar] [CrossRef]
- Bergen, A.W.; Cil, G.; Sargent, L.J.; Dave, C.V. Frailty risks of prescription analgesics and sedatives across frailty models: The health and retirement study. Drugs Aging 2022, 39, 377–387. [Google Scholar] [CrossRef]
- Ekram, A.R.M.S.; Woods, R.L.; Ryan, J.; Espinoza, S.E.; Gilmartin-Thomas, J.F.; Shah, R.C.; Mehta, R.; Kochar, B.; Lowthian, J.A.; Lockery, J.; et al. The association between polypharmacy, frailty and disability-free survival in community-dwelling healthy older individuals. Arch. Gerontol. Geriatr. 2022, 101, 104694. [Google Scholar] [CrossRef]
- Sargent, L.; Nalls, M.; Amella, E.J.; Mueller, M.; Lageman, S.K.; Bandinelli, S.; Colpo, M.; Slattum, P.W.; Singleton, A.; Ferrucci, L. Anticholinergic drug induced cognitive and physical impairment: Results from the InCHIANTI study. J. Gerontol. Ser. A 2020, 75, 995–1002. [Google Scholar] [CrossRef]
- Naharci, M.I.; Tasci, I. Frailty status and increased risk for falls: The role of anticholinergic burden. Arch. Gerontol. Geriatr. 2020, 90, 104136. [Google Scholar] [CrossRef]
- Larsen, R.T.; Turcotte, L.A.; Westendorp, R.; Langberg, H.; Hirdes, J.P. Frailty index status of Canadian home care clients improves with exercise therapy and declines in the presence of polypharmacy. J. Am. Med. Dir. Assoc. 2020, 21, 766–771.e1. [Google Scholar] [CrossRef]
- Uragami, Y.; Takikawa, K.; Kareki, H.; Kimura, K.; Yamamoto, K.; Iihara, N. Effect of number of medications and use of potentially inappropriate medications on frailty among early-stage older outpatients. J. Pharm. Health Care Sci. 2021, 7, 15. [Google Scholar] [CrossRef]
- Midão, L.; Brochado, P.; Almada, M.; Duarte, M.; Paúl, C.; Costa, E. Frailty status and polypharmacy predict all-cause mortality in community dwelling older adults in Europe. Int. J. Environ. Res. Public Health 2021, 18, 3580. [Google Scholar] [CrossRef] [PubMed]
- Jazbar, J.; Locatelli, I.; Kos, M. The association between medication or alcohol use and the incidence of frailty: A retrospective cohort study. BMC Geriatr. 2021, 21, 25. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Jang, S.Y.; Cheong, H.-K.; Oh, I.-H. Association of frailty with healthcare costs using claims data in Korean older adults aged 66. J. Nutr. Health Aging 2021, 25, 653–659. [Google Scholar] [CrossRef]
- Gulliford, M.; Ravindrarajah, R.; Hamada, S.; Jackson, S.; Charlton, J. Inception and deprescribing of statins in people aged over 80 years: Cohort study. Age Ageing 2017, 46, 1001–1005. [Google Scholar] [CrossRef]
- Jamsen, K.M.; Bell, J.S.; Hilmer, S.N.; Kirkpatrick, C.M.J.; Ilomäki, J.; Le Couteur, D.; Blyth, F.M.; Handelsman, D.J.; Waite, L.; Naganathan, V.; et al. Effects of changes in number of medications and drug burden index exposure on transitions between frailty states and death: The concord health and ageing in men project cohort study. J. Am. Geriatr. Soc. 2016, 64, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, T.G.; Silva, K.R.; Guerra, R.O.; Parente, R.C.P.; Borges, G.F.; Junior, R.C.F. Influence of the Amazonian context on the frailty of older adults: A population-based study. Arch. Gerontol. Geriatr. 2021, 93, 104162. [Google Scholar] [CrossRef]
- Coelho, T.; Paúl, C.; Gobbens, R.J.J.; Fernandes, L. Determinants of frailty: The added value of assessing medication. Front. Aging Neurosci. 2015, 7, 56. [Google Scholar] [CrossRef]
- Martinot, P.; Landré, B.; Zins, M.; Goldberg, M.; Ankri, J.; Herr, M. Association between potentially inappropriate medications and frailty in the early old age: A longitudinal study in the GAZEL cohort. J. Am. Med. Dir. Assoc. 2018, 19, 967–973.e3. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Chong, J.; Jung, H.-W.; Baek, J.Y.; Lee, E.; Jang, I.-Y. Association of the FRAIL scale with geriatric syndromes and health-related outcomes in Korean older adults. Ann. Geriatr. Med. Res. 2021, 25, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Kume, Y.; Takahashi, T.; Itakura, Y.; Lee, S.; Makizako, H.; Ono, T.; Shimada, H.; Ota, H. Polypharmacy and lack of joy are related to physical frailty among Northern Japanese community-dwellers from the ORANGE cohort study. Gerontology 2021, 67, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, J.A.; Souza, A.S.; Maia, L.C.; Costa, F.M.; Moraes, E.N.; Caldeira, A.P. Frailty in community-dwelling older people: Comparing screening instruments. Rev. Saude Publica 2020, 54, 119. [Google Scholar] [CrossRef] [PubMed]
- Lockery, J.E.; Ernst, M.E.; Broder, J.C.; Orchard, S.G.; Murray, A.; Nelson, M.R.; Stocks, N.P.; Wolfe, R.; Reid, C.M.; Liew, D.; et al. Prescription medication use in older adults without major cardiovascular disease enrolled in the aspirin in reducing events in the elderly (ASPREE) clinical trial. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2020, 40, 1042–1053. [Google Scholar] [CrossRef]
- Alves, M.K.L.; Oliveira, N.G.N.; Pegorari, M.S.; Tavares, D.M.d.S.; Rodrigues, M.C.S.; Bolina, A.F. Evidence of association between the use of drugs and community-dwelling older people frailty: A cross-sectional study. Sao Paulo Med. J. 2020, 138, 465–474. [Google Scholar] [CrossRef]
- Braun, T.; Thiel, C.; Ziller, C.; Rasche, J.; Bahns, C.; Happe, L.; Retzmann, T.; Grüneberg, C. Prevalence of frailty in older adults in outpatient physiotherapy in an urban region in the western part of Germany: A cross-sectional study. BMJ Open 2019, 9, e027768. [Google Scholar] [CrossRef]
- Huang, C.H.; Lai, Y.-C.; Lee, Y.C.; Teong, X.T.; Kuzuya, M.; Kuo, K.-M. Impact of health literacy on frailty among community-dwelling seniors. J. Clin. Med. 2018, 7, 481. [Google Scholar] [CrossRef]
- Fhon, J.R.; Rodrigues, R.A.; Santos, J.L.; Diniz, M.A.; Santos, E.B.; Almeida, V.C.; Giacomini, S.B. Factors associated with frailty in older adults: A longitudinal study. Rev. Saude Publica 2018, 52, 74. [Google Scholar] [CrossRef]
- Ballew, S.H.; Chen, Y.; Daya, N.R.; Godino, J.G.; Windham, B.G.; McAdams-DeMarco, M.; Coresh, J.; Selvin, E.; Grams, M.E. Frailty, kidney function, and polypharmacy: The atherosclerosis risk in communities (ARIC) study. Am. J. Kidney Dis. 2017, 69, 228–236. [Google Scholar] [CrossRef] [PubMed]
- König, M.; Spira, D.; Demuth, I.; Steinhagen-Thiessen, E.; Norman, K. Polypharmacy as a risk factor for clinically relevant sarcopenia: Results from the Berlin Aging Study II. J. Gerontol. Ser. A 2018, 73, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Closs, V.E.; Ziegelmann, P.K.; da Silva Filho, I.G.; Schwanke, C.H.A. Frailty and geriatric syndromes in elderly assisted in primary health care. Acta Sci. Health Sci. 2016, 38, 9–18. [Google Scholar] [CrossRef]
- Jankowska-Polańska, B.; Dudek, K.; Szymanska-Chabowska, A.; Uchmanowicz, I. The influence of frailty syndrome on medication adherence among elderly patients with hypertension. Clin. Interv. Aging 2016, 11, 1781–1790. [Google Scholar] [CrossRef]
- Verloo, H.; Goulet, C.; Morin, D.; von Gunten, A. Association between frailty and delirium in older adult patients discharged from hospital. Clin. Interv. Aging 2016, 11, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.-W.; Jang, I.-Y.; Lee, Y.S.; Lee, C.K.; Cho, E.-I.; Kang, W.Y.; Chae, J.H.; Lee, E.J.; Kim, D.H. Prevalence of frailty and aging-related health conditions in older Koreans in rural communities: A cross-sectional analysis of the aging study of Pyeongchang rural area. J. Korean Med. Sci. 2016, 31, 345–352. [Google Scholar] [CrossRef]
- Çakmur, H. Frailty among elderly adults in a rural area of Turkey. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2015, 21, 1232. [Google Scholar] [CrossRef]
- Wang, R.; Chen, L.; Fan, L.; Gao, D.; Liang, Z.; He, J.; Gong, W.; Gao, L. Incidence and effects of polypharmacy on clinical outcome among patients aged 80+: A five-year follow-up study. PLoS ONE 2015, 10, e0142123. [Google Scholar] [CrossRef]
- Gnjidic, D.; Hilmer, S.N.; Blyth, F.M.; Naganathan, V.; Cumming, R.G.; Handelsman, D.J.; McLachlan, A.J.; Abernethy, D.R.; Banks, E.; Le Couteur, D.G. High-risk prescribing and incidence of frailty among older community-dwelling men. Clin. Pharmacol. Ther. 2012, 91, 521–528. [Google Scholar] [CrossRef]
- Correa Miguel, R.d.C.; Dias, R.C.; Domingues Dias, J.M.; Azevedo da Silva, S.L.; Menicucci Filho, P.R.; Ribeiro, T.M.S. Frailty syndrome in the community-dwelling elderly with osteoarthritis. Rev. Bras. Reumatol. 2012, 52, 339–347. [Google Scholar]
- Rodríguez-Laso, Á.; García-García, F.J.; Rodríguez-Mañas, L. Predictors of Maintained Transitions Between Robustness and Prefrailty in Community-Dwelling Older Spaniards. J. Am. Med. Dir. Assoc. 2023, 24, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, A.D.; Reiners, A.A.; Azevedo, R.C.; Silva, K.M.; Silva, A.M. Pre-frailty in older adults: Prevalence and associated factors. Texto Contexto-Enferm. 2022, 31, e20210157. [Google Scholar] [CrossRef]
- Chen, Y.-Z.; Huang, S.-T.; Wen, Y.-W.; Chen, L.-K.; Hsiao, F.-Y. Combined effects of frailty and polypharmacy on health outcomes in older adults: Frailty outweighs polypharmacy. J. Am. Med. Dir. Assoc. 2021, 22, 606.e7–606.e18. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Sok, S.R.; Won, C.W. Factors affecting frailty among community-dwelling older adults: A multi-group path analysis according to nutritional status. Int. J. Nurs. Stud. 2021, 115, 103850. [Google Scholar] [CrossRef]
- Lewis, E.G.; Whitton, L.A.; Collin, H.; Urasa, S.; Howorth, K.; Walker, R.W.; Dotchin, C.; Mulligan, L.; Shah, B.; Mohamed, A.; et al. A brief frailty screening tool in Tanzania: External validation and refinement of the B-FIT screen. Aging Clin. Exp. Res. 2020, 32, 1959–1967. [Google Scholar] [CrossRef]
- Khera, S.; Abbasi, M.; Dabravolskaj, J.; Sadowski, C.A.; Yua, H.; Chevalier, B. Appropriateness of medications in older adults living with frailty: Impact of a pharmacist-led structured medication review process in primary care. J. Prim. Care Community Health 2019, 10, 2150132719890227. [Google Scholar] [CrossRef]
- Tampaki, M.; Livada, A.; Fourka, M.-N.; Lazaridou, E.; Kotsani, M.; Benetos, A.; Sfikakis, P.P.; Kravvariti, E. Inappropriate prescribing in geriatric rural primary care: Impact on adverse outcomes and relevant risk factors in a prospective observational cohort study. Aging Clin. Exp. Res. 2023, 35, 1901–1907. [Google Scholar] [CrossRef]
- Nishtala, P.S.; Pickering, J.W.; Bergler, U.; Mangin, D.; Hilmer, S.N.; Jamieson, H. Post Hoc Analyses of a Randomized Controlled Trial for the Effect of Pharmacist Deprescribing Intervention on the Anticholinergic Burden in Frail Community-Dwelling Older Adults. J. Am. Med. Dir. Assoc. 2023, 24, 1253–1260. [Google Scholar] [CrossRef]
- Fravel, M.A.; Ernst, M.E.; Gilmartin-Thomas, J.; Woods, R.L.; Orchard, S.G.; Owen, A.J.; The ASPirin in Reducing Events in the Elderly Investigator Group ASPirin in Reducing Events in the Elderly Investigator Group. Dietary supplement and complementary and alternative medicine use among older adults in Australia and the United States. J. Am. Geriatr. Soc. 2023, 71, 2219–2228. [Google Scholar] [CrossRef]
- Daou, T.; Kharma, J.A.; Daccache, A.; Bassil, M.; Naja, F.; Rahi, B. Association between Lebanese Mediterranean Diet and Frailty in Community-Dwelling Lebanese Older Adults—A Preliminary Study. Nutrients 2022, 14, 3084. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Zhou, X.; Liu, W.; Ma, Q.; Deng, X.; Fang, R. Evaluation of the correlation between frailty and sleep quality among elderly patients with osteoporosis: A cross-sectional study. BMC Geriatr. 2022, 22, 599. [Google Scholar] [CrossRef]
- Molist-Brunet, N.; Sevilla-Sánchez, D.; Puigoriol-Juvanteny, E.; Barneto-Soto, M.; González-Bueno, J.; Espaulella-Panicot, J. Improving individualized prescription in patients with multimorbidity through medication review. BMC Geriatr. 2022, 22, 417. [Google Scholar] [CrossRef]
- Thiruchelvam, K.; Byles, J.; Hasan, S.S.; Egan, N.; Kairuz, T. Home Medicines Review and frailty among community-dwelling older women. Int. J. Pharm. Pract. 2021, 29, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Brown, P.J.; Ciarleglio, A.; Roose, S.P.; Garcia, C.M.; Chung, S.; Fernandes, S.; Rutherford, B.R. Frailty and depression in late life: A high-risk comorbidity with distinctive clinical presentation and poor antidepressant response. J. Gerontol. Ser. A 2021, 77, 1055–1062. [Google Scholar] [CrossRef]
- Mejías-Trueba, M.; Rodríguez-Pérez, A.; Sotillo-Sánchez, I.; Sánchez-Fidalgo, S.; Nieto-Martin, M.D.; García-Cabrera, E. Prevalence of potentially inappropriate medications in patients with multimorbidity according to LESS-CHRON and STOPPFrail Criteria. J. Am. Med. Dir. Assoc. 2023, 24, 511–516.e3. [Google Scholar] [CrossRef]
- Salaffi, F.; Di Carlo, M.; Carotti, M.; Farah, S.; Giovagnoni, A. Frailty prevalence according to the Survey of Health, Ageing and Retirement in Europe-Frailty Instrument (SHARE-FI) definition, and its variables associated, in patients with symptomatic knee osteoarthritis: Findings from a cross-sectional study. Aging Clin. Exp. Res. 2021, 33, 1519–1527. [Google Scholar] [CrossRef]
- Cheung, J.T.K.; Yu, R.; Woo, J. Is polypharmacy beneficial or detrimental for older adults with cardiometabolic multimorbidity? Pooled analysis of studies from Hong Kong and Europe. Fam. Pract. 2020, 37, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Ambagtsheer, R.C.; Visvanathan, R.; Dent, E.; Yu, S.; Schultz, T.J.; Beilby, J.M.D. Commonly used screening instruments to identify frailty among community-dwelling older people in a general practice (primary care) setting: A study of diagnostic test accuracy. J. Gerontol. Ser. A 2020, 75, 1134–1142. [Google Scholar] [CrossRef]
- Sheppard, J.P.; Burt, J.; Lown, M.; Temple, E.; Lowe, R.; Fraser, R.; Allen, J.; Ford, G.A.; Heneghan, C.; Hobbs, F.R.; et al. Effect of antihypertensive medication reduction vs usual care on short-term blood pressure control in patients with hypertension aged 80 years and older: The OPTIMISE randomized clinical trial. JAMA 2020, 323, 2039–2051. [Google Scholar] [CrossRef]
- Cil, G.; Park, J.; Bergen, A.W. Self-reported prescription drug use for pain and for sleep and incident frailty. J. Am. Geriatr. Soc. 2019, 67, 2474–2481. [Google Scholar] [CrossRef] [PubMed]
- Reallon, E.; Chavent, B.; Gervais, F.; Dauphinot, V.; Vernaudon, J.; Krolak-Salmon, P.; Mouchoux, C.; Novais, T. Medication exposure and frailty in older community-dwelling patients: A cross-sectional study. Pharm. Weekbl. 2020, 42, 508–514. [Google Scholar] [CrossRef]
- Rieckert, A.; Trampisch, U.S.; Klaaßen-Mielke, R.; Drewelow, E.; Esmail, A.; Johansson, T.; Keller, S.; Kunnamo, I.; Löffler, C.; Mäkinen, J.; et al. Polypharmacy in older patients with chronic diseases: A cross-sectional analysis of factors associated with excessive polypharmacy. BMC Fam. Pract. 2018, 19, 113. [Google Scholar] [CrossRef]
- Öztürk, Y.; Cömertoğlu, E.O.; Hafızoğlu, M.; Kahyaoğlu, Z.; Çavuşoğlu, Ç.; Balcı, C.; Doğu, B.B.; Halil, M.; Aki, Ö.E.; Cankurtaran, M. The Relationship Between Polypharmacy and Geropsychiatric Assessment Scales in Geriatric Outpatients. Eur. J. Geriatr. Gerontol. 2023, 5, 225–230. [Google Scholar] [CrossRef]
- Fikree, S.; Hafid, S.; Lawson, J.; Agarwal, G.; Griffith, L.E.; Jaakkimainen, L.; Mangin, D.; Howard, M. The association between patients’ frailty status, multimorbidity, and demographic characteristics and changes in primary care for chronic conditions during the COVID-19 pandemic: A pre-post study. Fam. Pract. 2023, 40, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Vendola, M.C.C.; Jacob-Filho, W. Impact of oral health on frailty syndrome in frail older adults. Einstein 2023, 21, eAO0103. [Google Scholar] [CrossRef] [PubMed]
- Badrkhahan, S.Z.; Ala, M.; Fakhrzadeh, H.; Yaghoobi, A.; Mirzamohamadi, S.; Arzaghi, S.M.; Shahabi, S.; Sharifi, F.; Ostovar, A.; Fahimfar, N.; et al. The prevalence and predictors of geriatric giants in community-dwelling older adults: A cross-sectional study from the Middle East. Sci. Rep. 2023, 13, 12401. [Google Scholar] [CrossRef]
- Dixe, M.d.A.; Pinho, J.; Pereira, F.; Verloo, H.; Meyer-Massetti, C.; Pereira, S.G. Patterns of medication management and associated medical and clinical features among home-dwelling older adults: A cross-sectional study in Central Portugal. Int. J. Environ. Res. Public Health 2023, 20, 1701. [Google Scholar] [CrossRef]
- Salazar, J.; Borges, I.; Rivas-Motenegro, A.; Villasmil-Hernandez, N.; Nava, M.; Añez, R. Association of Newly Diagnosed Hypertension and Polypharmacy with Frailty in a Tertiary Hospital Patients from Maracaibo City, Venezuela. Curr. Hypertens. Rev. 2022, 18, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Kinoshita, K.; Satake, S.; Murotani, K.; Takemura, M.; Matsui, Y.; Arai, H. Physical frailty and hemoglobin-to-red cell distribution width ratio in Japanese older outpatients. J. Frailty Aging 2022, 11, 393–397. [Google Scholar] [CrossRef]
- Dautzenberg, L.; van Aarle, T.T.M.; Stella, P.R.; Emmelot-Vonk, M.; Weterman, M.A.; Koek, H.L. The impact of frailty on adverse outcomes after transcatheter aortic valve replacement in older adults: A retrospective cohort study. Catheter. Cardiovasc. Interv. 2022, 100, 439–448. [Google Scholar] [CrossRef]
- Ribeiro, É.C.T.; Sangali, T.D.; Clausell, N.O.; Perry, I.S.; Souza, G.C. C-reactive protein and frailty in heart failure. Am. J. Cardiol. 2022, 166, 65–71. [Google Scholar] [CrossRef]
- Pilleron, S.; Le Goff, M.; Ajana, S.; Helmer, C.; Pérès, K.; Dartigues, J.-F.; Tabue-Teguo, M.; Féart, C. Self-rated health and frailty in older adults from the population-based three-city bordeaux cohort. Gerontology 2022, 68, 755–762. [Google Scholar] [CrossRef]
- Molino, C.d.G.R.C.; Chocano-Bedoya, P.O.; Sadlon, A.; Theiler, R.; Orav, J.E.; Vellas, B.; Rizzoli, R.; Kressig, R.W.; Kanis, J.A.; Guyonnet, S.; et al. Prevalence of polypharmacy in community-dwelling older adults from seven centres in five European countries: A cross-sectional study of DO-HEALTH. BMJ Open 2022, 12, e051881. [Google Scholar] [CrossRef]
- Álvarez-Bustos, A.; Carnicero-Carreño, J.A.; Sanchez-Sanchez, J.L.; Garcia-Garcia, F.J.; Alonso-Bouzón, C.; Rodríguez-Mañas, L. Associations between frailty trajectories and frailty status and adverse outcomes in community-dwelling older adults. J. Cachexia Sarcopenia Muscle 2022, 13, 230–239. [Google Scholar] [CrossRef] [PubMed]
- O’dOnoghue, P.J.; Claffey, P.; Rice, C.; Byrne, L.; Cunningham, C.; Kenny, R.A.; Romero-Ortuno, R. Association between gait speed and the SHARE Frailty Instrument in a Falls and Syncope Clinic. Eur. Geriatr. Med. 2021, 12, 1101–1105. [Google Scholar] [CrossRef] [PubMed]
- Houghton, J.S.; Nickinson, A.T.; Helm, J.R.; Dimitrova, J.; Dubkova, S.; Rayt, H.S.; Gray, L.J.; Haunton, V.J.; Davies, R.S.; Sayers, R.D. Associations of clinical frailty with severity of limb threat and outcomes in chronic limb-threatening ischaemia. Ann. Vasc. Surg. 2021, 76, 406–416. [Google Scholar] [CrossRef] [PubMed]
- de Breij, S.; van Hout, H.P.; De Bruin, S.R.; Schuster, N.A.; Deeg, D.J.; Huisman, M.; Hoogendijk, E.O. Predictors of frailty and vitality in older adults aged 75 years and over: Results from the longitudinal aging study Amsterdam. Gerontology 2021, 67, 69–77. [Google Scholar] [CrossRef]
- Jung, H.; Kim, M.; Lee, Y.; Won, C.W. Prevalence of physical frailty and its multidimensional risk factors in Korean community-dwelling older adults: Findings from Korean frailty and aging cohort study. Int. J. Environ. Res. Public Health 2020, 17, 7883. [Google Scholar] [CrossRef]
- Arauna, D.; Cerda, A.; Garcia-García, J.F.; Wehinger, S.; Castro, F.; Méndez, D.; Alarcón, M.; Fuentes, E.; Palomo, I. Polypharmacy is associated with frailty, nutritional risk and chronic disease in chilean older adults: Remarks from piei-es study. Clin. Interv. Aging 2020, 15, 1013–1022. [Google Scholar] [CrossRef]
- O’COnnell, J.; Henman, M.C.; McMahon, N.; Burke, É.; McCallion, P.; McCarron, M.; O’DWyer, M. Medication burden and frailty in older adults with intellectual disability: An observational cross-sectional study. Pharmacoepidemiol. Drug Saf. 2020, 29, 482–492. [Google Scholar] [CrossRef]
- Doğan Varan, H.A.; Kilic, M.; Kizilarslanoğlu, M.; Tuna Doğrul, R.; Arik, G.; Kara, O.; Güner, G.; Şengül Ayçiçek, G.; Can, B.; Halil, M.; et al. Frailty and its correlates in older adults: A challenging and preventable geriatric syndrome. Erciyes Med. J. 2020, 42, 150. [Google Scholar] [CrossRef]
- Mino-León, D.; Sánchez-García, S.; Giraldo-Rodríguez, L.; Reyes-Morales, H. Potentially inappropriate prescribing to older adults in ambulatory care: Prevalence and associated patient conditions. Eur. Geriatr. Med. 2019, 10, 639–647. [Google Scholar] [CrossRef]
- Huguet, L.G.; González, M.N.; Kostov, B.; Carmona, M.O.; Francia, C.C.; Nieto, M.C.; Docón, A.H.; Sauquet, R.V.; Prado, R.G.; Sisó-Almirall, A. Pre frail 80: Multifactorial intervention to prevent progression of pre-frailty to frailty in the elderly. J. Nutr. Health Aging 2018, 22, 1266–1274. [Google Scholar] [CrossRef]
- Hasan, S.S.; Liew, A.S.C.; Chong, D.W.K.; Thiruchelvam, K.; Babar, Z.-U. Associations between Drug Burden Index, medication appropriateness and patient-reported outcomes in the community pharmacy setting in Malaysia. Drugs Ther. Perspect. 2018, 34, 437–443. [Google Scholar] [CrossRef]
- Yuki, A.; Otsuka, R.; Tange, C.; Nishita, Y.; Tomida, M.; Ando, F.; Shimokata, H. Polypharmacy is associated with frailty in Japanese community-dwelling older adults. Geriatr. Gerontol. Int. 2018, 18, 1497–1500. [Google Scholar] [CrossRef]
- Rhalimi, M.; Rauss, A.; Housieaux, E. Drug-related problems identified during geriatric medication review in the community pharmacy. Pharm. Weekbl. 2018, 40, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Hoeksema, A.; Spoorenberg, S.; Peters, L.; Meijer, H.; Raghoebar, G.; Vissink, A.; Wynia, K.; Visser, A. Elderly with remaining teeth report less frailty and better quality of life than edentulous elderly: A cross-sectional study. Oral Dis. 2017, 23, 526–536. [Google Scholar] [CrossRef]
- Shmuel, S.; Lund, J.L.; Alvarez, C.; Hsu, C.D.; Palta, P.; Kucharska-Newton, A.; Jordan, J.M.; Nelson, A.E.; Golightly, Y.M. Polypharmacy and incident frailty in a longitudinal community-based cohort study. J. Am. Geriatr. Soc. 2019, 67, 2482–2489. [Google Scholar] [CrossRef]
- Aznar-Tortonda, V.; Palazón-Bru, A.; la Rosa, D.M.F.-D.; Espínola-Morel, V.; Pérez-Pérez, B.F.; León-Ruiz, A.B.; Gil-Guillén, V.F. Detection of frailty in older patients using a mobile app: Cross-sectional observational study in primary care. Br. J. Gen. Pract. 2020, 70, e29–e35. [Google Scholar] [CrossRef]
- Sanghai, S.; Wong, C.; Wang, Z.; Clive, P.; Tran, W.; Waring, M.; Goldberg, R.; Hayward, R.; Saczynski, J.S.; McManus, D.D. Rates of potentially inappropriate dosing of direct-acting oral anticoagulants and associations with geriatric conditions among older patients with atrial fibrillation: The SAGE-AF study. J. Am. Heart Assoc. 2020, 9, e014108. [Google Scholar] [CrossRef] [PubMed]
- Vergara, I.; Mateo-Abad, M.; Saucedo-Figueredo, M.C.; Machón, M.; Montiel-Luque, A.; Vrotsou, K.; del Val, M.A.N.; Díez-Ruiz, A.; Güell, C.; Matheu, A.; et al. Description of frail older people profiles according to four screening tools applied in primary care settings: A cross sectional analysis. BMC Geriatr. 2019, 19, 342. [Google Scholar] [CrossRef]
- Lorenzo-López, L.; López-López, R.; Maseda, A.; Buján, A.; Rodríguez-Villamil, J.L.; Millán-Calenti, J.C. Changes in frailty status in a community-dwelling cohort of older adults: The VERISAÚDE study. Maturitas 2019, 119, 54–60. [Google Scholar] [CrossRef]
- Rea, F.; Savaré, L.; Valsassina, V.; Ciardullo, S.; Perseghin, G.; Corrao, G.; Mancia, G. Adherence to antidiabetic drug therapy and reduction of fatal events in elderly frail patients. Cardiovasc. Diabetol. 2023, 22, 53. [Google Scholar] [CrossRef]
- Anh, D.; Nguyen, T.; Nguyen, T.; Nguyen, T.V. The validity of the FRAIL scale in frailty screening among Vietnamese older people. Aging Med. Healthc. 2022, 13, 87–92. [Google Scholar] [CrossRef]
- Tembo, M.C.; Holloway-Kew, K.L.; Bortolasci, C.C.; Brennan-Olsen, S.L.; Williams, L.J.; Kotowicz, M.A.; Pasco, J.A. Association between serum interleukin-6 and frailty in older men: Cross-sectional data. Eur. Geriatr. Med. 2021, 12, 887–892. [Google Scholar] [CrossRef]
- Hasan, S.S.; Burud, I.A.S.; Kow, C.S.; Rasheed, M.K.; Chan, K.S.C.; Tay, P.K.; Ahmed, S.I. Use of potentially inappropriate medications among older outpatients and inpatients in a tertiary care hospital in Malaysia. Int. J. Clin. Pract. 2021, 75, e13714. [Google Scholar] [CrossRef]
- Thiruchelvam, K.; Byles, J.; Hasan, S.S.; Egan, N.; Cavenagh, D.; Kairuz, T. Common combinations of medications used among oldest-old women: A population-based study over 15 years. Aging Clin. Exp. Res. 2021, 33, 1919–1928. [Google Scholar] [CrossRef] [PubMed]
- Arias-Fernández, L.; Smith-Plaza, A.M.; Barrera-Castillo, M.; Prado-Suárez, J.; Lopez-Garcia, E.; Rodríguez-Artalejo, F.; Lana, A. Sleep patterns and physical function in older adults attending primary health care. Fam. Pract. 2021, 38, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Novaes, P.H.; Da Cruz, D.T.; Lucchetti, A.L.; Leite, I.C.; Lucchetti, G. The “iatrogenic triad”: Polypharmacy, drug–drug interactions, and potentially inappropriate medications in older adults. Int. J. Clin. Pharm. 2017, 39, 818–825. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-J.; Seo, S.-H.; Seo, A.-R.; Kim, B.-K.; Lee, G.-Y.; Choi, Y.-S.; Kim, J.-H.; Kim, J.-R.; Kang, Y.-S.; Jeong, B.-G.; et al. The association of perceived neighborhood walkability and environmental pollution with frailty among community-dwelling older adults in Korean rural areas: A cross-sectional study. J. Prev. Med. Public Health 2019, 52, 405–415. [Google Scholar] [CrossRef]
- Tan, L.F.; Lim, Z.Y.; Choe, R.; Seetharaman, S.; Merchant, R. Screening for frailty and sarcopenia among older persons in medical outpatient clinics and its associations with healthcare burden. J. Am. Med. Dir. Assoc. 2017, 18, 583–587. [Google Scholar] [CrossRef]
- Mertens, B.J.; Kwint, H.F.; Van Marum, R.J.; Bouvy, M.L. Are multidose drug dispensing systems initiated for the appropriate patients? Eur. J. Clin. Pharmacol. 2018, 74, 1159–1164. [Google Scholar] [CrossRef] [PubMed]
- Trevisan, C.; Veronese, N.; Maggi, S.; Baggio, G.; Toffanello, E.D.; Zambon, S.; Sartori, L.; Musacchio, E.; Perissinotto, E.; Crepaldi, G.; et al. Factors influencing transitions between frailty states in elderly adults: The Progetto Veneto Anziani Longitudinal Study. J. Am. Geriatr. Soc. 2017, 65, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Yaghi, N.; Yaghi, C.; Abifadel, M.; Boulos, C.; Feart, C. Dietary patterns and risk factors of frailty in Lebanese older adults. Nutrients 2021, 13, 2188. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, S.; Kim, M.; Kim, B.; Jeong, E.; Shim, H.; Won, C. A later menopausal age is associated with a lower prevalence of physical frailty in community-dwelling older adults: The Korean Frailty and Aging Cohort Study (KFACS). Arch. Gerontol. Geriatr. 2020, 91, 104243. [Google Scholar] [CrossRef]
- Romera-Liebana, L.; Orfila, F.; Segura, J.M.; Real, J.; Fabra, M.L.; Möller, M.; Lancho, S.; Ramirez, A.; Marti, N.; Cullell, M.; et al. Effects of a primary care-based multifactorial intervention on physical and cognitive function in frail, elderly individuals: A randomized controlled trial. J. Gerontol. Ser. A 2018, 73, 1668–1674. [Google Scholar] [CrossRef]
- Machón, M.; Mateo-Abad, M.; Vrotsou, K.; Zupiria, X.; Güell, C.; Rico, L.; Vergara, I. Dietary patterns and their relationship with frailty in functionally independent older adults. Nutrients 2018, 10, 406. [Google Scholar] [CrossRef]
- Buttery, A.K.; Busch, M.A.; Gaertner, B.; Scheidt-Nave, C.; Fuchs, J. Prevalence and correlates of frailty among older adults: Findings from the German health interview and examination survey. BMC Geriatr. 2015, 15, 22. [Google Scholar] [CrossRef] [PubMed]
- Anjum, D.Z.; Strange, J.E.; Fosbøl, E.; Garred, C.H.; Malik, M.E.; Andersson, C.; Jhund, P.S.; McMurray, J.J.V.; Petrie, M.C.; Kober, L.; et al. Initiation of Medical Therapy for Heart Failure Patients According to Kidney Function: A Danish Nationwide Study. Clin. Epidemiol. 2023, 15, 855–866. [Google Scholar] [CrossRef]
- Díez-Villanueva, P.; Cosín-Sales, J.; Roldán-Schilling, V.; Barrios, V.; Riba-Artés, D.; Gavín-Sebastián, O. Use of direct acting oral anticoagulants in elderly patients with atrial fibrillation: A multicenter, cross-sectional study in Spain. J. Clin. Med. 2023, 12, 1224. [Google Scholar] [CrossRef]
- Islam, F.; Panda, M.; Pathak, R.; Agarwalla, R.; Singh, V.; Singh, F. Interplay of multimorbidity and polypharmacy on a community dwelling frail elderly cohort in the peri-urban slums of Delhi, India. J. Fam. Med. Prim. Care 2020, 9, 1647–1655. [Google Scholar] [CrossRef]
- Panagiotakis, S.H.; Simos, P.; Basta, M.; Zaganas, I.; Perysinaki, G.S.; Akoumianakis, I.; Tziraki, C.; Lionis, C.; Vgontzas, A.; Boumpas, D. Interactions of mediterranean diet, obesity, polypharmacy, depression and systemic inflammation with frailty status. MAEDICA–J. Clin. Med. 2022, 17, 20–27. [Google Scholar] [CrossRef]
- Chao, C.-T.; Huang, J.-W.; COGENT (COhort of GEriatric Nephrology in NTUH) Study Group. Geriatric syndromes are potential determinants of the medication adherence status in prevalent dialysis patients. PeerJ 2016, 4, e2122. [Google Scholar] [CrossRef]
- van Kempen, J.A.L.; Melis, R.J.F.; Perry, M.; Schers, H.J.; Rikkert, M.G.M.O. Diagnosis of frailty after a comprehensive geriatric assessment: Differences between family physicians and geriatricians. J. Am. Board Fam. Med. 2015, 28, 240–248. [Google Scholar] [CrossRef]
- Strandberg, T.E.; Urtamo, A.; Kähärä, J.; Strandberg, A.Y.; Pitkälä, K.H.; Kautiainen, H. Statin treatment is associated with a neutral effect on health-related quality of life among community-dwelling octogenarian men: The Helsinki businessmen study. J. Gerontol. Ser. A 2018, 73, 1418–1423. [Google Scholar] [CrossRef]
- Cheong, V.-L.; Mehdizadeh, D.; Todd, O.M.; Gardner, P.; Zaman, H.; Clegg, A.; Alldred, D.P.; Faisal, M. The extent of anticholinergic burden across an older Welsh population living with frailty: Cross-sectional analysis of general practice records. Age Ageing 2023, 52, afad136. [Google Scholar] [CrossRef] [PubMed]
- Ye, L.; Elstgeest, L.E.M.; Zhang, X.; Alhambra-Borrás, T.; Tan, S.S.; Raat, H. Factors associated with physical, psychological and social frailty among community-dwelling older persons in Europe: A cross-sectional study of Urban Health Centres Europe (UHCE). BMC Geriatr. 2021, 21, 422. [Google Scholar] [CrossRef] [PubMed]
- Salinas-Rodríguez, A.; Manrique-Espinoza, B.; Rivera-Almaraz, A.; Ávila-Funes, J.A. Polypharmacy is associated with multiple health-related outcomes in Mexican community-dwelling older adults. Salud Pública Méx. 2020, 62, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Martins, B.A.; Visvanathan, R.; Barrie, H.; Huang, C.H.; Matsushita, E.; Okada, K.; Satake, S.; Uno, C.; Kuzuya, M. Frailty prevalence using Frailty Index, associated factors and level of agreement among frailty tools in a cohort of Japanese older adults. Arch. Gerontol. Geriatr. 2019, 84, 103908. [Google Scholar] [CrossRef]
- LaCroix, A.Z.; Gray, S.L.; Aragaki, A.; Cochrane, B.B.; Newman, A.B.; Kooperberg, C.L.; Black, H.; Curb, J.D.; Greenland, P.; Woods, N.F. Statin use and incident frailty in women aged 65 years or older: Prospective findings from the Women’s Health Initiative Observational Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2008, 63, 369–375. [Google Scholar] [CrossRef][Green Version]
- Gafoor, R.; Charlton, J.; Ravindrarajah, R.; Gulliford, M.C. Importance of frailty for association of antipsychotic drug use with risk of fracture: Cohort study using electronic health records. J. Am. Med. Dir. Assoc. 2019, 20, 1495–1501.e1. [Google Scholar] [CrossRef]
- Herr, M.; Cesari, M.; Landre, B.; Ankri, J.; Vellas, B.; Andrieu, S.; MAPT/DSA Study Group. Factors associated with changes of the frailty status after age 70: Findings in the MAPT study. Ann. Epidemiol. 2019, 34, 65–70.e1. [Google Scholar] [CrossRef]
- Lee, D.R.; Santo, E.C.; Lo, J.C.; Weintraub, M.L.R.; Patton, M.; Gordon, N.P. Understanding functional and social risk characteristics of frail older adults: A cross-sectional survey study. BMC Fam. Pract. 2018, 19, 170. [Google Scholar] [CrossRef]
- Lampela, P.; Taipale, H.; Hartikainen, S. Association between anticholinergic load and frailty in community-dwelling older people. J. Am. Geriatr. Soc. 2016, 64, 671–672. [Google Scholar] [CrossRef] [PubMed]
- Chi, C.-Y.; Wang, J.; Lee, S.-Y.; Chao, C.-T.; Hung, K.-Y.; Chien, K.-L. The Impact of Glucose-Lowering Strategy on the Risk of Increasing Frailty Severity among 49,519 Patients with Diabetes Mellitus: A Longitudinal Cohort Study. Aging Dis. 2023, 14, 1917–1926. [Google Scholar] [CrossRef]
- Sargent, L.; Zimmerman, K.M.; Mohammed, A.; Barrett, M.J.; Nawaz, H.; Wyman-Chick, K.; Mackiewicz, M.; Roman, Y.; Slattum, P.; Russell, S.; et al. Low-Income Older Adults’ Vulnerability to Anticholinergic Medication-Associated Frailty. Drugs Aging 2023, 40, 1123–1131. [Google Scholar] [CrossRef]
- Mizuno, T.; Godai, K.; Kabayama, M.; Akasaka, H.; Kido, M.; Isaka, M.; Kubo, M.; Gondo, Y.; Ogawa, M.; Ikebe, K.; et al. Age Group Differences in the Association Between Sleep Status and Frailty Among Community-Dwelling Older Adults: The SONIC Study. Gerontol. Geriatr. Med. 2023, 9, 23337214231205432. [Google Scholar] [CrossRef]
- Jamieson, H.; Nishtala, P.S.; Bergler, H.U.; Weaver, S.K.; Pickering, J.W.; Ailabouni, N.J.; Abey-Nesbit, R.; Gullery, C.; Deely, J.; Gee, S.B.; et al. Deprescribing anticholinergic and sedative drugs to reduce polypharmacy in frail older adults living in the community: A randomized controlled trial. J. Gerontol. Ser. A 2023, 78, 1692–1700. [Google Scholar] [CrossRef] [PubMed]
- Tabue-Téguo, M.; Villeneuve, R.; Helene-Pelage, J.; Cesari, M.; Chovino, J.; Boire, A.; Dramé, M.; Simo-Tabue, N.; Boucaud-Maitre, D. Drug storage, polypharmacy and frailty syndrome in older people: An observational study. Pan Afr. Med. J. 2023, 45, 29. [Google Scholar] [CrossRef] [PubMed]
- Ekram, A.S.; Ryan, J.; Espinoza, S.E.; Newman, A.B.; Murray, A.M.; Orchard, S.G.; Fitzgerald, S.M.; McNeil, J.J.; Ernst, M.E.; Woods, R.L. The association between frailty and dementia-free and physical disability-free survival in community-dwelling older adults. Gerontology 2023, 69, 549–560. [Google Scholar] [CrossRef]
- Alqahtani, B. Number of medications and polypharmacy are associated with frailty in older adults: Results from the Midlife in the United States study. Front. Public Health 2023, 11, 1148671. [Google Scholar] [CrossRef]
- Nishimura, S.; Kumamaru, H.; Shoji, S.; Nakatani, E.; Yamamoto, H.; Ichihara, N.; Sandhu, A.T.; Miyachi, Y.; Miyata, H.; Kohsaka, S. Frailty and subsequent adverse outcomes in older patients with atrial fibrillation treated with oral anticoagulants: The Shizuoka study. Res. Pract. Thromb. Haemost. 2023, 7, 100129. [Google Scholar] [CrossRef] [PubMed]
- Kravvariti, E.; Ntouros, P.A.; Vlachogiannis, N.I.; Pappa, M.; Souliotis, V.L.; Sfikakis, P.P. Geriatric frailty is associated with oxidative stress, accumulation, and defective repair of DNA double-strand breaks independently of age and comorbidities. J. Gerontol. Ser. A 2023, 78, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Pan, Y.; Song, Y.; Zhou, Y.; Zhang, W.; Li, X.; Li, J.; Li, Y.; Ma, L. Association of metformin exposure with low risks of frailty and adverse outcomes in patients with diabetes. Eur. J. Med. Res. 2023, 28, 65. [Google Scholar] [CrossRef]
- Şentürk Durmuş, N.; Akın, S.; Goksuluk, D. Prevalence of Potentially Inappropriate Medication and Frailty: A Comparison of Three Criteria in Older Turkish Adults. J. Clin. Pract. Res. 2023, 45, 55. [Google Scholar] [CrossRef]
- Arslan, M.; Çakır, M.; Koç, E.M.; Sozmen, K. Determinants of Frailty and Gait Speed in People Over 65 Years of Age. J. Clin. Pract. Res. 2023, 45, 62. [Google Scholar] [CrossRef]
- Doñate-Martínez, A.; Alhambra-Borrás, T.; Durá-Ferrandis, E. Frailty as a predictor of adverse outcomes among Spanish community-dwelling older adults. Int. J. Environ. Res. Public Health 2022, 19, 12756. [Google Scholar] [CrossRef]
- Ben Chaouacha, C.; Al Zaabi, B.; Al Farsi, Y.; Aftab, N.M. Frailty profile of geriatric patients according to the multidimensional prognostic index: A cross-sectional study in primary care in the Sultanate of Oman. Aging Med. Health 2022, 13, 184–192. [Google Scholar] [CrossRef]
- Toepfer, S.; König, M.; Spira, D.; Drewelies, J.; Kreutz, R.; Bolbrinker, J.; Demuth, I. Sex differences in characteristics associated with potentially inappropriate medication use and associations with functional capacity in older participants of the Berlin Aging Study II. Gerontology 2022, 68, 664–672. [Google Scholar] [CrossRef]
- Athuraliya, N.; Etherton-Beer, C. Health in Men Study: Is frailty a predictor of medication-related hospitalization? QJM Int. J. Med. 2022, 115, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Sütlü, S. Frailty Status and Related Factors of Elderly People Recieving Aid from the Social Assitance Foundation in Burdur Province. Turk. J. Geriatr. 2022, 25, 88–96. [Google Scholar] [CrossRef]
- Thapaliya, K.; Harris, M.L.; Byles, J.E. Polypharmacy trajectories among older women with and without dementia: A longitudinal cohort study. Explor. Res. Clin. Soc. Pharm. 2021, 3, 100053. [Google Scholar] [CrossRef]
- Çakmak, G.; Öztürk, Z.A. The Relationship Between Polypharmacy and Frailty in Older Adults: Which Frailty Assessment Tool Shows the Relationship Best? Prog. Nutr. 2021, 23, e2021295. [Google Scholar]
- de Breij, S.; Rijnhart, J.J.; Schuster, N.A.; Rietman, M.L.; Peters, M.J.; Hoogendijk, E.O. Explaining the association between frailty and mortality in older adults: The mediating role of lifestyle, social, psychological, cognitive, and physical factors. Prev. Med. Rep. 2021, 24, 101589. [Google Scholar] [CrossRef]
- Hung, C.-D.; Yang, C.-C.; Lee, C.-Y.; Hu, S.C.-S.; Chen, S.-C.; Hung, C.-H.; Chuang, H.-Y.; Chen, C.-Y.; Kuo, C.-H. Polypharmacy is significantly and positively associated with the frailty status assessed using the 5-item FRAIL scale, cardiovascular health phenotypic classification of frailty index, and study of osteoporotic fractures scale. J. Clin. Med. 2021, 10, 4413. [Google Scholar] [CrossRef] [PubMed]
- O’DOnovan, M.; Sezgin, D.; O’CAoimh, R.; Liew, A. The relationship between frailty and diabetes: An investigation of self-rated health, depression symptoms and quality of life in the Study of Health Aging and Retirement in Europe. Arch. Gerontol. Geriatr. 2021, 96, 104448. [Google Scholar] [CrossRef] [PubMed]
- Setiati, S.; Soejono, C.H.; Harimurti, K.; Dwimartutie, N.; Aryana, I.G.P.S.; Sunarti, S.; Budiningsih, F.; Mulyana, R.; Dwipa, L.; Sudarso, A.; et al. Frailty and its associated risk factors: First phase analysis of multicentre Indonesia longitudinal aging study. Front. Med. 2021, 8, 658580. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Reina, E.; Aguilar-Cano, L.; García-Merino, M.R.; Ocaña-Riola, R.; Valdellós, J.; Bellido-Estévez, I.; Ariza-Zafra, G. Assessing prevalence and factors related to frailty in community-dwelling older adults: A multinomial logistic analysis. J. Clin. Med. 2021, 10, 3576. [Google Scholar] [CrossRef] [PubMed]
- Kabayama, M.; Kamide, K.; Gondo, Y.; Masui, Y.; Nakagawa, T.; Ogawa, M.; Yasumoto, S.; Ryuno, H.; Akagi, Y.; Kiyoshige, E.; et al. The association of blood pressure with physical frailty and cognitive function in community-dwelling septuagenarians, octogenarians, and nonagenarians: The SONIC study. Hypertens. Res. 2020, 43, 1421–1429. [Google Scholar] [CrossRef]
- Elhussein, L.; Jödicke, A.M.; He, Y.; Delmestri, A.; Robinson, D.E.; Strauss, V.Y.; Prieto-Alhambra, D. Characterising complex health needs and the use of preventive therapies in the older population: A population-based cohort analysis of UK primary care and hospital linked data. BMC Geriatr. 2023, 23, 58. [Google Scholar] [CrossRef]
- Sanghai, S.R.; Liu, W.; Wang, W.; Rongali, S.; Orkaby, A.R.; Saczynski, J.S.; Rose, A.J.; Kapoor, A.; Li, W.; Yu, H.; et al. Prevalence of frailty and associations with oral anticoagulant prescribing in atrial fibrillation. J. Gen. Intern. Med. 2022, 37, 730–736. [Google Scholar] [CrossRef]
- Melo Filho, J.; Moreira, N.B.; Vojciechowski, A.S.; Biesek, S.; Bento, P.C.; Gomes, A.R. Frailty prevalence and related factors in older adults from southern Brazil: A cross-sectional observational study. Clinics 2020, 75, e1694. [Google Scholar] [CrossRef]
- Machón, M.; Mateo-Abad, M.; Clerencia-Sierra, M.; Güell, C.; Poblador-Pou, B.; Vrotsou, K.; Gimeno-Miguel, A.; Prados-Torres, A.; Vergara, I. Multimorbidity and functional status in older people: A cluster analysis. Eur. Geriatr. Med. 2020, 11, 321–332. [Google Scholar] [CrossRef]
- Shim, H.; Kim, S.; Kim, M.; Kim, B.S.; Jeong, E.; Lee, Y.J.; Won, C.W. Older men living with spouse and older women living with spouse and children have lower frailty prevalence: The Korean Frailty and Aging Cohort Study (KFACS). Ann. Geriatr. Med. Res. 2020, 24, 204–210. [Google Scholar] [CrossRef]
- Chumha, N.; Funsueb, S.; Kittiwachana, S.; Rattanapattanakul, P.; Lerttrakarnnon, P. An artificial neural network model for assessing frailty-associated factors in the Thai population. Int. J. Environ. Res. Public Health 2020, 17, 6808. [Google Scholar] [CrossRef]
- Oetsma, S.; Boonen, A.; Starmans, M.; Peeters, R.; van Onna, M. Validation of two frailty questionnaires in older patients with rheumatoid arthritis: A cross-sectional study. Clin. Exp. Rheumatol. 2020, 38, 523–528. [Google Scholar]
- Tembo, M.C.; Holloway-Kew, K.L.; Sui, S.X.; Dunning, T.; Low, A.C.H.; Yong, S.-J.; Ng, B.L.; Brennan-Olsen, S.L.; Williams, L.J.; Kotowicz, M.A.; et al. Prevalence of frailty in older men and women: Cross-sectional data from the Geelong Osteoporosis Study. Calcif. Tissue Int. 2020, 107, 220–229. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Honda, T.; Narazaki, K.; Chen, T.; Kishimoto, H.; Kumagai, S. Physical frailty and risk of needing long-term care in community-dwelling older adults: A 6-year prospective study in Japan. J. Nutr. Health Aging 2019, 23, 856–861. [Google Scholar] [CrossRef] [PubMed]
- Moulis, F.; Moulis, G.; Balardy, L.; Gérard, S.; Sourdet, S.; Rougé-Bugat, M.-E.; Lapeyre-Mestre, M.; Montastruc, J.-L.; Rolland, Y.; Vellas, B. Searching for a polypharmacy threshold associated with frailty. J. Am. Med. Dir. Assoc. 2015, 16, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Serra-Prat, M.; Papiol, M.; Vico, J.; Palomera, E.; Sist, X.; Cabré, M. Factors associated with frailty in community-dwelling elderly population. A cross-sectional study. Eur. Geriatr. Med. 2016, 7, 531–537. [Google Scholar] [CrossRef]
- Meid, A.D.; Quinzler, R.; Freigofas, J.; Saum, K.-U.; Schöttker, B.; Holleczek, B.; Heider, D.; König, H.-H.; Brenner, H.; Haefeli, W.E. Medication underuse in aging outpatients with cardiovascular disease: Prevalence, determinants, and outcomes in a prospective cohort study. PLoS ONE 2015, 10, e0136339. [Google Scholar] [CrossRef]
- Eyigor, S.; Kutsal, Y.G.; Duran, E.; Huner, B.; Paker, N.; Durmus, B.; Sahin, N.; Civelek, G.M.; Gokkaya, K.; Doğan, A.; et al. Frailty prevalence and related factors in the older adult—FrailTURK Project. AGE 2015, 37, 50. [Google Scholar] [CrossRef]
- Peel, N.M.; Runganga, M.; Hubbard, R. Multiple medication use in older patients in post-acute transitional care: A prospective cohort study. Clin. Interv. Aging 2014, 9, 1453–1462. [Google Scholar] [CrossRef]
- Koponen, M.P.; Bell, J.S.; Karttunen, N.M.; Nykänen, I.A.; Desplenter, F.A.; Hartikainen, S.A. Analgesic use and frailty among community-dwelling older people: A population-based study. Drugs Aging 2013, 30, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Jazbar, J.; Pišek, Š.; Locatelli, I.; Kos, M. Prevalence and incidence of frailty among community-dwelling older adults in Slovenia. Slov. J. Public Health 2021, 60, 190–198. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, J.A.; Lima, C.D.A.; da Costa, F.M.; Caldeira, A.P. Health care are associated with worsening of frailty in community older adults. Rev. Saude Publica 2019, 53, 32. [Google Scholar] [CrossRef] [PubMed]
- Porter, B.; Arthur, A.; Savva, G.M. How do potentially inappropriate medications and polypharmacy affect mortality in frail and non-frail cognitively impaired older adults? A cohort study. BMJ Open 2019, 9, e026171. [Google Scholar] [CrossRef]
- Nguyen, A.T.; Nguyen, L.H.; Nguyen, T.X.; Nguyen, T.T.H.; Nguyen, H.T.T.; Nguyen, T.N.; Pham, H.Q.; Tran, B.X.; Latkin, C.A.; Ho, C.S.H.; et al. Frailty prevalence and association with health-related quality of life impairment among rural community-dwelling older adults in Vietnam. Int. J. Environ. Res. Public Health 2019, 16, 3869. [Google Scholar] [CrossRef]
- Panagiotakis, S.H.; Simos, P.; Zaganas, I.; Basta, M.; Perysinaki, G.S.; Fountoulakis, N.; Giaka, M.; Kapetanaki, S.; Koutentaki, I.; Bertsias, A.; et al. Self-reported fatigue as a risk index for dementia diagnosis. Eur. Geriatr. Med. 2018, 9, 211–217. [Google Scholar] [CrossRef]
- Chen, P.-J.; Yang, K.-Y.; Perng, W.-C.; Lin, K.-C.; Wang, K.-Y. Effect of dyspnea on frailty stages and related factors in Taiwanese men with COPD. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 2463–2469. [Google Scholar] [CrossRef]
- Takeuchi, H.; Uchida, H.A.; Kakio, Y.; Okuyama, Y.; Okuyama, M.; Umebayashi, R.; Wada, K.; Sugiyama, H.; Sugimoto, K.; Rakugi, H.; et al. The prevalence of frailty and its associated factors in Japanese hemodialysis patients. Aging Dis. 2018, 9, 192–207. [Google Scholar] [CrossRef]
- Wong, S.; Katz, A.; Williamson, T.; Singer, A.; Peterson, S.; Taylor, C.; Price, M.; McCracken, R.; Thandi, M. Can linked electronic medical record and administrative data help us identify those living with frailty? Int. J. Popul. Data Sci. 2020, 5, 1343. [Google Scholar] [CrossRef]
- Herr, M.; Robine, J.-M.; Pinot, J.; Arvieu, J.-J.; Ankri, J. Polypharmacy and frailty: Prevalence, relationship, and impact on mortality in a French sample of 2350 old people. Pharmacoepidemiol. Drug Saf. 2015, 24, 637–646. [Google Scholar] [CrossRef]
- Meng, L.; Shi, H.; Shi, J.; Yu, P.-L.; Xi, H. Differences in clinical characteristics, muscle mass, and physical performance among different frailty levels in Chinese older men. Chin. Med. J. 2019, 132, 352–355. [Google Scholar] [CrossRef]
- Herr, M.; Sirven, N.; Grondin, H.; Pichetti, S.; Sermet, C. Frailty, polypharmacy, and potentially inappropriate medications in old people: Findings in a representative sample of the French population. Eur. J. Clin. Pharmacol. 2017, 73, 1165–1172. [Google Scholar] [CrossRef]
- Merchant, R.A.; Chen, M.Z.; Tan, L.W.L.; Lim, M.Y.; Ho, H.K.; van Dam, R.M. Singapore healthy older people everyday (HOPE) study: Prevalence of frailty and associated factors in older adults. J. Am. Med. Dir. Assoc. 2017, 18, 734.e9–734.e14. [Google Scholar] [CrossRef]
- Pao, Y.-C.; Chen, C.-Y.; Chang, C.-I.; Chen, C.-Y.; Tsai, J.-S. Self-reported exhaustion, physical activity, and grip strength predict frailty transitions in older outpatients with chronic diseases. Medicine 2018, 97, e10933. [Google Scholar] [CrossRef] [PubMed]
- Gnjidic, D.; Hilmer, S.N.; Blyth, F.M.; Naganathan, V.; Waite, L.; Seibel, M.J.; McLachlan, A.J.; Cumming, R.G.; Handelsman, D.J.; Le Couteur, D.G. Polypharmacy cutoff and outcomes: Five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J. Clin. Epidemiol. 2012, 65, 989–995. [Google Scholar] [CrossRef] [PubMed]
- Lakey, S.L.; LaCroix, A.Z.; Gray, S.L.; Borson, S.; Williams, C.D.; Calhoun, D.; Goveas, J.S.; Smoller, J.W.; Ockene, J.K.; Masaki, K.H.; et al. Antidepressant use, depressive symptoms, and incident frailty in women aged 65 and older from the w omen’s h ealth i nitiative observational study. J. Am. Geriatr. Soc. 2012, 60, 854–861. [Google Scholar] [CrossRef] [PubMed]
- Crentsil, V.; Ricks, M.O.; Xue, Q.-L.; Fried, L.P. A pharmacoepidemiologic study of community-dwelling, disabled older women: Factors associated with medication use. Am. J. Geriatr. Pharmacother. 2010, 8, 215–224. [Google Scholar] [CrossRef]
- Pérez-Ros, P.; Vila-Candel, R.; López-Hernández, L.; Martínez-Arnau, F.M. Nutritional status and risk factors for frailty in community-dwelling older people: A cross-sectional study. Nutrients 2020, 12, 1041. [Google Scholar] [CrossRef]
- García-Esquinas, E.; Graciani, A.; Guallar-Castillón, P.; López-García, E.; Rodríguez-Mañas, L.; Rodríguez-Artalejo, F. Diabetes and risk of frailty and its potential mechanisms: A prospective cohort study of older adults. J. Am. Med. Dir. Assoc. 2015, 16, 748–754. [Google Scholar] [CrossRef]
- Byrne, C.J.; Walsh, C.; Cahir, C.; Bennett, K. Impact of drug burden index on adverse health outcomes in Irish community-dwelling older people: A cohort study. BMC Geriatr. 2019, 19, 121. [Google Scholar] [CrossRef] [PubMed]
- Saeidimehr, S.; Delbari, A.; Zanjari, N.; Vatan, R.F. Factors related to frailty among older adults in Khuzestan, Iran. Salmand 2021, 16, 202–217. [Google Scholar] [CrossRef]
- Güngör Başaran, A.Y.; Akal Yıldız, E. Nutrition status, muscle mass, and frailty in older people: A cross-sectional study conducted in Cyprus. J. Am. Nutr. Assoc. 2022, 41, 318–324. [Google Scholar] [CrossRef]
- Chen, C.-Y.; Wu, S.-C.; Chen, L.-J.; Lue, B.-H. The prevalence of subjective frailty and factors associated with frailty in Taiwan. Arch. Gerontol. Geriatr. 2010, 50, S43–S47. [Google Scholar] [CrossRef]
- Chang, C.-I.; Chan, D.-C.; Kuo, K.-N.; Hsiung, C.A.; Chen, C.-Y. Prevalence and correlates of geriatric frailty in a northern Taiwan community. J. Formos. Med. Assoc. 2011, 110, 247–257. [Google Scholar] [CrossRef]
- Woo, J.; Leung, J. Multi-morbidity, dependency, and frailty singly or in combination have different impact on health outcomes. AGE 2014, 36, 923–931. [Google Scholar] [CrossRef] [PubMed]
- Moulis, F.; Moulis, G.; Balardy, L.; Gérard, S.; Montastruc, F.; Sourdet, S.; Rougé-Bugat, M.-E.; Lapeyre-Mestre, M.; Montastruc, J.-L.; Rolland, Y.; et al. Exposure to atropinic drugs and frailty status. J. Am. Med. Dir. Assoc. 2015, 16, 253–257. [Google Scholar] [CrossRef]
- Woo, J.; Yu, R.; Wong, M.; Yeung, F.; Wong, M.; Lum, C. Frailty screening in the community using the FRAIL scale. J. Am. Med. Dir. Assoc. 2015, 16, 412–419. [Google Scholar] [CrossRef]
- Ravindrarajah, R.; Dregan, A.; Hazra, N.C.; Hamada, S.; Jackson, S.H.; Gulliford, M.C. Declining blood pressure and intensification of blood pressure management among people over 80 years: Cohort study using electronic health records. J. Hypertens. 2017, 35, 1276–1282. [Google Scholar] [CrossRef]
- Woo, J.; Zheng, Z.; Leung, J.; Chan, P. Prevalence of frailty and contributory factors in three Chinese populations with different socioeconomic and healthcare characteristics. BMC Geriatr. 2015, 15, 163. [Google Scholar] [CrossRef]
- Thompson, M.Q.; Theou, O.; Yu, S.; Adams, R.J.; Tucker, G.R.; Visvanathan, R. Frailty prevalence and factors associated with the frailty phenotype and frailty index: Findings from the north West Adelaide health study. Australas. J. Ageing 2018, 37, 120–126. [Google Scholar] [CrossRef]
- Kleipool, E.E.F.; Nielen, M.M.J.; Korevaar, J.C.; Harskamp, R.E.; Smulders, Y.M.; Serné, E.; Thijs, A.; Peters, M.J.L.; Muller, M. Prescription patterns of lipid lowering agents among older patients in general practice: An analysis from a national database in the Netherlands. Age Ageing 2019, 48, 577–582. [Google Scholar] [CrossRef]
- Tabue-Teguo, M.; Grasset, L.; Avila-Funes, J.A.; Genuer, R.; Proust-Lima, C.; Péres, K.; Féart, C.; Amieva, H.; Harmand, M.G.-C.; Helmer, C.; et al. Prevalence and co-occurrence of geriatric syndromes in people aged 75 years and older in France: Results from the Bordeaux three-city study. J. Gerontol. Ser. A 2018, 73, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Hironaka, S.; Kugimiya, Y.; Watanabe, Y.; Motokawa, K.; Hirano, H.; Kawai, H.; Kera, T.; Kojima, M.; Fujiwara, Y.; Ihara, K.; et al. Association between oral, social, and physical frailty in community-dwelling older adults. Arch. Gerontol. Geriatr. 2020, 89, 104105. [Google Scholar] [CrossRef] [PubMed]
- Threapleton, C.J.; Kimpton, J.E.; Carey, I.M.; DeWilde, S.; Cook, D.G.; Harris, T.; Baker, E.H. Development of a structured clinical pharmacology review for specialist support for management of complex polypharmacy in primary care. Br. J. Clin. Pharmacol. 2020, 86, 1326–1335. [Google Scholar] [CrossRef]
- Taci, D.Y.; Yılmaz, S.; Arslan, I.; Fidancı, İ.; Çelik, M. The evaluation of frailty in the elderly and affecting biopsychosocial factors: A cross-sectional observational study. Iran. J. Public Health 2023, 52, 159–165. [Google Scholar] [CrossRef]
- Erdoğan, I.; Tuncer, O. Evaluation of the Relationship Between Frailty, Polypharmacy, and Depression in People 65 Years of Age and Older. Ank. Med. J. 2023, 23, 325–335. [Google Scholar] [CrossRef]
- Sánchez-García, S.; Gallegos-Carrillo, K.; Espinel-Bermudez, M.C.; Doubova, S.V.; Sánchez-Arenas, R.; García-Peña, C.; Salvà, A.; Briseño-Fabian, S.C. Comparison of quality of life among community-dwelling older adults with the frailty phenotype. Qual. Life Res. 2017, 26, 2693–2703. [Google Scholar] [CrossRef] [PubMed]
- Kleipool, E.E.; Hoogendijk, E.O.; Trappenburg, M.C.; Handoko, M.L.; Huisman, M.; Peters, M.J.; Muller, M. Frailty in older adults with cardiovascular disease: Cause, effect or both? Aging Dis. 2018, 9, 489–497. [Google Scholar] [CrossRef]
- Thein, F.S.; Li, Y.; Nyunt, M.S.Z.; Gao, Q.; Wee, S.L.; Ng, T.P. Physical frailty and cognitive impairment is associated with diabetes and adversely impact functional status and mortality. Postgrad. Med. 2018, 130, 561–567. [Google Scholar] [CrossRef]
- Esenkaya, M.E.; Dokuzlar, O.; Soysal, P.; Smith, L.; Jackson, S.E.; Isik, A.T. Validity of the Kihon Checklist for evaluating frailty status in Turkish older adults. Geriatr. Gerontol. Int. 2019, 19, 616–621. [Google Scholar] [CrossRef]
- Qiao, X.; Tian, X.; Liu, N.; Dong, L.; Jin, Y.; Si, H.; Liu, X.; Wang, C. The association between frailty and medication adherence among community-dwelling older adults with chronic diseases: Medication beliefs acting as mediators. Patient Educ. Couns. 2020, 103, 2548–2554. [Google Scholar] [CrossRef]
- Okui, N.; Okui, M. Ninjin’yoeito improves genitourinary symptoms in patients with frailty. Cureus 2023, 15, e40767. [Google Scholar] [CrossRef] [PubMed]
- Hoogendijk, E.O.; van der Horst, H.E.; Deeg, D.J.H.; Frijters, D.H.M.; Prins, B.A.H.; Jansen, A.P.D.; Nijpels, G.; van Hout, H.P.J. The identification of frail older adults in primary care: Comparing the accuracy of five simple instruments. Age Ageing 2013, 42, 262–265. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Contreras, L.; Martínez-Arnau, F.M.; Sancho-Cantus, D.; Cubero-Plazas, L.; Pérez-Ros, P. Fear of falling score is a predictor of falls in community-dwelling pre-frail and frail older people. Healthcare 2023, 11, 2132. [Google Scholar] [CrossRef]
- Jung, H.-W.; Yoo, H.-J.; Park, S.-Y.; Kim, S.-W.; Choi, J.-Y.; Yoon, S.-J.; Kim, C.-H.; Kim, K.-I. The Korean version of the FRAIL scale: Clinical feasibility and validity of assessing the frailty status of Korean elderly. Korean J. Intern. Med. 2016, 31, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.-W.; Kim, S.; Won, C.W. Validation of the Korean Frailty Index in community-dwelling older adults in a nationwide Korean Frailty and Aging Cohort study. Korean J. Intern. Med. 2021, 36, 456–466. [Google Scholar] [CrossRef]
- Ambrož, M.; de Vries, S.T.; Sidorenkov, G.; Hoogenberg, K.; Denig, P. Changes in blood pressure thresholds for initiating antihypertensive medication in patients with diabetes: A repeated cross-sectional study focusing on the impact of age and frailty. BMJ Open 2020, 10, e037694. [Google Scholar] [CrossRef]
- Pel-Littel, R.E.; Schuurmans, M.J.; Emmelot-Vonk, M.H.; Verhaar, H.J.J. Frailty: Defining and measuring of a concept. J. Nutr. Health Aging 2009, 13, 390–394. [Google Scholar] [CrossRef] [PubMed]
- van Kan, G.A.; Rolland, Y.; Houles, M.; Gillette-Guyonnet, S.; Soto, M.; Vellas, B. The assessment of frailty in older adults. Clin. Geriatr. Med. 2010, 26, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Bonaga, B.; Sánchez-Jurado, P.M.; Martínez-Reig, M.; Ariza, G.; Rodríguez-Mañas, L.; Gnjidic, D.; Salvador, T.; Abizanda, P. Frailty, polypharmacy, and health outcomes in older adults: The frailty and dependence in albacete study. J. Am. Med. Dir. Assoc. 2018, 19, 46–52. [Google Scholar] [CrossRef]
- Curtin, D.; Gallagher, P.F.; O’mahony, D. Explicit criteria as clinical tools to minimize inappropriate medication use and its consequences. Ther. Adv. Drug Saf. 2019, 10, 2042098619829431. [Google Scholar] [CrossRef]
- Ma, W.; Wang, H.; Wen, Z.; Liu, L.; Zhang, X. Potentially inappropriate medication and frailty in older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2023, 114, 105087. [Google Scholar] [CrossRef]
- Randles, M.A.; O’mahony, D.; Gallagher, P.F. Frailty and potentially inappropriate prescribing in older people with polypharmacy: A bi-directional relationship? Drugs Aging 2022, 39, 597–606. [Google Scholar] [CrossRef] [PubMed]
| Study ID Country | PIMs Criteria Used | Category | Non-Frail (%) | Pre-Frail (%) | Frail (%) |
|---|---|---|---|---|---|
| Bolina., 2019 [45] (Brazil) | Beers 2012 | At least one PIM | 94/554 = 17 | 277/834 = 33.2 | 112/219 = 51.1 |
| Aprahamian., 2018 * [25] (Brazil) | Beers 2015 | At least one PIM | 36/199 = 18.1 | 102/331 = 30.8 | 46/99 = 46.5 |
| Athuraliya., 2022 [184] (Australia) | Beers 2019 | At least one PIM | 221/3550 = 6.2 | N/A | 97/684 = 13.9 |
| Thiruchelvam., 2021 [40] (Australia) | Beers 2019 | At least one PIM in non-continuous polypharmacy | 4046/5655 = 71.5 | N/A | 993/1263 = 78.6 |
| At least one PIM in continuous polypharmacy | 1174/1258 = 93.3 | N/A | 786/820 = 95.9 | ||
| Thiruchelvam., 2021 [49] (Australia) | Beers 2019 | At least one PIM | 5316/7218 = 73.6 | N/A | 1811/2137 = 84.7 |
| Lockery., 2020 [70] (Australia, USA) | Beers 2019 | At least one PIM | 55/116 = 47.4 | 42/79 = 53.2 | 3/5 = 60.0 |
| Muhlack., 2018 [52] (Germany) | Beers 2019 | At least one PIM | N/A | N/A | 119/265 = 44.9 |
| EU (7)-PIM List | 153/265 = 57.7 | ||||
| PRISCUS List | 71/265 = 26.8 | ||||
| Porter., 2019 [211] (UK) | STOPP/START | Antipsychotic | 4/204 = 2 | 7/530 = 1.3 | 10/420 = 2.4 |
| Anticholinergics | 6/204 = 2.9 | 36/530 = 6.8 | 36/420 = 8.6 | ||
| Tricyclic antidepressants | 5/204 = 2.5 | 30/530 = 5.6 | 41/420 = 9.8 | ||
| Other antidepressants | 14/204 = 6.9 | 35/530 = 6.6 | 70/420 = 16.7 | ||
| Benzodiazepines | 4/204 = 2 | 14/530 = 2.6 | 28/420 = 6.7 | ||
| Proton pump inhibitors | 34/204 = 16.7 | 149/530 = 28.1 | 148/420 = 35.2 | ||
| Cox., 2023 * [33] (UK) | STOPP | No FRIDs | 14/39 = 35.9% | 12/46 = 26.1% | 1/15 = 6.67% |
| 1 FRID | 16/39 = 41.0% | 9/46 = 19.6% | 1/15 = 6.67% | ||
| >1 FRID | 9/39 = 23.1% | 25/46 = 54.3% | 13/15 = 86.7% | ||
| Uragami., 2021 * [58] (Japan) | STOPP-J | At least one PIM | 208/556 = 37.4 | 178/318 = 56 | 34/49 = 69.4 |
| Khera 2019 [90] (Canada) | STOPP/START v2 and Beers 2015 | At least one PIM in Frailty | N/A | N/A | 31/54 = 57.4 |
| Durmuş., 2023 [179] (Turkey) | TIME | PIM | 6/16 = 37.5 | 81/182 = 44.5 | 89/184 = 48.4 |
| Beers 2019 | PIM | 4/16 = 25.0 | 52/182 = 28.6 | 61/184 = 33.2 | |
| STOPP/START v2 | PIM | 4/16 = 25.0 | 42/182 = 23.1 | 52/184 = 28.3 | |
| Alves., 2020 * [71] (Brazil) | Brazilian Consensus on PIM for Older People | 53/181 = 29.3 | 160/323 = 49.5 | 41/76 = 53.9 |
| Study ID Country | Criteria Used to Identify DRP | Category | Non-Frail (%) | Pre-Frail (%) | Frail (%) |
|---|---|---|---|---|---|
| (Ye., 2022) * [26] (Netherlands, Greece, Croatia, Spain, United Kingdom) | MRQ-10 | Low risk ^ | 525/804 = 65.2 | N/A | 513/979 = 52.4 |
| High risk ^ | 279/804 = 34.8 | N/A | 466/979 = 47.6 | ||
| (Ye., 2021) * [161] (UK, Greece, Croatia, Netherlands, Spain) | MRQ-10 | Mean score | 4.06 (1.51) | N/A | 4.67 (1.68) |
| (Sargent., 2020) * [55] (Italy) | Anticholinergic Burden | ACB 1 | N/A | N/A | 117/512 = 22.9 |
| ACB 2 | N/A | N/A | 61/512 = 11.9 | ||
| ACB 3 | N/A | N/A | 45/512 = 8.8 | ||
| (Cheong., 2023) [160] (UK) | Anticholinergic Burden | ACB 1 | 72,010/255,402 = 28.2 | N/A | Mild: 99,685/185,902 = 53.6 Moderate: 47,608/69,867 = 68.1 Severe: 13,914/17,924 = 77.6 |
| ACB 2 | 170/255,402 = <0.1 | N/A | Mild: 269/185,902 = 0.2 Moderate: 168/69,867 = 0.2 Severe: 62/17,924 = 0.4 | ||
| ACB 3 | 12,508/255,402 = 4.9 | N/A | Mild: 21,582/185,902 = 11.6; Moderate: 11,239/69,867 = 16.1 Severe: 3438/17,924 = 19.2 | ||
| (Rhalimi 2018) * [130] (France) | SEGA | No DRP | N/A | N/A | Somewhat: 492/638 = 77 Frail: 75/121 = 62 Very: 79/131 = 60.3 |
| DRP | N/A | N/A | Somewhat: 146/638 = 23 Frail: 46/121 = 38 Very: 52/131 = 40 | ||
| (Athuraliya., 2022) [184] (Australia) | SFINX | Potential adverse DDI | 195/3550 = 5.47 | N/A | 127/684 = 18.22 |
| Frequency of any ADE | 242/3550 = 6.82 | N/A | 128/684 = 18.71 |
| Factor | Studies with No Significant Association (p ≥ 0.05) | Studies with Significant Association (p < 0.05) | Type of Association |
|---|---|---|---|
| Polypharmacy | |||
| ≥3 drugs | (Aprahamian., 2018; Brazil) [25] (1), (Aznar-Tortonda., 2020; Spain) [133] (8) | Positive | |
| ≥4 drugs | (JeanWoo., 2015; China) [234] (2) | (Aprahamian., 2018; Brazil) [25] (1) | |
| ≥5 drugs | (Huang., 2018; Taiwan) [73] (3), (Hasan., 2018; Malaysia) [128] (3), (Arslan., 2023; Turkey) [180] (2) | (Aprahamian., 2018; Brazil) [25] (1), (Ye., 2022; Netherlands, Greece, Croatia, Spain, United Kingdom) [26] (2), (Kurnat-Thoma., 2022; USA) [37] (3), (Moon., 2019; South Korea) [46] (3), (Closs., 2016; Brazil) [77] (4), (Jung., 2016; Korea) [80] (8), (Gnjidic., 2012; Australia) [83] (8), (Cheung 2020; Hong Kong, Israel, European countries) [101] (10), #1716 (Badrkhahan 2023; Iran) [110] (3), (DeGodoiRezendeCostaMolino 2022; European countries: Basel, Berlin, Coimbra, Geneva, Innsbruck, Toulouse, and Zurich) [117] (3), (Thapaliya., 2021; Australia) [186] (3), (Setiati., 2021; Indonesia) [191] (3), (Jazbar., 2021; Slovenia) [209] (9), (Prieto-Contreras., 2023; Spain) [251] (8) | Positive |
| ≥6 drugs | (Kume., 2021; Japan) [36] (3) | (Aprahamian., 2018; Brazil) [25] (1), (Yuki 2018; Japan) [129] (8) | Positive |
| ≥8 drugs | (Pao., 2018; Taiwan) [221] (8) | (Hung., 2021; Taiwan) [189] (8) | |
| 5–9 drugs | (Chaouacha., 2022; Oman) [182] (4) | (Saum., 2017; Germany) [47] (5,6), (Reallon 2020; France) [105] (4), (Herr., 2015; France) [217] (3) | Positive |
| ≥5 drugs plus PIM | (Aprahamian., 2018; Brazil) [25] (1) | Positive | |
| Hyper-polypharmacy | |||
| ≥10 drugs | (Saum., 2017; Germany) [47] (5,6), (Gnjidic., 2012; Australia) [83] (8), (Herr., 2015; France) [217] (3) | Positive | |
| (≥5 drugs) and (≥10 drugs) | (Lockery., 2020; Australia, USA) [70] (3) | Positive | |
| (>9 drugs) | (Reallon 2020; France) [105] (4), (Chaouacha., 2022; Oman) [182] (4) | Positive | |
| Medication use | |||
| Number of medications | (Gnjidic 2012; Australia) [83] (8), (Woo., 2015; China) [234] (3) | Positive | |
| Medication for high blood pressure, coronary and other heart diseases, diabetes, joint and other pain, anxiety, depression and sleep problems, osteoporosis, chronic bronchitis, inflammation | (Jazbar., 2021; Austria, Germany, Sweden, Spain, Italy, France, Denmark, Switzerland, Belgium, Israel, Czech Republic, Luxembourg, Slovenia, and Estonia) [60] (3) | Positive | |
| Medication for high blood cholesterol | (Jazbar., 2021; Austria, Germany, Sweden, Spain, Italy, France, Denmark, Switzerland, Belgium, Israel, Czech Republic, Luxembourg, Slovenia, and Estonia) [60] (3) | Negative | |
| Use of sleep medication | (Arias-Fernández., 2021; Spain) [142] (8), (Mizuno., 2023; Japan) [171] (8), (Woo., 2015; China) [234] (3) | Positive | |
| Current statin users, < 1 years of statin medication use, 1–3 years of statin medication use, >3 years of statin medication use | (LaCroix., 2008; USA) [164] (4) | No association between dose and duration of statin use | |
| First- and second-generation anti-psychotics | (Gafoor., 2019; UK) [165] (9) | Positive | |
| Benzodiazepine use | (Mizuno., 2023; Japan) [171] (8) | Positive | |
| Metformin use | (Liu., 2023; China) [178] (1) | Positive | |
| Oral anti-diabetic drugs, insulin, antihypertensives, lipid-lowering drugs | (García-Esquinas., 2015; Spain) [226] (8) | No association | |
| Antidepressant users with depressive symptoms | (Lakey., 2012; USA) [223] (4) | Positive | |
| Prescription of oral anticoagulation, among those with non-valvular atrial fibrillation; use of DOAC vs. warfarin, among those receiving OAC | (Sanghai., 2022; USA) [195] (8) | Positive | |
| Drug Burden Index | (Gnjidic., 2012; Australia) [83] (8), (Hasan 2018; Malaysia) [128] (3), (Byrne., 2019; Ireland) [227] (3) | Positive | |
| Cumulative exposure to anticholinergic and sedative drugs (Drug Burden Index) | (Reallon 2020; France) [105] (11) | Positive | |
| PIMs | |||
| PIMs (2019 Beers Criteria) | (Lockery., 2020; Australia, USA) [70] (3) | Positive association | |
| PIMs (2015 Beers Criteria) | (Aprahamian., 2018; Brazil) [25] (1), (Hasan 2018; Malaysia) [128] (3) | (Muhlack., 2019; Germany) [51] (7) | No association |
| PIMs (2012 Beers Criteria) | (Bolina., 2019; Brazil) [45] (4) | Positive | |
| Beers Criteria to avoid cognitively impaired patients (BEERS dementia PIM) | (Muhlack., 2019; Germany) [51] (7) | Positive | |
| PRISCUS PIM | (Muhlack., 2019; Germany) [51] (7) | Positive | |
| EU (7) PIM | (Muhlack., 2019; Germany) [51] (7) | Positive | |
| Brazilian Consensus on PIMs for Older People | (Alves., 2020; Brazil) [71] (3) | Positive | |
| START/STOPP version 2 criteria | (Tampaki 2023; Greece) [91] (9), (Hasan 2018; Malaysia) [128] (3) | No association | |
| Anticholinergic burden | (Cheong., 2023; UK) [160] (8) | Positive | |
| Anticholinergic drug scale (ADS) score (>0) | (Lampela., 2016; Finland) [168] (8) | Positive | |
| Drug-related problems | |||
| Risk of MRPs | (Ye., 2022; Netherlands, Greece, Croatia, Spain, United Kingdom) [26] (2) | Positive | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharma, R.; Sharma, T.; McCready-Branch, B.; Chauhan, A.; Carter, C.; Park, S.; Hudani, I.; Choudhuri, P.; Patel, T. Medication Use by Older Adults with Frailty: A Scoping Review. Pharmacy 2025, 13, 170. https://doi.org/10.3390/pharmacy13060170
Sharma R, Sharma T, McCready-Branch B, Chauhan A, Carter C, Park S, Hudani I, Choudhuri P, Patel T. Medication Use by Older Adults with Frailty: A Scoping Review. Pharmacy. 2025; 13(6):170. https://doi.org/10.3390/pharmacy13060170
Chicago/Turabian StyleSharma, Rishabh, Tanaya Sharma, Brent McCready-Branch, Arshia Chauhan, Caitlin Carter, SooMin Park, Imra Hudani, Prapti Choudhuri, and Tejal Patel. 2025. "Medication Use by Older Adults with Frailty: A Scoping Review" Pharmacy 13, no. 6: 170. https://doi.org/10.3390/pharmacy13060170
APA StyleSharma, R., Sharma, T., McCready-Branch, B., Chauhan, A., Carter, C., Park, S., Hudani, I., Choudhuri, P., & Patel, T. (2025). Medication Use by Older Adults with Frailty: A Scoping Review. Pharmacy, 13(6), 170. https://doi.org/10.3390/pharmacy13060170






