The Medication Safety Adventure Trail: An Educational Intervention to Promote Public Awareness on Medication Safety
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Tool Design
2.3. Implementation of the Educational Tool
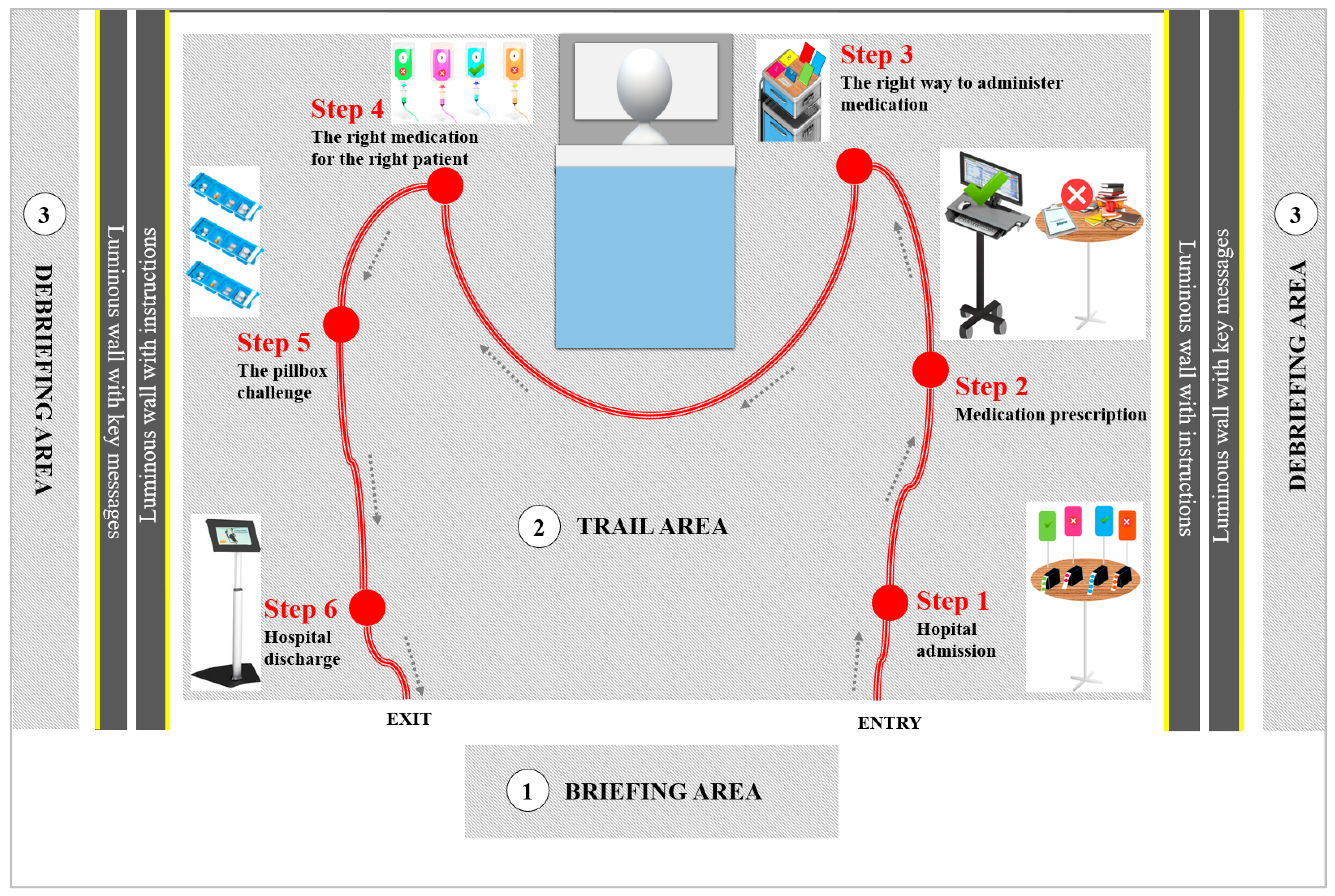
- A briefing area booth dedicated to welcoming participants and explaining the experiment;
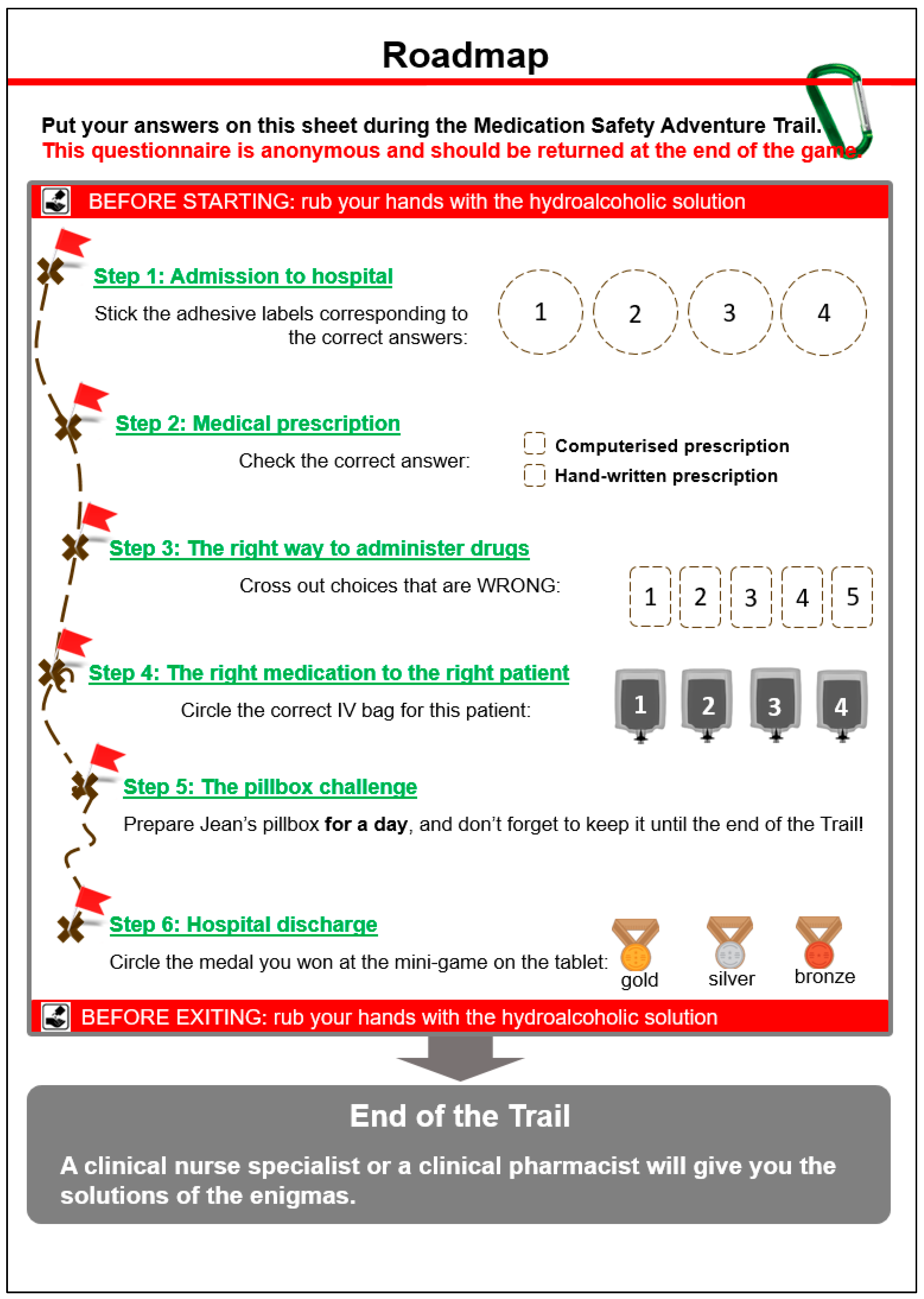
- A trail area recreating the environment of a patient’s room through which participants were guided using a rope and carabiner; along the trail, six steps from hospital admission to discharge were represented by interactive, playful content; at each step, participants had to solve an enigma about safe medication use and write the answer on their roadmap (Appendix A);
- Two debriefing areas where participants met a clinical pharmacist and/or a clinical nurse specialist after completing the trail to receive the correct answers to the quiz, ask any questions, and review the key safety messages.
2.4. Evaluation of the Tool
2.5. Knowledge and Degree of Certainty Assessment
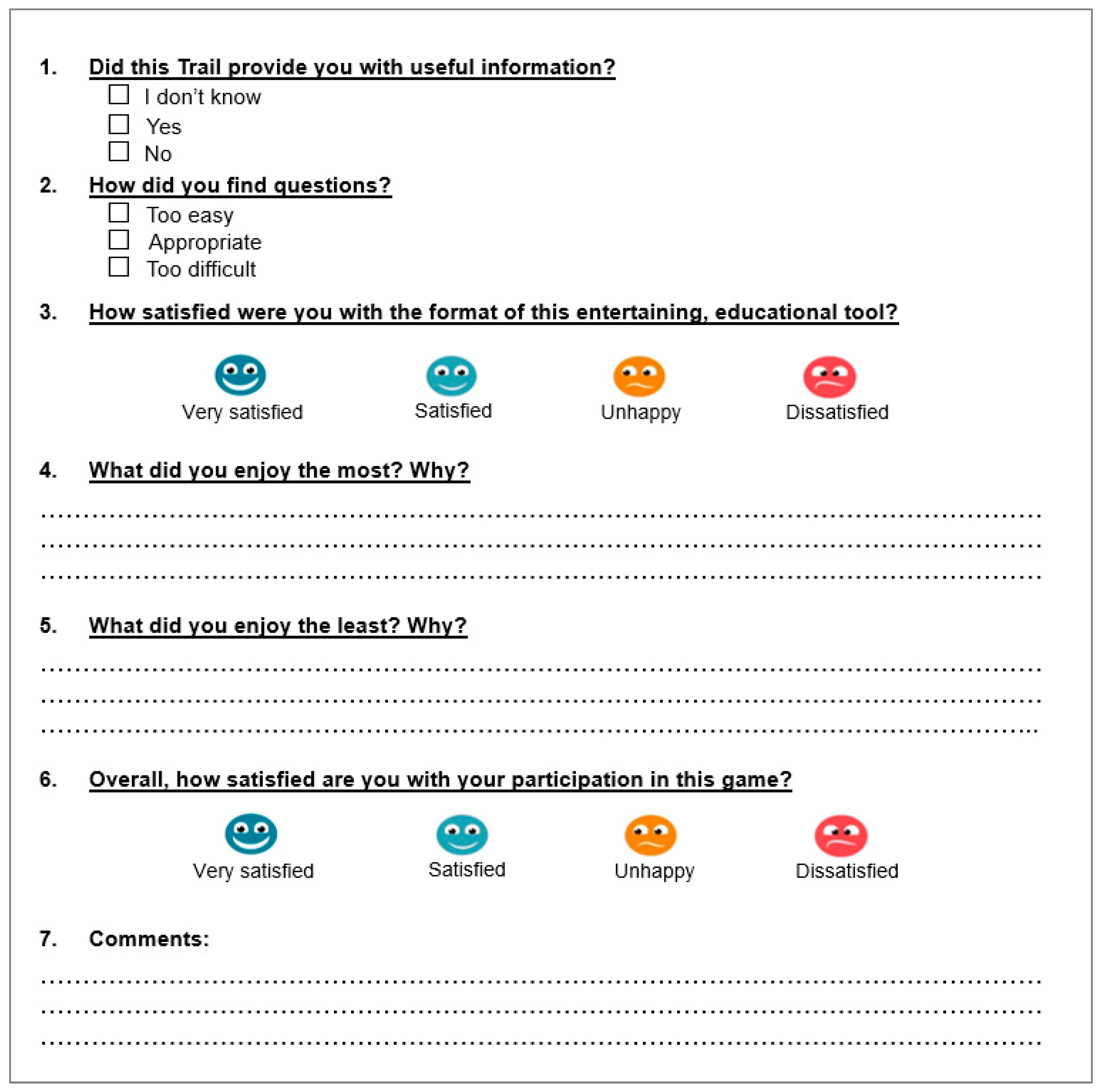
2.6. Satisfaction Assessment
2.7. Statistical Analysis
3. Results
3.1. Study Population
3.2. Knowledge and Degree of Certainty
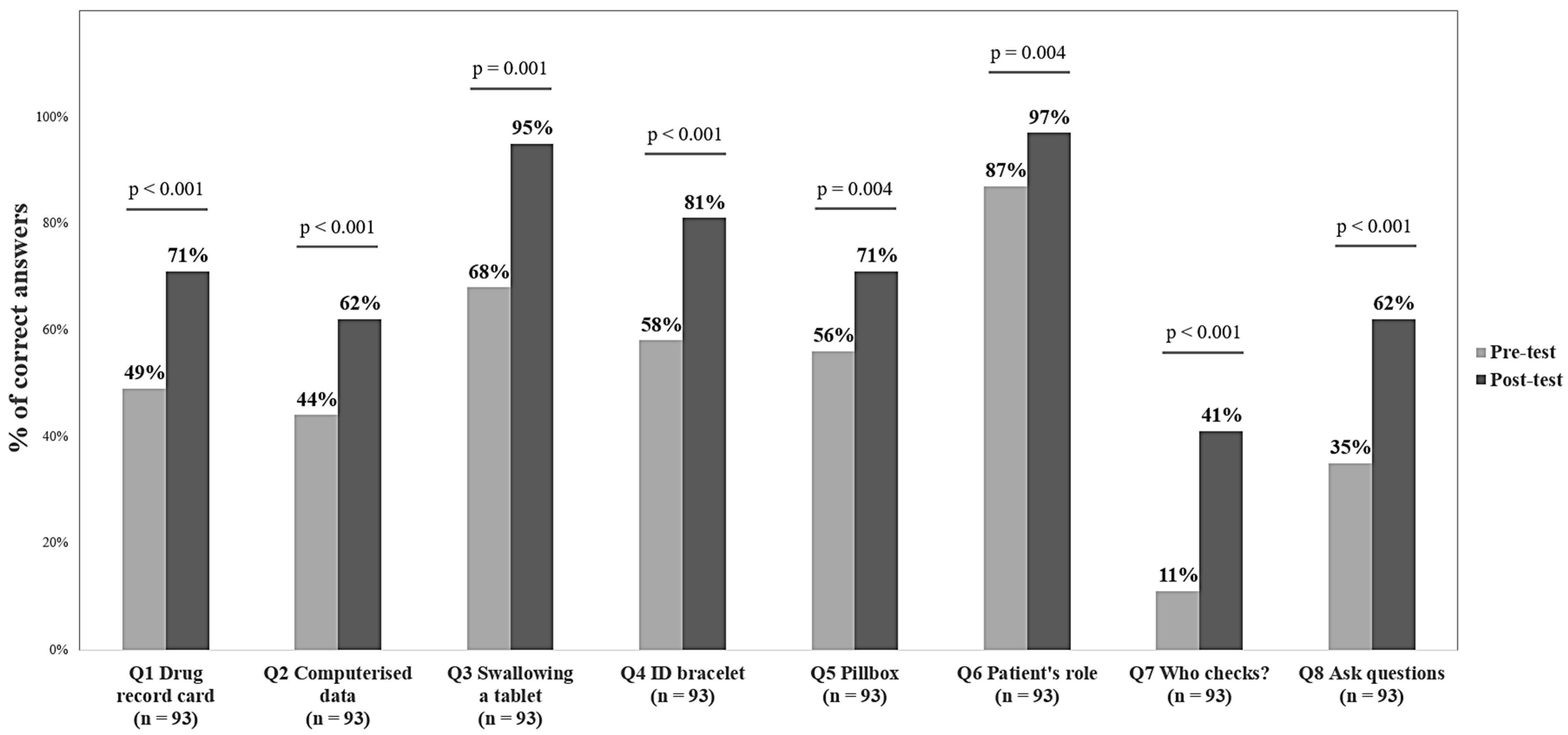
3.2.1. Comparison Between Pre-Tests and Post-Tests for All Participants
3.2.2. Comparison Between Healthcare Professionals and Other Participants
3.3. Satisfaction
4. Discussion
4.1. Summary of Results
4.2. The Tool’s Impact on Promoting Empowerment in Medication Safety
4.3. Strengths and Limitations
4.4. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ID | Identification |
| DC | Degree of certainty |
Appendix A. Roadmap
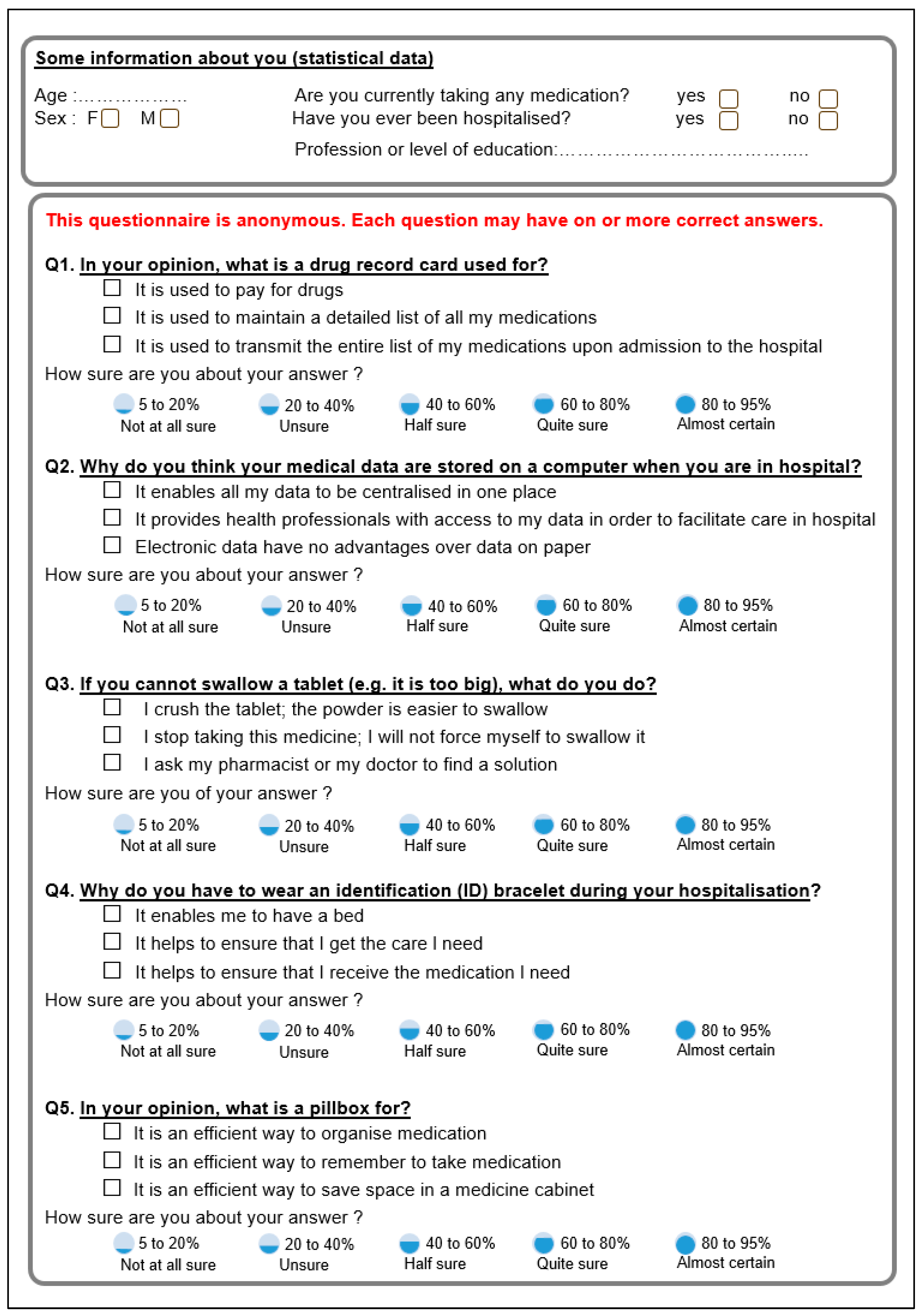
Appendix B. Pre-Test Questionnaire
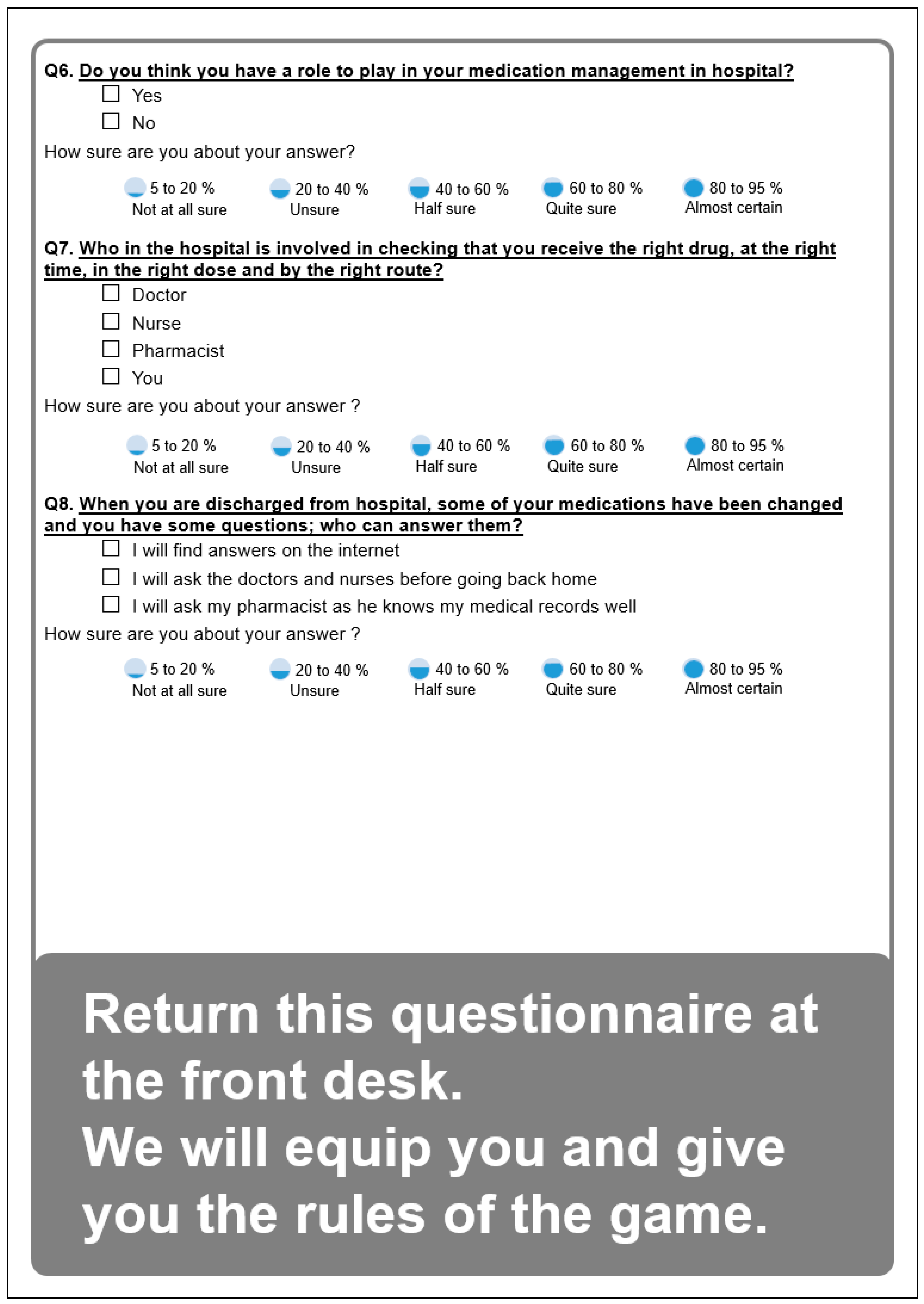
Appendix C. Roadmap Post-Test Satisfaction Questionnaire
References
- Medication Without Harm: Policy Brief, 1st ed.; World Health Organization: Geneva, Switzerland, 2024; ISBN 978-92-4-006276-4.
- World Health Organization. Medication Without Harm. Available online: https://www.who.int/initiatives/medication-without-harm (accessed on 31 March 2025).
- Radley, D.C.; Wasserman, M.R.; Olsho, L.E.; Shoemaker, S.J.; Spranca, M.D.; Bradshaw, B. Reduction in Medication Errors in Hospitals Due to Adoption of Computerized Provider Order Entry Systems. J. Am. Med. Inform. Assoc. 2013, 20, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Poon, E.G.; Keohane, C.A.; Yoon, C.S.; Ditmore, M.; Bane, A.; Levtzion-Korach, O.; Moniz, T.; Rothschild, J.M.; Kachalia, A.B.; Hayes, J.; et al. Effect of Bar-Code Technology on the Safety of Medication Administration. N. Engl. J. Med. 2010, 362, 1698–1707. [Google Scholar] [CrossRef]
- Sullivan, G.H. Five “Rights” Equal 0 Errors. RN 1991, 54, 65–67. [Google Scholar]
- Sallam, M.; Hamdan, A. Examining the Influence of Joint Commission International (JCI) Accreditation Surveys on Medication Safety Practices: A Cross-Sectional Study from Mediclinic Welcare Hospital in Dubai, UAE. J. Integr. Health 2023, 2, 68–73. [Google Scholar] [CrossRef]
- Jha, A.K.; Orav, E.J.; Zheng, J.; Epstein, A.M. Patients’ Perception of Hospital Care in the United States. N. Engl. J. Med. 2008, 359, 1921–1931. [Google Scholar] [CrossRef]
- World Health Organization. Patients for Patient Safety. Available online: https://www.who.int/initiatives/patients-for-patient-safety (accessed on 31 March 2025).
- Manary, M.P.; Boulding, W.; Staelin, R.; Glickman, S.W. The Patient Experience and Health Outcomes. N. Engl. J. Med. 2013, 368, 201–203. [Google Scholar] [CrossRef] [PubMed]
- Wandersman, A.; Alia, K.A.; Cook, B.; Ramaswamy, R. Integrating Empowerment Evaluation and Quality Improvement to Achieve Healthcare Improvement Outcomes. BMJ Qual. Saf. 2015, 24, 645–652. [Google Scholar] [CrossRef]
- Connolly, T.M.; Boyle, E.A.; MacArthur, E.; Hainey, T.; Boyle, J.M. A Systematic Literature Review of Empirical Evidence on Computer Games and Serious Games. Comput. Educ. 2012, 59, 661–686. [Google Scholar] [CrossRef]
- Pesare, E.; Roselli, T.; Corriero, N.; Rossano, V. Game-Based Learning and Gamification to Promote Engagement and Motivation in Medical Learning Contexts. Smart Learn. Environ. 2016, 3, 5. [Google Scholar] [CrossRef]
- Putz, L.-M.; Hofbauer, F.; Treiblmaier, H. Can Gamification Help to Improve Education? Findings from a Longitudinal Study. Comput. Hum. Behav. 2020, 110, 106392. [Google Scholar] [CrossRef]
- Doumas, I.; Everard, G.; Dehem, S.; Lejeune, T. Serious Games for Upper Limb Rehabilitation after Stroke: A Meta-Analysis. J. Neuroeng. Rehabil. 2021, 18, 100. [Google Scholar] [CrossRef] [PubMed]
- Martos-Cabrera, M.B.; Membrive-Jiménez, M.J.; Suleiman-Martos, N.; Mota-Romero, E.; Cañadas-De la Fuente, G.A.; Gómez-Urquiza, J.L.; Albendín-García, L. Games and Health Education for Diabetes Control: A Systematic Review with Meta-Analysis. Healthcare 2020, 8, 399. [Google Scholar] [CrossRef]
- Charlier, N.; Zupancic, N.; Fieuws, S.; Denhaerynck, K.; Zaman, B.; Moons, P. Serious Games for Improving Knowledge and Self-Management in Young People with Chronic Conditions: A Systematic Review and Meta-Analysis. J. Am. Med. Inform. Assoc. 2016, 23, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Maurin, K.D.; Girod, C.; Consolini, J.L.; Belzeaux, R.; Etain, B.; Cochet, B.; Leboyer, M.; Genty, C.; Gamon, L.; Picot, M.C.; et al. Use of a Serious Game to Strengthen Medication Adherence in Euthymic Patients with Bipolar Disorder Following a Psychoeducational Programme: A Randomized Controlled Trial. J. Affect. Disord. 2020, 262, 182–188. [Google Scholar] [CrossRef]
- Abraham, O.; LeMay, S.; Bittner, S.; Thakur, T.; Stafford, H.; Brown, R. Investigating Serious Games That Incorporate Medication Use for Patients: Systematic Literature Review. JMIR Serious Games 2020, 8, e16096. [Google Scholar] [CrossRef]
- Une Médication Sûre Lors de L’admission à L’hôpital. Available online: https://www.securitedespatients.ch/programmes-progress/la-securite-de-la-medication-aux-interfaces/#c1697 (accessed on 7 November 2020).
- Kirkpatrick, D.L.; Kirkpatrick, J.D. Evaluating Training Programs: The Four Levels, 3rd ed.; Berrett-Koehler: San Francisco, CA, USA, 2006; ISBN 978-1-57675-348-4. [Google Scholar]
- Leclercq, D. Une mata-analyse des degrés de certitude exprimés en mots. Evaluer J. Int. De Rech. En Educ. Et Form. 2017, 2, 69–105. [Google Scholar]
- Patientensicherheit Schweiz La Sécurité de la Médication aux Interfaces. Available online: https://patientensicherheit.ch/fr/programmes-nationaux/programmes-nationaux-de-mise-en-application/la-securite-de-la-medication-aux-interfaces/ (accessed on 31 March 2025).
- Wilke, D.; Schiek, S.; Knoth, H.; Bertsche, T. Medication Plans at Hospital Admission—A Multicentre Analysis Using Statutory Health Insurance Data. Dtsch. Med. Wochenschr. 2018, 143, e117–e124. [Google Scholar] [CrossRef]
- Chae, S.Y.; Chae, M.H.; Isaacson, N.; James, T.S. The Patient Medication List: Can We Get Patients More Involved in Their Medical Care? J. Am. Board Fam. Med. 2009, 22, 677–685. [Google Scholar] [CrossRef]
- Rizer, M.K.; Sieck, C.; Lehman, J.S.; Hefner, J.L.; Huerta, T.R.; McAlearney, A.S. Working with an Electronic Medical Record in Ambulatory Care: A Study of Patient Perceptions of Intrusiveness. Perspect. Health Inf. Manag. 2017, 14, 1g. [Google Scholar]
- Pearce, C.; Arnold, M.; Phillips, C.; Trumble, S.; Dwan, K. The Patient and the Computer in the Primary Care Consultation. J. Am. Med. Inform. Assoc. 2011, 18, 138–142. [Google Scholar] [CrossRef]
- de Jong, C.C.; Ros, W.J.G.; van Leeuwen, M.; Schrijvers, G. Exploring the Effects of Patients Taking a Vigilant Role in Collaborating on Their E-Medication Administration Record. Int. J. Med. Inform. 2016, 88, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Schwappach, D.L.B.; Wernli, M. Medication Errors in Chemotherapy: Incidence, Types and Involvement of Patients in Prevention. A Review of the Literature. Eur. J. Cancer Care 2010, 19, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Parand, A.; Faiella, G.; Franklin, B.D.; Johnston, M.; Clemente, F.; Stanton, N.A.; Sevdalis, N. A Prospective Risk Assessment of Informal Carers’ Medication Administration Errors within the Domiciliary Setting. Ergonomics 2018, 61, 104–121. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Pineda, A.; Gonzalez de Dios, J.; Guilabert Mora, M.; Mira-Perceval Juan, G.; Mira Solves, J.J. A Systematic Review on Pediatric Medication Errors by Parents or Caregivers at Home. Expert Opin. Drug Saf. 2022, 21, 95–105. [Google Scholar] [CrossRef]
- Mira, J.J.; Lorenzo, S.; Guilabert, M.; Navarro, I.; Pérez-Jover, V. A Systematic Review of Patient Medication Error on Self-Administering Medication at Home. Expert Opin. Drug Saf. 2015, 14, 815–838. [Google Scholar] [CrossRef]
- Pérez-Jover, V.; Mira, J.J.; Carratala-Munuera, C.; Gil-Guillen, V.F.; Basora, J.; López-Pineda, A.; Orozco-Beltrán, D. Inappropriate Use of Medication by Elderly, Polymedicated, or Multipathological Patients with Chronic Diseases. Int. J. Environ. Res. Public Health 2018, 15, 310. [Google Scholar] [CrossRef]
- Ryan, R.; Santesso, N.; Lowe, D.; Hill, S.; Grimshaw, J.; Prictor, M.; Kaufman, C.; Cowie, G.; Taylor, M. Interventions to Improve Safe and Effective Medicines Use by Consumers: An Overview of Systematic Reviews. Cochrane Database Syst. Rev. 2014, 2014, CD007768. [Google Scholar] [CrossRef]
- Oriol, P.; Fortier, É.; Grenier, D. The room of errors, fun and pedagogical. Rev. De L’infirmiere 2016, 221, 33–34. [Google Scholar] [CrossRef]
- Farnan, J.M.; Gaffney, S.; Poston, J.T.; Slawinski, K.; Cappaert, M.; Kamin, B.; Arora, V.M. Patient Safety Room of Horrors: A Novel Method to Assess Medical Students and Entering Residents’ Ability to Identify Hazards of Hospitalisation. BMJ Qual. Saf. 2016, 25, 153–158. [Google Scholar] [CrossRef]
- Backhouse, A.; Malik, M. Escape into Patient Safety: Bringing Human Factors to Life for Medical Students. BMJ Open Qual. 2019, 8, e000548. [Google Scholar] [CrossRef]
- Diemer, G.; Jaffe, R.; Papanagnou, D.; Zhang, X.C.; Zavodnick, J. Patient Safety Escape Room: A Graduate Medical Education Simulation for Event Reporting. MedEdPORTAL 2019, 15, 10868. [Google Scholar] [CrossRef] [PubMed]
- Veldkamp, A.; van de Grint, L.; Knippels, M.-C.P.J.; van Joolingen, W.R. Escape Education: A Systematic Review on Escape Rooms in Education. Educ. Res. Rev. 2020, 31, 100364. [Google Scholar] [CrossRef]
- Quek, L.H.; Tan, A.J.Q.; Sim, M.J.J.; Ignacio, J.; Harder, N.; Lamb, A.; Chua, W.L.; Lau, S.T.; Liaw, S.Y. Educational Escape Rooms for Healthcare Students: A Systematic Review. Nurse Educ. Today 2024, 132, 106004. [Google Scholar] [CrossRef] [PubMed]
- Chabrier, A.; Atkinson, S.; Bonnabry, P.; Bussières, J.-F. Utilisation Des Jeux d’évasion En Santé: Une Revue de Littérature. Can. J. Hosp. Pharm. 2019, 72, 388–402. [Google Scholar] [CrossRef]
| Safety Topics | Key Safety Messages |
|---|---|
| Admission to hospital |
|
| Medical prescription |
|
| The right way to administer medication |
|
| The right medication for the right patient |
|
| The pillbox challenge |
|
| Hospital discharge |
|
| Q1. What is a drug record card used for? |
| Q2. Why do you think your medical data are stored on a computer when you are in hospital? |
| Q3. If you cannot swallow a tablet (e.g., it is too big), what do you do? |
| Q4. Why do you have to wear an identification (ID) bracelet during your hospitalisation? |
| Q5. What is a pillbox for? |
| Q6. Do you think you have a role to play in your medication management in hospital? |
| Q7. Who in the hospital is involved in checking that you receive the right drug, at the right time, in the right dose and by the right route? |
| Q8. When you are discharged from hospital, some of your medications have been changed and you have questions; who can answer them? |
| Questions | Healthcare Professionals * (n = 35) | Other Participants * (n = 56) | ||||
|---|---|---|---|---|---|---|
| Pre-Test % (n) | Post-Test % (n) | p Value | Pre-Test % (n) | Post-Test % (n) | p Value | |
| Q1. Drug record card | 66 (23) | 89 (31) | 0.008 | 41 (23) | 59 (33) | 0.064 |
| Q2. Computerised data | 60 (21) | 71 (25) | 0.219 | 36 (20) | 57 (32) | 0.008 |
| Q3. Can’t swallow tablet | 83 (29) | 97 (34) | 0.125 | 59 (33) | 93 (52) | <0.001 |
| Q4. ID bracelet | 86 (30) | 89 (31) | 1 | 43 (24) | 75 (42) | <0.001 |
| Q5. Pillbox | 63 (22) | 71 (25) | 0.453 | 52 (29) | 71 (40) | 0.007 |
| Q6. Patient’s role | 57 (20) | 74 (26) | 0.109 | 84 (47) | 95 (53) | 0.031 |
| Q7. Who checks? | 23 (8) | 54 (19) | 0.001 | 4 (2) | 32 (18) | <0.001 |
| Q8. Ask questions | 94 (33) | 100 (35) | 0.500 | 23 (13) | 54 (30) | <0.001 |
| Number of correct answers, mean (SD) | 5.31 (1.94) | 6.46 (1.75) | <0.001 | 3.41 (1.92) | 5.36 (2.19) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Flornoy-Guédon, A.; Gschwind, L.; Poncet, A.; Chopard, P.; Fonzo-Christe, C.; Bonnabry, P. The Medication Safety Adventure Trail: An Educational Intervention to Promote Public Awareness on Medication Safety. Pharmacy 2025, 13, 75. https://doi.org/10.3390/pharmacy13030075
Flornoy-Guédon A, Gschwind L, Poncet A, Chopard P, Fonzo-Christe C, Bonnabry P. The Medication Safety Adventure Trail: An Educational Intervention to Promote Public Awareness on Medication Safety. Pharmacy. 2025; 13(3):75. https://doi.org/10.3390/pharmacy13030075
Chicago/Turabian StyleFlornoy-Guédon, Audrey, Liliane Gschwind, Antoine Poncet, Pierre Chopard, Caroline Fonzo-Christe, and Pascal Bonnabry. 2025. "The Medication Safety Adventure Trail: An Educational Intervention to Promote Public Awareness on Medication Safety" Pharmacy 13, no. 3: 75. https://doi.org/10.3390/pharmacy13030075
APA StyleFlornoy-Guédon, A., Gschwind, L., Poncet, A., Chopard, P., Fonzo-Christe, C., & Bonnabry, P. (2025). The Medication Safety Adventure Trail: An Educational Intervention to Promote Public Awareness on Medication Safety. Pharmacy, 13(3), 75. https://doi.org/10.3390/pharmacy13030075







