Prevalence and Determinants of Self-Medication Practices among Cardiovascular Patients from Béja, North West Tunisia: A Community-Pharmacy-Based Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Area, and Period
2.2. Source of Study Patients
2.3. Inclusion and Exclusion Criteria
- Inclusion criteria
- Exclusion criteria
2.4. Data Collection Procedure and Tool
- The investigators
- Study tool: the questionnaire
2.5. Variables Studied
- Independent variables: age, marital status, educational level, residence, employment status, socio-economic level, smoker status, alcohol intake, dietary practices, and physical activity.
- Dependent variable: self-medication practice (yes or no).
2.6. Operational Definition
2.7. Statistical Analyses
2.8. Ethical Considerations
3. Results
3.1. Prevalence of Self-Medication among Tunisian CV Patients
3.2. Socio-Demographic Characteristics and Lifestyle Habits of Study Participants
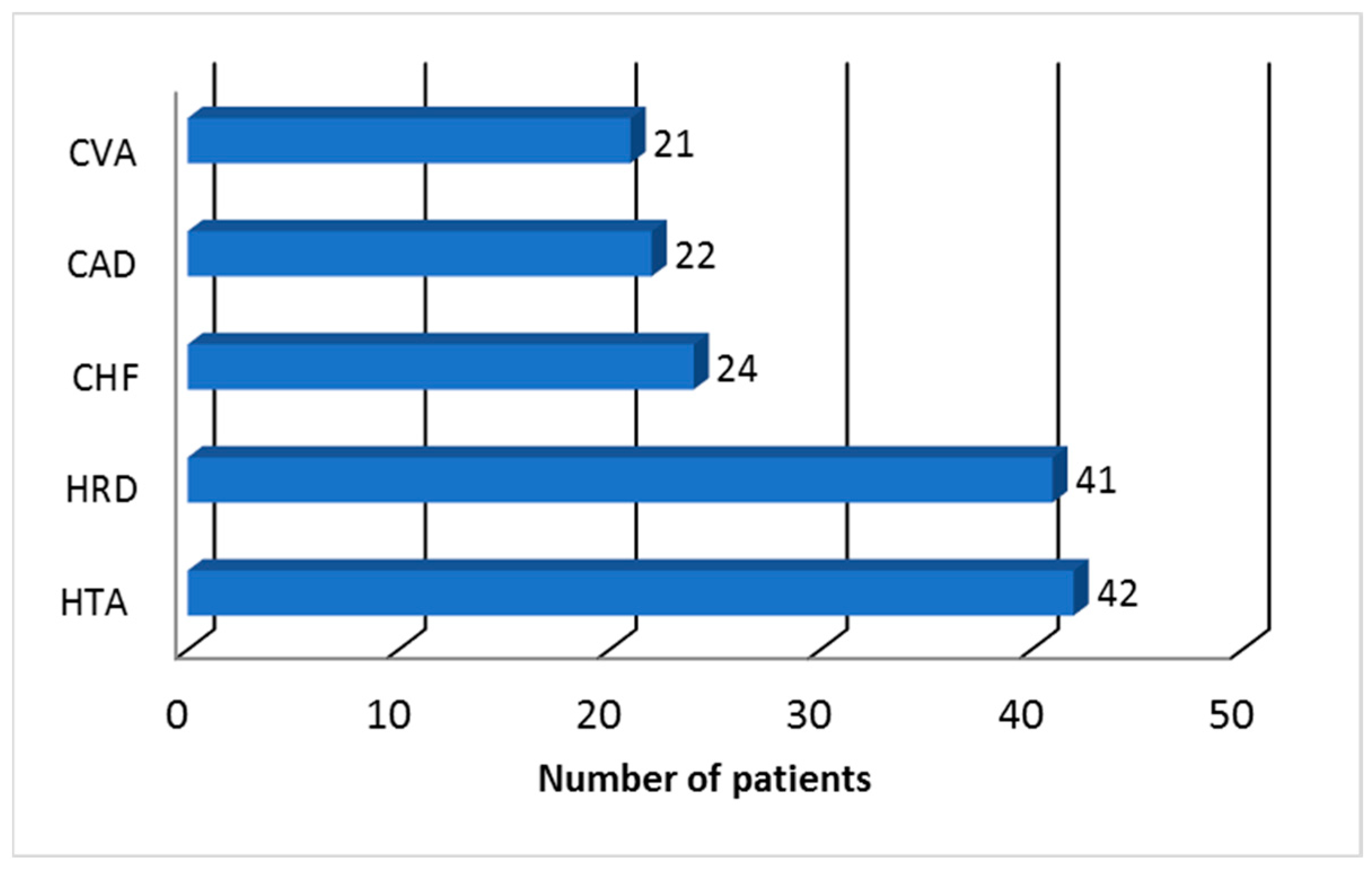
3.3. Cardiovascular History Profile of Tunisian Patients Who Practiced Self-Medication
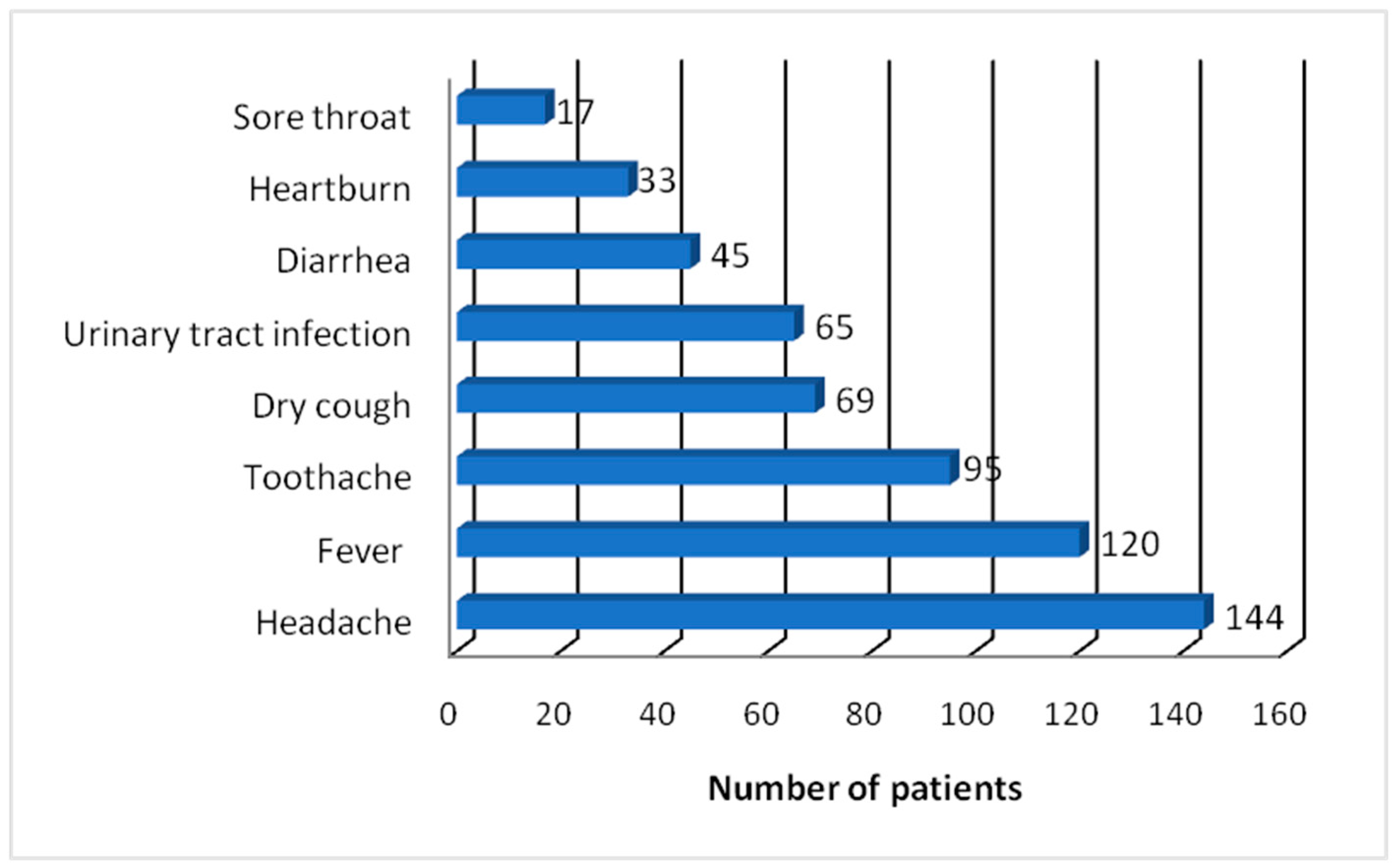
3.4. Reasons for Engaging in Self-Medication
3.5. Pharmacological Type of Medicine Used for Self-Medication
3.6. Factors Associated with Self-Medication Practice
4. Discussion
5. Recommendations for Healthcare Professionals
6. Strengths of the Current Study
7. Study Limitations
8. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ben Romdhane, H.; Khaldi, R.; Oueslati, A.; Skhiri, H. Transition Épidémiologique et Transition Alimentaire et Nutritionnelle En Tunisie. CIHEAM—Options Méditerr. 2002, 7–27. [Google Scholar]
- World Health Organization. The Top 10 Causes of Death. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death/ (accessed on 16 February 2024).
- Saleh, M. Main Causes of Death in Tunisia 2019. Available online: https://www.statista.com/statistics/1245703/mortality-rate-due-to-the-main-causes-of-death-in-tunisia/ (accessed on 16 February 2024).
- Ghannem, H.; Hadj Fredj, A. Epidemiology of Hypertension and Other Cardiovascular Disease Risk Factors in the Urban Population of Soussa, Tunisia. EMHJ—East. Mediterr. Health J. 1997, 3, 472–479. [Google Scholar] [CrossRef]
- Haj Amor, S.; Beaney, T.; Saidi, O.; Clarke, J.; Poulter, N.R.; Ben Alaya, N.; Ben Romdhane, H. May Measurement Month 2019: An Analysis of Blood Pressure Screening Results from Tunisia. Eur. Heart J. Suppl. 2021, 23, B144–B146. [Google Scholar] [CrossRef]
- Jemaa, R.; Razgallah, R.; Ben Ghorbel, I.; Rais, L.; Kallel, A. Prevalence of Cardiovascular Risk Factors in the Tunisian Population: The ATERA-Survey. Arch. Cardiovasc. Dis. Suppl. 2020, 12, 159. [Google Scholar] [CrossRef]
- World Health Organisation. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication; World Health Organisation: Geneva, Switzerland, 2000.
- Shrestha, A.B.; Aryal, M.; Magar, J.R.; Shrestha, S.; Hossainy, L.; Rimti, F.H. The Scenario of Self-Medication Practices during the COVID-19 Pandemic; a Systematic Review. Ann. Med. Surg. 2022, 82, 104482. [Google Scholar] [CrossRef]
- Almaqhawi, A.; Alhamad, M.; Albaqshi, B.; Alquraini, M.; Altaha, M.; Alhussain, H.; Alfayez, R.; Ibrahim Ali, S. Self-Medication Practices During the COVID-19 Pandemic Among the Adult Population in the Eastern Region of the Kingdom of Saudi Arabia. Cureus 2023, 15, e40505. [Google Scholar] [CrossRef]
- Feier, C.V.I.; Faur, A.M.; Muntean, C.; Blidari, A.; Contes, O.E.; Streinu, D.R.; Olariu, S. The Challenges of Gastric Cancer Surgery during the COVID-19 Pandemic. Healthcare 2023, 11, 1903. [Google Scholar] [CrossRef]
- Feier, C.V.I.; Bardan, R.; Muntean, C.; Olariu, A.; Olariu, S. Impact of the COVID-19 Pandemic on the Elective Surgery for Colorectal Cancer: Lessons to Be Learned. Medicina 2022, 58, 1322. [Google Scholar] [CrossRef]
- Asseray, N.; Ballereau, F.; Trombert-Paviot, B.; Bouget, J.; Foucher, N.; Renaud, B.; Roulet, L.; Kierzek, G.; Armand-Perroux, A.; Potel, G.; et al. Frequency and Severity of Adverse Drug Reactions Due to Self-Medication: A Cross-Sectional Multicentre Survey in Emergency Departments. Drug Saf. J. 2013, 36, 1159. [Google Scholar] [CrossRef]
- Shaghaghi, A.; Asadi, M.; Allahverdipour, H. Predictors of Self-Medication Behavior: A Systematic Review. Iran. J. Public Health 2014, 43, 136. [Google Scholar]
- Sparrow, R.T.; Khan, A.M.; Ferreira-Legere, L.E.; Ko, D.T.; Jackevicius, C.A.; Goodman, S.G.; Anderson, T.J.; Stacey, D.; Tiszovszky, I.; Farkouh, M.E.; et al. Effectiveness of Interventions Aimed at Increasing Statin-Prescribing Rates in Primary Cardiovascular Disease Prevention: A Systematic Review of Randomized Clinical Trials. JAMA Cardiol. 2019, 4, 1160–1169. [Google Scholar] [CrossRef]
- Ghodkhande, K.P.; Choudhari, S.G.; Gaidhane, A. Self-Medication Practices Among the Geriatric Population: A Systematic Literature Review. Cureus 2023, 15, e42282. [Google Scholar] [CrossRef]
- de Sanctis, V.; Soliman, A.T.; Daar, S.; Di Maio, S.; Elalaily, R.; Fiscina, B.; Kattamis, C. Prevalence, Attitude and Practice of Self-Medication among Adolescents and the Paradigm of Dysmenorrhea Self-Care Management in Different Countries. Acta Biomed. 2020, 91, 182–192. [Google Scholar] [CrossRef]
- Rahmawati, R.; Bajorek, B.V. Self-Medication among People Living with Hypertension: A Review. Fam. Pract. 2017, 34, 147–153. [Google Scholar] [CrossRef]
- Veliz-Rojas, L.; Mendoza-Parra, S.; Barriga, O.A.; Veliz-Rojas, L.; Mendoza-Parra, S.; Barriga, O.A. Automedicación En Usuarios Del Programa de Salud Cardiovascular En Una Comuna de Chile. Rev. Costarric. Salud Pública 2017, 26, 61–67. [Google Scholar]
- Ben Mabrouk, A.; Larbi Ammari, F.; Werdani, A.; Jemmali, N.; Chelli, J.; Mrabet, H.E.; Rassas, A.; Sfar, M.H.; El Mhamdi, S.; Mahjoub, B. Parental Self-Medication with Antibiotics in a Tunisian Pediatric Center. Therapie 2022, 77, 477–485. [Google Scholar] [CrossRef]
- Jemaa, F.C.; Khaldi, A.; Bessioud, L.; Borhene, J.; Akkad, T.; Ltaief, G. 1304 Self Medication in Children at the District of Tunis (Tunisia): Focus on Antibiotic Self Medication. Pediatr. Res. 2010, 68, 645. [Google Scholar] [CrossRef][Green Version]
- Brahim Salem, S. Determinants of Self-Medication Practice by Tunisians. World J. Pharm. Pharm. Sci. 2015, 4, 138–154. [Google Scholar]
- Béja—Wikipedia. Available online: https://en.wikipedia.org/wiki/B%C3%A9ja (accessed on 29 March 2024).
- Béja (Governorate, Tunisia)—Population Statistics, Charts, Map and Location. Available online: https://www.citypopulation.de/en/tunisia/admin/21__b%C3%A9ja/ (accessed on 29 March 2024).
- United Nations Educational Scientific and Cultural Organization (UNESCO). International Standard Classification of Education (ISCED); UNESCO: Montreal, QC, Canada, 2011. [Google Scholar]
- MedCalc Statistical Software—Free Trial. Available online: https://www.medcalc.org/ (accessed on 29 March 2024).
- Ministre de la Santé. Arrêté Du Ministre de La Santé Du 1er Juin 2015. J. Off. République Tunis. 2015, 1213–1262. Available online: http://www.dpm.tn/images/pdf/cc01012015fr.pdf (accessed on 12 February 2024).
- Ouertani, H.; Mkaouer, H.; Jegham, H.; Ben Amor, F.; Khattech-Tunisie, M.B. Enquête Sur l’automédication En Médecine Dentaire En Tunisie. Odonto-Stomatol. Trop. 2019, 42, 43–52. [Google Scholar]
- Sheikh-Taha, M.; Dimassi, H. Use of over the Counter Products in Older Cardiovascular Patients Admitted to a Tertiary Care Center in USA. BMC Geriatr. 2018, 18, 301. [Google Scholar] [CrossRef]
- Onchonga, D. A Google Trends Study on the Interest in Self-Medication during the 2019 Novel Coronavirus (COVID-19) Disease Pandemic. Saudi Pharm. J. SPJ 2020, 28, 903. [Google Scholar] [CrossRef]
- Flaherty, G.T.; Hession, P.; Liew, C.H.; Lim, B.C.W.; Leong, T.K.; Lim, V.; Sulaiman, L.H. COVID-19 in Adult Patients with Pre-Existing Chronic Cardiac, Respiratory and Metabolic Disease: A Critical Literature Review with Clinical Recommendations. Trop. Dis. Travel. Med. Vaccines 2020, 6, 16. [Google Scholar] [CrossRef]
- Shafie, M.; Eyasu, M.; Muzeyin, K.; Worku, Y.; Martín-Aragón, S. Prevalence and Determinants of Self-Medication Practice among Selected Households in Addis Ababa Community. PLoS ONE 2018, 13, e0194122. [Google Scholar] [CrossRef]
- Arrais, P.S.D.; Fernandes, M.E.P.; Pizzol, T.D.S.D.; Ramos, L.R.; Mengue, S.S.; Luiza, V.L.; Tavares, N.U.L.; Farias, M.R.; Oliveira, M.A.; Bertoldi, A.D. Prevalence of Self-Medication in Brazil and Associated Factors. Rev. Saude Publica 2016, 50 (Suppl. S2), 13s. [Google Scholar] [CrossRef]
- Woźniak-Holecka, J.; Grajek, M.; Siwozad, K.; Mazgaj, K.; Czech, E. Consumer Behavior in OTC Medicines Market. Przegląd Epidemiol. 2012, 66, 157–160. [Google Scholar]
- Aziz, M.M.; Masood, I.; Yousaf, M.; Saleem, H.; Ye, D.; Fang, Y. Pattern of Medication Selling and Self-Medication Practices: A Study from Punjab, Pakistan. PLoS ONE 2018, 13, e0194240. [Google Scholar] [CrossRef]
- Extavour, R.; Edwards, R. Non-prescription Medicine Use by Outpatients of a Hospital in North-central Trinidad Living with Hypertension, and the Potential Clinical Risks. Int. J. Pharm. Pract. 2008, 16, 287–293. [Google Scholar] [CrossRef]
- Neafsey, P.J.; Jarrín, O.; Luciano, S.; Coffman, M.J. Self-Medication Practices of Spanish-Speaking Older Adults in Hartford, Connecticut. Hisp. Health Care Int. 2007, 5, 169–179. [Google Scholar] [CrossRef]
- Neafsey, P.; Shellman, J. Adverse Self-Medication Practices Of Older Adults With Hypertension Attending Blood Pressure Clinics: Adverse Self-Medication Practices. Internet J. Ment. Health 2000, 1, 1–9. [Google Scholar]
- Scicluna, E.A.; Borg, M.A.; Gür, D.; Rasslan, O.; Taher, I.; Redjeb, S.B.; Elnassar, Z.; Bagatzouni, D.P.; Daoud, Z. Self-Medication with Antibiotics in the Ambulatory Care Setting within the Euro-Mediterranean Region; Results from the ARMed Project. J. Infect. Public Health 2009, 2, 189–197. [Google Scholar] [CrossRef]
- Suciu, M.; Suciu, L.; Vlaia, L.; Voicu, M.; Buda, V.; Drăgan, L.; Andor, M.; Vlaia, V.; Cristescu, C. Prevalence and the Patterns of Use of Non/-Steroidal Anti-Inflammatory Drugs (NSAIDs) and Paracetamol among the General Population. Farmacia 2019, 67, 337–345. [Google Scholar] [CrossRef]
- Severin, A.E.; Petitpain, N.; Scala-Bertola, J.; Latarche, C.; Yelehe-Okouma, M.; Di Patrizio, P.; Gillet, P. Good Use and Knowledge of Paracetamol (Acetaminophen) among Self-Medicated Patients: Prospective Study in Community Pharmacies. Therapie 2016, 71, 287–296. [Google Scholar] [CrossRef]
- Alchin, J.; Dhar, A.; Siddiqui, K.; Christo, P.J. Why paracetamol (acetaminophen) is a suitable first choice for treating mild to moderate acute pain in adults with liver, kidney or cardiovascular disease, gastrointestinal disorders, asthma, or who are older. Curr. Med. Res. Opin. 2022, 38, 811–825. [Google Scholar] [CrossRef]
- Dorji, T.; Gyeltshen, K.; Pongpirul, K. Rational Use of Paracetamol among Out-Patients in a Bhutanese District Hospital Bordering India: A Cross-Sectional Study. BMC Res. Notes 2018, 11, 660. [Google Scholar] [CrossRef]
- Analgesic Expert Group. Therapeutic Guidelines: Analgesic, 6th ed.; Therapeutic Guidelines Limited: West Melbourne, Australia, 2012. [Google Scholar]
- Moore, R.A.; Moore, N. Paracetamol and Pain: The Kiloton Problem. Eur. J. Hosp. Pharm. 2016, 23, 187–188. [Google Scholar] [CrossRef]
- Freo, U.; Ruocco, C.; Valerio, A.; Scagnol, I.; Nisoli, E. Paracetamol: A Review of Guideline Recommendations. J. Clin. Med. 2021, 10, 3420. [Google Scholar] [CrossRef]
- Fillingim, R.B. Sex, Gender, and Pain: Women and Men Really Are Different. Curr. Rev. Pain. 2000, 4, 24–30. [Google Scholar] [CrossRef]
- Ilhan, M.N.; Durukan, E.; Ilhan, S.Ö.; Aksakal, F.N.; Özkan, S.; Bumin, M.A. Self-Medication with Antibiotics: Questionnaire Survey among Primary Care Center Attendants. Pharmacoepidemiol. Drug Saf. 2009, 18, 1150–1157. [Google Scholar] [CrossRef]
- Alghanim, S. Self-Medication Practice among Patients in a Public Health Care System. East. Mediterr. Health J. 2011, 17, 409–416. [Google Scholar] [CrossRef]
- Fanelli, A.; Ghisi, D.; Aprile, P.L.; Lapi, F. Cardiovascular and Cerebrovascular Risk with Nonsteroidal Anti-Inflammatory Drugs and Cyclooxygenase 2 Inhibitors: Latest Evidence and Clinical Implications. Ther. Adv. Drug Saf. 2017, 8, 173–182. [Google Scholar] [CrossRef]
- Schjerning Olsen, A.M.; Fosbøl, E.L.; Lindhardsen, J.; Andersson, C.; Folke, F.; Nielsen, M.B.; Køber, L.; Hansen, P.R.; Torp-Pedersen, C.; Gislason, G.H. Cause-Specific Cardiovascular Risk Associated with Nonsteroidal Anti-Inflammatory Drugs among Myocardial Infarction Patients—A Nationwide Study. PLoS ONE 2013, 8, e54309. [Google Scholar] [CrossRef]
- European Medicines Agency. PRAC Recommends the Same Cardiovascular Precautions for Diclofenac as for Selective COX-2 Inhibitors. 2013. Available online: https://www.ema.europa.eu/en/news/prac-recommends-same-cardiovascular-precautions-diclofenac-selective-cox-2-inhibitors (accessed on 16 February 2024).
- Berhouma, L.; Besbes, A.; Chokri, A.; Selmi, J. Survey on Tunisian Dentists’ Anti-Inflammatory Drugs’ Prescription in Dental Practice. Sci. World J. 2021, 2021, 6633870. [Google Scholar] [CrossRef]
- Buda, V.; Prelipcean, A.; Cristescu, C.; Roja, A.; Dalleur, O.; Andor, M.; Danciu, C.; Ledeti, A.; Dehelean, C.A.; Cretu, O. Prescription Habits Related to Chronic Pathologies of Elderly People in Primary Care in the Western Part of Romania: Current Practices, International Recommendations, and Future Perspectives Regarding the Overuse and Misuse of Medicines. Int. J. Environ. Res. Public Health 2021, 18, 7043. [Google Scholar] [CrossRef]
- Suciu, M.; Suciu, L.; Vlaia, L.; Voicu, M.; Buda, V.; Drăgan, L.; Andor, M.; Vlaia, V.; Cristescu, C.; Hîrjău, M. The Prevalence of Inappropriate Use of Nsaids by Cardiovascular Patients for Musculoskeletal Disorders. Farmacia 2020, 68, 628–639. [Google Scholar] [CrossRef]
- Buda, V.; Prelipcean, A.; Andor, M.; Dehelean, L.; Dalleur, O.; Buda, S.; Spatar, L.; Mabda, M.C.; Suciu, M.; Danciu, C.; et al. Potentially Inappropriate Prescriptions in Ambulatory Elderly Patients Living in Rural Areas of Romania Using STOPP/START (Version 2) Criteria. Clin. Interv. Aging 2020, 15, 407. [Google Scholar] [CrossRef]
- Kretchy, I.A.; Owusu-Daaku, F.; Danquah, S. Patterns and Determinants of the Use of Complementary and Alternative Medicine: A Cross-Sectional Study of Hypertensive Patients in Ghana. BMC Complement. Altern. Med. 2014, 14, 44. [Google Scholar] [CrossRef]
- Osamor, P.E.; Owumi, B.E. Complementary and Alternative Medicine in the Management of Hypertension in an Urban Nigerian Community. BMC Complement. Altern. Med. 2010, 10, 36. [Google Scholar] [CrossRef]
- Taylor, F.R. Tobacco, Nicotine, and Headache. Headache 2015, 55, 1028–1044. [Google Scholar] [CrossRef]
- Carrasco-Garrido, P.; de Andrés, A.L.; Barrera, V.H.; Jiménez-Trujillo, I.; Fernandez-de-las-Peñas, C.; Palacios-Ceña, D.; García-Gómez-Heras, S.; Jiménez-García, R. Predictive Factors of Self-Medicated Analgesic Use in Spanish Adults: A Cross-Sectional National Study. BMC Pharmacol. Toxicol. 2014, 15, 36. [Google Scholar] [CrossRef]
- Hagen, K.; Linde, M.; Steiner, T.J.; Stovner, L.J.; Zwart, J.A. Risk Factors for Medication-Overuse Headache: An 11-Year Follow-up Study. The Nord-Trøndelag Health Studies. Pain 2012, 153, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Hachfi, W.; Kaabia, N.; Bougmiza, I.; Bellazreg, F.; Hattab, Z.; Ben Lasfar, N.; Bahri, F.; Letaief, A. Prescribing Practices of Fluoroquinolones in Tunisia. Rev. Medicale Liege 2011, 66, 205–208. [Google Scholar]
- Schytz, H.W.; Amin, F.M.; Jensen, R.H.; Carlsen, L.; Maarbjerg, S.; Lund, N.; Aegidius, K.; Thomsen, L.L.; Bach, F.W.; Beier, D.; et al. Reference Programme: Diagnosis and Treatment of Headache Disorders and Facial Pain. Danish Headache Society, 3rd Edition, 2020. J. Headache Pain 2021, 22, 22. [Google Scholar] [CrossRef]
- Van Hout, M.C.; Norman, I. Misuse of Non-Prescription Codeine Containing Products: Recommendations for Detection and Reduction of Risk in Community Pharmacies. Int. J. Drug Policy 2016, 27, 17–22. [Google Scholar] [CrossRef]
| Variables | Category | SMP Yes (n = 144; 96%) | SMP No (n = 6; 4%) | OR (95% CI) p-Value |
|---|---|---|---|---|
| Socio-demographic characteristics | ||||
| Gender | Female | 49 | 5 | 1 (reference) |
| Male | 95 | 1 | 9.69 (1.10 to 85.29) p = 0.04 * | |
| Age group | 20–39 years | 49 | 1 | 1 (reference) |
| 40–59 years | 28 | 2 | 0.29 (0.02 to 3.29) p = 0.31 | |
| 60–69 years | 40 | 2 | 0.41 (0.04 to 4.67) p = 0.47 | |
| 70–79 years | 27 | 1 | 0.55 (0.03 to 9.16) p = 0.68 | |
| Marital status | married | 18 | 2 | 1 (reference) |
| divorced | 31 | 1 | 3.44 (0.29 to 40.71) p = 0.33 | |
| widowed | 67 | 1 | 7.44 (0.64 to 86.81) p = 0.11 | |
| Single | 28 | 2 | 1.56 (0.20 to 12.05) p = 0.67 | |
| Level of education | Low | 44 | 1 | 6.77 (0.72 to 63.86) p = 0.09 |
| Moderate | 74 | 1 | 11.38 (1.22 to 106.56) p = 0.03 * | |
| High | 26 | 4 | 1 (reference) | |
| Residence | Urban | 104 | 1 | 13.00 (1.47 to 114.75) p = 0.02 * |
| Rural | 40 | 5 | 1 (reference) | |
| Employment status | Retired | 45 | 1 | 2.27 (0.26 to 20.02) p = 0.46 |
| Self-employed | 35 | 1 | 1.61 (0.18 to 14.21) p = 0.67 | |
| Housewife | 24 | 1 | 1.00 (0.11 to 8.95) p = 1.00 | |
| Employed | 14 | 1 | 0.54 (0.06 to 4.94) p = 0.58 | |
| Student | 5 | - | - | |
| Trader | 13 | 1 | 0.50 (0.05 to 4.58) p = 0.54 | |
| Farmer | 9 | 1 | 0.33 (0.04 to 3.16) p = 0.34 | |
| Socio-economic level | Lower | 76 | 1 | 13.41 (1.31 to 136.95) p = 0.03 * |
| Moderate | 51 | 2 | 4.50 (0.69 to 29.24) p = 0.12 | |
| High | 17 | 3 | 1 (reference) | |
| Patient’s lifestyle habits | ||||
| Smoker status | smoking | 111 | 2 | 6.73 (1.18 to 38.38) p = 0.03 * |
| non-smoker | 33 | 4 | 1 (reference) | |
| Alcohol intake | Yes | 53 | 2 | 1.16 (0.21 to 6.58) p = 0.86 |
| No | 91 | 4 | 1 (reference) | |
| Dietary practices | Yes | 85 | 1 | 7.20 (0.82 to 63.25) p = 0.07 |
| No | 59 | 5 | 1 (reference) | |
| Physical activity | Yes | 60 | 2 | 1.43 (0.25 to 8.05) p = 0.69 |
| No | 84 | 4 | 1 (reference) | |
| Items | Frequency of Subjects Surveyed | Percentage |
|---|---|---|
| I have an old prescription | 101 | 70.14% |
| I save time | 62 | 43.06% |
| Medical fees are high | 52 | 36.11% |
| The physician is busy with a lot of patients | 32 | 22.22% |
| The physician/clinic is too far from me | 27 | 18.75% |
| Pharmacological Classes of Drugs Used as Self-Medication | Frequency | Percentage |
|---|---|---|
| Analgesics | 144 | 100% |
| Paracetamol | 86 | 59.72% |
| Paracetamol + caffeine | 45 | 31.25% |
| Paracetamol + codeine | 13 | 9.03% |
| Non-steroidal anti-inflammatory drugs (NSAIDs) | 63 | 43.75% |
| Ibuprofen | 26 | 18.06% |
| Diclofenac | 20 | 13.89% |
| Acetylsalicylic acid | 17 | 11.81% |
| Antibiotics | 82 | 56.94% |
| Ciprofloxacin | 25 | 17.36% |
| Amoxicillin + clavulanic acid | 35 | 24.31% |
| Gentamicin | 22 | 15.28% |
| Cough suppressants | 69 | 47.92% |
| Codeine | ||
| Antacids | 33 | 22.92% |
| Sodium alginate + sodium bicarbonate | ||
| Antidiarrheals | 45 | 31.25% |
| Birth control pills | 20 | 13.89% |
| Variables | Category | SMP Yes (144) | SMP No (6) | p-Value a |
|---|---|---|---|---|
| Gender | Female | 49 | 5 | 0.023 * |
| Male | 95 | 1 | ||
| Age group | Under 60 years | 77 | 3 | 1 |
| Over 60 years | 67 | 3 | ||
| Marital status | Married | 18 | 2 | 0.1825 |
| b Unmarried | 126 | 4 | ||
| Education | <High level | 118 | 2 | 0.0149 * |
| High level | 26 | 4 | ||
| Residence | Urban | 104 | 1 | 0.0095 * |
| Rural | 40 | 5 | ||
| Employment status | Employed | 14 | 1 | 0.4746 |
| Unemployed | 130 | 5 | ||
| Socio-economic status | <High level | 127 | 3 | 0.0315 * |
| High level | 17 | 3 |
| Variables | Category | SMP Yes (144) | SMP No (6) | p-Value a |
|---|---|---|---|---|
| Smoker status | Smoking | 111 | 2 | 0.0328 * |
| Non-smoker | 33 | 4 | ||
| Alcohol intake | Yes | 53 | 2 | 1 |
| No | 91 | 4 | ||
| Dietary practices | Yes | 85 | 1 | 0.084 |
| No | 59 | 5 | ||
| Physical activity | Yes | 60 | 2 | 1 |
| No | 84 | 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suciu, M.; Vlaia, L.; Boujneh, E.; Suciu, L.; Buda, V.O.; Jianu, N.; Vlaia, V.; Cristescu, C. Prevalence and Determinants of Self-Medication Practices among Cardiovascular Patients from Béja, North West Tunisia: A Community-Pharmacy-Based Survey. Pharmacy 2024, 12, 68. https://doi.org/10.3390/pharmacy12020068
Suciu M, Vlaia L, Boujneh E, Suciu L, Buda VO, Jianu N, Vlaia V, Cristescu C. Prevalence and Determinants of Self-Medication Practices among Cardiovascular Patients from Béja, North West Tunisia: A Community-Pharmacy-Based Survey. Pharmacy. 2024; 12(2):68. https://doi.org/10.3390/pharmacy12020068
Chicago/Turabian StyleSuciu, Maria, Lavinia Vlaia, Eya Boujneh, Liana Suciu, Valentina Oana Buda, Narcisa Jianu, Vicențiu Vlaia, and Carmen Cristescu. 2024. "Prevalence and Determinants of Self-Medication Practices among Cardiovascular Patients from Béja, North West Tunisia: A Community-Pharmacy-Based Survey" Pharmacy 12, no. 2: 68. https://doi.org/10.3390/pharmacy12020068
APA StyleSuciu, M., Vlaia, L., Boujneh, E., Suciu, L., Buda, V. O., Jianu, N., Vlaia, V., & Cristescu, C. (2024). Prevalence and Determinants of Self-Medication Practices among Cardiovascular Patients from Béja, North West Tunisia: A Community-Pharmacy-Based Survey. Pharmacy, 12(2), 68. https://doi.org/10.3390/pharmacy12020068






