Vaccination Training for Pharmacy Undergraduates as a Compulsory Part of the Curriculum?—A Multicentric Observation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Training Course
2.3. Instruments
2.3.1. High-Fidelity Simulator
2.3.2. Self-Assessment Questionnaire
2.3.3. Satisfaction Questionnaire
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
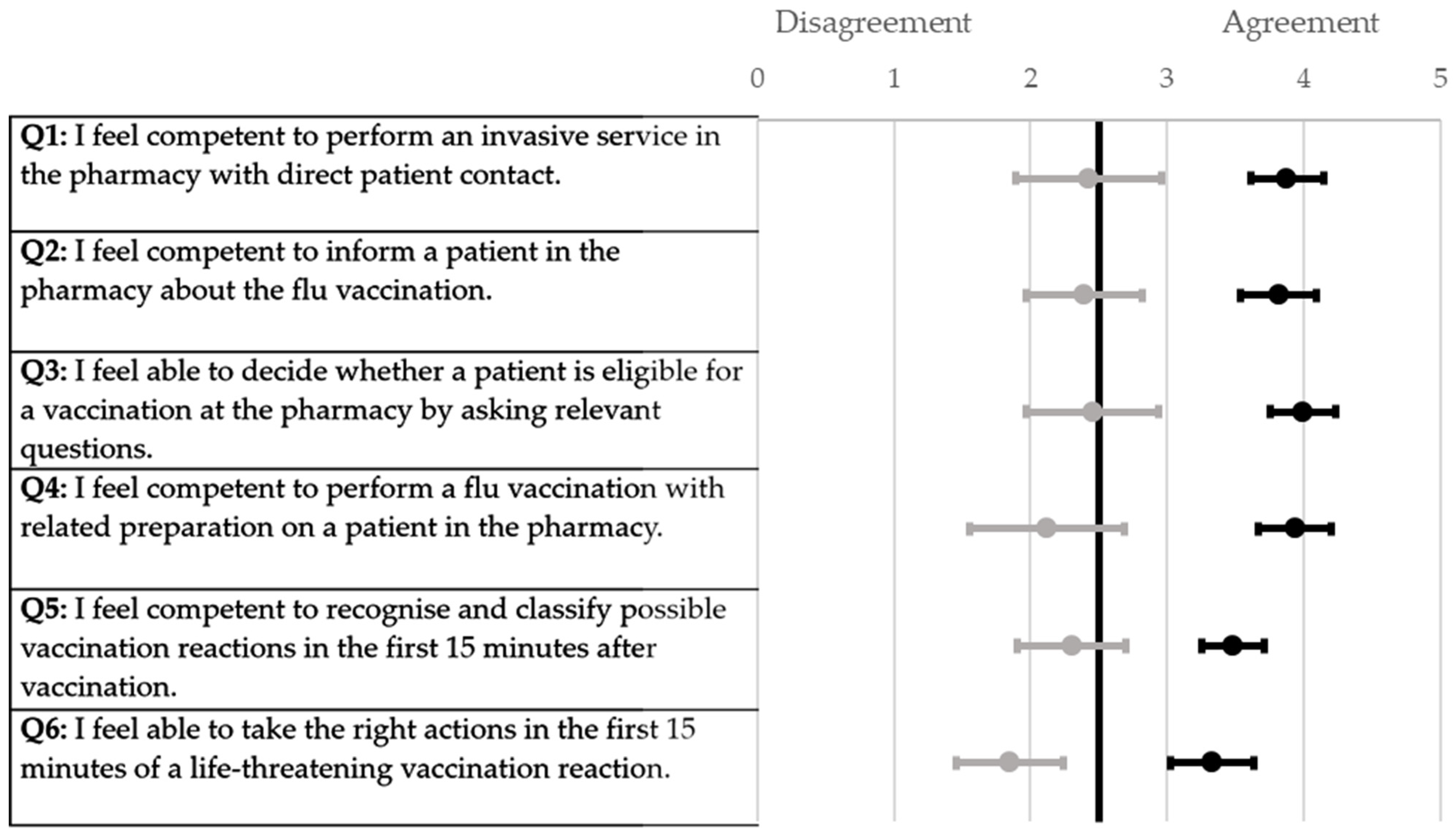
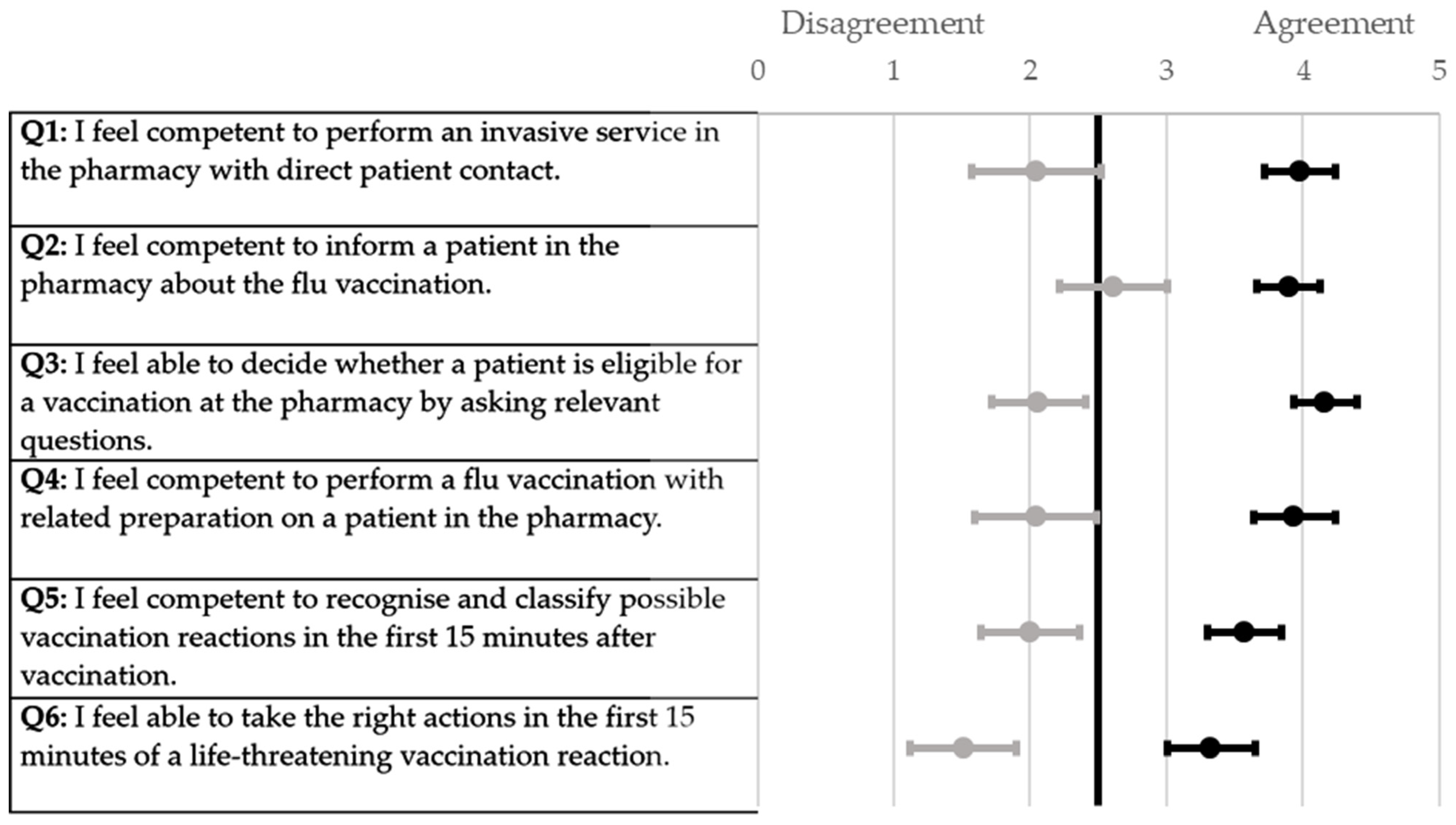
3.2. Self-Assessment Questionnaire
3.3. Satisfaction Questionnaire
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- ABDA. Grippeschutzimpfungen. Available online: https://www.abda.de/themen/grippeschutzimpfungen/ (accessed on 22 August 2023).
- Infektionsschuztzgesetz, Infection Protection Act of 20 July 2000 (Federal Law Gazette I p. 1045), last amended by Article 8v of the Act of 12 December 2023 (Federal Law Gazette 2023 I No. 359).
- ABDA. COVID-19 Vaccinations in Pharmacies Start on 8 February: Press Release. Available online: https://www.abda.de/aktuelles-und-presse/newsroom/detail/covid-19-impfungen-in-apotheken-starten-am-8-februar/ (accessed on 17 October 2023).
- International Pharmaceutical Federation. An Overview of Current Pharmacy Impact on Immunisation: A Global Report 2016. Available online: https://www.fip.org/files/fip/publications/FIP_report_on_Immunisation.pdf (accessed on 16 August 2022).
- World Health Organization. Seasonal Influenza Vaccines: An Overview for Decision-Makers. Available online: https://apps.who.int/iris/bitstream/handle/10665/336951/9789240010154-eng.pdf (accessed on 30 August 2022).
- Community Pharmacy England. Flu Vaccination—Statistics. Available online: https://cpe.org.uk/national-pharmacy-services/advanced-services/flu-vaccination-service/flu-vaccination-statistics/ (accessed on 22 August 2023).
- Nuffield Trust. Adult Flu Vaccination Coverage. Available online: https://www.nuffieldtrust.org.uk/resource/adult-flu-vaccination-coverage (accessed on 22 August 2023).
- The Pharmaceutical Society of Ireland. Report on the Evaluation of the Seasonal Influenza Vaccination Service in Pharmacy 2014/2015. 2015. Available online: https://www.thepsi.ie/Libraries/Pharmacy_Practice/PSI_2014_15_Report_on_Seasonal_Influenza_Vaccination_Service.sflb.ashx (accessed on 18 August 2022).
- Czech, M.; Balcerzak, M.; Antczak, A.; Byliniak, M.; Piotrowska-Rutkowska, E.; Drozd, M.; Juszczyk, G.; Religioni, U.; Vaillancourt, R.; Merks, P. Flu Vaccinations in Pharmacies-A Review of Pharmacists Fighting Pandemics and Infectious Diseases. Int. J. Environ. Res. Public Health 2020, 17, 7945. [Google Scholar] [CrossRef] [PubMed]
- Eurostat. Flu Vaccinations at Age 65 and Over. Available online: https://ec.europa.eu/eurostat/databrowser/view/HLTH_PS_IMMU/bookmark/table?lang=de&bookmarkId=8b35002c-47c2-4ac3-8a01-7dc03aa42d05 (accessed on 22 August 2023).
- Ecarnot, F.; Crepaldi, G.; Juvin, P.; Grabenstein, J.; Del Giudice, G.; Tan, L.; O‘Dwyer, S.; Esposito, S.; Bosch, X.; Gavazzi, G.; et al. Pharmacy-based interventions to increase vaccine uptake: Report of a multidisciplinary stakeholders meeting. BMC Public Health 2019, 19, 1698. [Google Scholar] [CrossRef] [PubMed]
- Isenor, J.E.; Edwards, N.T.; Alia, T.A.; Slayter, K.L.; MacDougall, D.M.; McNeil, S.A.; Bowles, S.K. Impact of pharmacists as immunizers on vaccination rates: A systematic review and meta-analysis. Vaccine 2016, 34, 5708–5723. [Google Scholar] [CrossRef] [PubMed]
- Kelling, S.E. Exploring Accessibility of Community Pharmacy Services. Innov. Pharm. 2015, 6, 210. [Google Scholar] [CrossRef]
- ABDA. Apothekendichte im Europäischen Vergleich (Pharmacy Density in European Comparison). Available online: https://www.abda.de/fileadmin/user_upload/assets/ZDF/ZDF21/ZDF_21_86_Apothekendichte_im_europaeischen_Vergleich.pdf (accessed on 27 December 2023).
- International Pharmaceutical Federation. Community Pharmacy at a Glance: Regulation, Scope of Practice, Remuneration, and Distribution of Medicines through Community Pharmacy Premises and Other Outlets. Available online: https://www.fip.org/file/5015 (accessed on 27 December 2023).
- International Pharmaceutical Federation. Supporting Life-Course Immunisation through Pharmacy-Based Vaccination: Enabling Equity, Access and Sustainability: A Toolkit for Pharmacist. Available online: https://www.fip.org/file/5588 (accessed on 26 October 2023).
- Singh, G.; Kleanthous, V.; Slade, S. How vaccination training for pharmacy students can help solve the current NHS workforce crisis. Pharm. J. 2022, 309, 3965. [Google Scholar] [CrossRef]
- International Pharmaceutical Federation. An Overview of Pharmacy’s Impact on Immunisation Coverage: A Global Survey: The Hague 2020. Available online: https://www.fip.org/file/4751 (accessed on 16 August 2023).
- Benkert, T. Symposium “Vaccination in Pharmacies”. 21 March 2023. Available online: https://www.abda.de/fileadmin/user_upload/assets/Pressetermine/2023/BAK-Symposium_2023/BAK-Symposium-2023-Benkert.pdf (accessed on 27 October 2023).
- Korayem, G.B.; Alshaya, O.A.; Kurdi, S.M.; Alnajjar, L.I.; Badr, A.F.; Alfahed, A.; Cluntun, A. Simulation-Based Education Implementation in Pharmacy Curriculum: A Review of the Current Status. Adv. Med. Educ. Pract. 2022, 13, 649–660. [Google Scholar] [CrossRef] [PubMed]
- Sayyed, S.A.; Sharkas, A.R.; Ali Sherazi, B.; Dabidian, A.; Schwender, H.; Laeer, S. Development and Assessment of Innovative High-Fidelity Simulation Vaccination Course Integrating Emergency Cases for Pharmacy Undergraduates—A Randomized Controlled Study. Vaccines 2023, 11, 324. [Google Scholar] [CrossRef]
- Microsoft Corporation. Microsoft Excel 2019; Microsoft Corporation: Redmond, WA, USA, 2019. [Google Scholar]
- OriginLab Corporation. Origin(Pro); OriginLab Corporation: Northampton, MA, USA, 2021. [Google Scholar]
- Qualtrics. Qualtrics; Qualtrics: Provo, UT, USA, 2005. [Google Scholar]
- Bushell, M.; Frost, J.; Deeks, L.; Kosari, S.; Hussain, Z.; Naunton, M. Evaluation of Vaccination Training in Pharmacy Curriculum: Preparing Students for Workforce Needs. Pharmacy 2020, 8, 151. [Google Scholar] [CrossRef]
- Mills, S.; Emmerton, L.; Sim, T.F. Immunization training for pharmacy students: A student-centered evaluation. Pharm. Pract. 2021, 19, 2427. [Google Scholar] [CrossRef]
- Marcum, Z.A.; Maffeo, C.M.; Kalsekar, I. The impact of an immunization training certificate program on the perceived knowledge, skills and attitudes of pharmacy students toward pharmacy-based immunizations. Pharm. Pract. 2010, 8, 103–108. [Google Scholar] [CrossRef]
- Carroll, P.R.; Hanrahan, J. Development and evaluation of an interprofessional student-led influenza vaccination clinic for medical, nursing and pharmacy students. Pharm. Pract. 2021, 19, 2449. [Google Scholar] [CrossRef] [PubMed]
- Yuan, H.B.; Williams, B.A.; Fang, J.B.; Ye, Q.H. A systematic review of selected evidence on improving knowledge and skills through high-fidelity simulation. Nurse Educ. Today 2012, 32, 294–298. [Google Scholar] [CrossRef]
- La Cerra, C.; Dante, A.; Caponnetto, V.; Franconi, I.; Gaxhja, E.; Petrucci, C.; Alfes, C.M.; Lancia, L. Effects of high-fidelity simulation based on life-threatening clinical condition scenarios on learning outcomes of undergraduate and postgraduate nursing students: A systematic review and meta-analysis. BMJ Open 2019, 9, e025306. [Google Scholar] [CrossRef] [PubMed]
- McCoy, C.E.; Rahman, A.; Rendon, J.C.; Anderson, C.L.; Langdorf, M.I.; Lotfipour, S.; Chakravarthy, B. Randomized Controlled Trial of Simulation vs. Standard Training for Teaching Medical Students High-quality Cardiopulmonary Resuscitation. West. J. Emerg. Med. 2019, 20, 15–22. [Google Scholar] [CrossRef]
- Jessee, J.K.; Miller, A.; Ebied, A.M. Beyond the Classroom: An Observational Study to Assess Student Pharmacists’ Confidence and Perception of a High-Fidelity Manikin Chemotherapy Infusion Reaction Simulation. J. Pharm. Technol. 2022, 38, 135–141. [Google Scholar] [CrossRef]
- Morris, A.; Young, G.; Roller, L.; Li, F.; Takamoto, P.; Baumgartner, L. High-fidelity simulation increases pharmacy resident perceived competence during medical emergencies. Curr. Pharm. Teach. Learn. 2019, 11, 1016–1021. [Google Scholar] [CrossRef] [PubMed]
- Abajas-Bustillo, R.; Amo-Setién, F.; Aparicio, M.; Ruiz-Pellón, N.; Fernández-Peña, R.; Silio-García, T.; Leal-Costa, C.; Ortego-Mate, C. Using High-Fidelity Simulation to Introduce Communication Skills about End-of-Life to Novice Nursing Students. Healthcare 2020, 8, 238. [Google Scholar] [CrossRef] [PubMed]
- Bingham, A.L.; Sen, S.; Finn, L.A.; Cawley, M.J. Retention of advanced cardiac life support knowledge and skills following high-fidelity mannequin simulation training. Am. J. Pharm. Educ. 2015, 79, 12. [Google Scholar] [CrossRef]
- Vyas, D.; McCulloh, R.; Dyer, C.; Gregory, G.; Higbee, D. An interprofessional course using human patient simulation to teach patient safety and teamwork skills. Am. J. Pharm. Educ. 2012, 76, 71. [Google Scholar] [CrossRef]
- Thompson Bastin, M.L.; Cook, A.M.; Flannery, A.H. Use of simulation training to prepare pharmacy residents for medical emergencies. Am. J. Health Syst. Pharm. 2017, 74, 424–429. [Google Scholar] [CrossRef]
- ABDA. Schutzimpfungen in Apotheken (Vaccination in Pharmacies). Available online: https://www.abda.de/fuer-apotheker/schutzimpfungen/schutzimpfungen-in-apotheken/ (accessed on 27 December 2023).
- Carroll, P.R.; Chen, Y.; Vicheth, P.; Webber, P.; Hanrahan, J.R. Evaluation of a vaccination training program for pharmacy graduands in Australia. Curr. Pharm. Teach. Learn. 2020, 12, 850–857. [Google Scholar] [CrossRef] [PubMed]
- Au, M.L.; Tong, L.K.; Li, Y.Y.; Ng, W.I.; Wang, S.C. Impact of scenario validity and group size on learning outcomes in high-fidelity simulation: A systematics review and meta-analysis. Nurse Educ. Today 2023, 121, 105705. [Google Scholar] [CrossRef] [PubMed]



| Bonn (n = 33) | Duesseldorf (n = 42) | Greifswald (n = 49) | Total (n = 124) | |
|---|---|---|---|---|
| Age | ||||
| Mean (±SD) | 23.91 (±1.88) | 24.79 (±3.54) | 23.31 (±1.79) | 23.97 (±2.60) |
| Median | 24 | 24 | 23 | 23 |
| Range | 21–28 | 21–38 | 21–28 | 21–38 |
| Gender | ||||
| Female, n (%) | 23 (69.70) | 32 (76.19) | 28 (57.14) | 83 (66.94) |
| Male, n (%) | 10 (30.30) | 10 (23.81) | 21 (42.86) | 41 (33.06 |
| Previous or current experience (e.g., pharmaceutical technician, vaccination centre) | ||||
| No, n (%) | 28 (84.85) | 35 (83.33) | 37 (75.51) | 100 (80.65) |
| Yes, n (%) | 5 (15.15) | 7 (16.67) | 12 (24.49) | 24 (19.35) |
| Bonn (n = 33) Mean (CI) | Duesseldorf (n = 42) Mean (CI) | Greifswald (n = 49) Mean (CI) | Total (n = 124) Mean (CI) | p2-Value | ||
|---|---|---|---|---|---|---|
| Q1 | Pre-Training | 2.42 (0.53) | 1.24 (0.41) | 2.04 (0.47) | 1.87 (0.28) | <0.01 |
| Post-Training | 3.88 (0.27) | 3.76 (0.25) | 3.98 (0.26) | 3.88 (0.15) | 0.26 | |
| p1-Value | <0.01 | <0.01 | <0.01 | <0.01 | ||
| Q2 | Pre-Training | 2.39 (0.43) | 2.07 (0.33) | 2.61 (0.40) | 2.37 (0.23) | 0.17 |
| Post-Training | 3.82 (0.28) | 3.60 (0.28) | 3.90 (0.23) | 3.77 (0.15) | 0.31 | |
| p1-Value | <0.01 | <0.01 | <0.01 | <0.01 | ||
| Q3 | Pre-Training | 2.45 (0.48) | 1.93 (0.32) | 2.06 (0.34) | 2,12 (0.22) | 0.18 |
| Post-Training | 4.00 (0.24) | 4.14 (0.25) | 4.16 (0.23) | 4.11 (0.14) | 0.47 | |
| p1-Value | <0.01 | <0.01 | <0.01 | <0.01 | ||
| Q4 | Pre-Training | 2.12 (0.57) | 1.12 (0.34) | 2.04 (0.45) | 1.75 (0.27) | <0.01 |
| Post-Training | 3.94 (0.27) | 3.81 (0.33) | 3.94 (0.30) | 3.90 (0.18) | 0.74 | |
| p1-Value | <0.01 | <0.01 | <0.01 | <0.01 | ||
| Q5 | Pre-Training | 2.30 (0.40) | 1.81 (0.35) | 2.00 (0.36) | 2.02 (0.21) | 0.24 |
| Post-Training | 3.48 (0.23) | 3.43 (0.25) | 3.57 (0.27) | 3.50 (0.15) | 0.65 | |
| p1-Value | <0.01 | <0.01 | <0.01 | <0.01 | ||
| Q6 | Pre-Training | 1.85 (0.39) | 1.14 (0.34) | 1.51 (0.39) | 1.48 (0.22) | 0.04 |
| Post-Training | 3.33 0.30) | 3.14 (0.23) | 3.33 (0.32) | 3.27 (0.17) | 0.37 | |
| p1-Value | <0.01 | <0.01 | <0.01 | <0.01 | ||
| Bonn (n = 33) Mean (CI) | Duesseldorf (n = 42) Mean (CI) | Greifswald (n = 49) Mean (CI) | Total (n = 124) Mean (CI) | p-Value | |
|---|---|---|---|---|---|
| Q1 | 4.55 (0.24) | 4.69 (0.18) | 4.49 (0.21) | 4.57 (0.12) | 0.22 |
| Q2 | 3.67 (0.30) | 3.69 (0.29) | 3.88 (0.25) | 3.76 (0.16) | 0.60 |
| Q3 | 4.48 (0.27) | 4.55 (0.20) | 4.43 (0.22) | 4.48 (0.13) | 0.64 |
| Q4 | 4.39 (0.26) | 4.38 (0.23) | 4.39 (0.24) | 4.39 (0.14) | 0.94 |
| Q5 | 2.88 (0.47) | 3.10 (0.38) | 3.39 (0.41) | 3.15 (0.24) | 0.25 |
| Q6 | 4.36 (0.25) | 4.24 (0.24) | 4.39 (0.21) | 4.33 (0.13) | 0.67 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sayyed, S.A.; Kinny, F.A.; Sharkas, A.R.; Schwender, H.; Woltersdorf, R.; Ritter, C.; Laeer, S. Vaccination Training for Pharmacy Undergraduates as a Compulsory Part of the Curriculum?—A Multicentric Observation. Pharmacy 2024, 12, 12. https://doi.org/10.3390/pharmacy12010012
Sayyed SA, Kinny FA, Sharkas AR, Schwender H, Woltersdorf R, Ritter C, Laeer S. Vaccination Training for Pharmacy Undergraduates as a Compulsory Part of the Curriculum?—A Multicentric Observation. Pharmacy. 2024; 12(1):12. https://doi.org/10.3390/pharmacy12010012
Chicago/Turabian StyleSayyed, Shahzad Ahmad, Florian Andreas Kinny, Ahmed Reda Sharkas, Holger Schwender, Ronja Woltersdorf, Christoph Ritter, and Stephanie Laeer. 2024. "Vaccination Training for Pharmacy Undergraduates as a Compulsory Part of the Curriculum?—A Multicentric Observation" Pharmacy 12, no. 1: 12. https://doi.org/10.3390/pharmacy12010012
APA StyleSayyed, S. A., Kinny, F. A., Sharkas, A. R., Schwender, H., Woltersdorf, R., Ritter, C., & Laeer, S. (2024). Vaccination Training for Pharmacy Undergraduates as a Compulsory Part of the Curriculum?—A Multicentric Observation. Pharmacy, 12(1), 12. https://doi.org/10.3390/pharmacy12010012






